Abstract
Preliminary studies on HCV-cirrhotics listed for transplant suggest that Sofosbuvir in combination with Ribavirin is very effective in promoting viral clearance and preventing disease recurrence. Unfortunately, the high cost of such treatment (€46 500 per 12 weeks treatment) makes its cost-effectiveness questionable. A semi-Markov model was developed to assess the cost-effectiveness of Sofosbuvir/Ribavirin treatment in cirrhotic patient without HCC (HCV-CIRRH) and with HCC (HCV-HCC) listed for transplant. In the base-case analysis, the incremental cost-effectiveness ratio for 24 weeks of Sofosbuvir/Ribavirin was €44 875 per quality-adjusted life-year gained in HCV-CIRRH and €60 380 in HCV-HCC patients. Both results were above the willingness to pay threshold of €37 000 per quality-adjusted life-year. Our data also show that in order to remain cost-effective (with a 24 weeks treatment), any novel interferon-free treatment endowed with ideal efficacy should cost less than €67 224 or than €95 712 in HCV-cirrhotics with and without HCC, respectively. The results shows that Sofosbuvir/Ribavirin therapy, given to patients listed for transplant, is not cost-effective at current prices despite being very effective, and new, more effective treatments will have little economic margins to remain cost-effective. New interferon-free combinations have the potential to revolutionize the treatment and prognosis of HCV-positive patients listed for transplant; however, without sustainable prices, this revolution is unlikely to happen.
Introduction
Hepatitis C virus (HCV) is the main indication for orthotopic liver transplantation (OLT), ranging from about 10% in northern European countries to almost 50% in southern Europe (1–3). Unfortunately, all patients undergoing OLT with detectable HCV viremia experience HCV reinfection shortly after transplant. Between 20% and 30% of them develop cirrhosis within 5 years (4,5) and 45% decompensate within 1 year from the diagnosis of cirrhosis (4–6). Some patients develop a form of severe cholestatic hepatitis, leading to death in 1–2 years. HCV-posttransplant hepatitis dramatically recurs also after retransplantation and, thus, recurrent HCV is usually not an accepted indication for re-OLT. The current standard of care for recurrent HCV hepatitis is treatment with peg-interferon/ribavirin; unfortunately, less than 50% of the patients can actually be treated and the response rate among treated patients is below 30% (7).
The most relevant risk factors for severe HCV recurrence after transplant include advanced age, and steatosis of the donor, and female gender and diabetes of the recipient. However, the strongest risk factor for recurrence is viremia at transplant. Thus, the ideal approach to prevent HCV recurrence would be to treat all listed HCV-positive patients and to perform the transplant when their HCV viremia becomes undetectable. Unfortunately, because of the contraindications to interferon in these frail patients, treatment with interferon/rivabirin in HCV-patients in the transplant list is rarely feasible, with low efficacy (less than 20%) and with collateral effects that may negatively impact the transplantability of the patient (7).
With the advent of highly effective and tolerated direct-acting antivirals (DAAs), it is now possible to use interferon-free regimens to prevent the recurrence of HCV hepatitis by inducing a negative pretransplant viremia (8–10). Because of the high costs of this treatment, we performed a cost-effectiveness analysis comparing the interferon-free treatment for which preliminary data are available (Sofosbuvir plus Ribavirin–SOF/RBV) to the current standard of care (no antiviral treatment). The simulation was performed in HCV-infected patients in the transplant waiting list (WL), either for cirrhosis and hepatocellular carcinoma within Milano criteria or with cirrhosis without HCC. Further, because new interferon-free treatments based on associations of DAAs will soon be tested also in the transplant setting, we estimated the cost threshold for a hypothetical ideal DAAs treatment combination endowed with further increased effectiveness and tolerability to remain cost-effective in this setting.
Materials and Methods
Overview
We designed and developed a decision-analytic semi-Markov (11) model to simulate the progression of a HCV-infected cirrhotic with or without HCC from the time of listing until death and we used this model to study the cost-effectiveness of SOF/RBV-based interferon-free regimen. The parameters were adjusted to reflect two specific scenarios among patients listed for transplantation: cirrhotic patient without HCC (HCV-CIRRH) and patient with HCC (HCV-HCC). This distinction was made to account that, on the contrary to HCV-HCC patients, in some HCV-CIRRH patients, achievement of SVR would eliminate the need for transplantation. We compared the cost-effectiveness of the current standard of care (no treatment) with the following strategy: SOF/RBV up to a maximum of 24 weeks or until OLT if performed before the 24th week from the initiation of treatment. Patients with all genotypes and MELD below 25 were simulated in the analysis and treated in the same way.
The model estimated the costs related to the treatment with SOF/RBV, the costs associated to each health state, the life-years (LYSs), the quality-adjusted life-years (QALYs) and the incremental cost-effectiveness ratio (ICER) expressed as € per QALY gained. The analysis was run in the cost perspective of the Italian National Healthcare System (NHS), using the 2014 prices expressed in Euro. The time horizon of the simulation was lifetime, with 1 month Markov cycles. Future costs and clinical benefits were discounted at 3% per year. The model was conceptualized and developed following modeling good research practice international guidelines (12,13).
Further, as mentioned previously, because promising new DAA-based interferon-free treatments using combinations of antivirals endowed with higher efficacy and safety will be available soon, we used the model to assess the cost threshold, of a hypothetical new DAAs treatment combination, to be cost-effective assuming 95% probabilities of achieving persistent HCV-RNA clearance before the transplant. We also provide an estimate of the maximum allowable weekly costs as a function of treatment duration.
Model structure
The model simulated the disease progression of two types of patients, HCV-CIRRH and HCV-HCC, listed for liver transplant (Figure 1) and considered the following health states: dropout from WL due to progression of liver failure or HCC progression (“Dropout for worsening”), dropout from WL due to spontaneous improvement of liver function (“Dropout for improvement”), dropout from WL due to improvement SOF/RBV treatment-related (“Dropout for SOF/RBV”), OLT without HCV significant recurrence (“OLT—No or mild recurrence”), OLT with HCV recurrence and development of compensated cirrhosis (“OLT–CC recurrence”) and OLT with HCV recurrence and development of decompensated cirrhosis (“OLT-DC recurrence”).
Figure 1. Diagrammatic representation of the Markov Model.
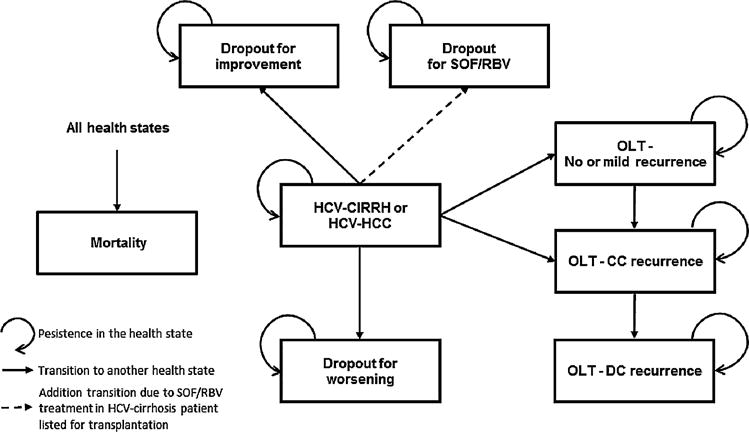
The states of the model are represented by the rectangles. CC, compensated cirrhosis; DC, decompensated cirrhosis; HCV, hepatitis C virus; HCV-CIRRH or HCC-HCV, HCV-infected cirrhosis or HCV-infected hepatocellular carcinoma (depending on the scenario considered for the analysis); OLT, orthotopic liver transplant; SOF/RBV, treatment with Sofosbuvir and Ribavirin.
Treatment strategies
The treatment used in the simulation was 24 weeks therapy of 400 mg daily dose of SOF and 1000 mg daily dose of RBV, based on the study of Curry et al showing that virtually all treated patients were able to achieve a pretransplant HCV-RNA clearance but also that the HCV-RNA clearance had to be maintained for at least 1 month before LT, to end up with very high post OLT SVR (>90%) (8). Treatment was started at the time of listing and had a maximal duration of 24 weeks, unless transplant occurred before the 24th weeks. The limit of 24 weeks was set not to delay transplants too long as the risk of a virological breakthrough increases with time.
Input parameters for the model
An extensive literature review was performed to obtain the reference data upon which to set the model. In the cases in which specific data were not available, some assumptions were made based on the opinion of experts. Table 1 reports a summary of all parameters used in the base case analysis for the two scenarios, including clinical, health-outcomes and costs. Supporting Information reports the methods and assumptions used to estimate the values of the parameters.
Table 1.
Model parameter values and ranges
| Model parameters | Base case value (range) | References |
|---|---|---|
| Model assumptions | ||
| Discount rate cost/outcomes | 0.03 (0–0.06) | (14) |
| Time horizon | Lifetime | – |
| Perspective | Italian NHS | – |
| Cohort characteristic | ||
| Age | 55 (45–65) | (2) |
| SOF/RBV efficacy | ||
| Probability of SVR with SOF/RBV treatment | 0.700 (0.525–0.875) | (8) |
| Pretransplant probabilities (monthly probability) | ||
| Probability of OLT | 0.0492 (0.0369–0.0615) | (2) |
| Dropout probability for liver failure progression | 0.0017 (0.0013–0.0021) | (2,15) |
| Dropout probability for spontaneous liver improvement | 0.0021 (0.0016–0.0026) | (2,15) |
| Dropout probability from WL due to improvement SOF/RBV treatment-related in only cirrhotic patients | 0.1 (0.05–0.15) | Assumption |
| Posttransplant probabilities (monthly probability) | ||
| Probability of HCV-cirrhosis recurrence when HCV-RNA negativity at transplantation | 0.0005 (0.0004–0.0006) | Assumption |
| Probability of HCV-cirrhosis recurrence when HCV-RNA is positive at transplantation | 0.0055 (0.0041–0.0068) | (5) |
| Probability of decompensation from HCV-cirrhosis recurrence | 0.0444 (0.0333–0.0555) | (6) |
| Mortality (monthly probability) | ||
| HCV-infected cirrhotic or HCC listed for transplant | 0.0060 (0.0045–0.0075) | (2) |
| Dropout for liver failure progression | 0.7846 (0.5884–0.9807) | (15) |
| Dropout for spontaneous liver improvement | 0.0014 (0.0011–0.0018) | (15) |
| Dropout from WL due to improvement SOF/RBV treatment-related | 0.0027 (0.0020–0.0034) | (16) |
| OLT in the first 3 months | 0.0170 (0.0127–0.0212) | (3) |
| OLT-No or mild recurrence | 0.0021 (0.0009–0.0037) | Assumption |
| OLT-CC recurrence | 0.0125 (0.0094–0.0156) | (6) |
| OLT-DC recurrence | 0.0716 (0.0537–0.0895) | (6) |
| Utility weights | ||
| HCV-infected cirrhosis listed for transplant | 0.793 (0.714–0.872) | (17) |
| HCV-infected HCC listed for transplant | 0.871 (0.697–0.871) | (17) |
| Dropout for liver failure progression | 0.743 (0.669–0.817) | Assumption |
| Dropout for spontaneous liver improvement | 0.877 (0.789–0.965) | (17) |
| Dropout from WL due to improvement SOF/RBV treatment-related | 0.877 (0.789–0.965) | (17) |
| OLT-No or mild recurrence (in the first 6 months after liver transplant) | 0.852 (0.767–0.937) | (17) |
| OLT-No or mild recurrence (after the first 6 months from liver transplant) | 0.910 (0.819–1.000) | (17) |
| OLT-CC recurrence (in the first 6 months after liver transplant) | 0.852 (0.767–0.937) | (17) |
| OLT-CC recurrence (after the first 6 months from liver transplant) | 0.877 (0.789–0.965) | (17) |
| OLT DC recurrence | 0.793 (0.714–0.872) | (17) |
| Monthly cost (2014 €) | ||
| HCV-infected cirrhotic or HCC listed for transplant | €890 (668–1113) | (18) |
| Dropout from WL for liver failure progression | €1,780 (1335–2225) | Assumption |
| Dropout from WL for spontaneous liver improvement | €126 (95–158) | (20) |
| Dropout from WL due to improvement SOF/RBV treatment-related | €126 (95–158) | (20) |
| OLT (first month) | €83,530 (62648–104413) | (19) |
| OLT-No or mild recurrence (after first month from liver transplant) | €1,474 (1105–1.842) | (20–22) |
| OLT-CC recurrence (after first month from liver transplant) | €1,532 (1226–1915) | (20–22) |
| OLT-DC recurrence | €3984 (2988–4980) | (20–22) |
| Treatment costs (2014 €) | ||
| Sofosbuvir 400mg | €537 (375–696) | (23) |
| Ribavirin 1100 mg | €17 | (24) |
CC, compensated cirrhosis; DC, decompensated cirrhosis; HCV, hepatitis C virus; HCC, hepatocellular carcinoma; OLT, orthotopic liver transplant; SOF/RBV, treatment with Sofosbuvir and Ribavirin; WL, waiting list.
Analysis
The model estimated costs, LYs and QALYs under the two treatment strategies for the two group of patient (HCV-CIRRH or HCV-HCC) listed for transplant. Results are presented as incremental cost-effectiveness ratios (ICERs) per QALY gained (which are calculated as the difference in the expected cost produced by the two interventions divided by the difference in the expected QALYs produced by the two interventions). To be considered cost-effective, the ICER should be under the willingness to pay (WTP) threshold of 37 000 € per QALY gained, which is considered acceptable by leading regulatory agencies such as NICE-UK, AHRQ–USA and CADTH-Canada. To test the robustness of the model’s assumption and specific parameters, we performed a one-way sensitivity analysis by changing parameters using a plausible range or the 95% confidence interval (Table 1). Because of their uncertainty and high impact on the results, we performed a further specific sensitivity analysis to understand the effect of the duration of SOF/RBV, cost of SOF and probability of dropout from the list due to clinical improvement on the ICER.
A probabilistic sensitivity analysis was also performed to address the uncertainty of the model parameters. Statistical distributions were assigned to the model parameters to evaluate the uncertainty around the point estimates. Uncertainty in all model parameters was assessed using a Monte Carlo simulation, drawing parameter values at random 1000 times from the appropriate corresponding distributions. The results from the simulations were used to generate cost-effectiveness acceptability curve (CEAC) to explore the probability that SOF/RBV treatment would be economically attractive at any given cost-effectiveness threshold. The CEAC indicated the probability that the SOF/RBV treatment is cost-effective compared to the standard of care, given the values and uncertainty of the parameters used in the model and for different values of the acceptable WTP.
Further, we performed another analysis to estimate the maximum weekly cost of a hypothetical new DAAs combination treatment to be cost-effectiveness at a WTP of €37 000. The weekly price was estimated in function of the treatment duration. We hypothesized this new treatment as outperforming SOF/RBV and considered the possible scenario with 95% probability of persistent HCV-RNA clearance. The analyses were based on the simultaneous variation of both the weekly treatment cost and the treatment duration for HCV-CIRRH patients and for HCV-HCC patients needed to remain at the WPT threshold.
Results
Results shown in Table 2 indicate that treatment with SOF/RBV in patients with HCV-cirrhosis and HCV-HCC listed for transplant is superior to the standard of care in terms of QALYs and LYs gained, but more expensive. In the group of HCV-cirrhosis patients listed for transplant, SOF/RBV treatment showed an incremental life-expectancy of 3.67 years/patient and an increment in QALYs of 2.07/patient. The life time total cost per patient was €292 981 in the SOF/RBV scenario with an incremental life time total cost of €92 983 when compared to untreated patients. The ICERs for SOF/RBV treatment strategy relative to the standard of care was €44 875 per QALY gained, which is above the WTP threshold of €37 000 per QALY gained.
Table 2.
Base case results: lifetime costs and health benefits of treatment strategies in cirrhosis and in HCC scenario
| Treatment strategy | LYs | Discounted QALYs | Discounted costs (€) | Incremental LYs | Incremental QALYs | Incremental cost (€) | ICER (€/QALY) |
|---|---|---|---|---|---|---|---|
| HCV-cirrhosis listed for liver transplant | |||||||
| No antiviral treatment | 9.76 | 6.88 | €199 998 | – | – | – | – |
| SOF/RBV | 13.43 | 8.96 | €292 981 | 3.67 | 2.07 | €92 983 | € 44 875 |
| HCV-HCC listed for liver transplant | |||||||
| No antiviral treatment | 9.76 | 6.99 | €199 998 | – | – | – | – |
| SOF/RBV | 13.00 | 8.83 | €311 200 | 3.23 | 1.84 | €111 202 | €60 380 |
HCC-HCC, hepatocellular carcinoma; ICER, incremental cost-effectiveness ratio; LYs, life years; QALYs, quality-adjusted life-years; SOF/RBV, treatment with Sofosbuvir and Ribavirin.
In the HCV-HCC patient listed for transplant, SOF/RBV-treated patient incremental life-expectancy was 3.23 years per patient with an increment in QALYs of 1.84 per patient. The life time total cost per patient was €311 200 in the SOF/RBV treatment scenario with an incremental cost of €111 202 when compared to untreated patients. The ICERs for SOF/RBV treatment strategy relative to the standard of care (€60 380 per QALY gained) was well above the WTP threshold.
Sensitivity analysis
Results from the one-way sensitivity analysis reported in Figure S1 shows the impact of changing the value of several parameters on the ICER. In one-way sensitivity analyses, we evaluated the effect of increasing or decreasing each individual input variable, while keeping the other input variables unchanged. The results showed that in both scenarios (Figure S1A and B), the ICERs were more sensitive to changes in the following parameters: annual outcome and cost discount rate, the SVR probability after SOF/RBV therapy, the age of the subject at transplantation, the cost of SOF, the probability of HCV-cirrhosis recurrence, the cost and utility associated with “OLT-No or mild recurrence.” Further, the dropout probability from WL due to clinical improvement related to SOF/RBV treatment showed a high impact on the results in the HCV-cirrhosis scenario. Because the value of this last parameter was based on assumption, we performed a more extensive one-way sensitivity analysis changing the dropout probability from WL due to clinical improvement from 0% to 30%; the results are showed in Figure S2. The results reported an ICER below the WTP when the drop out probability was higher than 16%.
Another one-way sensitivity analysis was performed by varying the values of the duration of SOF/RBV treatment, as shown in Figure 2. It is evident that the ICER was under the WTP threshold (i.e. treatment was cost-effective) only when the duration of the therapy was lower than 19 weeks in the HCV-CIRRH scenario (Figure 2A). Differently, in the HCV-HCC scenario, the ICER was higher than €37 000 even when the duration of the therapy was limited to 12 weeks (Figure 2B).
Figure 2. ICER (€ per QALY gained) values changing the SOF/RBV treatment duration strategies in the HCV-CIRRH (A) and HCV-HCC scenario (B).
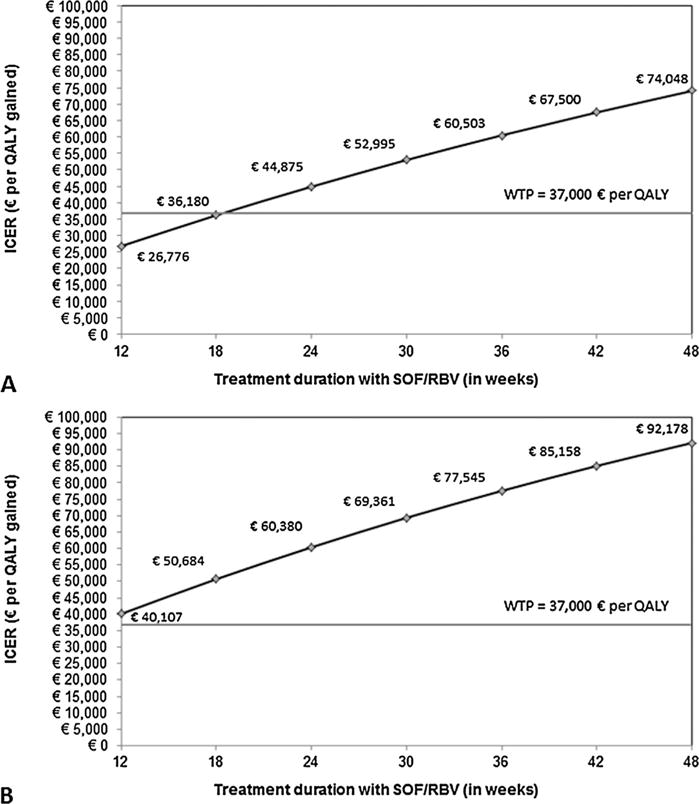
HCV, hepatitis C virus; HCV-CIRRH, HCV cirrhotic patient listed for liver transplantation; HCV-HCC, HCV patient with hepatocellular carcinoma listed for liver transplantation; ICER, incremental cost-effectiveness ratio; QALY, quality-adjusted life-year; SOF/RBV, sofosbuvir in combination with ribavirin treatment; WTP, willingness to pay.
A final one-way sensitivity analysis was performed changing the 12 weeks cost of SOF from €30 000 to €60 000. The ICER was under the WTP threshold when the cost was €36 000 or lower only in the HCV-CIRRH scenario (Figure S3A). In HCV-HCC scenario, the ICER was higher than €37 000 also when the SOF cost was set at €30 000 per 12 weeks of treatment (Figure S3B).
The WTP threshold is not fixed parameter, but may vary according to several socio-economic conditions and the health care system. Thus, we used the results of the probabilistic sensitivity analysis to generate a cost-effectiveness acceptability curve (CEACs) (Figure 3). The CEAC clearly shows that in listed patients with HCV-Cirrhosis, SOF/RBV has only a probability of 16% to be cost-effective if WTP per QALY is set at €37 000 (Figure 3A). In listed HCV-HCC patients, the probability to be cost-effective decreases to almost 2% (Figure 3B).
Figure 3. Cost-effectiveness acceptability curve (ICER reported as € per QALY gained) in the HCV-CIRRH (A) and HCV-HCC scenario (B).
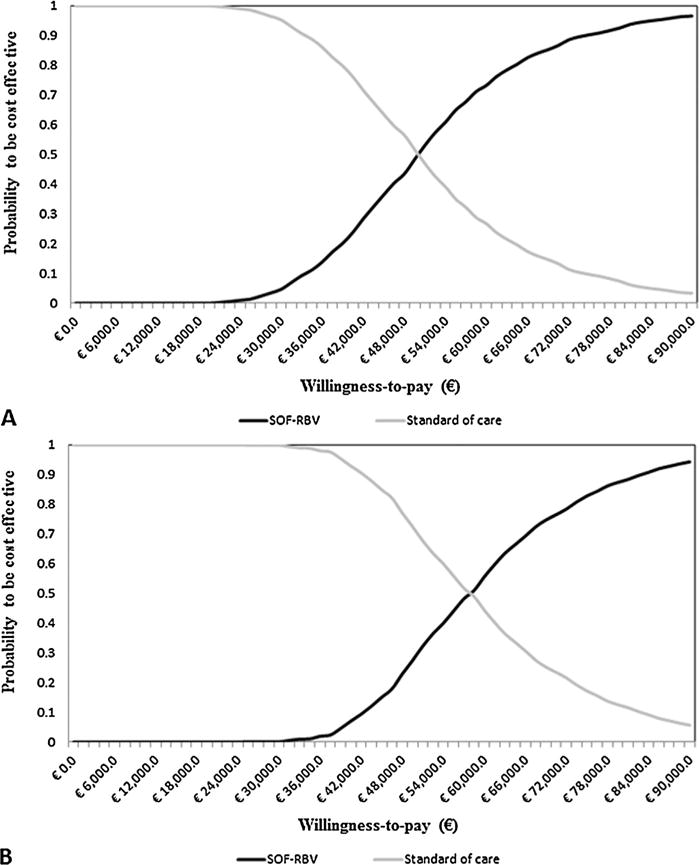
HCV, hepatitis C virus; HCV-CIRRH, HCV cirrhotic patient listed for liver transplantation; HCV-HCC, HCV patient with hepatocellular carcinoma listed for liver transplantation; ICER, incremental cost-effectiveness ratio; QALY, quality-adjusted life-year; SOF/RBV, sofosbuvir in combination with ribavirin treatment.
Cost threshold for a hypothetical ideal cost-effective DAA treatment
Our data indicate that because of the cost of the drug, the high clinical effectiveness of SOF/RBV does not translate into a substantial cost-effectiveness, even in the most favorable scenario. Some of the assumptions of the model might prove optimistic when SOF/RBV will be tested on the field. Specifically, we assumed that SOF/RBV is capable of inducing a persistent HCV-RNA clearance in 90% of treated patients and that viral clearance will persist until liver transplantation. This may not be always the case as the interval between end of treatment and the availability of a liver transplantation widens. Hopefully, new interferon-free combinations will be available in the near future which will reduce to a minimum the risk of relapse while waiting for a transplant.
Thus, we determined the cost threshold of an ideal DAA to remain cost effective at WTP threshold of €37 000/QALY. This analysis shows that even assuming an extremely high efficacy and tolerability of new regimens, the total cost of any new drug or drug combination should be lower than €95 712 (€3988 per week) in the HCV-cirrhotic patients and €67 224 (€2801 per week) in the HCV-HCC group, for 24 weeks treatment.
Future DAAs combinations will likely allow shorter treatment duration; therefore, the maximum allowable cost per week of any new regimen will depend on its duration. Thus, we estimated the maximum weekly cost of hypothetical new DAAs able to induce a 95% of HCV-RNA clearance in listed patients in order to remain cost-effectiveness at a WTP threshold of € 37 000, as a function of treatment duration (Figure 4). These plots show the changes in both the weekly treatment cost and the treatment duration. For treatment durations of 12 and 20 weeks, respectively, DAAs treatment is cost-effective in HCV-cirrhosis patients when the weekly cost is lower than €7387 and €4670 (Figure 4A). In HCV-HCC patients, DAAs treatment is cost-effective in HCV-HCC patients when the weekly cost lower than €5179 and €3275 (Figure 4B).
Figure 4. Analysis at the simultaneous variation of both the weekly treatment cost and the treatment duration related to HCV-CIRRH (A) and HCV-HCC (B) scenario (WTP = €37 000 per QALY and HCV-RNA clearance = 95%).
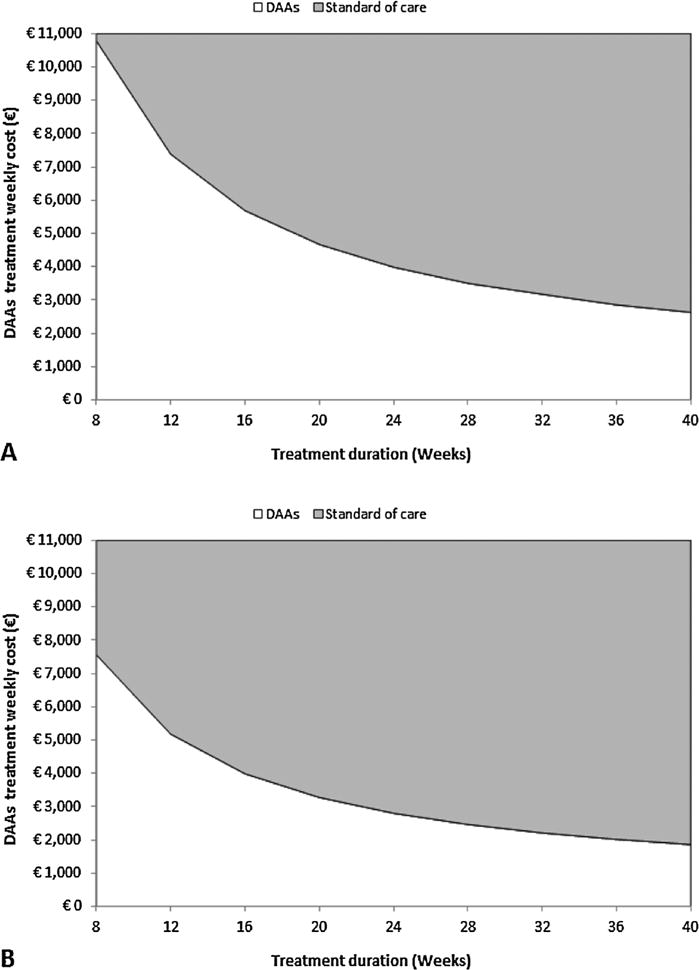
If the intersection of the two variables falls on the white side of the graph, DAAs treatment is the cost-effective strategy; conversely, if the intersection falls on the gray side, standard of care (no antiviral treatment) is the cost-effective strategy. DAAs, direct-acting antivirals; HCV, hepatitis C virus; HCV-CIRRH, HCV cirrhotic patient listed for liver transplantation; HCV-HCC, HCV patient with hepatocellular carcinoma listed for liver transplantation; HCV-RNA hepatitis C virus ribonucleic acid; QALY, quality-adjusted life-year; WTP, willingness to pay.
Discussion
The increasing demand for transplantation in HCV-related end-stage liver disease, combined with the negative impact of recurrent HCV on patient and graft survival, represents one of the major unmet medical need in hepatology. In countries with a high prevalence of HCV infection, such as Italy, the number of HCV-positive patients on the liver transplant lists approximates 50% of the candidates (3). Prevention of graft infection by HCV through universal pretransplant viral treatment, with peg-interferon/rivabirin has generated disappointing results. The availability of interferon-free regimens with direct acting antivirals (Sofosbuvir is the first such compounds in the market at this time) is a major step forward in the treatment of HCV infection because of the efficacy and low collateral effects. Unfortunately, the cost-effectiveness of these treatments is under question because of the high cost.
The results of the cost-effectiveness analysis of SOF/RBV treatment in patients with HCV-related liver disease listed for liver transplant clearly indicate that SOF/RBV treatment initiated when the patient on the WL has a high efficacy with an incremental life-expectancy of 3.67 years per patient, an increment in QALYs of 2.07, in the HCV-cirrhosis scenario, and an incremental life-expectancy of 3.23 years per patient, and increment in QALYs of 1.82, in the HCV-HCC scenario. Unfortunately, the ICERs obtained from our simulation, €44 875 per QALY gained in HCV-cirrhosis and €60 380 in HCV-HCC, were both over the WTP threshold of €37 000.
Cost-effectiveness is not achieved despite the high potency and tolerability of SOF/RBV therapy. In the model, we assumed that SOF/RBV was able to induce HCV-RNA clearance in 90% of treated patients (8,9), and that 70% of the patients were able to maintain the virological response posttransplant. Experience with SOF/RBV in liver transplant candidates is still limited, and, thus, these estimates may turn-out to be optimistic. For example, a sizable percentage of cirrhotic patient, who do not receive a transplant within 6 months from the beginning of the treatment, may experience an HCV relapse, and not be protected from recurrence. These conditions would in theory result in a higher ICER/QALY and further decrease SOF/RBV cost-effectiveness. Figures S1, S2 and S3 show the one-way sensitivity analyses performed and how several other variables may influence the ICER, increasing the variability of the cost-effectiveness.
One of the most important variables is the duration of treatment. At the current costs, SOF/RBV therapy became cost-effective only when the duration of treatment remained below 19 weeks in HCV-cirrhotics.
Having the limits of SOF/RBV in mind and considering that new associations of DAAs with higher efficacy and a shorter duration of treatment will be available soon, we then determined the maximum cost allowable for a hypothetical new DAAs treatment combination to be cost-effective according to the length of duration of treatment. To simulate the best possible scenario, we considered a 95% efficacy both for sustained viral eradication pretransplant, and for the chance to remain HCV-free after transplant. Even the most effective drug or combination of drugs, when administered for 24 weeks was cost-effective only if the total cost was below €95 712 (€3988 per week) for patients with HCV-cirrhosis and €67 224 (€2801 per week) for those with HCV-HCC.
Our study shows that at the current costs, SOF/RBV for 24 weeks is not cost-effective, and may become cost-effective only if the duration of the treatment is significantly shortened, but unfortunately, data from clinical studies are not sufficient to reliably model a 12-week treatment. Furthermore, the cost-effectiveness may be considerably changed by a number of other variables, as shown in the sensitivity analysis. Our study also provides important information as to the maximal cost allowable for any forthcoming new DAA or combination of DAA with ideal efficacy to remain cost-effective. It is clear that at the current cost of SOF/RBV, even the most innovative drug or combination of drugs will have little margin to remain cost-effective.
It should also be clear that to be cost-effective does not mean to be sustainable. Sustainability of these treatments is a major issue and will need to be addressed by allocating treatment only to those cases with the higher risk of severe recurrence or to established severe posttransplant recurrence (thereby limiting the cost-effectiveness of the treatment) or by negotiating more sustainable prices or payment systems in order to give the opportunity to treat more patients. Furthermore, the willingness to pay threshold, in addition to being specific to a given country, should also change in relation to the prevalence of treatable cases and the budget that can be allocated to that treatment. In the United States, for example, where the price of 24 weeks of SOF/RBV is $169 038 (€132 286) (25), the ICER for SOF/RBV treatment would be even higher than what reported in our simulation. Further, in the United States, more than half of all adult liver transplantations are usually performed on HCV-positive recipients (26,27); this means that approximately 3200 patients listed for OLT would be eligible for treatment each year at a cost of around $170 000 (€133 090) indicating that the immediate burden in the United States would be around $544.0 M (€425.9 M) per year.
On the contrary, given the uncertainties of the treatment duration and the timing for transplant, payment should be on a per-treatment basis (fixed price, rather than per week). In Italy, where a similar scenario is being explored, the price of SOF/RBV for 48 weeks of treatment in a patient listed for transplant would be €45 000 (SOF) plus €5700 (RBV) and the ICER would be €28 230 in the HCV-CIRRH patients (Table S1), below the WTP threshold of €37 000. While in the HCV-HCC patients, the ICER would be €41 709 (Table S1) slightly above the WTP threshold. In Italy, approximately 500 patients listed for OLT would be eligible for treatment each year which means that under these pricing conditions, the immediate burden for the Italian health care system would be around €25.35 M per year, increasing the yearly expenses for liver transplant by about 25%.
In conclusion, new interferon-free DAAs combinations have the potential to revolutionize the treatment and prognosis of HCV-positive patients listed for transplant; however, without a sustainable price, this revolution is likely to remain only potential. More favorable pricing policies particularly for those patients requiring longer treatment, as liver transplant candidates, would make the treatment cost-effective and sustainable.
Supplementary Material
Figure S1: One way sensitivity analysis - Tornado diagram. SOF/RBV compared to No antiviral treatment in HCV-CIRRH (A) and in HCV-HCC scenario (B). Thirteen parameters that more influenced the ICER in the two protocol treatment are reported. The horizontal axis represents the ICER as €/QALY. The width of the bars illustrates the range ICER. Upper and lower limits of values evaluated in sensitivity analysis are reported in Table 1 of the manuscript. The bars are ordered from the greatest width at the top to the least width at the bottom. The vertical dashed line represents the base case.
Figure S2: ICER (€ per QALY gained) values changing the dropout probability from WL due to improvement SOF/RBV treatment-related in the HCV-CIRRH.
Figure S3: ICER (€ per QALY gained) values changing the SOF price in the HCV-CIRRH (A) and HCV-HCC scenario (B).
Table S1: Pay-back after 12 weeks of treatment scenario: lifetime Costs and Health Benefits of Treatment Strategies in cirrhosis and in HCC scenario.
Acknowledgments
M.S. gratefully acknowledges the support of NIH grant DK34989: Silvio O. Conte Digestive Diseases Research Core Centers (clinical core).
Abbreviations
- CC
compensated cirrhosis
- CEAC
cost-effectiveness acceptability curve
- DAAs
direct-acting antivirals
- DC
decompensated cirrhosis
- HCC
hepatocellular carcinoma
- HCV
hepatitis C virus
- HCV-CIRRH
HCV cirrhotic patient listed for liver transplantation
- HCV-HCC
HCV patient with hepatocellular carcinoma listed for liver transplantation
- ICER
incremental cost-effectiveness ratio
- LYs
life years
- NHS
National Health System
- OLT
orthotopic liver transplantation
- QALYs
quality-adjusted life-years
- SOF/RBV
sofosbuvir in combination with ribavirin treatment
- WL
waiting list
- WTP
willingness to pay
Footnotes
Disclosure
The authors of this manuscript have conflicts of interest to disclose by the American Journal of Transplantation. M.S. has received grant and nonfinancial support from Gilead, advisory boards and speaking honoraria from Jansen, grants and speaking honoraria from Bayer, other from MSD, outside the submitted work. L.S.B. has received grant from Gilead, outside the submitted work. L.G.M. has received grants from MSD, grants from Jansen, outside the submitted work and personal fees from Bayer in area other than hepatology. P.A.C. has received personal fee from BMS, outside the submitted work. The other authors declare no competing interests.
Supporting Information
Additional Supporting Information may be found in the online version of this article.
References
- 1.Adam R, Karam V, Delvart V, et al. Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR) J Hepatol. 2012;57:675–688. doi: 10.1016/j.jhep.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 2.Italian National Transplant Center—Sistema Informativo Trapianto. [cited 2014 January 15]. Available from: https://trapianti.sanita.it/statistiche/home.asp.
- 3.Angelico M, Cillo U, Fagiuoli S, et al. Liver Match, a prospective observational cohort study on liver transplantation in Italy: Study design and current practice of donor-recipient matching. Dig Liver Dis. 2011;43:155–164. doi: 10.1016/j.dld.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 4.Crespo G, Mariño Z, Navasa M, Forns X. Viral hepatitis in liver transplantation. Gastroenterology. 2012;142:1373–1383. doi: 10.1053/j.gastro.2012.02.011. [DOI] [PubMed] [Google Scholar]
- 5.Prieto M, Berenguer M, Rayón JM, et al. High incidence of allograft cirrhosis in hepatitis C virus genotype 1b infection following transplantation: Relationship with rejection episodes. Hepatology. 1999;29:250–256. doi: 10.1002/hep.510290122. [DOI] [PubMed] [Google Scholar]
- 6.Berenguer M, Prieto M, Rayón JM, et al. Natural history of clinically compensated hepatitis C virus-related graft cirrhosis after liver transplantation. Hepatology. 2000;32:852–858. doi: 10.1053/jhep.2000.17924. [DOI] [PubMed] [Google Scholar]
- 7.Roche B, Samuel D. Hepatitis C virus treatment pre- and post-liver transplantation. Liver Int. 2012;32:120–128. doi: 10.1111/j.1478-3231.2011.02714.x. [DOI] [PubMed] [Google Scholar]
- 8.Curry MP, Forns X, Chung RT, et al. Sofosbuvir and ribavirin prevent recurrence of HCV infection after liver transplantation: An open-label study. Gastroenterology. 2015;148:100–107. doi: 10.1053/j.gastro.2014.09.023. [DOI] [PubMed] [Google Scholar]
- 9.Afdhal N, Everson G, Calleja JL, et al. Sofosbuvir and ribavirin for the treatment of chronic HCV with cirrhosis and portal hypertension with and without decompensation: Early virologic response and safety. J Hepatol. 2014;60:S28. [Google Scholar]
- 10.Gane EJ, Agarwal K. Directly acting antivirals (DAAs) for the treatment of chronic hepatitis C virus infection in liver transplant patients: “A flood of opportunity”. Am J Transplant. 2014;14:994–1002. doi: 10.1111/ajt.12714. [DOI] [PubMed] [Google Scholar]
- 11.Briggs A, Sculpher M. Claxton K Decision modelling for health economic evaluation. Oxford: Oxford University Press; 2006. [Google Scholar]
- 12.Roberts M, Russell LB, Paltiel AD, Chambers M, McEwan P, Krahn M. On Behalf of the ISPOR-SMDM Modeling Good Research Practices Task Force. Conceptualizing a model: A report of the ISPOR-SMDM Modeling Good Research Practices Task Force-2. Value Health. 2012;15:804–811. doi: 10.1016/j.jval.2012.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siebert U, Alagoz O, Bayoumi AM, et al. On Behalf of the ISPOR-SMDM Modeling Good Research Practices Task Force. State-transition modeling: A report of the ISPOR-SMDM Modeling Good Research Practices Task Force-3. Value Health. 2012;15:812–820. doi: 10.1016/j.jval.2012.06.014. [DOI] [PubMed] [Google Scholar]
- 14.Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 15.Cadahá V, González-Diéguez ML, Alonso P, et al. Exclusions and deaths on the liver transplant waiting list. Transplant Proc. 2010;42:622–624. doi: 10.1016/j.transproceed.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 16.Alazawi W, Cunningham M, Dearden J, Foster GR. Systematic review: Outcome of compensated cirrhosis due to chronic hepatitis C infection. Aliment Pharmacol Ther. 2010;32:344–355. doi: 10.1111/j.1365-2036.2010.04370.x. [DOI] [PubMed] [Google Scholar]
- 17.Cortesi PA, Scalone L, Ciampichini R, et al. Health related quality of life in the major liver conditions. Hepatology. 2013;58:1210A. [Google Scholar]
- 18.Ciampichini R, Fagiuoli S, Scalone L, et al. Societal burden in Hepatits C patients: The COME study results. Value Health. 2012;15:A138. [Google Scholar]
- 19.Conferenza delle regioni e delle province autonome 13/41/cr05a/c7—Accordo interregionale per la compensazione della mobilità sanitaria. [cited 2014 May 4]. Available from: http://www.sanita.ilsole24ore.com/pdf2010/Sanita2/_Oggetti_Correlati/Documenti/Regioni-e-Aziende/TUC_2012.pdf?uuid=5c5fbc90-a757-11e2-82ba-89cca4ad5083.
- 20.Logge C, Vettorazzi E, Fischer L, Nashan B, Sterneck M. Cost-effectiveness analysis of antiviral treatment in liver transplant recipients with HCV infection. Transpl Int. 2013;26:527–534. doi: 10.1111/tri.12085. [DOI] [PubMed] [Google Scholar]
- 21.Cortesi PA, Ciaccio A, Rota M, et al. Management of treatment-naïve chronic hepatitis C genotype 1 patients: A cost-effectiveness analysis of treatment options. J Viral Hepat. 2015;22:175–183. doi: 10.1111/jvh.12278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siebert U, Sroczynski G, Aidelsburger P, et al. Clinical effectiveness and cost effectiveness of tailoring chronic hepatitis C treatment with peginterferon alpha-2b plus ribavirin to HCV genotype and early viral response: A decision analysis based on German guidelines. Pharmacoeconomics. 2009;27:341–354. doi: 10.2165/00019053-200927040-00006. [DOI] [PubMed] [Google Scholar]
- 23.Gazzetta Ufficiale Della Repubblica Italiana. [cited 2014 December 17]. Available from: http://www.gazzettaufficiale.it/atto/serie_generale/caricaDettaglioAtto/originario?atto.dataPubblicazioneGazzetta=2014-12-05&atto.codiceRedazionale=14A09382&elenco30giorni=false.
- 24.Italian Medicines Agency (AIFA) [cited 2014 May 4]. Available at: http://www.agenziafarmaco.gov.it.
- 25.Hagan LM, Sulkowski MS, Schinazi RF. Cost analysis of sofosbuvir/ribavirin versus sofosbuvir/simeprevir for genotype 1 hepatitis C virus in interferon-ineligible/intolerant individuals. Hepatology. 2014;60:37–45. doi: 10.1002/hep.27151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Key challenges in HCV management in the transplant setting. [cited 2014 October 20]. Available from: http://www.clinicaloptions.com/Hepatitis/Treatment%20Updates/HCV%20Transplant/CCO%20Slidesets/Key_Challenges_%20for_Transplant.aspx.
- 27.U.S. Department of Health & Human Services. Organ procurement and transplantation network. OPTN/SRTR 2012 Annual Data Report: Liver. [cited 2014 October 20]. Available from: http://optn.transplant.hrsa.gov/converge/data/annualReport.asp.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1: One way sensitivity analysis - Tornado diagram. SOF/RBV compared to No antiviral treatment in HCV-CIRRH (A) and in HCV-HCC scenario (B). Thirteen parameters that more influenced the ICER in the two protocol treatment are reported. The horizontal axis represents the ICER as €/QALY. The width of the bars illustrates the range ICER. Upper and lower limits of values evaluated in sensitivity analysis are reported in Table 1 of the manuscript. The bars are ordered from the greatest width at the top to the least width at the bottom. The vertical dashed line represents the base case.
Figure S2: ICER (€ per QALY gained) values changing the dropout probability from WL due to improvement SOF/RBV treatment-related in the HCV-CIRRH.
Figure S3: ICER (€ per QALY gained) values changing the SOF price in the HCV-CIRRH (A) and HCV-HCC scenario (B).
Table S1: Pay-back after 12 weeks of treatment scenario: lifetime Costs and Health Benefits of Treatment Strategies in cirrhosis and in HCC scenario.


