Abstract
Background
Because simultaneous liver and kidney transplantation has been limited as a standard practice because of a severe shortage of deceased donors in Japan, living donor (LD) liver transplantation alone (LTA) is indicated in most recipients with maintenance renal replacement therapy (MRRT).
Methods
A retrospective nationwide survey of LD LTA was performed for liver transplant patients on MRRT. The characteristics of donors and recipients, postoperative complications, survival rate, and causes of death were analyzed.
Results
In the adult cases (n = 28), the overall survival rate at 1 year and 5 years were 66.1% and 57.3%, respectively. When compared with those adults without MRRT (n = 237), it was significantly worse. In the 7 pediatric cases, the overall survival rate at 1 and 5 years were both 83.3%. Three adult recipients died of nonaneurysm cerebral hemorrhage after 1 year and 1 adult recipient died of acute heart failure after 7 months. In adult recipients with MRRT, graft weight versus standard liver volume, and duration and blood loss in LTA surgery were associated with poor outcomes after LD LTA. Multivariate analysis revealed that MRRT was highest hazard ratio on patient survival after LD LTA.
Conclusions
Early post-LD LTA mortality was higher in patients with MRRT than in those without MRRT with characteristic causes. Smaller grafts for size and a complicated surgery were associated with poor outcome after LD LTA. Thus, LD LTA in adult patients on MRRT should be carefully treated with meticulous postoperative management and follow-up.
In patients with end-stage kidney and liver failure, simultaneous kidney and liver transplantation (SLKT) is a therapeutic choice.1 However, because deceased donors are rarely available in Asian countries, liver transplantation alone (LTA) from a living donor (LD) is a realistic option for patients with end-stage liver disease on maintenance renal replacement therapy (MRRT).2 As compared with full-size liver transplantation, the graft for LD LTA is partial, which requires more meticulous fluid management because of the higher portal venous pressure.3 Therefore, patients with an impaired kidney function need careful management, especially with regard to immunosuppressive agents and antibiotic therapy.4
End-stage renal disease requiring dialysis is associated with poor health outcomes, including a 10-fold increase in risk of hospitalization and an expected life span between one fourth and one sixth that of the general population.5 In general and cardiac surgery, complication and mortality rates in dialysis patients have been the subject of several articles. Gajdos et al6 reported a significantly elevated risk of complications and death after nonemergent general surgery, especially in MRRT patients 65 years or older. The most common postoperative adverse events in dialysis patients were pulmonary complications, whereas the most lethal complications were vascular events (myocardial infarction or stroke). In addition, it is important to note that a correlation between mortality and nutritional parameters as well as physiological state was found in patients on long-term MRRT.
Therefore, if LT is to be considered, we have to carefully consider LTA unless simultaneous kidney transplantation is performed. Studies on LD LTA have not yet clearly elucidated its outcome. The aim of this retrospective study was to examine the outcome of LD LTA for patients with MRRT in a nationwide survey in Japan.
PATIENTS AND METHODS
Subjects
By the end of 2013, 219 deceased donor LT and 7255 LD liver transplantation (LDLT) procedures were registered with the Japanese Liver Transplantation Society (JLTS).7 Our nationwide survey in Japan was performed as a research project of the JLTS and was approved by the ethics committee of Nagasaki University Hospital (13120802) and the other participating facilities. The indications for performing LD LTA for MRRT were at the discretion of each facility. After initial surveillance, it was found that among patients on MRRT between 1996 and 2013, only 35 patients underwent LD LTA. Detailed data were collected for those 35 patients including 7 pediatric patients younger than 15 years from 13 facilities. Because LDLT is usually an elective procedure, thorough whole body surveillance was performed in each patient before LD LTA, including cardiovascular status. Before LD LTA, no cardiovascular diseases were reported.
As a control group, 237 LD LTA patients who were not on MRRT were analyzed for patient survival, and a multivariate analysis was conducted to determine a hazard model. Data for graft weight (GW)/recipient standard liver volume (SLV) were only available from the 237 patients who were registered with JLTS in 2012. Therefore, for this cohort, only patient survival up to 3 years was obtained and used for analysis.
The study was conducted in accordance with the Declaration of Helsinki of 2013.
Definition of MRRT
In adults, all patients who had an arteriovenous fistula (shunt) before LT were included in the study. They were usually on MRRT 3 times per week on outpatient basis. Patients with acute hemodialysis without MRRT were excluded from this study, including continuous venovenous hemodialysis. Patients who had been on MRRT and switched to continuous venovenous hemodialysis just before LT were included in this study. Of the pediatric patients, 5 were on peritoneal dialysis and 2 on maintenance HD on an outpatient basis. The baseline characteristics of the patients at the time of LD LTA are shown in Table 1.
TABLE 1.
Baseline demographics of the recipients and donors at time of LD LTA
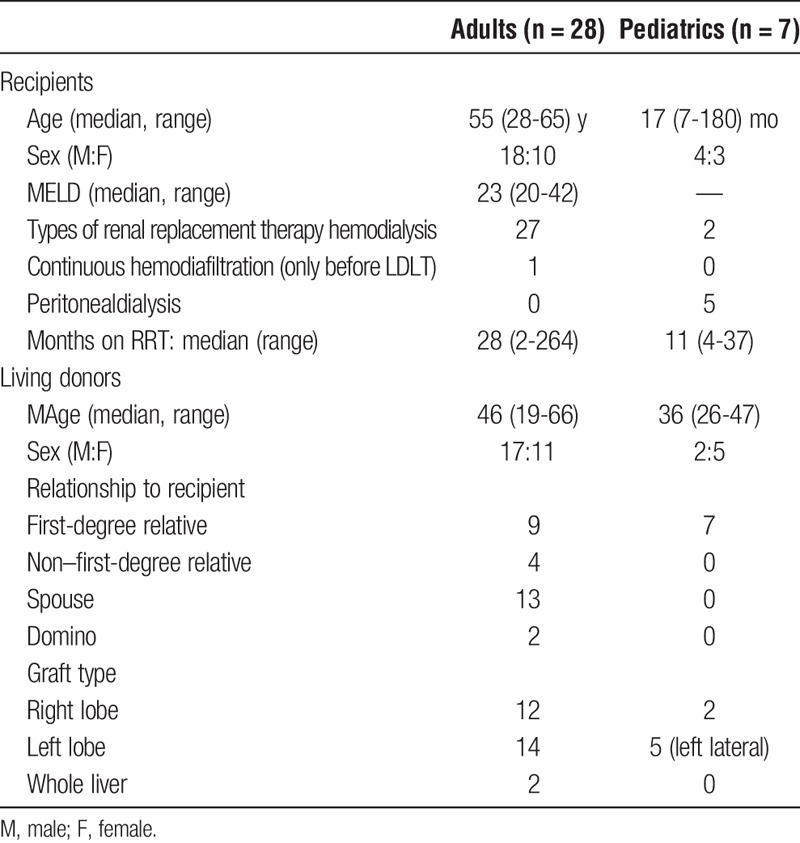
Variables
Basic information collected on the patients were age, sex, type of MRRT just before LTA, model for end-stage liver disease (MELD) score before LT, graft type, GW versus SLV and relation of the LD to the recipient. Standard liver volume of the recipient was calculated using the formula proposed by Urata et al.8 All data were subgrouped by adult and pediatric patients. Pediatric patients were defined as those younger than 15 years. The duration of MRRT, cause of renal disease, and indications for LTA were analyzed. In addition, the type of immunosuppression after LTA, patient survival, cause of death, and rate of secondary kidney transplantation were analyzed. Differences in the demographic characteristics between survival cases and deceased cases were analyzed as well.
Statistics
All data are expressed as the mean with standard deviation or median values with ranges. The statistical analysis was performed using the Mann-Whitney U test for continuous values and the χ2 test for categorical values. Patient survival rates were calculated using the Kaplan-Meier method and were compared using the log-rank test. Risk ratios are expressed as hazard ratios with confidence intervals (CI). The MELD score was not included among the variables for the multivariate analysis because MRRT is one of the factors in MELD score. Statistical significance was defined as a P value less than 0.05. The statistical analyses were performed with the JMP 11 software program (SAS Institute Inc., Cary, NC).
RESULTS
Recipient Characteristics
In 28 adults, the median age of the LD LTA recipients was 55 years old with a male-female ratio of 18:10. The median MELD score was 23. The MRRT immediately before LD LTA was regular MRRT in 27 patients and continuous veno-venous HD in 1 MRRT patient. The median period of MRRT was 28 months. On the other hand, the mean age of the pediatric LDLT recipients was 17 months old with a male-female ratio of 4:3. The MRRT before LD LTA for the pediatric patients was peritoneal dialysis in 5 and HD in 2. The median MRRT was 11 months (Table 1).
The indications for LD LTA in adult recipients included viral hepatitis in 10 patients (hepatitis B in 4, C in 5, and B+C in 1), and concomitant hepatocellular carcinoma in 5 of those 10 patients. Other causes included polycystic liver in 6, primary hyperoxaluria in 3, nonalcoholic steatohepatitis in 2, alcoholic liver cirrhosis in 3, primary sclerosing cholangitis in 1, congenital absence of the portal vein in 1, fulminant hepatitis in 1, and unknown origin in 1. For the 7 pediatric patients, the causes for LD LTA were primary hyperoxaluria in 5, congenital hepatic fibrosis in 1, and intrahepatic cholestasis in 1 (Table 2).
TABLE 2.
Indication of LD LTA and etiology of end-stage renal failure
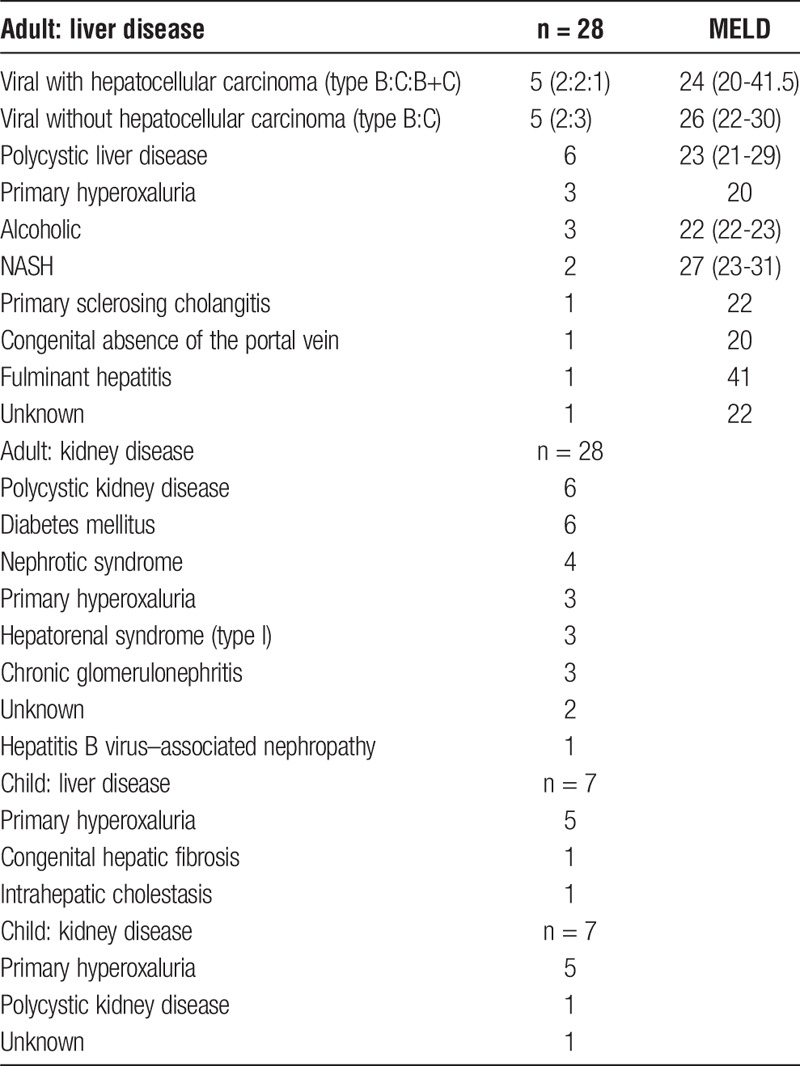
The etiologies of primary renal disease for MRRT in adults were polycystic kidney disease in 6 patients, diabetes mellitus in 6, nephrotic syndrome in 2, primary hyperoxaluria in 3, hepatorenal syndrome (type I) in 3, chronic glomerulonephritis in 3, unknown origin in 2, urethral stone in 1, and hepatitis B–related nephropathy in 1. On the other hand, primary hyperoxaluria was the major cause of the MRRT in pediatric patients, followed by polycystic kidney disease (Table 2).
LD Characteristics
The median age of the LD for the adult MRRT patients was 46 years with a male-female ratio of 17:11. The relationship to the LDLT recipient was a spouse in 13, a first-degree relative in 9, a non–first-degree relative in 4, and domino in 2. The grafts used for adult patients consisted of the right lobe in 12, the left lobe in 14, and the whole liver from a domino donor in 2. For pediatric LDLT, all LDs (median, 36 years; male-female, 2:5) were parents who donated the left lateral lobe of their liver in 5 and the right lobe in 2.
Liver Transplant Outcome
Patient survival after LD LTA in adult patients was 66.1% at 1 year and 57.3% at 5 years, with a median survival time of 3008 days (Figure 1). As compared with the control group without MRRT, the survival rate for adult LD LTA patients was significantly lower with MRRT (MRRT+ (n = 28) 1-year survival = 66.1%, 3-year survival = 57.3%; MRRT− (n=237) 1-year survival = 83.8%, 3-year survival = 80.0%) (Figure 2). In the pediatric patients, 5-year patient survival was 83.3% (Figure 1). Re-LT was not performed for any of the patients in the study.
FIGURE 1.
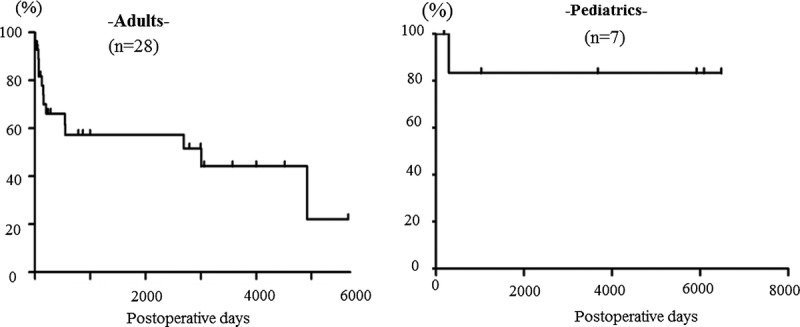
Overall patient survival after living donor liver transplantation alone for adult and pediatric patients with maintenance hemodialysis.
FIGURE 2.
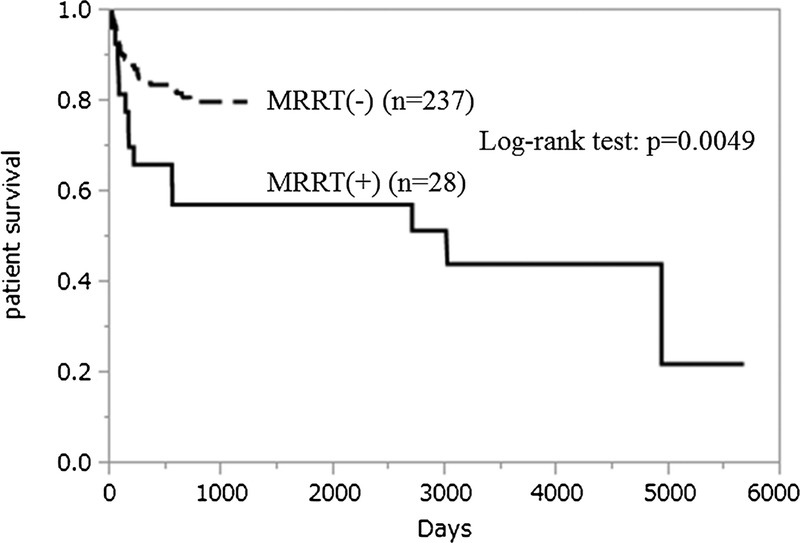
Overall patient survival after living donor liver transplantation for adults with and without maintenance hemodialysis.
Immunosuppression
Regarding immunosuppression, induction therapy was done mostly with tacrolimus and steroids. As a maintenance regimen 3 months after LD LTA, tacrolimus-based regimen was the most used. Regarding the route of the immunosuppressant, the oral or enteral route for both induction and maintenance regimens was the most frequently used.
Complications and Causes of Death After LDLT
In the adult patients, infection was noted as the most common postoperative complication in 14 cases (50%; 1 fungal, 4 cytomegalovirus, and 9 bacterial [1+ cytomegalovirus]), followed by abdominal hemorrhage in 7 (23%), biliary complication in 5 (16%) and vascular in 2 (6%). In the pediatric patients, only 1 experienced infection, which was treated successfully. The rate of acute cellular rejection was the same (20-30%) in both the adult and pediatric LD LTA patients (Tables 2 and 3).
TABLE 3.
Cause of death after LD LTA
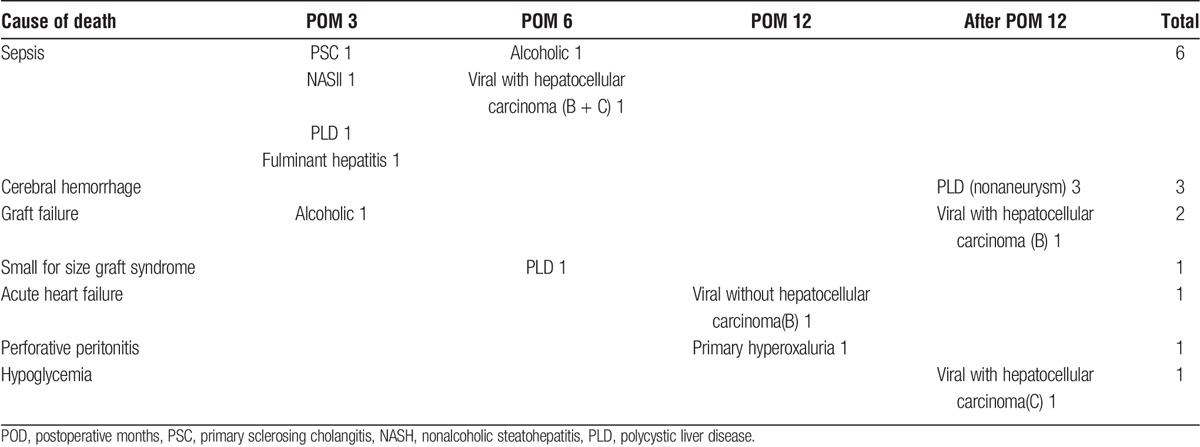
Within 6 months, 6 adult patients died of sepsis due to 5 bacterial and 1 fungal infection. Cause of death was nonaneurysm cerebral hemorrhage in 3, probably because of damage to the peripheral blood vessels due to long-term MRRT. In addition, the 1 death from acute heart failure was possibly due to fluid imbalance due to the MRRT. One pediatric on MRRT patient with hyperoxaluria died of perforative peritonitis (Table 3).
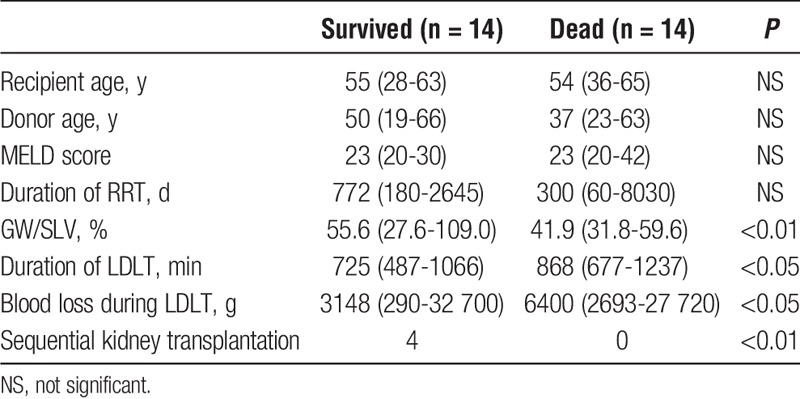
Smaller GW per SLV ratio, duration of LD LTA surgery, and blood loss during LD LTA were significantly associated with poor outcomes after LD LTA (Table 4).
TABLE 4.
Difference in character of adult LD LTA recipients
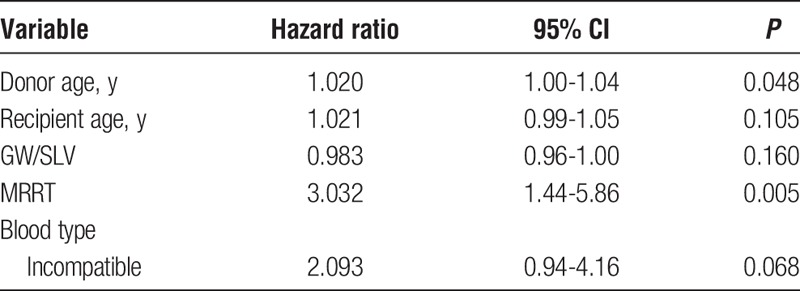
Multivariate Analysis on Patient Survival Rates
The demographics of the patients who underwent LD LTA with or without MRRT are shown in Table 5. The number of deaths included 14 with MRRT and 46 without MRRT. The five factors used for a multivariate analysis were all factors registered in the Japan Liver Transplant Registry in 2012, and are specified in Table 6. Because MRRT is included in the MELD score, there was a significant difference in the MELD scores between the 2 cohorts. A multivariate analysis showed MRRT to be the highest hazard ratio with certain CI for patient survival after LD LTA (Table 6).
TABLE 5.
Demographic characteristics of LD LTA recipients for comparison
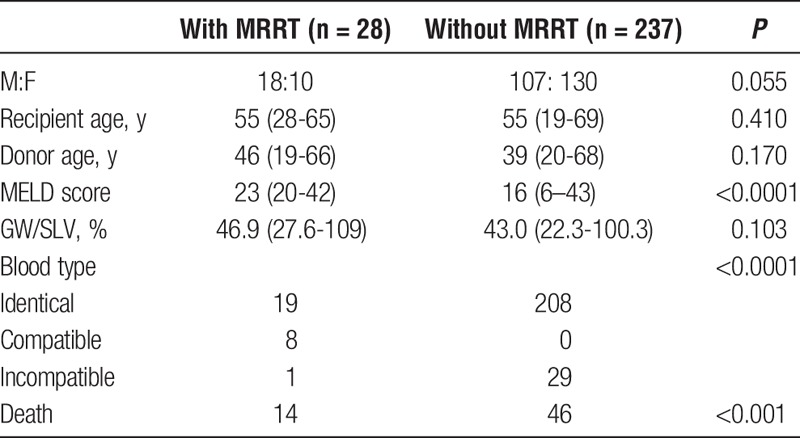
TABLE 6.
Multivariate analysis for patient survival after LD LTA
RRT After LD LTA
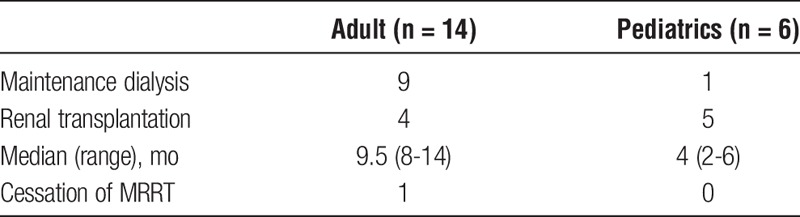
After LD LTA, of the 20 surviving patients, 10 patients continued MRRT and 9 underwent secondary sequential kidney transplantation from a LD at median 9.5 months after LD LTA in adults and 4 months after LD LTA in pediatrics, all from the previous liver donors. In 1 adult patient (a 57-year-old man with MELD 22), MRRT became unnecessary at 1 year after the LD LTA. The primary liver and kidney diseases of the patient were alcoholic liver cirrhosis and nephrotic syndrome (Table 7).
TABLE 7.
RRT after LD LTA (survived cases)
DISCUSSION
This nationwide survey demonstrated that the outcome of LD LTA for adult patients on MRRT was worse than for adult patients without MRRT, which was described in the annual report of the JLTS (overall survival, 80.5% at 1 year and 71.8% at 5 years in adults, and 88.5% and 85.7% in pediatrics, respectively).7 In addition, it was shown that there were specific causes of death such as cerebrovascular disease after LTA for adult patients with MRRT. On the other hand, the outcome for pediatric patients was acceptable, although they were mostly on peritoneal dialysis not on HD. Although there have been some case reports that showed favorable results after LTA on MHD, this is the first large study reporting LTA on MRRT patients, especially with LD.2
The American College of Surgeons National Surgical Quality Improvement Program data sets for 2005 to 2007 demonstrated CKD 5 (eGFR less than 15 mL/min or dialysis) had an adjusted hazard ratio for 30-day mortality of 3.05 (95% CI, 2.68-3.47) in general and vascular surgery.9 Squires et al10 demonstrated that preoperative serum creatinine of 1.8 mg/dL or greater identifies patients at significantly increased risk of postoperative major complications, particularly respiratory failure after major hepatectomy. Therefore, even for general surgeries, few patients with substantial renal insufficiency are deemed good operative candidates.
Northup et al11 demonstrated a duration of pretransplant RRT for more than 90 days to be a significant predictor of lack of spontaneous recovery of renal function after LT. In the most recent literature, Chang et al12 demonstrated using a Markov model that the 1-year survival rate of patients who received pretransplant RRT more than 30 days before SLKT were able to show a significantly better survival rate than with LTA followed by immediate kidney transplantation despite their MELD score.
Using the United Network for Organ Sharing database, Schmitt et al13 demonstrated that SLKT patients had a non-significant difference in survival compared with patients who had undergone LTA at 1 year (81.0% vs 78.8%). In patients undergoing SLKT, there was an improved survival at 1 year compared with LTA patients on hemodialysis. In patients with renal failure, but not on hemodialysis, there was no difference in survival between SLKT and LTA. However, that study did not separate patients with acute and chronic renal failure as the reason for the hemodialysis.14 In addition, their patients' mean waiting time for LT or combined transplantation were 200 and 233 days, respectively.15 The period of hemodialysis before LT was not shown. In Japan, because simultaneous liver and kidney transplantation has been limited as a standard practice because of a severe shortage of deceased donors, the only sequential liver and kidney transplants were those from the same donor. Therefore, as shown in Table 7, the length of time between LD LTA and kidney transplant was rather long.
As we hypothesized, in our study, smaller graft size for recipients and complicated surgery were associated with poor outcome after LD LTA. However, these findings might not be specific for MRRT patients, because these patients' cause of death was mainly sepsis until 6 months. However, as patients on MRRT are said to be prone to infection and cerebrovascular disease, posttransplant attention to these potentials should be given to these patients on MRRT without secondary renal transplantation. When we compared the MRRT+ cohort to the cohort without MRRT, using multivariate analysis, MRRT had the highest hazard ratio for patient survival after LDLT.
Of 4 patients with secondary kidney transplant, 3 had oxalosis, and 1 had liver cirrhosis due to hepatitis C virus infection with hepatocellular carcinoma. The 4 patients received both kidney and liver transplants from the same LD. However, a partial liver was initially transplanted followed by kidney from the same LD to reduce the burden on the LDs. As described about, 3 of 4 hyperoxaluria patients survived after LD LTA and subsequent kidney transplantation. When even including these hyperoxaluria patients, the overall patient survival on MRRT was lower than those without MRRT probably because of the difficulty of postoperative management after LTA with partial liver requiring meticulous fluid management as one of the reasons. Additionally, because of the small number of patients on MRRT in this study, we believe that a stratified survival analysis would not provide any conclusive results. This was the reason why we placed all patients together in this analysis.
As indicated, the MELD score did not reflect the severity of liver diseases in our cohort. First of all, as described in the Results section, indications for LD LTA were polycystic disease in 6, HCC in LC in 5, hyperoxaluria in 3, and primary sclerosing cholangitis, portal vein absence in 1, none of which would increase the MELD score. Therefore, the pre-LD LTA MELD score in our cohort did not increase much.
In conclusion, this nationwide survey in Japan analyzed the results of LD LTA in patients with MRRT for the first time. Early post-LD LTA mortality was higher in patients with MRRT in adults but still can be considered as a life-saving procedure. Cerebrovascular disease was recognized as a characteristic complication in adult recipients with MRRT. In pediatric MRRT patients, LD LTA before kidney transplantation could be considered acceptable treatment. Thus, LD LTA in adult patients on MRRT should be carefully treated with meticulous postoperative management and follow-up.
ACKNOWLEDGMENTS
The authors thank Shintato Yagi and Akira Mori (Kyoto University), Tomoharu Yoshizumi and Toru Ikegami (Kyushu University), Toshihiko Ikegami. (Shinshu University), Yorihisa Urata (Osaka City University), Hiroyuki Sugo and Noboru Nakayama (Juntendo University), Ikuo Takeda (Tohoku University), Akinobu Taketomi (Hokkaido University), Hiroyuki Takamura (Kanazawa University), Mitsuhisa Takatsuki (Nagasaki University), Yoshinobu Sato and Takashi. Kobayashi (Niigata University), Takayuki Takeichi (Kumamoto University), and Ayumi Tsuji (Nagasaki University) for their assistance with the data collection.
Footnotes
Published online 2 May 2016.
The authors declare no conflicts of interest.
All authors listed on the article's title page participated meaningfully in the study and have seen and approved the final manuscript. In accordance with ICMJE guidelines for authorship, this article's authors have made substantial contributions to the article's conception design; acquisition, analysis, and interpretation of data; drafting and critically revising the article for important intellectual content; giving final approval of the version to be published.
Contributor Information
Collaborators: for the Japanese Liver Transplant Society
REFERENCES
- 1.Brennan TV, Lunsford KE, Vagefi PA, et al. Renal outcomes of simultaneous liver-kidney transplantation compared to liver transplant alone for candidates with renal dysfunction. Clin Transplant. 2015;29:34–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Morita K, Shirabe K, Yoshizumi T, et al. Feasible isolated liver transplantation for a cirrhotic patient on chronic hemodialysis. Case Rep Gastroenterol. 2013;7:299–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Samstein B, Smith AR, Freise CE, et al. Complications and their resolution in recipients of deceased and living donor liver transplants: findings from the A2ALL cohort study. Am J Transplant. 2016;16:594–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olthoff KM, Smith AR, Abecassis M, et al. Defining long-term outcomes with living donor liver transplantation in North America. Ann Surg. 2015;262:465–475; discussion 473–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thamer M, Ray NF, Fehrenbach SN, et al. Relative risk and economic consequences of inpatient care among patients with renal failure. J Am Soc Nephrol. 1996;7:751–762. [DOI] [PubMed] [Google Scholar]
- 6.Gajdos C, Hawn MT, Kile D, et al. Risk of major nonemergent inpatient general surgical procedures in patients on long-term dialysis. JAMA Surg. 2013;148:137–143. [DOI] [PubMed] [Google Scholar]
- 7.Umeshita K, Inomata Y, Furukawa H. Liver transplantation in Japan—registry by the Japanese Liver Transplantation Society. Ishoku. 2016. (in Japanese). [DOI] [PubMed] [Google Scholar]
- 8.Urata K, Kawasaki S, Matsunami H, et al. Hepatology. 1995;21:1317–1321. [PubMed] [Google Scholar]
- 9.Gaber AO, Moore LW, Aloia TA, et al. Cross-sectional and case-control analysis of the association of kidney function staging with adverse postoperative outcomes in general and vascular surgery. Ann Surg. 2013;258:169–177. [DOI] [PubMed] [Google Scholar]
- 10.Squires MH, III, Lad NL, Fisher SB, et al. The effect of preoperative renal insufficiency on postoperative outcomes after major hepatectomy: a multi-institutional analysis of 1,170 patients. J Am Coll Surg. 2014;219:914–922. [DOI] [PubMed] [Google Scholar]
- 11.Northup PG, Argo VB, Bakhru MR, et al. Pretransplant predictors of recovery of renal function after liver transplantation. Liver Transpl. 2010;16:440–446. [DOI] [PubMed] [Google Scholar]
- 12.Chang Y, Gallon L, Jay C, et al. Comparative effectiveness of liver transplant strategies for end-stage liver disease patients on renal replacement therapy. Liver Transpl. 2014;20:1034–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schmitt TM, Kumer SC, Al-Osaimi A, et al. Combined liver-kidney and liver transplantation in patients with renal failure outcomes in the MELD era. Transpl Int. 2009;22:876–883. [DOI] [PubMed] [Google Scholar]
- 14.Gonwa TA, McBride MA, Anderson K, et al. Continued influence of preoperative renal function on outcome of orthotopic liver transplant (OLTX) in the US: where will MELD lead us? Am J Transplant. 2006;6:2651–2659. [DOI] [PubMed] [Google Scholar]
- 15.Compagnon P, Metzler P, Samuel D, et al. Long-term results of combined liver-kidney transplantation for primary hyperoxaluria type 1: the French experience. Liver Transpl. 2014;20:1475–1485. [DOI] [PubMed] [Google Scholar]


