Abstract
Background:
A modified Michelassi strictureplasty over the ileocaecal valve or ileocolic anastomosis could be an alternative to ileocaecal resection. This study assessed the outcome of the modified Michelassi strictureplasty in patients with extensive stenotic terminal ileal Crohn’s disease [CD].
Methods:
This type of strictureplasty was proposed to all patients with an extensive strictured [neo-] terminal ileal segment [> 20 cm]. Short- and long-term outcome data were retrieved from a prospectively maintained database. Safety and medium-term efficacy were studied, using both postoperative magnetic resonance enterography [MRE] and ileocolonoscopy at 6 months.
Results:
Between June 2009 and September 2014, 29 CD patients had a modified strictureplasty [male 9/29, median age 38 [range: 16–64] years]. The median length of strictureplasty was 50 [27–110] cm. Twelve patients underwent a total of 30 additional procedures during surgery, mainly additional short strictureplasties, but also segmental resections. The majority had a laparoscopic-assisted procedure. Median length of hospital stay was 9 [6–17] days. Two patients had an early rescue procedure to oversew a small anastomotic leak. MRE and ileocolonoscopy at follow-up showed a remarkable regression of inflammation and bowel wall thickness. Clinical recurrence, necessitating initiation or modification of medical therapy, and surgical recurrence were reported in 11 and 1 patient after a median follow-up of 21 [1–54] months, respectively.
Conclusion:
A modified long Michelassi strictureplasty appears to be safe in patients with extensive stricturing Crohn’s ileitis. Significant mucosal and bowel wall healing is observed and suggests that clearance of microbial stasis may play a role in this process.
Keywords: Strictureplasty, Crohn’s disease, terminal ileum
1. Introduction
Despite important advances in drug development, including the introduction of biological therapies, medical treatment fails to treat penetrating and fibrostenotic complications of Crohn’s disease satisfactorily, rendering surgery unavoidable. About half of Crohn’s patients will need surgery at least once during their disease course.1,2 Bowel-sparing strategies are the cornerstone of surgery in order to avoid short bowel syndrome after repeated bowel resections. About 40% of the patients will indeed need a second surgical intervention due to CD recurrence, with an 8% risk of developing intestinal failure in the long term because of repeated extensive resections.3,4,5
Several types of strictureplasties have emerged to treat stenotic segments.6 Both the Heineke-Mickulicz [HM] and the Finney strictureplasties are considered ‘conventional’ strictureplasties.6 HM is appropriate to treat short strictures of less than 7cm. A Finney strictureplasty is able to treat longer segments; however, a bypass with a giant lateral diverticulum is then created, leading to bacterial overgrowth.7 Conventional strictureplasties are therefore not suitable to bridge long affected segments. More recently the side-to-side isoperistaltic strictureplasty [SSIS] was described to treat longer stenotic segments or several consecutive strictures close to each other, the so-called chain of sausages.8 In the latter case, subsequent HM could not be performed because of the increased traction on the consecutive suture lines. The introduction of the SSIS gave the surgeon an additional tool to avoid resection of long affected segments and subsequently decrease the risk of short bowel syndrome.
Besides the ability to treat long segments, sparing bowel length by avoiding resections, the SSIS is safe in terms of morbidity and mortality.9,10 Moreover, mucosal healing within the strictureplasty has been reported.11
We performed SSIS in a series of CD patients with either primary or secondary extensive stenotic [neo-] terminal ileal CD. The aim was to assess short- and medium-term outcome, including the need for re-operation or medical therapy and assessment of endoscopic and transmural response.
2. Materials and Methods
All patients with extensive stricturing terminal ileal CD eligible for an SSIS were assessed during weekly multidisciplinary meetings involving radiologists, gastroenterologists, and colorectal surgeons. Small bowel imaging (computed tomography [CT[ or magnetic resonance enterography [MRE]) and colonoscopies were reviewed and patients with stenotic [neo-] terminal Crohn’s ileitis ≥ 20cm and in the absence of a fistula, abscess or phlegmone, were proposed for strictureplasty. Upon consent, the ultimate feasibility of the strictureplasty was assessed during surgery.
2.1. Surgery
Primary cases were approached laparoscopically to mobilise the right colon. A 12-mm trocar was placed just underneath the umbilicus. Three 5-mm trocars were subsequently placed in the left upper quadrant, the left lower quadrant ,and the hypogastrium. An inferomedial approach was used to mobilise the ascending colon including the hepatic flexure, in order to end up with a complete mobile right hemicolon. If laparoscopy was not possible, the same mobilisation was performed by laparotomy.
In laparoscopic cases, extraction of the terminal ileum was done through a transumbilical incision. The length of incision was not measured but the incision was lengthened slightly to enable reduction of the bulky strictureplasty into the abdomen. Once the bowel was externalised, the feasibility of a strictureplasty was assessed. The presence of any septic complication [mesenteric fistula or abscess, not detected on preoperative imaging], an excessively thickened mesentery, or marked fat creeping covering the complete serosal surface, were contraindications to performing a strictureplasty. In those patients an ileocaecal resection was performed.
A suitable place to divide the bowel was assessed in the middle of the affected segment. Since bowel wall fibrosis and thickness can be pronounced, a relatively soft spot should be used for bowel division. This enables the surgeon to avoid too much traction on the inlet stitches because of rigid tissue, which may cause a leak. The most proximal segment was then slid over the ileocaecal valve and longitudinally opened in order to start the posterior suture, starting from the caecum towards the more proximal segments. After ending the posterior anastomosis, the distal segment including the caecum and the ileocaecal valve were opened. From there on the anterior suture line was initiated. A single-layer, interrupted suture using Vicryl 2-0 [Ethicon®, Cincinnati, USA] was used. Haemostasis of mucosal bleeding was controlled with separated Monocryl 3-0 stitches [Ethicon®, Cincinnati, USA], when necessary.
A relative stricture at the inlet of the SSIS was observed during follow-up in the 10 first patients. Therefore, a Sasaki modification at the inlet was performed in the subsequent cases.12 This modification consisted of performing an HM strictureplasty at the inlet of the strictureplasty, in order to obtain a wider inlet, avoiding any stricture [Figure 2C]. A drain was used in the first cases, but omitted in the latter ones after the occurrence of a leak due to suction of the drain on the anastomosis. The surgical technique is shown in Figures 1 and 2.
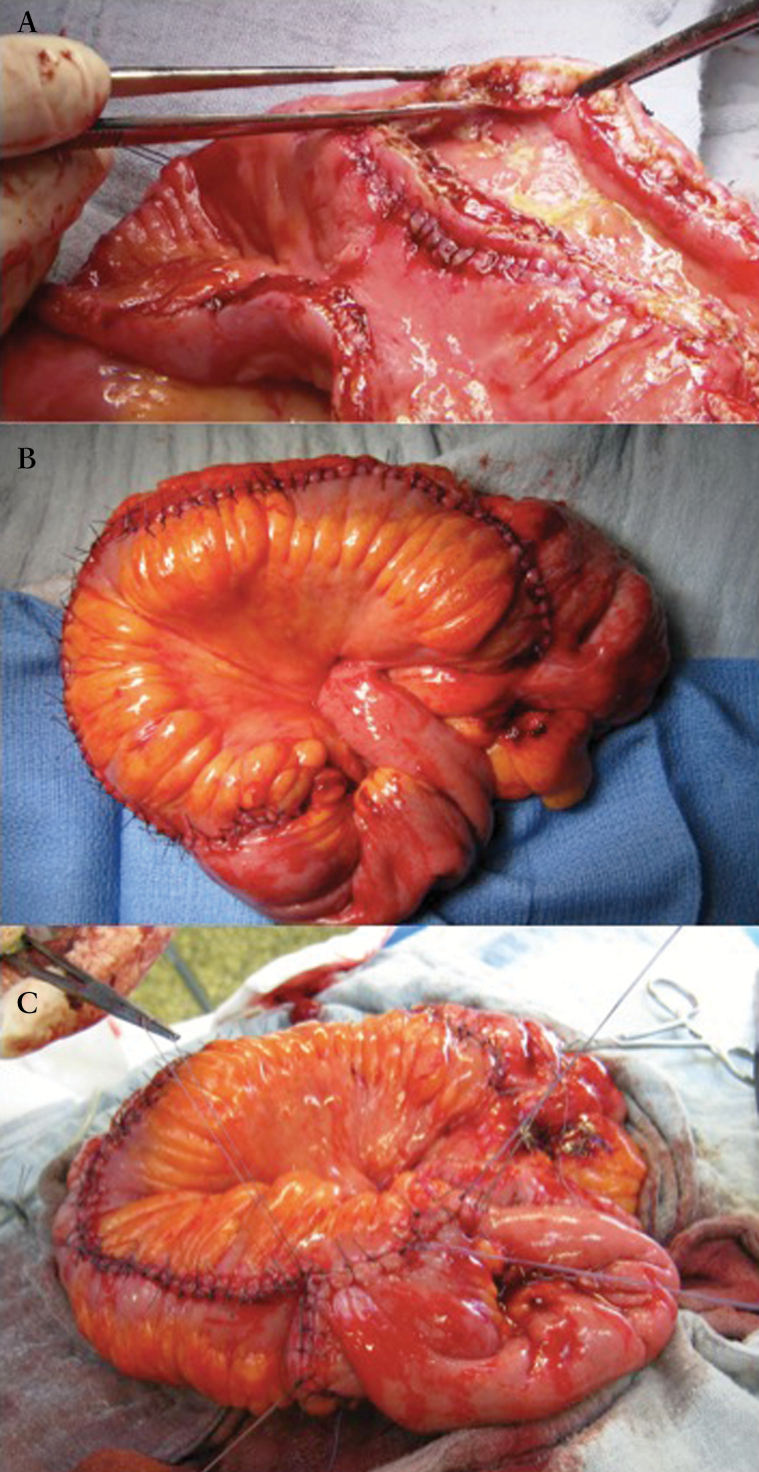
Figure 2.
A) the thickened bowel wall and prominent serpenginous ulcera are clearly visible on this peroperative picture. B) SSIS over the ileocecal valve. C) A Sasaki modification is made at the inlet of the strictureplasty.
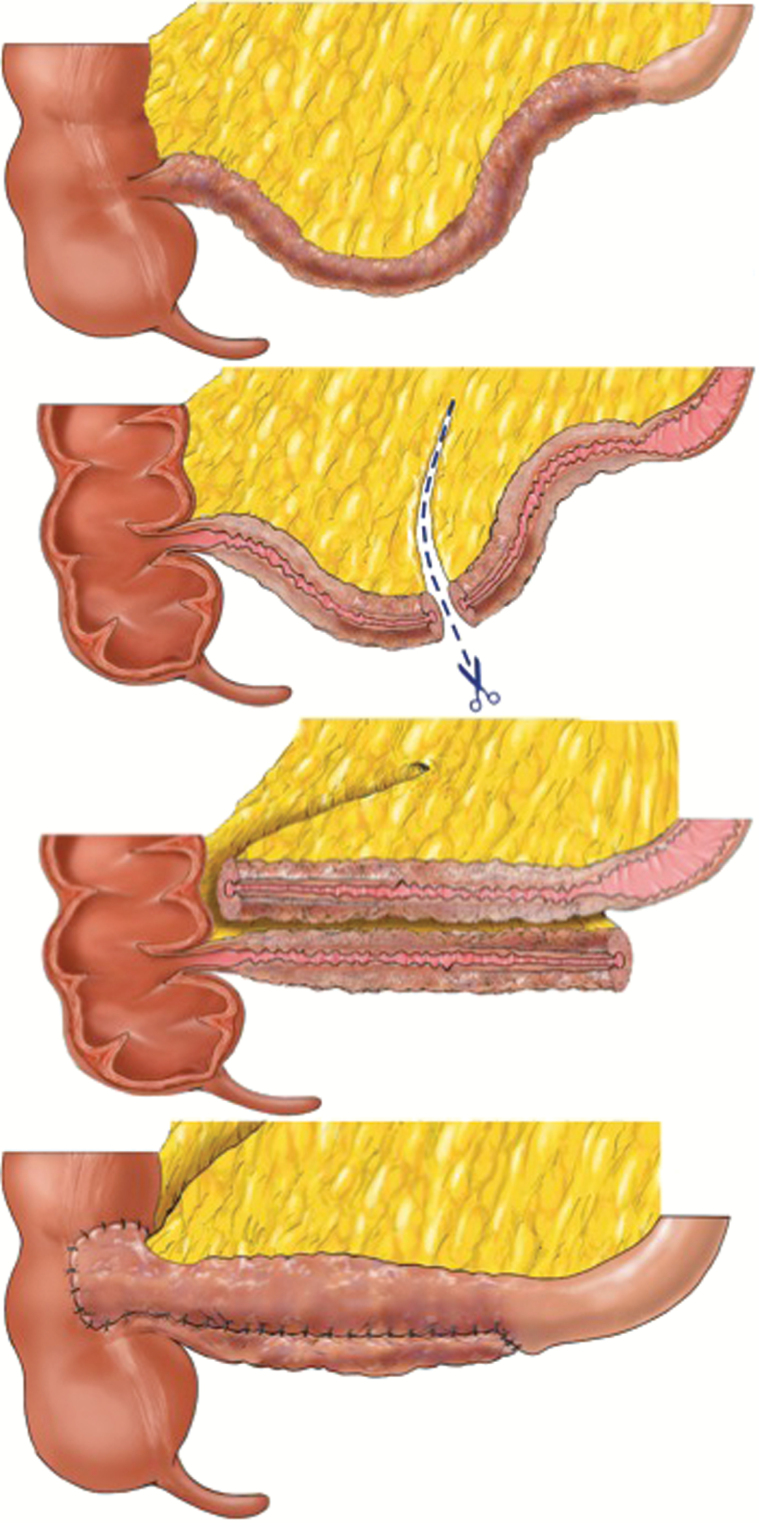
Figure 1.
The stenotic terminal ileum is divided in the middle. The proximal segment is slid over the distal segment, including the ileocaecal valve. A side-to-side isoperistaltic strictureplasty is than performed with separate stitches.
2.1. Follow up
Postoperative morbidity was classified using the Clavien-Dindo score.13
Standardised clinical follow-up was done at 1 and 6 months. Patients had an ileocolonoscopy and MRE at 6 months. The first five patients of the study had medical prophylaxis after surgery, whereas in the subsequent patients medical treatment was only restarted based on both the postoperative clinical, endoscopic, and radiological findings. Patients with active Crohn’s disease outside the strictureplasty were kept on medical treatment after surgery.
Clinical recurrence was defined as either symptomatic or asymptomatic endoscopic recurrence or persistent inflammation requiring medical treatment. Surgical recurrence was defined as the need for any surgical intervention with either resection or strictureplasty at the site of the primary strictureplasty.
As no specific score has been developed to assess endoscopic recurrence in a long strictureplasty, a simplified endoscopic score for Crohn’s disease [SES-CD] was therefore used as surrogate, only taking the terminal ileum into account [range 0–12].14 Two dedicated gastroenterologists [SV, MF] scored all endoscopies independently.
Patients who underwent both a preoperative and a postoperative MRE in our centre were assessed using the Magnetic Resonance Index of Activity [MaRIA] score to compare the preoperative and postoperative situations at the site of strictureplasty.15 Two independent radiologists [JR, DVB], with more than 10 years of experience in bowel imaging, assessed the MaRIA scores.
2.3. Statistical analysis
Descriptive statistics were performed on all data. Values are expressed as median and range or mean and standard deviation [SD]. Paired t-testing was used to compare preoperative and postoperative MaRIA scores with the inter-observer variability for the SES-CD score. The reproducibility coefficient [RC] and intra-class correlation [ICC] were calculated for both scores [SES-CD and MaRIA]. The RC refers to a 95% range of expected absolute inter-observer differences, and the ICC refers to the consistency of quantitative measures made by two different observers. A high RC represents therefore a poor reproducibility, whereas a low score reflects good inter-observer reproducibility. On the other hand, a high ICC reflects a high consistency in measures between two observers.
3. Results
3.1. Patients
Between June 2009 and September 2014, a total of 29 patients were operated [male 9/29, median age 38 [16–64] years]. Median disease duration was 8 [0–34] years; 26 patients underwent primary surgery with a strictureplasty over the ileocaecal valve. Three patients had a strictureplasty over the ileocolic anastomosis after previous ileocolic resection. The median length of strictureplasty was 50 [27–110] cm. Patients’ characteristics and surgical details are depicted in Tables 1 and 2.
Table 1.
Study population characteristics; n [%].
| Gender | |
| Male | 9 [31%] |
| Female | 20 [69%] |
| Median age at surgery, years [range] | 38 [16–64] |
| Disease duration in years [range] | 8 [0–34] |
| Montréal classification | |
| Age [years] | |
| A1 [< 17] | 5 [17%] |
| A2 [17–40] | 18 [62%] |
| A3 [> 40] | 6 [21%] |
| Location | |
| L1 [terminal ileum] | 22 [76%] |
| L3 [ileocolic] | 7 [24%] |
| Behaviour | |
| B1 [non structuring, non penetrating] | - |
| B2 [stricturing] | 26 [90%] |
| B3 [penetrating] | 3 [10%] |
| P [anal involvement] | 4 [14%] |
| Preoperative Crohn’s medication | |
| None | 6 [21%] |
| Anti-TNF alpha | 16 [76%] |
| Mesalazine | 3 [10%] |
| Vedoluzimab | 1 [3%] |
| Methylprednisolone | 2 [7%] |
| Budesonide | 4 [14%] |
| Smoking | 11 [38%] |
TNF, tumour necrosis factor.
Table 2.
Surgical characteristics and postoperative outcome, n [%].
| Access | |
| Laparoscopy | 24 [83%] |
| Laparotomy | 5 [17%] |
| Conversion to laparotomy | - |
| Median length of treated segment in cm [range] | 50 [27–110] |
| Additional surgical procedures | |
| HM-strictureplasty | 20 |
| Judd strictureplasty | 2 |
| Segmental enterectomy | 6 |
| Anterior resection | 1 |
| Reversal of Hartmann resection | 1 |
| Median duration of hospital stay [range] | 9 [617] |
| Median length of postoperative ileus [range] | 5 [212] |
| Postoperative morbidity | |
| Clavien-Dindo classification | |
| 0 | 16 [55%] |
| 1 | 4 [14%] |
| 2 | 6 [21%] |
| 3a | - |
| 3b | 3 [10%] |
| 4 | - |
| Postoperative prophylactic treatment | |
| None | 24 [83%] |
| Anti-TNF alpha | 4 [14%] |
| Methothrexate | 1 [3%] |
HM = Heineke-Mickulicz strictureplasty; TNF, tumour necrosis factor.
3.2. Postoperative morbidity and mortality
The median length of stay was 9 [6–17] days with prolonged postoperative ileus being the main reason for delayed discharge [median: 5 [2–12] days] [Table 2]. Two patients had an anastomotic leak in the early postoperative period. The first case was a small suction lesion created by the drain left against the suture line. The other case presented with a small leak at the inlet of the strictureplasty, created by too much traction on the stitches. Both strictureplasties could be saved by additional stitches. One patient had a re-look laparoscopy to exclude a leak, because of high inflammatory parameters. No leak was found and the patient was further treated with antibiotics. Following these cases, no drains were left behind and special attention was given to the choice of the inlet of the strictureplasty to avoid traction on those stitches. No anastomotic leaks were reported in the last 24 patients. Clavien-Dindo classification is represented in Table 2. No mortality was reported.
3.3. Postoperative healing
Six of the 29 patients received immediate medical therapy postoperatively; the remaining 23 patients did not receive any therapy after surgery. In the first five patients, the policy was to prescribe immediate postoperative medical treatment because of the remaining mucosal inflammation within the strictureplasty, and medical treatment was continued in another patient for active rheumatoid arthritis. Median follow-up was 21 [1–54] months; 26 patients had a postoperative ileocolonoscopy [Figure 3]. Three patients refused to have an ileocolonoscopy in our centre. After a median interval of 6 months [range: 2–20], median SES-CD score was 4 [0–8] and 5 [0–10]. The mean interobserver difference was 0.23 [p = 0.41]. Intra-class correlation was 0.774 [95% CI: 0.559–0.892], the reproducibility coefficient equalling 3.3.
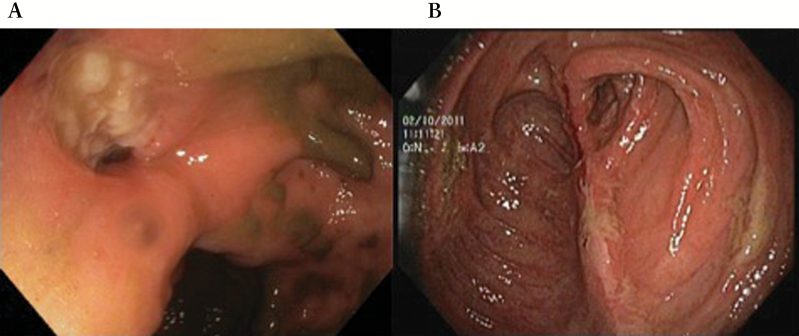
Figure 3.
A) Preoperative picture of the caecum with on the left side the stenotic and ulcerated ileocaecal valve. B) Picture 6 months after surgery within the strictureplasty with a clearly visible longitudinal suture line. Only some superficial ulcers are visible on the suture line.
In all, 25 patients had a postoperative MRE at a median time interval of 6.5 [5–27] months. Five patients had both a pre- and postoperative MRE in our centre, which made preoperative and postoperative values comparable. Mean MaRIA score decreased from 33.2 [SD: 12.95] to 21.2 [SD: 9.91] by the first radiologist, whereas the second radiologist reported a mean preoperative score of 22.2 [SD: 5.36] vs a postoperative score of 13.8 [SD: 5.40] [p = 0.15]. Reproducibility coefficient was 28.9 and 17.5 for preoperative and postoperative MaRIA values, respectively [Figure 4]. ICC of preoperative measures was 0, and ICC for postoperative measures was 0.55. Another 21 patients underwent only a postoperative MRE; MaRIA score was not assessed due to missing preoperative MRE. However, luminal patency was present in all patients with minor inflammatory changes. Three patients refused any postoperative MRE.
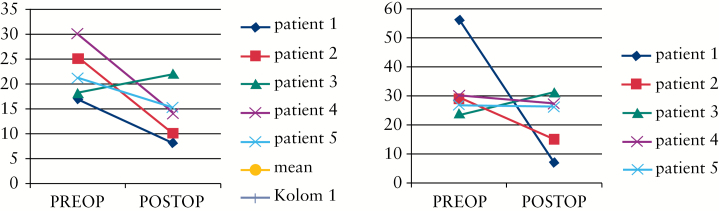
Figure 4.
Two independent radiologists calculated the MaRIA score of both the pre- and postoperative MRE’s in 5 patients. The reproducibility coefficient was 28.9 and 17.5 for pre- and postoprative MaRIA values respectively. MaRIA scores are decreasing, however not significantly (p = 0.15).
3.4. Clinical and surgical recurrence
Clinical recurrence was reported in 11 patients after a median follow-up of 13 [4–28] months. One patient needed a pneumatic dilatation at the inlet of the strictureplasty, and another patient was re-operated for stenotic recurrence at 48 months. None of these two patients had the Sasaki modification. An HM strictureplasty at the inlet of the Michelassi strictureplasty was performed to alleviate the short stricture. A third patient needed a lysis of adhesions for obstructive symptoms, without any signs of Crohn’s recurrence. After a median follow-up of 21 [1–54] months, none of the strictureplasties was resected.
4. Discussion
This pilot study demonstrates the feasibility and safety of the long SSIS over the ileocaecal valve or ileocolic anastomosis for inflammation-induced fibrosis of the [neo-] terminal ileum in CD patients. Despite an acceptable postoperative morbidity rate, prolonged postoperative ileus occured in many patients. Prolonged ileus is suspected to be the consequence of prolonged manipulation of the treated segment while performing the strictureplasty, causing postoperative bowel wall oedema. Two patients presented with a leak in our early experience, which probably reflects the learning curve of this technically demanding procedure. After adapting the technique by omitting any postoperative drainage and performing a thorough selection of the ‘landing place’ of the strictureplasty, no anastomotic leaks were reported in the last 24 patients.With these techniques, rather heavily inflamed segments can be treated, even in the presence of extensive ulceration and bowel wall thickness. The presence of phlegmon, abscess or fistula originating from the treated segment would definitely be a contraindication for performing a stricturplasty, unless the fistula is located at the anti-mesenteric side and can be excised.
Significant mucosal healing after a median interval of 6 months was observed. Although healing was not complete in every patient, important improvement was however clearly visible, even in patients without any medical prophylaxis. Moreover, MRE showed bowel wall healing and absence of any strictures within the treated segment. About 38% of the patients were considered to have a clinical recurrence, at a median follow-up of 13 months. Only one patient showed surgical recurrence after 48 months. A comparable rate of surgical recurrence between strictureplasty and resection has been reported.9
No standardised scores have been elaborated for the assessment of long strictureplasties. Therefore the SES-CD and MaRIA scores were used as surrogates for quantifying mucosal and bowel wall healing in those patients. Although inter-observer variability of the SES-CD score was very satisfying, the inter-observer variability for the MaRIA score seemed unreliable in this series. This is most probably due to the small number of subjects. However, further standardisation of the MaRIA score in long strictureplasties should be undertaken.
Although no data are available about its mechanisms, endoscopic improvement [sometimes mucosal healing] appeared to be the consequence of surgery, since most patients did not receive any Crohn’s medication postoperatively. We speculate that the alleviation of faecal stasis may play a key role in postoperative mucosal healing, modifying the microbial-mucosal interaction. Functional recovery of strictureplasties has never been investigated because of the often difficult accessibility of the treated segment for investigational purposes. Performing a strictureplasty over the ileocaecal valve or ileocolic anastomosis gave the opportunity for flexible endoscopic monitoring, offering a good clinical model for research on the healing process and functional recovery of the treated segment. Further research should therefore focus on the mechanisms of healing and on the assessment of functional recovery, in terms of motility and absorptive function, of the operated segment.
In this study, patients with a diseased bowel length of 20cm on were included arbitrarily. One may wonder whether this is an appropriate threshold; however, it is not possible yet to know the right trade-off for performing a strictureplasty in patients with terminal ileal CD. Further research will indicate which patients would be the best candidates for conservative surgery. Indeed, should clear functional recovery be observed, it would make sense to save a short strictured segment, whereas saving a bowel segment without any functional recovery would be unnecessary. Research on the mechanisms of healing and functional recovery will help surgeons to decide in which cases performing strictureplasty in order to conserve bowel length would be most appropriate.
Some concern has been expressed about the cancer risk at the strictureplasty site. Small bowel cancer risk is indeed increased after long-standing inflammation, but the absolute risk remains extremely low.16 To our knowledge, only four case reports have been published describing the risk of encountering cancer during the strictureplasty formation or the risk of developing cancer at the strictureplasty site.17,18,19,20 It has been recommended to take mucosal biopsies when a mucosal lesion is suspicious for cancer, avoiding routine biopsies.9 Routine follow-up for Crohn’s recurrence should include ileocolonoscopy which would reveal most cases of postoperative cancer within the strictureplasty.
This conservative approach is not new. Since the SSIS was described by Michelassi in 1996, the technique has extended the technical feasibility to preserve small bowel in patients with stenotic Crohn’s disease. 8 In 1997, Poggioli et al. described a modification of this technique to preserve the terminal ileum in primary ileocaecal disease.11 This technique was a Finney-shaped strictureplasty incorporating the diseased terminal ileum segment in the caecum and ascending colon, forming an anisoperistaltic configuration. In 1998, again Poggioli et al. proposed a side-to-side entero-enteric neoileocolic anastomosis [using an isoperistaltic Michelassi type of strictureplasty] in recurrent Crohn’s disease.21 In both techniques and for the first time, it was possible to control the regression of inflammation by colonoscopy. However, the major advantage of using a SSIS over the ileocaecal valve is to avoid incorporation of healthy bowel length in the long strictureplasty. Ultimately, if resection is needed, the colonic resection can be restricted to the caecum. In a Finney-type of reconstruction as proposed by Poggioli, this would result in right or extended right hemicolectomy.
This study has several limitations. First, no control group was included, rendering comparison with intestinal resection impossible. However, the aim of this series is to report short- and medium-term outcome of this modified type strictureplasty. Moreover, no standardised scoring system has been described to assess mucosal and transmural healing in long strictureplasties. However, both the SES-CD and the MaRIA scores were used as surrogate to measure healing. Finally, no standardised postoperative therapy was used in the first five patients. However, even in the patients not having any kind of postoperative medical treatment, significant endoscopic and transmural improvement was observed. Moreover, this study is the first series of patients treated with a modified type Michelassi strictureplasty for primary or secondary extensive [neo-] terminal Crohn’s ileitis.
4.1. Conclusions
In this pilot study, we confirm the safety and feasibility of the SSIS over the ileocaecal valve, and furthermore show that this procedure is associated with extensive mucosal healing of a previously long affected and stenotic segment, hence offering new opportunities for the management of these patients.
Funding
None.
Conflict of Interest
None.
Author Contributions
ADBVO, SV, DVB, MF, GVA, AW, and ADH were responsible for the treatment of all included patients. ADBVO, SV, MF, GVA, AW, and ADH were responsible for designing the study. ADBVO, SV, DVB, JR, and MF were responsible for acquisition of the data. ADB, SV, MF, DVB, and JR were responsible for interpretation of the data. ADBVO was responsible for drafting the manuscript. All authors reviewed and accepted the final version of the manuscript.
References
- 1. Peyrin-Biroulet L, Loftus EV, Jr, Colombel JF, Sandborn WJ. The natural history of adult Crohn’s disease in population-based cohorts. Am J Gastroenterol 2010;105:289–97. [DOI] [PubMed] [Google Scholar]
- 2. Lakatos PL, Golovics PA, David G, et al. Has there been a change in the natural history of Crohn’s disease? Surgical rates and medical management in a population-based inception cohort from Western Hungary between 1977–2009. Am J Gastroenterol 2012;107:579–88. [DOI] [PubMed] [Google Scholar]
- 3. Watanabe T, Sasaki I, Sugita A, et al. Time trend and risk factors for reoperation in Crohn’s disease in Japan. Hepatogastroenterology 2012;59:1081–6. [DOI] [PubMed] [Google Scholar]
- 4. Bernell O, Lapidus A, Hellers G. Risk factors for surgery and postoperative recurrence in Crohn’s disease. Ann Surg 2000;231:38–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Watanabe K, Sasaki I, Fukushima K, et al. Long-term incidence and characteristics of intestinal failure in Crohn’s disease: a multicenter study. J Gastroenterol 2014;49:231–8. [DOI] [PubMed] [Google Scholar]
- 6. Campbell L, Ambe R, Weaver J, Marcus SM, Cagir B. Comparison of conventional and nonconventional strictureplasties in Crohn’s disease: a systematic review and meta-analysis. Dis Colon Rectum 2012;55:714–26. [DOI] [PubMed] [Google Scholar]
- 7. Taschieri AM, Cristaldi M, Elli M, et al. Description of new “bowel-sparing” techniques for long strictures of Crohn’s disease. Am J Surg 1997;173:509–12. [DOI] [PubMed] [Google Scholar]
- 8. Michelassi F. Side-to-side isoperistaltic strictureplasty for multiple Crohn’s strictures. Dis Colon Rectum 1996;39:345–9. [DOI] [PubMed] [Google Scholar]
- 9. Yamamoto T, Fazio VW, Tekkis PP. Safety and efficacy of strictureplasty for Crohn’s disease: a systematic review and meta-analysis. Dis Colon Rectum 2007;50:1968–86. [DOI] [PubMed] [Google Scholar]
- 10. Michelassi F, Taschieri A, Tonelli F, et al. An international, multicenter, prospective, observational study of the side-to-side isoperistaltic strictureplasty in Crohn’s disease. Dis Colon Rectum 2007;50:277–84. [DOI] [PubMed] [Google Scholar]
- 11. Poggioli G, Stocchi L, Laureti S, et al. Conservative surgical management of terminal ileitis: side-to-side enterocolic anastomosis. Dis Colon Rectum 1997;40:234–7; discussion 238–9. [DOI] [PubMed] [Google Scholar]
- 12. Sasaki I, Shibata C, Funayama Y, et al. New reconstructive procedure after intestinal resection for Crohn’s disease: modified side-to-side isoperistaltic anastomosis with double Heineke-Mikulicz procedure. Dis Colon Rectum 2004;47:940–3. [DOI] [PubMed] [Google Scholar]
- 13. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Daperno M, D’Haens G, Van Assche G, et al. Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: the SES-CD. Gastrointest Endosc 2004;60:505–12. [DOI] [PubMed] [Google Scholar]
- 15. Rimola J, Rodriguez S, Garcia-Bosch O, et al. Magnetic resonance for assessment of disease activity and severity in ileocolonic Crohn’s disease. Gut 2009;58:1113–20. [DOI] [PubMed] [Google Scholar]
- 16. Canavan C, Abrams KR, Mayberry J. Meta-analysis: colorectal and small bowel cancer risk in patients with Crohn’s disease. Aliment Pharmacol Ther 2006;23:1097–104. [DOI] [PubMed] [Google Scholar]
- 17. Jaskowiak NT, Michelassi F. Adenocarcinoma at a strictureplasty site in Crohn’s disease: report of a case. Dis Colon Rectum 2001;44:284–7. [DOI] [PubMed] [Google Scholar]
- 18. Marchetti F, Fazio VW, Ozuner G. Adenocarcinoma arising from a strictureplasty site in Crohn’s disease. Report of a case. Dis Colon Rectum 1996;39:1315–21. [DOI] [PubMed] [Google Scholar]
- 19. Menon AM, Mirza AH, Moolla S, Morton DG. Adenocarcinoma of the small bowel arising from a previous strictureplasty for Crohn’s disease: report of a case. Dis Colon Rectum 2007;50:257–9. [DOI] [PubMed] [Google Scholar]
- 20. Partridge SK, Hodin RA. Small bowel adenocarcinoma at a strictureplasty site in a patient with Crohn’s disease: report of a case. Dis Colon Rectum 2004;47:778–81. [DOI] [PubMed] [Google Scholar]
- 21. Poggioli G, Selleri S, Stocchi L, et al. Conservative surgical management of perforating Crohn’s disease: side-to-side enteroenteric neoileocolic anastomosis: report of two cases. Dis Colon Rectum 1998;41:1577–80. [DOI] [PubMed] [Google Scholar]