Abstract
Massively parallel sequencing has permitted an unprecedented examination of the cancer exome, leading to predictions that all genes important to cancer will soon be identified by genetic analysis of tumours. To examine this potential, here we evaluate the ability of state-of-the-art sequence analysis methods to specifically recover known cancer genes. While some cancer genes are identified by analysis of recurrence, spatial clustering or predicted impact of somatic mutations, many remain undetected due to lack of power to discriminate driver mutations from the background mutational load (13–60% recall of cancer genes impacted by somatic single-nucleotide variants, depending on the method). Cancer genes not detected by mutation recurrence also tend to be missed by all types of exome analysis. Nonetheless, these genes are implicated by other experiments such as functional genetic screens and expression profiling. These challenges are only partially addressed by increasing sample size and will likely hold even as greater numbers of tumours are analysed.
 Next generation sequencing has been pivotal in identifying somatic mutations in cancer samples. In this study, the authors analyse whole exome sequencing data using a variety of bioinformatic methods to identify mutations in known cancer genes and find that many cancer genes are not detected by these methods.
Next generation sequencing has been pivotal in identifying somatic mutations in cancer samples. In this study, the authors analyse whole exome sequencing data using a variety of bioinformatic methods to identify mutations in known cancer genes and find that many cancer genes are not detected by these methods.
Extensive collaborative projects1,2,3,4,5,6,7 have released thousands of tumour exomes into the public domain, charting the complete sequences of the protein-coding regions8. Analysis of these data has revealed that each adult tumour carries ∼20–300 genes with somatic alterations to single nucleotides (single-nucleotide variants, SNVs)9 or short (∼2–10) base insertions and deletions. In addition, tumours are perturbed by gene copy number variants (CNVs) and translocations of sequence, including aberrant fusion of two or more distinct genes within the same open reading frame (gene fusions)10,11. Given this landscape, an imminent challenge is to determine how best to interpret cancer genomic data, including which of the identified alterations promote the initiation or progression of cancer10,12.
Towards this end, an increasing number of bioinformatic approaches are being developed with the goal of distinguishing true cancer ‘driver genes' from genes randomly perturbed by ‘passenger' mutations9,13,14,15,16,17. The main methodology has been to look for recurrent mutations within a cohort, based on how often a gene is altered relative to an expected background rate9,13,14. Other prominent methods score the predicted impact of a mutation on protein structure or function15,16 or recognize spatial clustering of mutations within particular domains or residues15,17. Indeed, many of the best characterized cancer genes, such as TP53, PTEN and PIK3CA, are readily identified by any of these approaches15. Such success at recovering known cancer genes through exome analysis has led to recent estimates that we will soon obtain a comprehensive catalogue of all cancer genes if enough tumours are analysed, for example, 250,000 tumours covering 50 cancer types18.
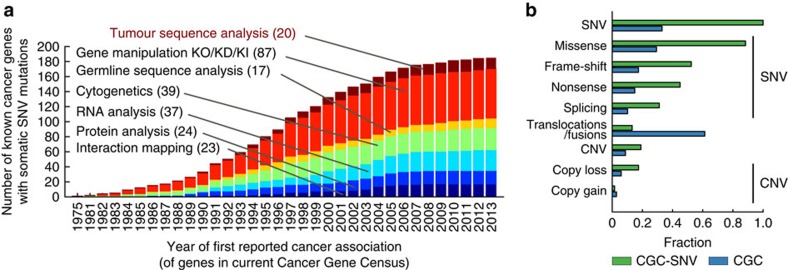
Accurate identification of all cancer genes is an ambitious task, however, and one can conceive of reasons why recovering all cancer genes might be difficult using the prevailing methods. First, despite many decades of study there remains no real consensus as to what exactly defines a ‘cancer gene'. Most broadly, a cancer gene has been defined as any gene harbouring alterations that ‘confer growth advantage on the cancer cell and are positively selected in the microenvironment of the tissue in which the cancer arises'19. Given this definition, it is unclear whether all such genes could be identified from analysis of somatic alterations in the exome, as alterations can also be selected from intergenic sequences20, the germline21 or, potentially, purely epigenetic causes22. To point, most known cancer genes (∼85%) were first identified through principles and experimental techniques other than somatic exome sequencing (Fig. 1a,b). Examples include screens for human or viral DNA capable of transforming cells (for example, RAS)23, systematic mutagenesis (for example, PLEG1)24, differential expression or phosphorylation (for example, TP53)25 or linkage of inherited germline variants to increased risk in familial cancers (for example, BRCA1)26. On the other hand, it is quite possible that cancer genes affected by one type of alteration also tend to be affected by other types, allowing them to be identified by multiple modes of analysis. For example, although TP53 was first identified based on differential expression, it was soon thereafter found to be recurrently mutated in the majority of cancers25,27.
Figure 1. Original experimental techniques used to identify currently known cancer genes.
(a) Shown is the cumulative number of cancer genes known to be perturbed by somatic single-nucleotide variations, as recorded in the COSMIC CGC, according to the year of first cancer-related publication indexed in PubMed. Each bar is coloured by the experimental technique categories used by these first publications. In parenthesis is the number of genes associated with each experimental category as of 2013. (b) Proportion of the different types of somatic alteration included in the CGC. In blue are the proportions for all somatically altered genes; in green are the same proportions for genes also known to have single-nucleotide alterations.
Second, the key task is not just to identify any genetic variant, but to classify variants that are functional from random passengers. Success at this classification task depends on the ability to cleanly discriminate cancer from non-cancer genes using some property, for example, mutation recurrence in a cohort. Previously15,28, the focus has been to evaluate the proportion of genes identified in tumour sequence analysis that are likely to be cancer genes (precision) rather than the proportion of all cancer genes that are identified by a given method (recall). Achieving high recall may be difficult if some cancer genes are rarely altered, in which case an absence of statistically significant recurrence for a genetic alteration is not evidence that it lacks a functional effect.
Here we evaluate current tumour sequence analysis methods by their precision and recall for detecting known cancer genes. We find that these methods tend towards high precision but low recall, meaning that many true cancer genes are being missed by all methods. Estimates of statistical power suggest that this challenge is not likely to be addressed purely by increasing the number of tumour exomes analysed.
Results
Tumour exome analysis methods
We considered five main methods, all of which have been explicitly designed with the goal of identifying cancer genes and were recently used in publications of The Cancer Genome Atlas (see http://www.nature.com/tcga/): MutSig Suite9, OncodriveFM29, OncodriveClust30, ActiveDriver17 and MuSIC13. Each of these approaches has been previously applied to analyse tumour exome data for 12 or more separate tissues and for a pooled ‘pancancer' cohort, which combines all tissues into a single analysis (MAIN-METHODS, Table 1). The MutSig Suite tests each gene for enrichment of somatic SNVs versus a gene-specific background model. Enrichment is measured in terms of three properties—SNV recurrence, impact on protein structure or function and spatial clustering—yielding a single P value of significance integrating the three measures. OncodriveFM and OncodriveClust test for enrichment of SNVs for functional impact and spatial clustering, respectively. ActiveDriver examines clustering of SNVs in the active domains of kinase proteins. MuSIC scores enrichment of SNVs using the same three properties as the MutSig Suite but with a different background model.
Table 1. Prominent methods for cancer gene discovery by somatic exome analysis.
| Method | Data type (method)* | Analysis principle | No. tissue cohorts (no. patients) | Total genes identified | Genes non-unique/unique to method | CGC non-unique/unique to method† | Ref. |
|---|---|---|---|---|---|---|---|
| MAIN-METHODS | |||||||
| MutSig Suite | SNV (WES) | Combined (frequency, function, clustering) | 21 (4,742) | 260 | 191/69 | 98/7 | 9,18 |
| OncodriverFM | SNV (WES) | Function | 28 (6,792) | 426 | 281/145 | 127/31 | 29 |
| OncodriverCL | SNV (WES) | Clustering | 28 (6,792) | 79 | 72/7 | 52/2 | 30 |
| ActiveDriver | SNV (WES) | Clustering (+phos-associated mutations) | 12 (3,205) | 106 | 74/32 | 30/5 | 15,17 |
| MuSIC | SNV (WES) | Combined (frequency, function, clustering, correlation with clinical phenotype) | 12 (3,205) | 182 | 141/41 | 81/3 | 13,15 |
| ALT-METHODS | |||||||
| Gistic2.0—amplifications | CNV (SNP6) | Frequency | 34 (10,752) | 1,569 | 432/1137 | 53/21 | 14 |
| Gistic2.0—deletions | CNV (SNP6) | Frequency | 34 (10,752) | 6,897 | 671/6226 | 98/65 | 14 |
| IntOGen—CNV | CNV (SNP6) | Frequency+RNA expression | 16 (4,068) | 29 | 28/1 | 25/0 | 16 |
| Dendrix | SNV (WES) | Mutual exclusivity | 12 (3,281) | 17 | 28/2 | 23/1 | 32 |
| HotNet2 | SNV+CNV (WES+SNP6) | Network | 12 (3,281) | 147 | 96/51 | 43/0 | 31 |
| Fusion/translocations | FUS (RNA-seq) | Recurrent fusions | 13 (4,366) | 492 | 236/256 | 41/18 | 33 |
| TOTALS: | 42 | 8,871 | 906/7,967 | 175/153 | |||
*Data types: CNV, copy number variant; FUS, gene fusion; SNV, single nucleotide variant. Methods: RNA-seq, RNA sequencing; SNP6, affymetrix SNP array; WES, whole-exome sequencing.
†Number of genes identified within the CGC-positive reference set.
We also considered five analysis methods that, although not specifically designed for cancer gene discovery, can be used for this purpose (ALT-METHODS, Table 1): Gistic2.0, a method for identifying focused genomic regions affected by recurrent CNVs (we used all genes within so-called ‘narrow peaks')14; IntOGenCNV, which identifies genes within recurrent CNVs that have corresponding changes in messenger RNA (mRNA) expression level16; HotNet2, a method for mining public databases of molecular interactions to identify subnetworks of genes recurrently affected by SNVs and CNVs (we used all genes in ‘core' and ‘linker' networks)31; Dendrix, a method for detecting ‘mutually exclusive' gene sets, in which SNVs are found in no more than one of these genes per patient32; and a method for detecting recurrent gene fusion events which we have labelled Fusion-genes33. All of the above methods pertain to somatic alterations to genes and, in particular, the MAIN-METHODS are based wholly on analysis of exome SNVs as the primary focus of our study. Some of the ALT-METHODS are assisted by additional measurements, for example, mRNA expression.
Cancer gene reference lists
To benchmark these methods, we considered multiple cancer gene lists compiled by various groups34,35,36,37 (Table 2). The Cancer Gene Census version 73 (CGC) is a set of 571 genes manually curated by the Sanger Institute34. It includes genes affected by alterations of all types, including somatic and germline SNVs, CNVs and translocations; genes are annotated with the relevant cancer tissue types when this information is available. We considered the entire CGC as well as the subsets of genes known to be impacted by the various alteration types (CGC-SNV, CGC-CNV, CGC-TRANS, CGC-SOMATIC and CGC-GERMLINE). Second, we queried UniprotKB, a manually curated database of protein functions35, for the keyword-terms ‘proto-oncogene,' ‘oncogene' and ‘tumour-suppressor gene,' resulting in 413 human genes. Third, a query of DISEASES36, a database of disease-gene associations based largely on text-mining approaches, yielded a list of 691 genes associated with cancer. Fourth, the Atlas of Genetics and Cytogenetics in Oncology and Haematology (AGO) provides a set of 1,430 cancer genes manually curated by a collaborative effort spanning multiple centres37. We also assembled a list of negative control genes, that is, genes in which alterations are less likely to drive cancer. AGO provides such a negative set of 7,410 genes that have no evidence for association with cancer. We further filtered this list by excluding any gene in a cancer-related pathway from the MSigDB database38, resulting in a conservative set of 2,217 negative control genes (AGO-NEG).
Table 2. Overview of positive cancer reference sets.
| Number of genes | Curation process | Alteration type | Somatic/germline | Ref. | |
|---|---|---|---|---|---|
| CGC-Somatic | 532 | Manual | SNV, CNV, Trans/fusion | Somatic | 34 |
| CGC-SNV | 188 | Manual | SNV | Somatic | 34 |
| CGC-TRANS* | 327 | Manual | Trans/fusion (not SNV) | Somatic | 34 |
| CGC-CNV* | 15 | Manual | CNV (not SNV) | Somatic | 34 |
| CGC-Germline† | 38 | Manual | SNV, CNV, Trans/fusion | Germline (not somatic) | 34 |
| UniprotKB | 412 | Manual | Unspecified | Both | 35 |
| Text-mining | 711 | Automated | Unspecified | Both | 36 |
| AGO | 1,430 | Manual | Unspecified | Both | 37 |
*Genes altered by translocations/fusions or CNVs, respectively, but not by SNVs.
†Genes altered in germline only; excludes genes also altered somatically.
Assessments of performance
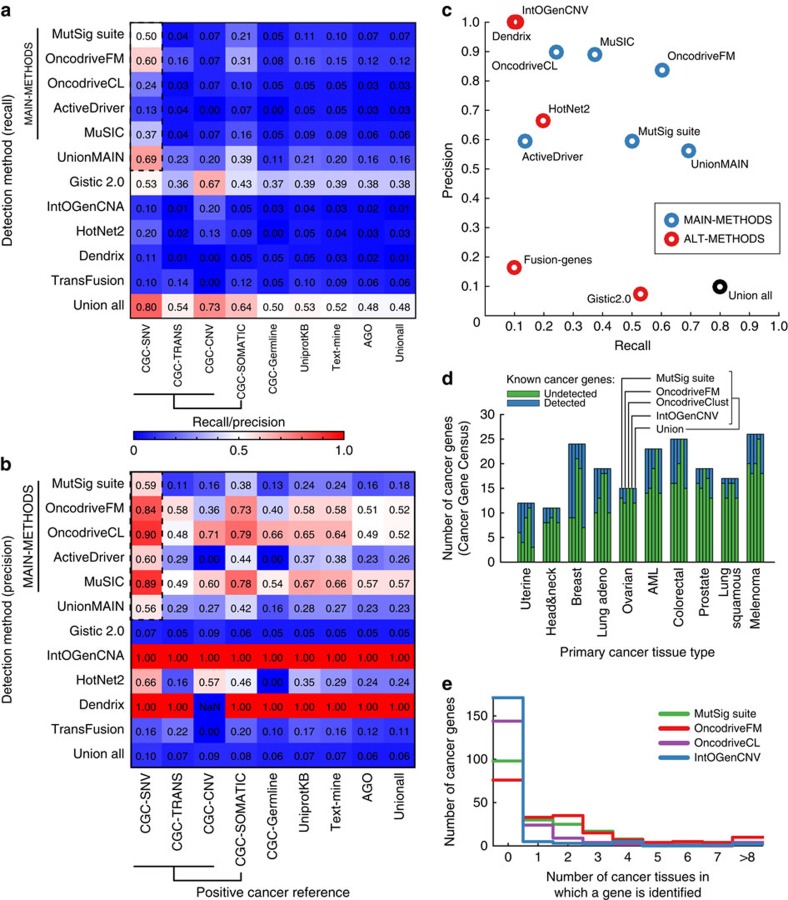
These benchmarks were used to evaluate each tumour sequence analysis method as follows. First, method performance was evaluated by considering the set of genes identified, whether by analysis of separate tissues or by pan-cancer analysis of all tissues together. We found that most methods were conservative in their detection, favouring precision over recall (Fig. 2a,b, Supplementary Fig. 1). Among the five MAIN-METHODS, testing against the CGC-SNV cancer reference and AGO-NEG negative control sets, recall ranged from 13% to a peak of 60% (Fig. 2c). In contrast, precision ranged from 59 to 90%. Performance results for other cancer genes sets were comparable or lower (Fig. 2a,b). Thus, the genes identified by tumour sequence analysis are likely to be known cancer genes (higher precision) but correspond to a smaller fraction of all known cancer genes (lower recall). As all methods had access to the same sets of reference cancer genes used for our benchmarks, and may have trained against these, these findings may represent an upper bound on performance.
Figure 2. Performance of methods.
Heatmaps showing the (a) recall and (b) precision of each method (rows) tested against each positive cancer reference set (columns). Dashed box highlights the performance of MAIN-METHODS on the CGC-SNV reference set. To compute precision, we assume the proportion of cancer genes is 5% of all human genes; precision values for other proportions are shown in Supplementary Fig. 1 with qualitatively similar results. (c) Precision/recall plot detailing results from a and b for CGC-SNV cancer genes. (d) Summary of CGC-SNV genes curated for particular cancer tissues versus their cancer detection status based on genome analysis by four different methods and their union. (e) Count of CGC-SNV genes as a function of the number of cancer tissue types in which each gene has been detected thus far.
Next, we analysed the ability of the panel of methods to identify reference cancer genes specifically annotated to particular tissue types (Fig. 2d). For this purpose, we considered genes identified by a method when analysing data from each tumour tissue individually. Analysed in this way, recall was in the range of 0–75% with a median of 27%, depending on tissue and method (CGC-SNV set, Fig. 2d and Supplementary Fig. 2). Overall, we found that 59% of CGC-SNV reference genes annotated to a particular tissue were not identified by any of the methods applied to that tissue (Supplementary Fig. 2). On the other hand, of those identified, the majority were detected in more than one tissue type (Fig. 2e), which also held true when examining tumour suppressor and oncogenes separately (Supplementary Fig. 3). Thus, analysis of tumour genome data from single tissues results in low recall characteristics that are qualitatively similar to those observed earlier in the aggregate analysis.
Of the 239 CGC cancer genes identified by any sequence analysis method, most were found by multiple methods (53% were by 2 or more, 27% by 4 or more). This observation led us to postulate that some cancer genes might be easier (or harder) to detect through all forms of sequence analysis. Further exploratory analysis revealed that genes identified by two or more methods tended towards high mutation frequency (one-sided Wilcoxon P<7.8 × 10−13, Supplementary Fig. 4). Moreover, a high mutation frequency was strongly associated with the performance of all methods, particularly in terms of recall, regardless of whether that method had been specifically designed as a mutation frequency detector (Supplementary Figs 5 and 6). Conversely, all methods tended to miss infrequently mutated genes. For example, methods such as MutSigCV identify genes based on increased frequency of SNVs compared with the genome-wide mutation rate, while methods such as oncodriveFM detect SNVs likely to be highly damaging to protein function; regardless, these methods show a very strong correspondence in the sets of cancer genes they identify15,29. Thus, genes that are commonly impacted by one type of event are likely to be impacted by other types of events also; conversely, genes rarely affected by an event type tend to be rarely affected by other types of events also. Given this consistent bias, it might be difficult for any method based solely on sequence analysis to recover some (for example, rarely mutated) cancer genes.
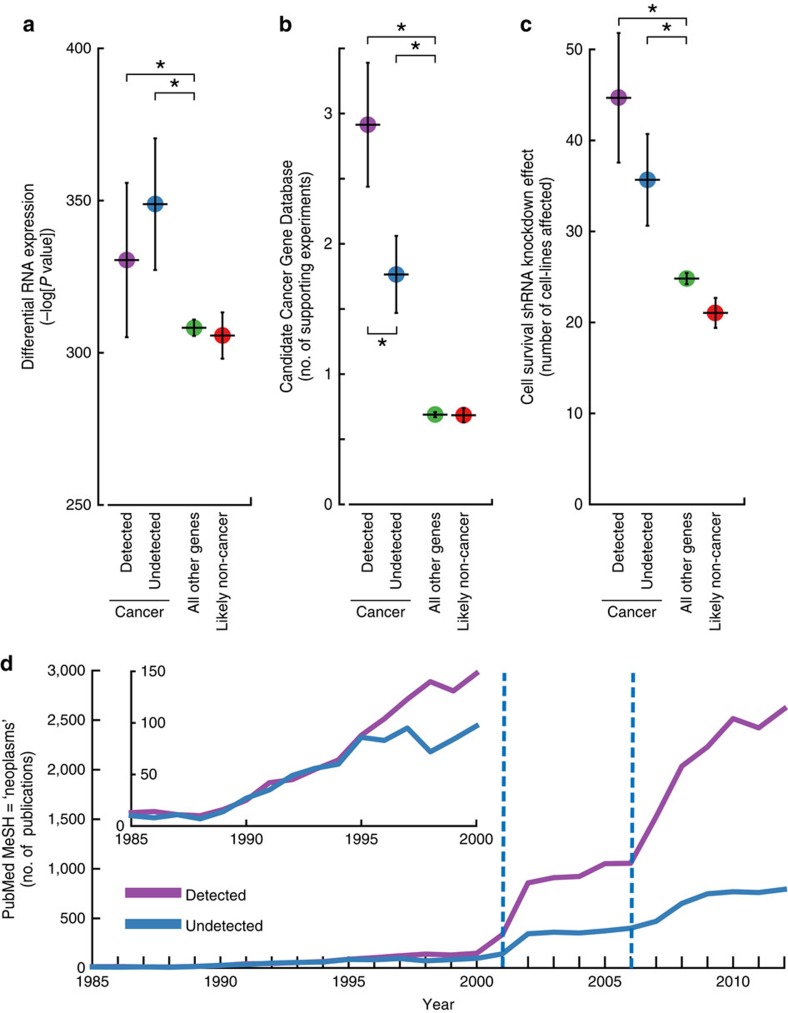
Undetected reference genes have support in independent data
A potential concern following these performance assessments was the validity of the cancer gene reference lists, as these lists might contain genes erroneously labelled as positive or negative cancer genes. If a positive reference set were to include many genes with no functional role in cancer, or with low penetrance (that is, mutations that do not always lead to cancer), this situation could clearly explain the low recall of these methods. Accordingly, we examined the support of the reference sets according to experimental measures independent of somatic mutations, including tumour mRNA expression and functional genetic screening by gene knockout or knockdown. First, we observed that, as a whole, genes in the positive reference sets were significantly differentially expressed between tumour and normal samples. This was true of the genes detected by a MAIN-METHOD and also true of those undetected by any method (one-sided Wilcoxon P<5.6 × 10−2 and P<4.0 × 10−5, respectively, Fig. 3a and Supplementary Fig. 7). Second, we found that genes in the positive reference sets had orthologs that were significantly enriched in genetic screens for cancer drivers in mice, as previously determined by transposon-mediated gene knockout39. Once again, this result held true whether or not the reference genes had been detected by sequence analysis methods (one-sided Wilcoxon P<1.49 × 10−43 and P<3.06 × 10−18, respectively; Fig. 3b and Supplementary Fig. 7). Third, both the detected and undetected cancer genes were strongly enriched for genes affecting cancer cell line growth, as previously determined by small hairpin RNA (shRNA) knockdown40 (one-sided Wilcoxon P<4.5 × 10−22 and P<2.15 × 10−18, respectively, Fig. 3c and Supplementary Fig. 7). By all three of these measures, the negative control genes were found to be no different or significantly lower than background (two-sided Wilcoxon P=0.51, P=0.23 and P<0.02 for differential expression, mouse genetic screens and cancer cell line genetic screens, respectively, for AGO-NEG). Although it is impossible to rule out any error in the reference sets, these findings suggest that they can be validated by multiple experimental screens performed independently of each other. Moreover, reference genes undetected by sequence analysis methods have a similar level of support as reference genes that are detected in terms of both differential expression and knockdown effect on cell line growth. Despite this support, undetected cancer genes have similar mutation frequencies as the negative reference genes or the genome-wide background (two-sided Kolmogorov–Smirnov test (KS-test) P=0.76, Supplementary Fig. 8), suggesting a reason why they have not yet been found by any sequence analysis method.
Figure 3. Experimental support for reference cancer gene lists.
(a–c) Support for CGC cancer genes detected by any of the MAIN-METHODS for analysing tumour genomes (Cancer Detected) versus those cancer genes that were undetected by any of these (cancer undetected). Also shown is support for the AGO-NEG negative control set of non-cancer genes (Likely non-cancer) and the remainder of genes in the genome-wide background (all other genes). Whisker plots indicate mean and the 95% confidence interval of the mean. Support is evaluated using: (a) RNA-seq tumour-normal differential expression in The Cancer Genome Atlas (TCGA). (b) Number of times a gene has been identified in independent cancer genetic screens in mice. (c) Number of Project Achilles cell lines with a measured impact (top/bottom 10%) on growth as a result of shRNA knockdown. An asterisk (*) indicates a significant difference in medians was found between the two sets. (d) The number of cancer publications by year comparing detected and undetected CGC cancer genes.
We also found a large difference between cancer genes detected versus undetected by sequence analysis in terms of literature citations. Whereas both detected and undetected positive reference genes show a significantly elevated number of publications compared with background (one-sided Wilcoxon P<8.3 × 10−44 and P<2.5 × 10−16, respectively), far more publications are devoted to those that are detected by sequence analysis (one-sided Wilcoxon P<2.7 × 10−22). In fact, genes in either category are cited with similar frequency in cancer publications through the late 1990's (Fig. 3d). Starting in 2001, however, the citation rate for detected cancer genes increases significantly, with a second rate increase starting in 2006 (F-test for both increases, P<2.3 × 10−24). As these increases coincide with the emergence of human genomics and next-generation sequencing, respectively, one might speculate that DNA sequencing technology may have encouraged a focus in cancer research towards a particular class of ‘sequence-detectable' cancer genes.
Effects of increasing genome number and coverage
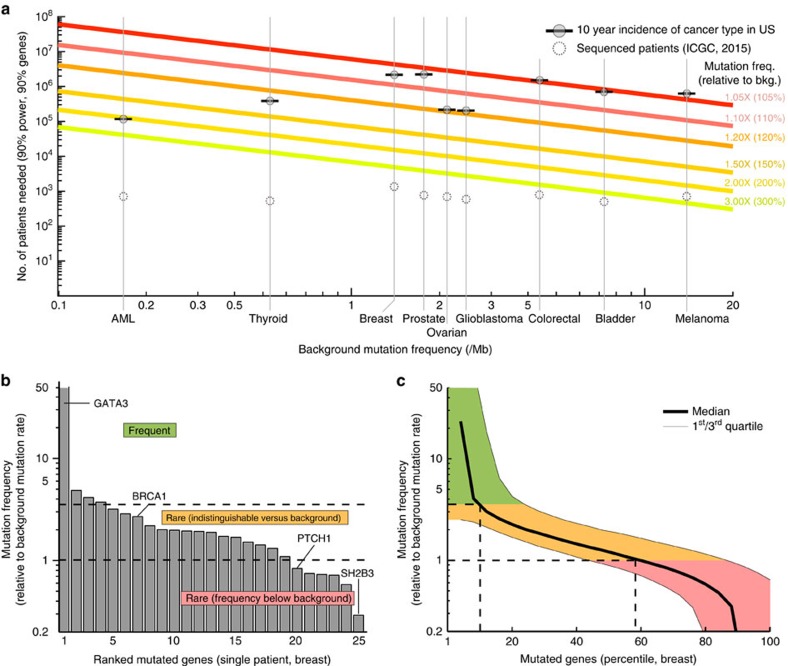
Given the expected growth in DNA sequencing capacity over the next few years, it seems feasible that such information will soon be generated for a large proportion of cancer patients. Thus, a key remaining question was whether the low recall of exome sequence analysis methods might be addressed in the near future given much greater numbers of samples. Using a previously described power calculation18, we estimated the minimum gene mutation frequency that can be distinguished accurately as a function of the number of tumour exomes analysed. By sequencing up to every new cancer patient in the United States, totalling ∼1.3 million new cases annually41, we found that the minimum detectable mutation frequency is indeed expected to decrease, from the present ∼3.4 times the background mutation rate to ∼1.1 (melanoma) to 2.0 (AML) times the background (Fig. 4a). Interestingly, nearly half of somatically mutated genes fall below that range (shown for breast cancer in Fig. 4b,c). These findings suggest that even if we analysed the exomes of all tumours in the US for 10 years using current methods, known cancer genes might remain undetected.
Figure 4. Power to detect recurrently mutated genes as the number of tumour exomes increases.
(a) Number of patient samples (y axis) necessary for detecting a cancer gene, as a function of the background somatic mutation rate of the tissue (x axis) and the fold increase in mutation rate of the cancer gene above this background (coloured lines). The total 10-year U.S. incidences of major cancer types are indicated (grey circles with horizontal bars), along with the number of patients currently sequenced as listed by the ICGC database v20 (dotted circles). (b) Mutated genes of a single breast adenocarcinoma patient, ranked by mutation frequency within tumours of this tissue type. (c) Same analysis showing the median behaviour for 881 The Cancer Genome Atlas (TCGA) patients with breast cancer. Mutated genes in each patient are ranked by mutation frequency; the median mutation frequency over all patients is plotted for each percentile.
Another key question will be whether or not replacing exome sequencing with whole-genome sequencing (WGS) will improve the ability to identify certain cancer genes. For example, the promoter of the TERT telomerase gene has been found to be frequently mutated in cancer42,43, allowing this gene to be clearly implicated by WGS. If many genes are like TERT, WGS might indeed pave the way for identifying a comprehensive catalogue of cancer genes. On the other hand, WGS greatly increases the number of background/passenger mutations under consideration and faces unique challenges such as associating mutations outside of coding regions with specific effects. While there are still too few cancer WGS studies to allow more than a cursory analysis, a recent WGS study of ovarian tumours reported no additional cancer genes beyond what had been found by earlier exome sequencing of the same cancer type44.
An important distinction to be made is the difference between a recurrent alteration within a patient population (for example, BRAF V600E in melanoma), and a gene acting as a driver within a particular tumour under a specific context (for example, germline variants, tissue type and therapeutic regimen). While ‘cohort drivers' are certainly interesting from a translational perspective, there is ample evidence for rare yet clinically important events45,46,47,48. Fundamentally, a complete compendium of cancer genes should include both cohort-recurrent alterations and individual, contextually-active drivers, including those that show a measurable effect only when analysed in combination.
From a clinical perspective, an individual patient cares not whether the cancer genes causing their tumour are frequently mutated in other patients, but whether their mutations can be targeted. Recurrent driver mutations are likely selected early during tumorigenesis49, hence their critical role in many patients and potential as compelling drug targets in different cancer types. However, individual cancers may also be affected by rare mutations affecting the same pathways as common oncogenic drivers, and they too are selected in individual patients rendering them compelling personal drug targets. The findings presented here suggest that ignoring such mutations may miss important therapeutic opportunities. Indeed, cancer gene panels currently in use as clinical diagnostics45,50,51,52 are based primarily on the most recurrently mutated genes in favour of more comprehensive alternatives. Before expanding the clinical panels to sequence all genes or all genomic DNA, we still need some method, or collection of methods, to distinguish which sequences are clinically important. Given the success of experimental techniques independent of sequence analysis (Fig. 1a), a viable strategy may be to complement ongoing genome sequencing campaigns with renewed efforts in cell biology, biochemistry, transcriptional profiling and other ‘omics analysis to identify the key genes of cancer.
Methods
Tumour somatic mutation data
We use somatic mutation data provided in the supplement of Lawrence et al.4, downloaded from http://tumorportal.org on 22 January 2014, and available in Synapse (http://www.synapse.org), accession number syn1729383. These data contain tumour somatic variants and short insertion, and deletions for a set of 4,742 patients from 21 cancer types18.
Genes detected by each method
The analysis presented here is exclusively based on results previously published for each of the respective methods, collected from publications listed in Table 1. Given the wide range of parameters and processing steps, we believe the best way to represent all methods is to use their own previously presented results from each publication.
Analysis of literature support
To evaluate literature support for each cancer gene (Fig. 1a), we use the NCBI gene2pubmed table (ftp://ftp.ncbi.nlm.nih.gov/gene/DATA/gene2pubmed.gz, 11 February 2015), from which we can compile a list of 1,015,815 publications (PubMed IDs) associated with human genes. The corresponding PubMed XML record for each publication is analysed to extract the associated MeSH subject terms, which are then indexed to the MeSH term tree (2015 version) propagating each association to all ancestor terms. We select publications that are MeSH-annotated as cancer related (Neoplasm;C04) with a corresponding experimental technique (Investigative Techniques;E05). The resulting mapping of PubMed publications to MeSH terms is used to compile all distinct cancer-related publications with an experimental component for each cancer gene. From this information we classify the first such publication of each gene into seven broad experimental categories by manual curation. Techniques or MeSH terms that cannot be assigned non-ambiguously are discarded (for example, PCR amplifications). To compare the amount of publications for cancer genes detected by any of MAIN-METHODS versus those left undetected, we examine all PubMed publications with cancer MeSH annotation (Neoplasm;C04) as above. To test for association between detected/undetected status and publication date, the number of publications per year (pubYear) is fit using a generalized linear model with three binary categorical variables: isDetected (detected or undected), isGenomeEra (published after the year 2000, the approximate era of genome sequencing) and isNextGenEra (published after 2006, the approximate era of next-generation sequencing). The optimal model is selected using a standard step-up procedure based on a Bayesian information criteria. This model: pubYear ∼1 + isDetected*isGenomeEra + isDetected* isNextGenEra) includes a significant interaction between isDetected and isGenomeEra, and between isDetected and isNextGenEra (Z-test P<4.3 × 10−3 and Z-test P<1.3 × 10−5 respectively). A similar regression restricted to the period 1985–2000 fails to produce a model with any non-constant significant terms.
Classification performance
We use three measures of classification performance to compare the different methods for cancer gene detection. In each instance we use a positive and negative cancer reference and compare it with the cancer genes detected by a given method. The set of detected genes also found in the positive set is referred to as the true-positive (TP) set; similarly the set of detected genes not in the negative reference set is referred to as the false-positive (FP) set. The set of genes undetected in the negative set is referred to as the true-negative (TN) set; the set of undetected genes in the positive set is referred to as the false-negative (FN) set. Genes not included in either the positive or negative reference sets are ignored. To evaluate performance we use the following three measures: precision, TP/(TP+FP); recall, TP/(TP+FN); and informedness, recall+specificity−1.
Differential expression analysis
The Cancer Genome Atlas tumour and normal RNA-seq mRNA expression data are downloaded from Firehose (http://gdac.broadinstitute.org/, 14 February 2015) after normalization of RNA-seq reads to expected read counts using the RSEM algorithm and quantile normalization across all cancer tissue cohorts. We examine differential expression between tumour and normal samples in eight cohorts which each have >40 normal samples (breast, head/neck, clear cell renal, liver, lung adeno, lung squamous, prostate and thyroid), spanning a total of 540 normal and 4,816 tumour samples. We test for differential expression using a Welch's t-test for a difference in means of samples with unequal variances, and use the sum of the negative log P values across the nine cohorts as a single summary statistic per gene.
Response to shRNA knockdown
Project Achilles shRNA response data (v2.4.3, 14 November 2014) provide RNAi knockdown values for 56,904 hairpin shRNA by 216 cell lines. These values are normalized using a simplified version of the ATARiS algorithm53 resulting in knockdown values for 14,082 genes. For every gene we record the number of cell lines with knockdown values in the top or bottom 10%.
Mutation frequency calculations
Mutation frequency versus background is calculated using the MutSigCV method to detect enrichment in mutations9. Briefly, for every gene g and patient p, the non-synonymous (ns) mutation frequency  is the ratio of observed ns mutations nns to expected ns mutations Ens:
is the ratio of observed ns mutations nns to expected ns mutations Ens:
 |
Ens is estimated separately for each gene using a local regression method as reported18. MutSigCV computes the  statistic for different classifications of mutations (transitions, transversions, nonsense, missense, etc.), then combines these different statistics to compute an overall P value of significance that each gene is frequently mutated in the patient cohort, assuming a beta-binomial null distribution. We base our analysis on the implementation and covariates provided as part of MutSigCV v1.4, downloaded on 22 June 2014. We have optimized this code for efficiency and to exploit parallel processing, but otherwise it is algorithmically identical to the original implementation.
statistic for different classifications of mutations (transitions, transversions, nonsense, missense, etc.), then combines these different statistics to compute an overall P value of significance that each gene is frequently mutated in the patient cohort, assuming a beta-binomial null distribution. We base our analysis on the implementation and covariates provided as part of MutSigCV v1.4, downloaded on 22 June 2014. We have optimized this code for efficiency and to exploit parallel processing, but otherwise it is algorithmically identical to the original implementation.
Estimating power to detect genes by mutation frequency
Following a previously described procedure18, we estimate the sample size needed to detect a frequently mutated gene at a genome-wide level of significance (α<5 × 10−6) with power at least 90% (β≥0.9). Effect size (ϕ) is computed as the difference in proportions between the mutation rate of the cancer gene (P1) and the background mutation rate of similar genes in that tissue type (P0). Given α, β and ϕ, sample size is computed using a standard method54. P0 is defined as described18:
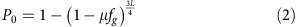 |
μ A variable representing the background mutation frequency of the tissue.
fg=3.9 A gene-specific background mutation rate estimated by MutSigCV. The selected value corresponds to the 90 percentile of genes.
L=1,500 The length of a gene in coding bases, representing the 90 percentile of genes.
¾ Corresponds to the typical fraction of mutations that are non-synonymous.
R A variable representing the mutation frequency above background.
P1 frequency is defined as a multiplicative product of the background:
 |
Data availability
Data used in this study was gathered from publicly available sources as indicated above. Literature support and year of first mention in cancer publication for each cancer gene was downloaded from NCBI gene2pubmed table (ftp://ftp.ncbi.nlm.nih.gov/gene/DATA /gene2pubmed.gz, downloaded on 11 February 2015). Cancer genes detected by each method were downloaded from the Supplementary Information and accompanying data provided along with publications referenced in Table 1. Known cancer reference genes were downloaded from the sources indicated in Table 2, in particular, Sanger Institute Cancer Gene Censuses database (CGC, http://cancer.sanger.ac.uk/files/cosmic/current_release/cancer_gene_census.csv, version 73, downloaded on 28 June 2015). Tumour expression data were downloaded from the Firehose repository (http://gdac.broadinstitute.org/, downloaded on 14 February 2015). Response to shRNA knockdown measurements were downloaded from the Project Achilles data portal (http://www.broadinstitute.org/achilles/datasets/5, version 2.4.3, download on 14 November 2014). Mouse genetic screening data were downloaded from the CCGD database (http://ccgd-starrlab.oit.umn.edu/, downloaded on 19 August 2015). Tumour somatic mutation data for individual patients is available on Synapse (http://www.synapse.org), accession number syn1729383. All other data is contained within the Article and Supplementary Information, or available from the authors on request.
Additional information
How to cite this article: Hofree, M. et al. Challenges in identifying cancer genes by analysis of exome sequencing data. Nat. Commun. 7:12096 doi: 10.1038/ncomms12096 (2016).
Supplementary Material
Acknowledgments
This work was supported by the National Institutes of Health (R01 ES014811 and U24 CA184427) and a generous donation from the Fred Luddy Family Foundation. We thank Billur H. Engin for contributions that were not included in this work. We further wish to thank Anne-Ruxandra Carvunis, John Paul Shen, Andrew Gross, James Jensen, Michael Kramer and Eran Hodis for insightful comments and suggestions on the manuscript and figures.
Footnotes
Author contributions M.H. and T.I. designed the study. M.H. performed the statistical analyses. M.H., H.C. and T.I. analysed the data. M.H., J.F.K. and T.I. wrote the manuscript, with contributions from H.C., S.B., P.S.M. and S.F.
References
- Pleasance E. D. et al. A comprehensive catalogue of somatic mutations from a human cancer genome. Nature 463, 191–196 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ley T. J. et al. DNA sequencing of a cytogenetically normal acute myeloid leukaemia genome. Nature 456, 66–72 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hudson T. J. et al. International network of cancer genome projects. Nature 464, 993–998 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodis E. et al. A landscape of driver mutations in melanoma. Cell 150, 251–263 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cancer Genome Atlas Research Network. Comprehensive genomic characterization defines human glioblastoma genes and core pathways. Nature 455, 1061–1068 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cancer Genome Atlas Research Network. The Cancer Genome Atlas Pan-Cancer analysis project. Nat. Genet. 45, 1113–1120 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cancer Genome Atlas Research Network. Integrated genomic characterization of papillary thyroid carcinoma. Cell 159, 676–690 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilks C. et al. The Cancer Genome Atlas Pan-Cancer analysis project. Database 2014, bau093 (2014).25267794 [Google Scholar]
- Lawrence M. S. et al. Mutational heterogeneity in cancer and the search for new cancer-associated genes. Nature 499, 214–218 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogelstein B. et al. Cancer genome landscapes. Science 339, 1546–1558 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solimini N. L. et al. Recurrent hemizygous deletions in cancers may optimize proliferative potential. Science 337, 104–109 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garraway L. A. & Lander E. S. Lessons from the cancer genome. Cell 153, 17–37 (2013). [DOI] [PubMed] [Google Scholar]
- Dees N. D. et al. MuSiC: identifying mutational significance in cancer genomes. Genome Res. 22, 1589–1598 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mermel C. H. et al. GISTIC2.0 facilitates sensitive and confident localization of the targets of focal somatic copy-number alteration in human cancers. Genome Biol. 12, R41 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamborero D. et al. Comprehensive identification of mutational cancer driver genes across 12 tumor types. Sci. Rep. 3, 2650 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubio-Perez C. et al. In silico prescription of anticancer drugs to cohorts of 28 tumor types reveals targeting opportunities. Cancer Cell 27, 382–396 (2015). [DOI] [PubMed] [Google Scholar]
- Reimand J. & Bader G. D. Systematic analysis of somatic mutations in phosphorylation signaling predicts novel cancer drivers. Mol. Syst. Biol. 9, 637 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence M. S. et al. Discovery and saturation analysis of cancer genes across 21 tumour types. Nature 505, 495–501 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stratton M. R., Campbell P. J. & Futreal P. A. The cancer genome. Nature 458, 719–724 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinhold N., Jacobsen A., Schultz N., Sander C. & Lee W. Genome-wide analysis of noncoding regulatory mutations in cancer. Nat. Genet. 46, 1160–1165 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meindl A. et al. Germline mutations in breast and ovarian cancer pedigrees establish RAD51C as a human cancer susceptibility gene. Nat. Genet. 42, 410–414 (2010). [DOI] [PubMed] [Google Scholar]
- Whitesell L. & Lindquist S. L. HSP90 and the chaperoning of cancer. Nat. Rev. Cancer 5, 761–772 (2005). [DOI] [PubMed] [Google Scholar]
- Shih C. & Weinberg R. A. Isolation of a transforming sequence from a human bladder carcinoma cell line. Cell 29, 161–169 (1982). [DOI] [PubMed] [Google Scholar]
- Touw I. P. & Erkeland S. J. Retroviral insertion mutagenesis in mice as a comparative oncogenomics tool to identify disease genes in human leukemia. Mol. Ther. 15, 13–19 (2007). [DOI] [PubMed] [Google Scholar]
- Vogelstein B., Lane D. & Levine A. J. Surfing the p53 network. Nature 408, 307–310 (2000). [DOI] [PubMed] [Google Scholar]
- Easton D. F., Bishop D. T., Ford D. & Crockford G. P. Genetic linkage analysis in familial breast and ovarian cancer: results from 214 families. The Breast Cancer Linkage Consortium. Am. J. Hum. Genet. 52, 678–701 (1993). [PMC free article] [PubMed] [Google Scholar]
- Dittmer D. et al. Gain of function mutations in p53. Nat. Genet. 4, 42–46 (1993). [DOI] [PubMed] [Google Scholar]
- Kandoth C. et al. Mutational landscape and significance across 12 major cancer types. Nature 502, 333–339 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Perez A. & Lopez-Bigas N. Functional impact bias reveals cancer drivers. Nucleic Acids Res. 40, e169 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamborero D., Gonzalez-Perez A. & Lopez-Bigas N. OncodriveCLUST: exploiting the positional clustering of somatic mutations to identify cancer genes. Bioinformatics 29, 2238–2244 (2013). [DOI] [PubMed] [Google Scholar]
- Leiserson M. D. et al. Pan-cancer network analysis identifies combinations of rare somatic mutations across pathways and protein complexes. Nat. Genet. 47, 106–114 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vandin F., Upfal E. & Raphael B. J. De novo discovery of mutated driver pathways in cancer. Genome Res. 22, 375–385 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshihara K. et al. The landscape and therapeutic relevance of cancer-associated transcript fusions. Oncogene 34, 4845–4854 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes S. A. et al. COSMIC (the Catalogue of Somatic Mutations in Cancer): a resource to investigate acquired mutations in human cancer. Nucleic Acids Res. 38, D652–D657 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- UniProt C. UniProt: a hub for protein information. Nucleic Acids Res. 43, D204–D212 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pletscher-Frankild S., Palleja A., Tsafou K., Binder J. X. & Jensen L. J. DISEASES: text mining and data integration of disease-gene associations. Methods 74, 83–89 (2015). [DOI] [PubMed] [Google Scholar]
- Huret J. L. et al. Atlas of genetics and cytogenetics in oncology and haematology in 2013. Nucleic Acids Res. 41, D920–D924 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liberzon A. et al. Molecular signatures database (MSigDB) 3.0. Bioinformatics 27, 1739–1740 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abbott K. L. et al. The Candidate Cancer Gene Database: a database of cancer driver genes from forward genetic screens in mice. Nucleic Acids Res. 43, D844–D848 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowley G. S. et al. Parallel genome-scale loss of function screens in 216 cancer cell lines for the identification of context-specific genetic dependencies. Sci. Data 1, 140035 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group, U. S. C. S. W. United States Cancer Statistics: 1999–2010 Incidence and Mortality Web-based Report. in cdc.gov Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute (2014). [Google Scholar]
- Vinagre J. et al. Frequency of TERT promoter mutations in human cancers. Nat. Commun. 4, 2185 (2013). [DOI] [PubMed] [Google Scholar]
- Huang F. W. et al. Highly recurrent TERT promoter mutations in human melanoma. Science 339, 957–959 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patch A. M. et al. Whole-genome characterization of chemoresistant ovarian cancer. Nature 521, 489–494 (2015). [DOI] [PubMed] [Google Scholar]
- Simon R. & Roychowdhury S. Implementing personalized cancer genomics in clinical trials. Nat. Rev. Drug Discov. 12, 358–369 (2013). [DOI] [PubMed] [Google Scholar]
- Trudel S. et al. The clinical response to vemurafenib in a patient with a rare BRAFV600DK601del mutation-positive melanoma. BMC Cancer 14, 727 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johung K. L. et al. Extended survival and prognostic factors for patients with ALK-rearranged non-small-cell lung cancer and brain metastasis. J. Clin. Oncol. 34, 123–129 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dietrich S. et al. BRAF inhibition in refractory hairy-cell leukemia. N. Engl. J. Med. 366, 2038–2040 (2012). [DOI] [PubMed] [Google Scholar]
- McGranahan N. et al. Clonal status of actionable driver events and the timing of mutational processes in cancer evolution. Sci. Transl. Med. 7, 283ra54 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolli N. et al. A next generation sequencing-based approach to detect gene mutations, copy number changes and IGH translocations in multiple myeloma. Blood 124, 3364–3364 (2014). [Google Scholar]
- Frampton G. M. et al. Development and validation of a clinical cancer genomic profiling test based on massively parallel DNA sequencing. Nat. Biotechnol. 31, 1023–1031 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hovelson D. H. et al. Development and validation of a scalable next-generation sequencing system for assessing relevant somatic variants in solid tumors. Neoplasia 17, 385–399 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shao D. D. et al. ATARiS: computational quantification of gene suppression phenotypes from multisample RNAi screens. Genome Res. 23, 665–678 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences xxi, 567 p.L. Erlbaum Associates (1988). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data used in this study was gathered from publicly available sources as indicated above. Literature support and year of first mention in cancer publication for each cancer gene was downloaded from NCBI gene2pubmed table (ftp://ftp.ncbi.nlm.nih.gov/gene/DATA /gene2pubmed.gz, downloaded on 11 February 2015). Cancer genes detected by each method were downloaded from the Supplementary Information and accompanying data provided along with publications referenced in Table 1. Known cancer reference genes were downloaded from the sources indicated in Table 2, in particular, Sanger Institute Cancer Gene Censuses database (CGC, http://cancer.sanger.ac.uk/files/cosmic/current_release/cancer_gene_census.csv, version 73, downloaded on 28 June 2015). Tumour expression data were downloaded from the Firehose repository (http://gdac.broadinstitute.org/, downloaded on 14 February 2015). Response to shRNA knockdown measurements were downloaded from the Project Achilles data portal (http://www.broadinstitute.org/achilles/datasets/5, version 2.4.3, download on 14 November 2014). Mouse genetic screening data were downloaded from the CCGD database (http://ccgd-starrlab.oit.umn.edu/, downloaded on 19 August 2015). Tumour somatic mutation data for individual patients is available on Synapse (http://www.synapse.org), accession number syn1729383. All other data is contained within the Article and Supplementary Information, or available from the authors on request.