Abstract
Study Design
Prospective observational study.
Objective
Patient-based subjective ratings of symptoms and function have traditionally been used to gauge the success and extent of recovery following spine surgery. The main drawback of this type of assessment is the inherent subjectivity involved in patient scoring. We aimed to objectively measure functional outcome in patients having lumbar spine surgery using quantitative physical activity measurements derived from accelerometers.
Methods
A prospective study of 30 patients undergoing spine surgery was conducted with subjective outcome scores (visual analog scale [VAS], Oswestry Disability Index [ODI] and Short Form 12 [SF-12]) recorded; patients were given a Fitbit accelerometer (Fitbit Inc., San Francisco, California, United States) at least 7 days in advance of surgery to record physical activity (step count, distance traveled, calories burned) per day. Following surgery, postoperative activity levels were reported at 1-, 2-, and 3-month follow-up.
Results
Of the 28 compliant patients who completed the full trial period, mean steps taken per day increased 58.2% (p = 0.008) and mean distance traveled per day increased 63% (p = 0.0004) at 3-month follow-up. Significant improvements were noted for mean changes in VAS back pain, VAS leg pain, ODI, and SF-12 Physical Component Summary (PCS) scores. There was no significant correlation between the improvement in steps or distance traveled per day with improvements in VAS back or leg pain, ODI, or PCS scores at follow-up.
Conclusions
High compliance and statistically significant improvement in physical activity were demonstrated in patients who had lumbar decompression and lumbar fusion. There was no significant correlation between improvements in subjective clinical outcome scores with changes in physical activity measurements at follow-up. Limitations of the present study include its small sample size, and the validity of objective physical activity measurements should be assessed in future larger, prospective studies.
Keywords: accelerometer, Fitbit, fusion, lumbar back pain, lumbar stenosis, physical activity, objective measurement, spine surgery
Introduction
The assessment of patient recovery, rehabilitation, and clinical outcome postoperatively is important for the validation of the safety, efficacy, and economic dynamics of various spine surgical techniques.1 Traditionally, patient-based subjective ratings of symptoms and function have been used to gauge the success and extent of recovery. Commonly used scores include the visual analog scale (VAS); Short Form (SF)-8, SF-12, SF-36; and Oswestry Disability Index (ODI). Although these scores have been used extensively to demonstrate the safety and efficacy of surgical interventions, the main drawback of this type of assessment is the inherent subjectivity involved in patient scoring.2 3 Indeed, patients' own perception of their disability and symptoms, as well as variation in each patient's own environment, can have an unaccounted influence on the subjective patient-based scores.3 4
Furthermore, the issue of subjective outcome rating is increasingly important in the compensation arena. The studies that assessed patient outcome and fusion status following anterior cervical decompression fusion for radiculopathy note similar rates of fusion between compensable and noncompensable patients, but with a higher rate of poorer outcome based on subjective scoring analysis in the compensable group.5
Although pain scores have been previously used as a surrogate indicator of the level of ambulatory impairment, several recent studies have demonstrated poor correlation between subjective pain scores and ambulatory capacity measured using treadmill and walking test assessments.6 Advances in technology have led to the advent of accelerometer devices, which have the ability to accurately record physical activity data in real time, including number of steps and distance traveled. Accelerometer devices are able to produce objective measurements of physical activity outcome,7 and thus may potentially give rise to an opportunity to assess postoperative recovery in terms of physical capacity using objective measurements.8
To the best of our knowledge, no study thus far has prospectively investigated objective physical activity measurements after lumbar spine surgery and tested whether these measurements correlate well with subjective functional scores. Therefore, the aim of this study was to objectively measure functional outcome in patients who had lumbar spine surgery using quantitative physical activity measurements as derived from the accelerometers.
Methods
Ethics Approval
Approval was obtained from the South Eastern Sydney Local Health District, New South Wales, Australia (HREC 13/090). All participants provided written informed consent.
Patient Recruitment
The study was a consecutive, single-surgeon prospective series. The patients were enrolled between 2013 and 2014 by the senior author (R.J.M.), who performed all the surgical procedures. The inclusion criteria were patients who underwent lumbar spine surgery within this recruitment period, with indications including low back pain, radiculopathy, and claudication. The procedures performed included anterior lumbar interbody fusion (ALIF), laminectomy, diskectomy, and posterior lumbar interbody fusion. The exclusion criteria included infection, osteoporosis, cancer, and any other comorbid conditions that were thought to substantially limit activity beyond symptoms of back pain, radiculopathy, and neurogenic claudication. Patients who were not motivated to pursue the requirements of the study, those with poor memory or mental health issues, and those who would not consent to the study were excluded.
Accelerometry
Physical activity performance was assessed with a Fitbit zip accelerometer (Fitbit Inc., San Francisco, California, United States). The Fitbit activity monitor is a small, lightweight, commercially available device that is clipped to the patient's belt or waistband or can be worn in pant pockets. The Fitbit was utilized as the battery life was 6 months, which enhanced compliance. Patients were given a unique username and password (consent obtained) to access the data. The Fitbit was synced to the patients' smartphone or computer, if a smartphone was not available.
The Fitbit device is equipped with a three-dimensional accelerometer and altimeter. Based on the inbuilt algorithms and validation studies,9 the Fitbit device is able to estimate the number of steps taken, flights of stairs climbed, distance walked, and calories expended. The authors (P.J.R., R.J.M., and M.M.) verified the accuracy of the Fitbit by testing it while walking and running, and the accuracy was found to be 98 ± 1%.
The Fitbit activity monitor was used to record average physical activity date, preoperatively and postoperatively. For the present study, follow-ups at 1, 2, and 3 months were reported. The parameters recorded included number of steps taken, distance traveled, and calories burned, which were used to calculate the average number of steps per day, distance traveled per day, and calories burned per day on follow-up. An example of such data recorded by the Fitbit activity tracker and synced to a mobile/computer is demonstrated in Fig. 1.
Fig. 1.
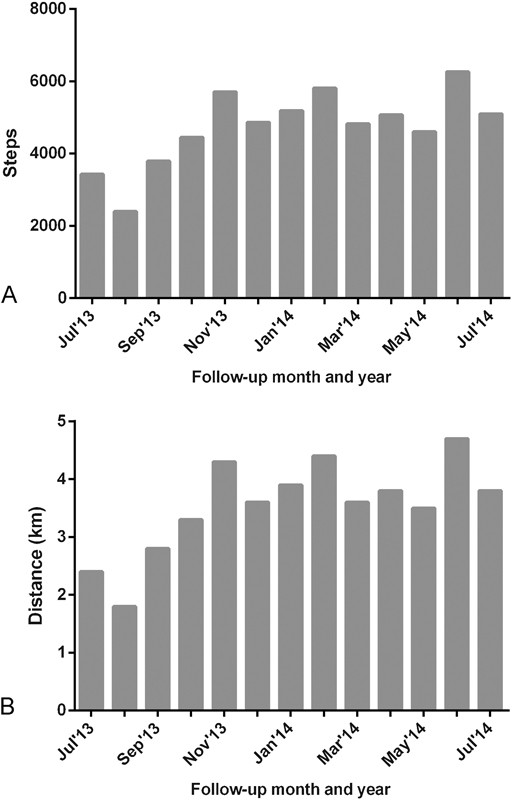
Screenshot of prospective data collection indicating (A) average steps per day and (B) average distance traveled per day from a patient recovering from a two-level fusion over 12-month periods. The initial month of data shown is the average number of steps per day or distance traveled per day preoperatively.
Self-Reported Outcomes
Patient clinical outcomes were measured using self-reported scores, including the 10-point VAS for back and leg pain, the ODI, and the SF-12, which included Mental Component Summary (MCS) and Physical Component Summary (PCS). The outcomes were measured preoperatively and postoperatively at each visit.
Statistics
The demographic variables including age and gender were summarized using descriptive statistics (mean ± standard deviation or percentage). Gaussian normality distribution was verified using the D'Agostino-Pearson omnibus test. The pre- and postoperative parameters were compared with a two-tailed, paired-sample t test. A p value < 0.05 was considered significant. All statistical analyses were performed using SPSS software (version 22.0, IBM, Armonk, New York, United States). The Pearson correlation test was performed to determine whether there was a significant correlation between changes in physical activity parameters (steps, distance, calories) versus changes in clinical outcome (VAS, ODI, and SF-12 MCS and PCS scores). The Pearson correlation was presented as r and p value, where r signifies the strength of the correlation. The close the value of r is to 1 or −1, the stronger the correlation; an r value close to 0 signifies almost negligible correlation.
Results
A total of 30 patients were included in the study. Twenty-eight patients completed the accelerometer physical activity and clinical follow-up period. Two patients lost their Fitbit and therefore objective data analysis was not complete and they were excluded. The average age of the cohort was 42.60 ± 10.34 years, and 17 patients were men (60.7%). ALIF was performed in 7 patients (25%), laminectomy in 13 patients (46.4%), posterior lumbar interbody fusion in 2 patients (7.1%) and diskectomy in 6 patients (21.4%). The primary indications included low back pain (n = 4), radiculopathy (n = 14), and claudication (n = 4) with several patients having multiple indications.
In the preoperative period, the mean number of steps taken per day was 5,255 ± 2,883 steps. Following lumbar spine surgery, the number of steps per day at 1-month follow-up was 4,574 ± 2,186, compared with 7,135 ± 3,112 at 2-month follow-up and 8,312 ± 4,218 at 3-month follow-up. There was a significant increase in the number of steps compared with preoperative status at 2-month follow-up (35.8%, p = 0.002) and 3-month follow-up (58.2%, p = 0.008; Fig. 2).
Fig. 2.
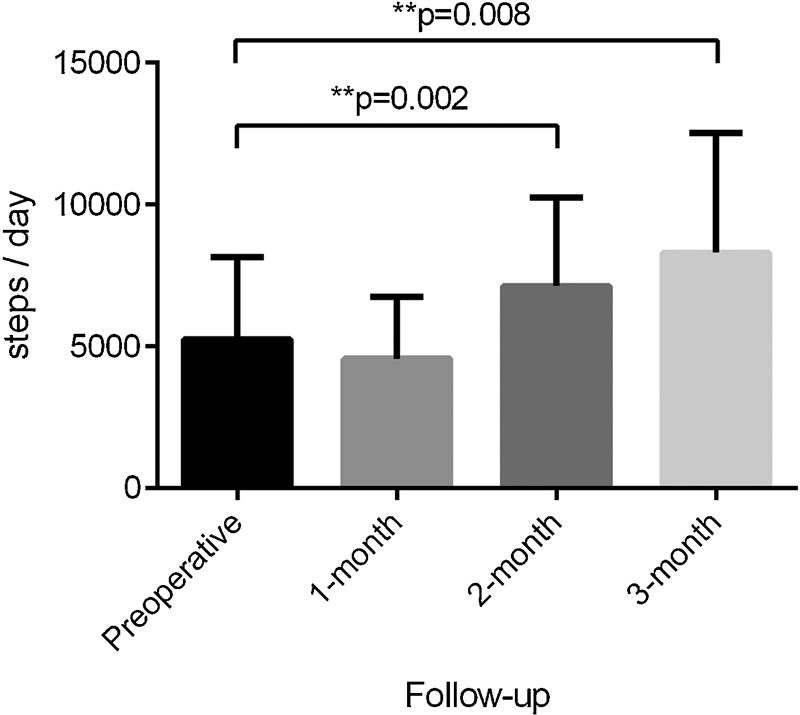
Change in number of steps per day taken at follow-up.
The mean distance traveled in the preoperative period was 3.8 ± 2.2 km/d, compared with 3.4 ± 1.7 km/d at 1-month follow-up. There was a 39.5% significant increase in distance traveled per day at 2-month follow-up to 5.3 ± 2.5 km (p = 0.002), and 63% increase to 6.2 ± 3.6 km/d at 3-month follow-up (p = 0.0004). There was no difference in the number of steps taken preoperatively versus early postoperative phase (1-month follow-up; Fig. 3).
Fig. 3.
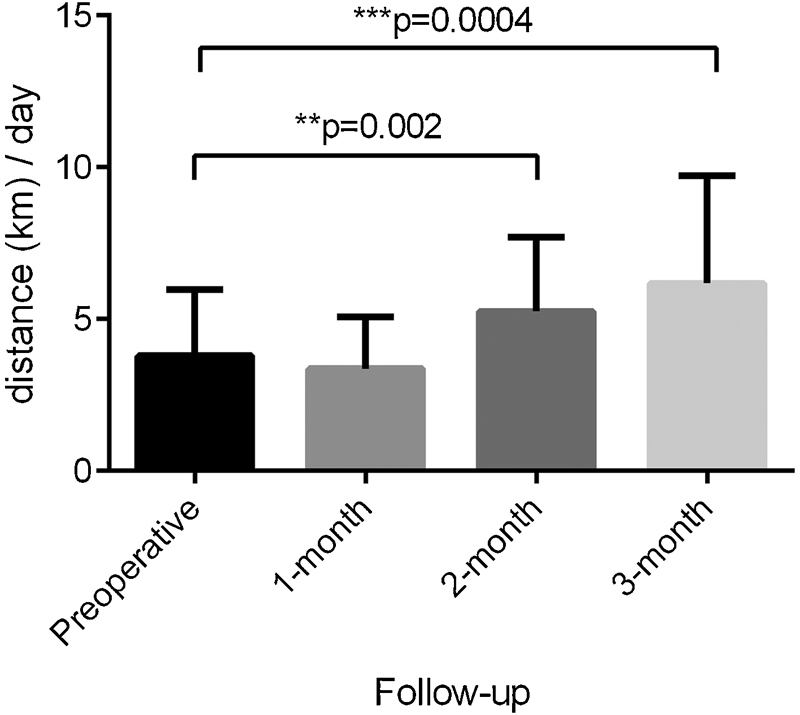
Change in distance traveled per day at follow-up.
The mean number of calories consumed in the preoperative phase was 2,137 ± 481 per day, compared with 2,089 ± 401 per day at 1-month, 2,228 ± 490 per day at 2-month, and 2,592 ± 1,185 per day at 3-month follow-up. There was no significant difference in calories consumed between these phases (Fig. 4).
Fig. 4.
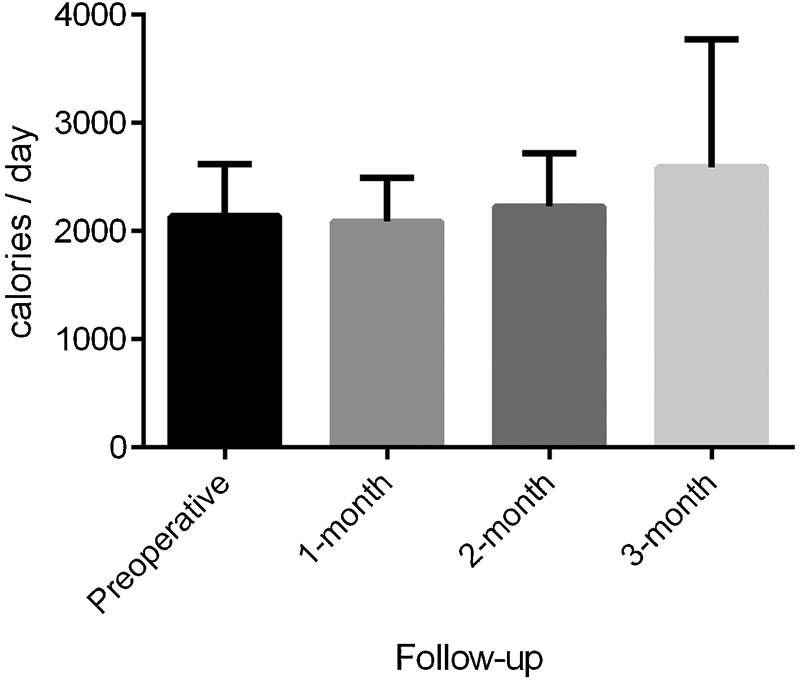
Change in calories per day consumed at follow-up.
At latest follow-up, there was a significant reduction in VAS back pain score from 7.0 ± 2.7 to 2.8 ± 1.9 (p = 0.0002). VAS leg pain scores also significant decreased postoperatively from 6.3 ± 3.3 to 1.5 ± 0.7 (p = 0.01). After surgery and follow-up, there was a significant increase in ODI scores from 46.0 ± 19.0 to 26.9 ± 17.7 (p = 0.005). Although there was no change in the MCS component of SF-12 scores (p = 0.65), a significant increase in the PCS component of SF-12 scores from 33.0 ± 8.2 to 44.0 ± 8.7 (p = 0.02) was noted (Fig. 5).
Fig. 5.
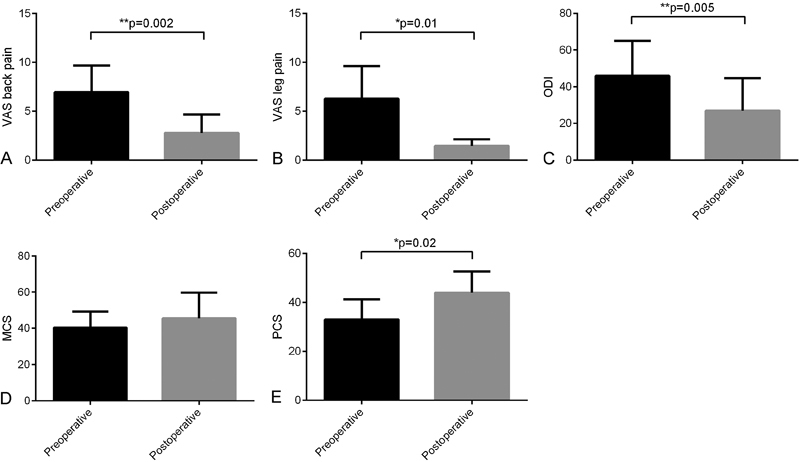
Preoperative and postoperative clinical outcomes following lumbar spine surgery: (A) visual analog scale (VAS) back pain; (B) VAS leg pain; (C) Oswestry Disability Index (ODI); (D) Short Form 12 (SF-12) Mental Component Summary (MCS) score; (E) SF-12 Physical Component Summary (PCS) score.
The Pearson correlation test was used to evaluate the contributions of physical performance to clinical and function outcome. The analysis between improvement in number of steps per day with change in VAS back pain (r = − 0.446, p = 0.316), VAS leg pain (r = − 0.472, p = 0.285), and PCS (r = 0.058, p = 0.902) scores showed no significant correlation. There was also no significant correlation between improved distance traveled per day with change in VAS back pain (r = 0.333, p = 0.348), VAS leg pain (r = − 0.012, p = 0.975), and PCS (r = 0.117, p = 0.747) scores.
Discussion
The current prospective series demonstrates that: (1) accelerometry is a feasible method of measuring objective physical activity parameters with high patient compliance; (2) there was a significant improvement in steps per day and distance traveled per day at follow-up following lumbar spine surgery; and (3) although both subjective pain/functional scores and physical activity parameters improved with follow-up, the lack of correlation indicates the limited power of subjective scores to predict physical activity levels during recovery and follow-up from lumbar spine surgery.
Few researchers have studied the role of accelerometers for objective measurements of physical activity in patients with lumbar spinal pathology and in patients undergoing lumbar surgery. In one such study in patients with lumbar spine stenosis by Pryce et al,10 accelerometers was used to measure physical activity, including the number of calories consumed per kilogram per day, the intensity and duration of exercise, and ambulation via bout length. Linear regression and adjusted models were then use to correlate this data with clinical outcome scores including ODI and SF-36 in 33 patients with lumbar spinal stenosis. The authors concluded that subjective measurements for pain and disability had limited ability to predict real-life physical performance in patients with lumbar spine stenosis.
This study is the first to our knowledge that is focused on patients undergoing lumbar spine surgery for pain, radiculopathy, or claudication. The physical activity parameters were very similar preoperatively versus the early postoperative phase (1-month follow-up), given that the patients were still recovering from their surgery and had reduced ambulation. However, beyond this temporal threshold, significant improvements in number of steps taken and distance traveled were seen at 2-month and 3-month follow-up. This result was also similarly reflected in the significant improvements in VAS back and leg pain scores, ODI, and physical component of SF-12. Similar to the study by Pryce et al,10 no correlation was found between clinical physical activity and functional clinical scores. Thus, these results provide evidence that subjective patient-based scores are not adequate to predict real-life physical activity at follow-up. This trend suggests that pain is not the only factor responsible for physical activity impairment following lumbar surgery, and thus, data based only on patient self-scores should be interpreted with caution.1 Rather, a holistic assessment of patient function and recovery following spinal surgery may be achieved with objective measurements, which can be obtained using accelerometers. Overall, the present results suggest that the use of accelerometers to measure physical activity parameters over follow-up is feasible in patients having spine surgery.
The use of objective physical activity measurements with the accelerometer may potentially help overcome several limitations of self-reported outcomes, including documenting inaccuracies, the prevalence of overreporting activity levels, and the lack of standardization across different publications as to which scoring system to use.11 12 In contrast to the relatively labor-intensive surveys and repetition at different follow-up periods, continuous accelerometer collection of data can be automated with inbuilt algorithms.8 13 14 However, objective physical activity measurements using accelerometers still require validation in a spine surgery population, which should be addressed in future prospective trials.
The introduction of accelerometer-based objective physical activity measurements provides a whole new platform for new research opportunities. Potential future studies may look to explore any differences between the different surgical approaches in terms of postoperative recovery physical activity. For example, objective physical activity measurements may have a potential role in the assessment of minimally invasive lumbar fusion surgery versus traditional open surgery, whereas the present studies in the literature based on self-scored clinical outcomes have been met with resistance and controversy. In addition, accelerometers may potentially be useful in planning and evaluating physical activity interventions as part of follow-up physiotherapy.
Strengths of the Study
This study is the first to evaluate physical activity in a spine surgery cohort using accelerometers. The strengths also include the prospective nature of the assessment and the relatively long-term evaluation of physical activity, with prior studies using only 7-day assessment.10 A high rate of compliance was found, demonstrating that the use of accelerometers for postoperative follow-up after lumbar spine surgery is feasible.
Limitations
The present study is constrained by several limitations. First, the prospective study cohort is heterogeneous, including patients with various procedures such as ALIF, diskectomy, and laminectomy. Given the relatively small number of patients in this cohort, subgroup and multivariate analysis to compare outcome differences between these procedures was not feasible.15 In addition, the indications for lumbar spine surgery were varied and included radiculopathy, claudication, and low back pain. Because of the small number of patients and the different pathologies surgically treated in multiple ways, we could not assess which pathology and which surgery would be best suited for this activity-measuring technique. Recent studies have also suggested differences in accuracies in various physical activity tracking technologies, with smartphone applications as a potential alternative for measuring objective measurements.16 Future prospective studies should investigate the long-term outcomes in terms of objective physical activity measurements and how they compare and correlate with long-term clinical outcome based on subjective rating scores. Future studies should also use a larger sample size and stratify outcomes according to surgery and indication.
Conclusions
This study is the first to examine the role of measuring objective physical activity and demonstrates high compliance and statistically significant improvement in patients having lumbar decompression and lumbar fusion. However, there was no significant correlation found between improvements in subjective clinical outcome scores with changes in physical activity measurements at follow-up. The limitations of the present study include its small sample size. The validity of objective physical activity measurements should be assessed in future larger, prospective studies.
Ethics Approval
South Eastern Sydney Local Health District, New South Wales, Australia (HREC 13/090). All participants provided written informed consent.
Footnotes
Disclosures Ralph J. Mobbs, Speakers' bureau: Stryker Spine, Synthes; Royalties: Stryker Spine; Stock/stock options: Medtronic, J&J; Meeting expenses: Orthotec Kevin Phan, none Monish Maharaj, none Prashanth J. Rao, none
References
- 1.Chapman J R Norvell D C Hermsmeyer J T et al. Evaluating common outcomes for measuring treatment success for chronic low back pain Spine (Phila Pa 1976) 201136(21, Suppl):S54–S68. [DOI] [PubMed] [Google Scholar]
- 2.DeVine J Norvell D C Ecker E et al. Evaluating the correlation and responsiveness of patient-reported pain with function and quality-of-life outcomes after spine surgery Spine (Phila Pa 1976) 201136(21, Suppl):S69–S74. [DOI] [PubMed] [Google Scholar]
- 3.Iversen M D, Katz J N. Examination findings and self-reported walking capacity in patients with lumbar spinal stenosis. Phys Ther. 2001;81(7):1296–1306. [PubMed] [Google Scholar]
- 4.Dunn A S, Passmore S R, Burke J, Chicoine D. A cross-sectional analysis of clinical outcomes following chiropractic care in veterans with and without post-traumatic stress disorder. Mil Med. 2009;174(6):578–583. doi: 10.7205/milmed-d-02-3508. [DOI] [PubMed] [Google Scholar]
- 5.Mobbs R J, Gollapudi P R, Chandran N K. Outcome following anterior cervical discectomy in compensation patients. J Clin Neurosci. 2001;8(2):124–125. doi: 10.1054/jocn.2000.0764. [DOI] [PubMed] [Google Scholar]
- 6.Gülbahar S, Berk H, Pehlivan E. et al. [The relationship between objective and subjective evaluation criteria in lumbar spinal stenosis] Acta Orthop Traumatol Turc. 2006;40(2):111–116. [PubMed] [Google Scholar]
- 7.Berlin J E, Storti K L, Brach J S. Using activity monitors to measure physical activity in free-living conditions. Phys Ther. 2006;86(8):1137–1145. [PubMed] [Google Scholar]
- 8.Bassett D R Jr, Cureton A L, Ainsworth B E. Measurement of daily walking distance-questionnaire versus pedometer. Med Sci Sports Exerc. 2000;32(5):1018–1023. doi: 10.1097/00005768-200005000-00021. [DOI] [PubMed] [Google Scholar]
- 9.Takacs J, Pollock C L, Guenther J R, Bahar M, Napier C, Hunt M A. Validation of the Fitbit One activity monitor device during treadmill walking. J Sci Med Sport. 2014;17(5):496–500. doi: 10.1016/j.jsams.2013.10.241. [DOI] [PubMed] [Google Scholar]
- 10.Pryce R, Johnson M, Goytan M, Passmore S, Berrington N, Kriellaars D. Relationship between ambulatory performance and self-rated disability in patients with lumbar spinal stenosis. Spine (Phila Pa 1976) 2012;37(15):1316–1323. doi: 10.1097/BRS.0b013e31824a8314. [DOI] [PubMed] [Google Scholar]
- 11.Noorkõiv M, Rodgers H, Price C I. Accelerometer measurement of upper extremity movement after stroke: a systematic review of clinical studies. J Neuroeng Rehabil. 2014;11:144. doi: 10.1186/1743-0003-11-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tudor-Locke C E, Myers A M. Challenges and opportunities for measuring physical activity in sedentary adults. Sports Med. 2001;31(2):91–100. doi: 10.2165/00007256-200131020-00002. [DOI] [PubMed] [Google Scholar]
- 13.Appelboom G, Yang A H, Christophe B R. et al. The promise of wearable activity sensors to define patient recovery. J Clin Neurosci. 2014;21(7):1089–1093. doi: 10.1016/j.jocn.2013.12.003. [DOI] [PubMed] [Google Scholar]
- 14.Culhane K M, Lyons G M, Hilton D, Grace P A, Lyons D. Long-term mobility monitoring of older adults using accelerometers in a clinical environment. Clin Rehabil. 2004;18(3):335–343. doi: 10.1191/0269215504cr734oa. [DOI] [PubMed] [Google Scholar]
- 15.Phan K, Tian D H, Cao C, Black D, Yan T D. Systematic review and meta-analysis: techniques and a guide for the academic surgeon. Ann Cardiothorac Surg. 2015;4(2):112–122. doi: 10.3978/j.issn.2225-319X.2015.02.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Case M A, Burwick H A, Volpp K G, Patel M S. Accuracy of smartphone applications and wearable devices for tracking physical activity data. JAMA. 2015;313(6):625–626. doi: 10.1001/jama.2014.17841. [DOI] [PubMed] [Google Scholar]


