Abstract
Background
The study of military-related mental health has been disproportionately focused on current symptomology rather than potentially more informative life course mental health. Indeed, no study has assessed age-of-onset and projected lifetime prevalence of disorders among reservists.
Methods
Age-of-onset and projected lifetime DSM-IV anxiety, mood, and substance use disorders were assessed in 671 Ohio Army National Guard soldiers aged 17–60 years. Between 2008 and 2012, face-to-face clinical assessments and surveys were conducted using the Structured Clinical Interview for DSM-IV and Clinician-Administered PTSD Scale.
Results
Lifetime prevalence of psychiatric disorders was 61%. Alcohol abuse/dependence (44%) and major depressive disorder (23%) were the most common disorders. The majority (64%) of participants reported disorders antedating enlistment. Median age-of-onset varied with anxiety disorders – particularly phobias and OCD – having the earliest (median = 15 years) and mood disorders the latest median age-of-onset (median = 21 years).
Limitations
The study was limited by both the retrospective investigation of age-of-onset and the location of our sample. As our sample may not represent the general military population, our findings need to be confirmed in additional samples.
Conclusions
Each psychiatric disorder exhibited a distinct age-of-onset pattern, such that phobias and OCD onset earliest, substance use disorders onset during a short interval from late-adolescence to early-adulthood, and mood disorders onset the latest. Our finding that the majority of participants reported disorders antedating enlistment suggests that an assessment of lifetime psychopathology is essential to understanding the mental health burden of both current and former military personnel.
Keywords: Military personnel, Age-of-onset, Psychiatric disorder, Military medicine
1. Introduction
It is estimated that nearly one in five United States (US) military service members are experiencing a psychiatric disorder at any given time (Riddle et al., 2007). While nearly all military studies ask questions of service members about their military experiences and beyond, much of the scientific writing in this area has omitted discussion of pre-military experiences and how they might shape “military mental health”. This potential set of omitted variables that might be of consequence here emerges readily from a life course perspective on the production of mental health.
Psychiatric epidemiology has been revolutionized by the development of a life course approach for examining physical and social exposure across the life span on adult disease risk (Koenen et al., 2014; Kuh et al., 2003). Just 4 decades ago psychiatric disorder age-of-onset was a controversial and uncertain topic (Rutter, 1972), while now we understand that the majority of psychiatric disorders first onset prior to age 15 (Kessler et al., 2007; Kim-Cohen et al., 2003). The importance of employing a life course perspective when examining psychiatric disorders among service members is hinted at in examples from recent literature. For example, Gallaway et al. (2013) documented that soldiers granted enlistment waivers for pre-military concerns (e.g., alcohol or drugs problems,) from 2003 to 2008 were significantly more likely to test positive for an illicit substance, be screened for admission to an alcohol/drug abuse program, and attrite from the Army for behavioral misconduct. Further, several studies have documented that about half of military suicides are among service members that have never deployed (LeardMann et al., 2013; Schoenbaum et al., 2014), that most of the suicidal behaviors during military service have had pre-enlistment onset (Nock et al., 2014), and that exposure to child abuse prior to military service is associated with suicidal behaviors during military service (Afifi et al., 2016). Nonetheless, military studies continue to primarily examine recent exposures, lending to the paucity of literature into life course factors among military personnel.
The focus on deployment experiences as the cause of psychiatric disorders among service members, rather than on the life course patterns of psychiatric disorders (e.g., pre-military psychiatric disorders, age-of-onset) that might be more central to the production of the health indicators of interest, has limited our understanding about the course of psychiatric disorders both prior to and during military service. Furthermore, understanding the life course patterns of mental illness among service members can change the narrative about the etiology of psychiatric disorders during military service, such that military experiences might be exacerbating earlier symptomology, rather than first incident disorders. However, our understanding of early life, pre-military, mental illness remains limited.
Mental illness is a major health concern in the US armed forces, particularly among the Reserves and National Guard (reserve component) (Cohen et al., 2015). Investigations to date have indicated that the reserve component suffers a greater burden of psychiatric disorders compared to the active component (Cohen et al., 2015; Iowa Persian Gulf Study Group, 1997; Milliken et al., 2007; Thomas et al., 2010). Prior to 2001, the National Guard had largely supported individual states during times of emergency; however, in the aftermath of the Vietnam War, the Total Force Policy was adopted to treat the 2 components (i.e., active-duty and reserve component) as a single operational force. As a result, during the height of mobilization in Operation Enduring Freedom and Operation Iraqi Freedom and (OEF/OIF) the reserve component forces constituted about 40% of deployed service members in combat operations. This reliance on the reserve component is not idiosyncratic to OEF/OIF; it is part of the Department of Defense's long-term strategic vision to increase the size, roles, and responsibilities of the reserve component moving forward (Department of Defense, 2011; Department of Defense, 2008). Nonetheless, there is a paucity of research addressing the mental health of reservists (Cohen et al., 2015).
In this study we used face-to-face clinical assessment using gold-standard instruments to document the age-of-onset and projected lifetime prevalence of psychiatric disorders in a representative sample of Ohio Army National Guard soldiers. Thus the first aim of this study was to investigate the lifetime prevalence and age-of-onset of DSM-IV psychiatric disorders using the Structured Clinical Interview for DSM-IV (SCID) and Clinician-Administered PTSD Scale (CAPS). The second aim was to use the lifetime prevalence of psychiatric disorders, and their respective age-of-onset, to determine the probability of disorder onset at each year of life from age 0–50 years. The third aim was to compare the psychiatric disorder age-of-onset to respondents' date of enlistment to determine the prevalence of disorders that onset prior to initiating military service. We hypothesized that substance use disorders and PTSD would be the most prevalent psychiatric disorders. Secondly, we expected substance use disorders to onset prior to military service, particularly during late-adolescents to early-adulthood (e.g., 16–24). Third, we expected PTSD, the sentinel trauma-related psychiatric disorder, to onset primarily after respondents enlisted into military service.
2. Methods
2.1. Participants
We used data from an in-depth clinical cohort study, nested within the Ohio Army National Guard (OHARNG) Mental Health Initiative (MHI). The OHARNG MHI is a representative longitudinal cohort study examining risk and resilience factors among OHARNG members (Calabrese et al., 2011). To examine the validity of the telephone survey mental health screening tools, we randomly selected 500 respondents from the baseline OHARNG MHI telephone survey sample. In addition, we randomly selected an additional 171 recently enlisted OHARNG to the clinical validation subsample in 2011 (n = 105) and 2012 (n = 171) to increase both the analytical power and provide data on the most recent cohort of OHARNG.
For the purpose of the current study, we used baseline data from the in-depth clinical cohort of the OHARNG MHI study. The clinical cohort was predominantly white (87%), male (87%), and single-never married (51%) (Table 1). The median age of the sample was 26 years (standard deviation: 9.6 years) and ranged from 17 to 60 years. In addition, most respondents were enlisted rank (E1–E9; 90%) and had deployed one or more times (55%). Overall, the clinical cohort was similar to the target population (i.e., Ohio National Guard service members) on all demographic and military characteristics.
Table 1.
Baseline characteristics of 671 Ohio Army National Guard study participants, 2008–2012.
| Variable | Study Participants (N=671) |
Ohio National Guard 2008 Profile (N=10,778) |
||
|---|---|---|---|---|
|
|
|
|||
| No. | % | No. | % | |
| Age, years | ||||
| 17–24 | 278 | 41.4 | 6430 | 39.1 |
| 25–34 | 221 | 32.9 | 5477 | 33.3 |
| 35–44 | 114 | 17.0 | 3361 | 20.5 |
| 45+ | 58 | 8.6 | 1166 | 7.1 |
| Sex | ||||
| Male | 586 | 87.3 | 14,239 | 86.6 |
| Female | 85 | 12.7 | 2195 | 13.4 |
| Race/ethnicity | ||||
| White | 586 | 87.3 | 9512 | 88.3 |
| African American | 48 | 7.2 | 1083 | 10.0 |
| Other | 36 | 5.4 | 183 | 1.7 |
| Missing | 1 | 0.2 | ||
| Marital status | ||||
| Single, never married | 345 | 51.4 | 5967 | 55.4 |
| Married | 265 | 39.5 | 4154 | 38.5 |
| Divorced/separated/ | 61 | 9.1 | 657 | 6.1 |
| widowed | ||||
| Rank | ||||
| Enlisted (E1–E9) | 603 | 89.6 | 9750 | 90.5 |
| Officer (W1–5/O1–10) | 68 | 10.1 | 1028 | 9.5 |
| Prior deployment | ||||
| Yes | 367 | 54.7 | 5863 | 54.4 |
| No | 304 | 45.3 | 4915 | 45.6 |
Note: E=enlisted; O=officer; W=warrant officer.
2.2. Procedures
Study trained clinicians completed face-to-face clinical interviews in private locations (e.g., private library room) with 671 participants from June 2008 to February 2012. Study staff performed monthly inter-rater reliability for the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and Clinician-Administered PTSD Scale (CAPS) to assure that the interviewers were standardized in their diagnostic assessment methods and interviewing techniques; results revealed moderate to excellent interrater agreement ( 4 0.9) and Free-Marginal Multirater Kappas ( 4 0.85). A comprehensive description of OHARNG Mental Health Initiative sampling strategy and recruitment has been previously published (Prescott et al., 2014). The study was approved by the local institutional review boards and written informed consent was obtained from all participants.
2.3. Measures
The diagnostic interview included both the CAPS (Blake et al., 2000) and the SCID (First et al., 2002, 1996). First, the CAPS was administered twice to assess both lifetime and current PTSD symptoms based on the individuals' self-selected “worst deployment related trauma” and then again for their “worst not related to deployment” (Breslau et al., 1998). Posttraumatic stress disorder diagnosis was based on DSM-IV criteria using the frequency Z 1 and intensity Z 2 methods (Blake et al., 2000), which is considered the gold standard for identifying PTSD cases for lifetime PTSD diagnosis (Weathers et al., 2001); compared to the SCID, the CAPS has been found to have a test-retest reliability (kappa) of 0.73, 84% sensitivity, and 90% specificity (Weathers et al., 2001). Respondents meeting diagnostic criteria on either the CAPS related to their worst deployment related traumatic event or the CAPS related to their worst non-deployment related traumatic event were classified as having PTSD.
The SCID was administered to assess Axis I disorders (First et al., 1996), which were then categorized into three overarching groups: anxiety disorder (panic disorder, agoraphobia without panic disorder, specific phobia, social phobia, obsessive-compulsive disorder (OCD)), mood disorders (major depressive disorder (MDD) and bipolar disorder I/II), and substance use disorders (SUD; alcohol and/or drug abuse or dependence). Total unique diagnoses were summed and categorized into a single interval variable representing comorbidity. All diagnoses were based on DSM-IV criteria and subthreshold disorders were not considered for this analysis. Previous reliability studies of the SCID have found that reliability estimates vary across the disorders, ranging from about 0.60 to 1.00 (Lobbestael et al., 2011; Zanarini et al., 2000).
Study clinicians using SCID guidelines determined retrospective age-of-onset. Assessing the reliability of self-reported age-of-onset, Farrer et al. (1989) found perfect agreement for age-of-onset in about 25-33% of persons with MDD and the highest test-retest reliability among persons 18–19 (r = .91) and 20–29 (r = .77). Likewise, Prusoff et al. (1988) documented similarly high correlation of self-reported age-of-onset among respondents diagnosed with MDD (r = .71) and panic disorder (r = .70), with moderate correlation among respondents diagnosed with phobic disorders (r = .58) and alcohol use disorder (r = .41).
Standard demographic and military characteristics were assessed, including: age, sex, race/ethnicity, marital status, rank, and lifetime deployment.
2.4. Statistical analysis
First, cumulative lifetime prevalence was estimated as the proportion of respondents who ever fulfilled DSM-IV diagnostic criteria for a given disorder for at least part of their lives up to their age at baseline interview.
Second, we performed a stratified analysis to assess the presence of a secular trend (i.e., cohort effect). This step was required because we accrued study participants over 4 years and the actuarial method assumes constant conditional risk of disease onset at a given year of life. Upon evidence that there was no secular trend across the cohorts, we assumed constant conditional risk and concatenated all baseline data.
Third, age-of-onset distributions and projected lifetime risk to age 50 years were estimated using the actuarial (life table) method (Halli and Rao, 1992; Rosner, 2006) executed in SAS 9.2 (Cary, NC). The actuarial method differs from the more familiar Kaplan and Meier (1958) method because it takes a time interval (e.g., 1-year) as its primary unit, while the Kaplan-Meier approach calculates the probability of each event at the time it occurs. Therefore, the actuarial method was better suited for our data as we only assessed the age at first diagnosis (i.e., 1-year interval) and not the exact date. The actuarial method calculates the cumulative incidence as the probability of an event in a given interval as the proportion of new events during that period of time, in which the denominator is the initial population corrected for losses. This measure corresponds to the interval-based probability of the event (Rosner, 2006). For this study, cumulative probability of event was estimated for 1-year intervals for 50 years with the probability estimated for every year of age.
3. Results
Lifetime prevalence and projected lifetime risk at age 50 of common mood, anxiety, and substance disorders is presented in Table 2. Overall, 61% of the sample met criteria for at least one lifetime disorder. Substance use disorders were the most prevalent diagnoses (47%), followed by mood (28%) and anxiety disorders (22%). Prevalence of the individual anxiety disorders were evenly distributed within the category with a difference of less that 4% between the least and most common diagnoses, agoraphobia without panic disorder (3%) and PTSD (6%), respectively. Conversely, MDD accounted for the preponderance of diagnosed mood disorders. Finally, comorbidity was substantial; specifically, about 30% of respondents met diagnostic criteria for two or more psychiatric disorders.
Table 2.
Lifetime prevalence and age-of-onset of DSM-IV disorders in Ohio Army National Guard study participants, 2008–2012 (N=671).
| Mental disorders | Prevalence | Age-of-onseta | ||
|---|---|---|---|---|
|
|
|
|||
| No. | % | Median | IQRb | |
| Anxiety disorders | ||||
| Panic disorder | 30 | 4.5 | 24.0 | 15.0 |
| Agoraphobia, without panic disorder | 20 | 3.0 | 19.5 | 14.0 |
| Specific phobia | 39 | 5.8 | 10.0 | 13.0 |
| Social phobia | 43 | 6.4 | 11.0 | 7.0 |
| Posttraumatic stress disorder | 42 | 6.3 | 20.0 | 11.0 |
| Obsessive compulsive disorder | 25 | 3.7 | 12.5 | 13.0 |
| Other anxiety disorder | 33 | 4.9 | 20.0 | 13.0 |
| Any anxiety disorder | 144 | 21.5 | 15.0 | 14.0 |
| 2+ Anxiety disorders | 41 | 6.1 | 13.0 | 15.5 |
| Mood disorders | ||||
| Major depressive disorder | 154 | 23.0 | 21.0 | 13.0 |
| Bipolar I/ II | 29 | 4.3 | 20.0 | 12.0 |
| Other mood disorders | 41 | 6.1 | 24.0 | 14.0 |
| Any mood disorder | 190 | 28.3 | 21.0 | 13.0 |
| 2+ Mood disorders | 12 | 1.8 | 20.0 | 13.5 |
| Substance use disorders | ||||
| Alcohol use disorderc | 293 | 43.7 | 20.0 | 4.0 |
| Drug use disorder | 91 | 13.6 | 16.0 | 4.0 |
| Any | 313 | 46.7 | 19.0 | 4.0 |
| Both alcohol and drug abuse | 71 | 10.6 | 16.5 | 2.5 |
| Aggregate mental disorders | ||||
| 0 | 259 | 38.6 | – | – |
| 1 | 204 | 30.4 | 19.0 | 4.0 |
| 2 | 115 | 17.1 | 17.0 | 5.0 |
| 3+ | 93 | 13.9 | 15.0 | 8.0 |
Note: IQR=inter-quartile range.
Retrospectively reported age-of-onset.
Inter-quartile range (IQR) is the range between then 25th and 75th percen-tiles on the age-of-onset distribution.
Includes abuse and dependence.
Age-of-onset distributions are presented in Table 3. Anxiety disorders (15 years) had an earlier median age-of-onset compared to substance use disorders (19 years) or mood disorders (21 years). There was noticeable variability in median age-of-onset within and between diagnosis categories. For example, within anxiety disorders, age-of-onset clustered within two groups; specific phobia, social phobia, and OCD had a median age-of-onset of 10–13 years, while agoraphobia without panic disorder, PTSD, panic disorder, and other anxiety disorders had a median age-of-onset of 19, 20, 20, and 24 years, respectively. Conversely, substance use disorders had similar median age-of-onsets (16–20 years) and narrow distributions (IQR 4 years). However, while substance abuse had similar means and IQRs, drug use/dependence predominately onset prior to 18 years (67%), compared to the majority of alcohol abuse/dependence that had first onsets between 18 and 24 years (74%). Finally, we observed an inverse association between the number of comorbid psychiatric disorders and age-of-onset, such that respondents who were diagnosed with a greater number of comorbid psychiatric disorders tended to report an earlier age of first disorder onset.
Table 3.
Median age-of-onset and distribution of DMS-IV mental disorders in a population-based study of the Ohio Army National Guard, 2008–2012 (N=671).
| Anxiety disorders | Mood disorders | Substance disorders | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| Panic disorder |
Agoraphobia, without panic disorder |
Specific phobia |
Social phobia |
Post-trau- matic stress disorder |
Obsessive compulsive disorder |
Other an- xiety disorder |
Major de- pressive disorder |
Bipolar I/II | Other mood disorder |
Alcohol use disorderc |
Drug use disorderc |
|
| Mediana | 24 (15) | 19 (14) | 10 (13) | 11 (7) | 20 (11) | 13 (13) | 20 (13) | 21 (13) | 20 (12) | 24 (14) | 20 (4) | 16 (4) |
| (IQR)b | ||||||||||||
| <18 | 12.0% | 44.4% | 70.0% | 95.1% | 35.9% | 68.2% | 38.1% | 33.6% | 39.1% | 26.7% | 12.1% | 66.7% |
| Years | ||||||||||||
| 18–24 | 44.0% | 22.2% | 26.7% | 2.4% | 38.5% | 18.2% | 28.6% | 32.1% | 30.4% | 40.0% | 74.1% | 31.2% |
| Years | ||||||||||||
| 25+ | 44.0% | 33.3% | 3.3% | 2.4% | 25.6% | 13.6% | 33.3% | 34.3% | 30.4% | 33.3% | 13.8% | 2.2% |
| Years | ||||||||||||
Retrospectively reported age-of-onset.
Inter-quartile range (IQR) is the range between then 25th and 75th percentiles on the age-of-onset distribution.
Includes abuse and dependence.
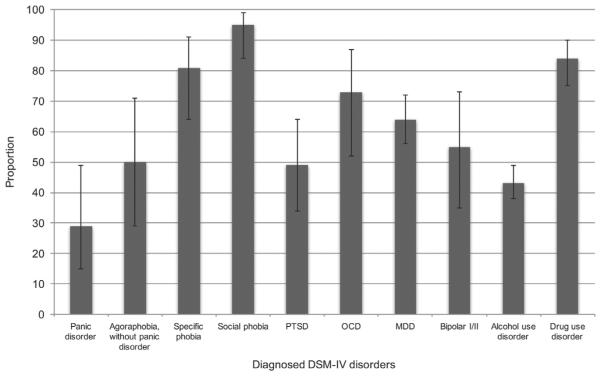
The proportion of disorders with age-of-onset prior to military service aligned well with median age-of-onset, where social phobia (95%), specific phobia (81%), and OCD (73%) had first onsets primarily prior to service (Fig. 1). Additionally, about half of bipolar I/II (52%), agoraphobia without panic (50%), and PTSD (49%) diagnoses had first onsets prior to service.
Fig. 1.
Proportion of diagnosed psychiatric disorders that had first onsets prior to military service in a representative study of the Ohio Army National Guard, 2008–2012. PTSD, posttraumatic stress disorder; OCD, obsessive-compulsive disorder; MDD, major depressive disorder.
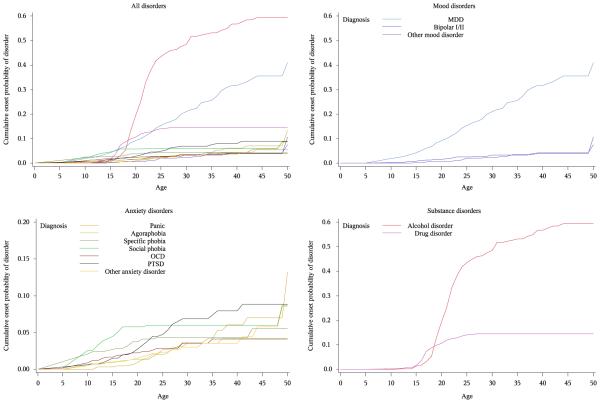
Fig. 2 presents cumulative onset probability of psychiatric disorders using the actuarial method. This figure supports Table 3 by showing variability in age-of-onset distributions of psychiatric disorders. For example, while mood disorders are predicted to occur at fairly regular intervals, following a linear trend (albeit with different slopes), substance use disorders are predicted to occur within a fairly small age interval (i.e., less variation around the mean age-of-onset) – aligning with the large IQR of anxiety and mood disorders (13–14 years), compared to substance use disorders (IQR = 4 years) documented in Table 3. Further, the lifetime prevalence of alcohol abuse/dependence (59.4%, 95% CI: 53.7, 65.1) and MDD (38.7%, 95%CI: 31.0, 47.5) is relatively higher than all other disorders, which cluster between about 4% and 15%.
Fig. 2.
Cumulative onset probability distributions of common psychiatric disorders within a representative sample of the Ohio Army National Guard service members (N = 671). The estimated cumulative onset probabilities were determined using the actuarial (life table) method. Note y-axis for anxiety disorder (lower-left quadrant) is 0.0–0.2; all other y-axis range from 0.0–0.6. Abbreviations: PTSD, posttraumatic stress disorder; OCD, obsessive-compulsive disorder; MDD, major depressive disorder.
4. Discussion
Using data from a representative sample of Ohio Army National Guard soldiers we found that 61% of reservists met diagnostic criteria for one or more psychiatric disorders at some time in their lives. Alcohol abuse/dependence and MDD were the most common individual disorders, whereas anxiety disorders were categorically less prevalent. Importantly, about half of participants reported that disorders onset prior to military service for several assessed psychiatric disorders, including: social phobia, specific phobia, drug abuse/dependence, OCD, PTSD, and bipolar I/II disorders.
We found that the majority of reservists reported disorders starting before military service. We are aware of only two previous studies that attempted to document age-of-onset of DSM-consistent disorders in a military population that may serve as a point of comparison (Gadermann et al., 2012; Kessler et al., 2014). Gadermann et al. (2012) restricted and weighted National Comorbidity Survey Replication (NCS-R) data based on Army socio-demographics to estimate MDD lifetime prevalence and age-of-onset for the U.S. Army. We found higher estimates of lifetime prevalence of MDD (41%) and lower proportion of pre-enlistment onset (47%) compared to Gadermann et al. (2012), who estimated 16% and 70% respectively. That we found higher estimates of lifetime MDD and lower proportion of pre-enlistment onset likely is a product of the Gadermann et al. (2012) study design, which weighted the NCS-R, a national survey of DSM-IV psychiatric disorders in the civilian U.S. household population, to match the sociodemographics of the U.S. Army. Because Gadermann et al. (2012) limited the NCS-R sample to persons meeting very strict military regulations (e.g., high school education/GED, no felony conviction, free from physical or severe psychiatric disorder), military regulations that the military later relaxed during OEF/OIF (Gallaway et al., 2013), their sample is likely to underestimate the true burden of lifetime disorders.
Kessler et al. (2014), using computer-administered questionnaires, estimated 30-day prevalence of DSM disorders and pre-enlistment age-of-onset in a nationally representative sample of active-duty US Army soldiers. We observed a higher prevalence of disorders, but more informative, a higher proportion of pre-enlistment disorders. For example, Kessler et al. (2014) documented 30% of PTSD had pre-military age-of-onset, compared to 49% in this study. That we observed a higher prevalence of both lifetime disorders and disorders with pre-enlistment age-of-onset compared to Kessler et al. (2014) can likely be attributed to differences in how our studies assessed symptomology. Specifically, Kessler et al. (2014) screened for 30-day prevalence of psychiatric disorders using fully structured, computer-administered, interviews, whereas our study clinicians employed “gold standard” structured clinical interviews to diagnose lifetime psychiatric disorders. Previous studies have documented that both civilians (Hardeveld et al., 2013) and military personnel (Fink et al., 2016) with mental disorders often cycle between stages of remission and recurrence. While our estimates of lifetime diagnosis may include those with remitted symptoms (over-estimating 30 day estimates), our study's inclusion of lifetime disorders is likely to provide improved estimates of the population's psychiatric burden compared to previously documented estimates.
Our observation that most soldiers reported that their psychiatric disorders onset prior to military service may explain recent studies that have observed little or no association between deployment and mental and substance use disorders among representative samples of service members (Cerda et al., 2014; Larson et al., 2008; LeardMann et al., 2013). For example, Larson et al. (2008) found that U.S. Marines are diagnosed more frequently during the initial months after enlistment rather than after combat deployment. A more recent study of Canadian military forces found that Afghanistan-related deployment contributed to about 9% of past-year psychiatric disorders, whereas child abuse contributed to about 29% of past-year disorders (Boulos and Zamorski, 2016). One explanation for a weaker association between military deployment and psychopathology is the “healthy warrior effect” (Larson et al., 2008; Wilson et al., 2009), which suggests that psychologically unfit personnel are identified early in training and only those service members proven resilient are then eligible for combat tours. In contrast to this literature emphasizing the contribution of pre-military experiences on military mental health, much extant literature has shown that deployment and combat exposures increase psychiatric symptomology and disorders (Hoge et al., 2004); however, many of these studies exclusively examined deployed service members with no comparison category (Cohen et al., 2015), which may have biased results away from the null. Our findings should not be taken to suggest that deployment and combat exposures are not associated with increased risk for psychiatric disorders, rather that analyses of data from only deployed service members may be oversimplifying a complex association between pre-military experiences and psychiatric symptomatology and recent traumatic event exposure.
The lifetime prevalence and predicted age-of-onset curves in our sample were comparable to previous studies in civilians. Specifically, psychiatric disorders predominately start in youth; with anxiety disorders having the earliest age-of-onset (Kessler et al., 2005) and mood disorders the latest. Anxiety disorders tend to fall into two distinct sets with phobias and OCD occurring earlier, whereas panic, agoraphobia, and PTSD onset later in life (Kessler et al., 2005). And in contrast to the earlier onset anxiety disorders that increase at an exponential rate during childhood, the later onset anxiety (i.e., panic, agoraphobia, PTSD) and mood disorders tend to increase in a roughly linear manner over the entire life course (Kessler et al., 2007, 2005). Moreover, our results are consistent with previous findings that SUDs commonly start during late adolescence and early adulthood in both military and nonmilitary populations (Ames and Cunradi, 2004; Kessler et al., 2007). One hypothesis proposes that the propensity to experiment with psychoactive substances during adolescence increases due to social pressure, but use is curbed during professional integration as a result of social constraints and work environments (Warner et al., 2011). This is particularly true in the military that has a zero tolerance policy towards illegal drugs, while service members perceive a relatively accepting culture towards alcohol use (Ames and Cunradi, 2004). Our results support this discrepancy in perceptions and policy as more than 80% of drug use disorders had first onsets prior to joining the military compared to more than 60% of the alcohol use disorders that onset after joining the military.
5. Limitations
This study is not without limitations. First, self-report data may result in the under-reporting of lifetime psychiatric disorders. While military personnel are likely to provide truthful answers if they believe a survey will be used for legitimate purposes and individual answers will remain confidential (Warner et al., 2011), the presence or perception of mental illness stigma (Kim et al., 2010) and a bias against reporting embarrassing behaviors (Cannell et al., 1977) remain prevalent in the military. We compensated for this concern by assuring participants that individual answers will remain confidential, both verbally and in writing, prior their volunteering for the study. Additionally, we improved confidentiality by having civilian clinicians conduct all assessments in neutral locations without the presence of military personnel.
Second, lifetime psychiatric disorder symptoms and age-of-onset were self-reported, which may lead to underestimates of the lifetime prevalence of psychiatric disorders (Takayanagi et al., 2014) and recall bias, respectively. In addition, we presented age-of-onset as a binary phenomenon; however, we must acknowledge that the onset of a disorder likely represents a gradual process of symptom development. Although study clinicians asked respondents to report the earliest age at which their symptoms seem to go together, representing a disorder over early subthres-hold symptomology, we cannot rule out the possibility that respondents might have incorrectly recalled the earliest age of disorder onset.
Third, the actuarial method used to estimate lifetime risk assumes that first onset of a disorder is conditionally uniformly distributed within a year of age (Rosner, 2006). While over half of the sample had previously deployed, which is associated with exposure to several traumatic events, the population did not all deploy during the same age interval. Therefore, it is reasonable to assume risk did not change rapidly within a given age interval for all members of the cohort. Additionally, our stratified analysis did not show any age-of-onset differences between birth cohorts. Fourth, the available sample size and number of cases did not allow an examination of stratified tables, such as comparing differences in age-of-onset among deployers and non-deployers. We acknowledge this is an important next step for future studies.
Finally, the sample was predominantly white male US National Guard personnel from the state of Ohio; therefore, the generalizability of our results is limited. Compared to the general US National Guard population, a larger proportion of our sample was younger (age 17–24: 41% v 31%) and never married (51% v 45%), whereas a similar proportion of our sample was male (87% v 85%) and enlisted rank (90% v 88%) (Fink et al., 2016). Although our findings were derived from a geographically defined sample and require replication in additional military samples, the similar age-of-onset patterns between our study and Army STARRS (Kessler et al., 2014) provide some confidence in the generalizability of our estimates.
6. Conclusions and implications
In summary, we documented a high prevalence of psychiatric disorders in this sample with about half of participants reporting pre-military disorder onset. These findings suggest that military leaders aiming to identify soldiers at risk of mental illness should expand current identification methods – assessing contemporary military and civilian stressors – to assess early life mental illness. The observation that a high proportion of participants reported that their psychiatric disorder onset prior to enlistment suggests the need for improved efforts to identify and support incoming soldiers with lifetime mental illness that may affect the potential consequences of traumatic exposure incurred during their military careers.
Acknowledgements
The informatics support for this research was provided by the Michigan State University Clinical and Translation Sciences Institute, through its Biomedical Research Informatics Core (BRIC)
References
- Afifi TO, Taillieu T, Zamorski MA, Turner S, Cheung K, Sareen J. Association of child abuse exposure with suicidal ideation, suicide plans, and suicide attempts in military personnel and the general population in Canada. JAMA Psychiatry. 2016;73:229–238. doi: 10.1001/jamapsychiatry.2015.2732. [DOI] [PubMed] [Google Scholar]
- Ames G, Cunradi C. Alcohol use and preventing alcohol-related problems among young adults in the military. Alcohol Res. Health. 2004;28:252–257. [Google Scholar]
- Blake D, Weathers FW, Nagy L, Kaloupek D, Klauminzer G, Charney D, Keane TM, Buckley TC. National Center for Postraumatic Stress Disorder, Behavioral Science Division. Boston, MA: 2000. Instruction Manual: Clinician-Administered PTSD Scale. [Google Scholar]
- Boulos D, Zamorski MA. Contribution of the mission in Afghanistan to the burden of past-year mental disorders in Canadian armed forces personnel, 2013. Can. J. Psychiatry. 2016;61:64S–76S. doi: 10.1177/0706743716628857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of trauma. Arch. Gen. Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Calabrese JR, Prescott M, Tamburrino M, Liberzon I, Slembarski R, Goldmann E, Shirley E, Fine T, Goto T, Wilson K, Ganocy S, Chan P, Serrano MB, Sizemore J, Galea S. PTSD comorbidity and suicidal ideation associated with PTSD within the Ohio Army National Guard. J. Clin. Psychiatry. 2011;72:1072–1078. doi: 10.4088/JCP.11m06956. [DOI] [PubMed] [Google Scholar]
- Cannell CF, Marquis KH, Laurent A. A summary of studies of interviewing methodology. Vital and health statistics. Series 2. Data evaluation and methods research. 1977:1–78. i–viii. [PubMed] [Google Scholar]
- Cerda M, Richards C, Cohen GH, Calabrese JR, Liberzon I, Tamburrino M, Galea S, Koenen KC. Civilian stressors associated with alcohol use disorders in the national guard. Am. J. Prev. Med. 2014;47:461–466. doi: 10.1016/j.amepre.2014.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen GH, Fink DS, Sampson L, Galea S. Mental health among reserve component military service members and veterans. Epidemiol. Rev. 2015:37. doi: 10.1093/epirev/mxu007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Defense . Title 10: United States Code Armed Forces. US Government Printing Office; Washington, DC: 2011. [Google Scholar]
- Department of Defense . Directive 1200.17. Government Printing Office; Washington, DC: 2008. [Google Scholar]
- Department of D.S. Fink GH, Cohen LA, Sampson RK, Gifford CS, Fullerton RJ, Ursano S, Galea Incidence of and risk for post-traumatic stress disorder and depression in a representative sample of US Reserve and National Guard. Annals of Epi. 2016;2016;26:189–197. doi: 10.1016/j.annepidem.2016.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrer LA, Florio LP, Bruce ML, Leaf PJ, Weissman MM. Reliability of self-reported age at onset of major depression. Journal of Psychiatric Research. 1989;23:35–47. doi: 10.1016/0022-3956(89)90015-0. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams DR. User's guide for the structure clinical interview for DSM-IV-TR Axis I disorders. Biometrics Research; New York, NY: 2002. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JB. Structured Clinical Interview for Axis I DSM-IV Disorders – Patient Edition. Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Gadermann AM, Engel CC, Naifeh JA, Nock MK, Petukhova M, Santiago PN, Wu B, Zaslavsky AM, Kessler RC. Prevalence of DSM-IV major depression among U.S. military personnel: meta-analysis and simulation. Mil. Med. 2012;177:47–59. doi: 10.7205/milmed-d-12-00103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallaway MS, Bell MR, Lagana-Riordan C, Fink DS, Meyer CE, Millikan AM. The association between US Army enlistment waivers and subsequent behavioral and social health outcomes and attrition from service. Mil. Med. 2013;178:261–266. doi: 10.7205/MILMED-D-12-00316. [DOI] [PubMed] [Google Scholar]
- Halli S, Rao K. Advanced Techniques of Population Analysis. Plenum; New York, NY: 1992. [Google Scholar]
- Hardeveld F, Spijker J, De Graaf R, Nolen WA, Beekman AT. Recurrence of major depressive disorder and its predictors in the general population: results from the Netherlands Mental Health Survey and Incidence Study (NEM-ESIS) Psychol. Med. 2013;43:39–48. doi: 10.1017/S0033291712002395. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems and barriers to care. N. Engl. J. Med. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Iowa Persian Gulf Study Group Self-reported illness and health status among Gulf War veterans. JAMA: J. Am. Med. Assoc. 1997;277:238–245. [PubMed] [Google Scholar]
- Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J. Am. Stat. Assoc. 1958;53:457–481. [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Amminger GP, Arguilar-Gaxiola S, Alonso J, Lee S, Ustun TB. Age of onset of mental disorders: a review of recent literature. Curr. Opin. Psychiatry. 2007;20:359–364. doi: 10.1097/YCO.0b013e32816ebc8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Heeringa SG, Stein MB, Colpe LJ, Fullerton CS, Hwang I, Naifeh JA, Nock MK, Petukhova M, Sampson NA, Schoenbaum M, Zaslavsky AM, Ursano RJ, S.C. for the Army Thirty-day prevalence of DSM-IV mental disorders among nondeployed soldiers in the US army: results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS) JAMA Psychiatry. 2014 doi: 10.1001/jamapsychiatry.2014.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim PY, Thomas JL, Wilk JE, Castro CA, Hoge CW. Stigma, barriers to care, and use of mental health services among active duty and National Guard soldiers after combat. Psychiatr. Serv. 2010;61:582–588. doi: 10.1176/ps.2010.61.6.582. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder: developmental followback of a prospective-longitudinal cohort. Arch. Gen. Psychiatry. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- Koenen KC, Rudenstine S, Susser E, Galea S. A Life Course Approach to Mental Disorders. Oxford University Press; Oxford, UK: 2014. [Google Scholar]
- Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Life course epidemiology. J. Epidemiol. Community Health. 2003;57:778–783. doi: 10.1136/jech.57.10.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson GE, Highfill-McRoy RM, Booth-Kewley S. Psychiatric diagnoses in historic and contemporary military cohorts: combat deployment and the healthy warrior effect. Am. J. Epidemiol. 2008;167:1269–1276. doi: 10.1093/aje/kwn084. [DOI] [PubMed] [Google Scholar]
- LeardMann CA, Powell TM, Smith TC, Bell MR, Smith B, Boyko EJ, Hooper TI, Gackstetter GD, Ghamsary M, Hoge CW. Risk factors associated with suicide in current and former US military personnel. JAMA. 2013;310:496–506. doi: 10.1001/jama.2013.65164. [DOI] [PubMed] [Google Scholar]
- Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the structured clinical interview for DSM-IV axis I disorders (SCID I) and axis II disorders (SCID II) Clin. Psychol. Psychother. 2011;18:75–79. doi: 10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA: J. Am. Med. Assoc. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Nock MK, Stein MB, Heeringa SG, Ursano RJ, Colpe LJ, Fullerton CS, Hwang I, Naifeh JA, Sampson NA, Schoenbaum M, Zaslavsky AM, Kessler RC, S.C. for the Army Prevalence and correlates of suicidal behavior among soldiers: results from the army study to assess risk and resilience in service-members (Army STARRS) JAMA Psychiatry. 2014 doi: 10.1001/jamapsychiatry.2014.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prescott MR, Tamburrino M, Calabrese JR, Liberzon I, Slembarski R, Shirley E, Fine T, Goto T, Wilson K, Ganocy S, Chan P, Derus A, Serrano MB, Sizemore J, Kauffman J, Galea S. Validation of lay-administered mental health assessments in a large Army National Guard cohort. Int. J. Methods Psychiatr. Res. 2014;23:109–119. doi: 10.1002/mpr.1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prusoff BA, Merkangas KR, Weissman MM. Lifetime prevalence of psychiatric disorders: Recall 4 years later. J. Psych. Res. 1988;22:107–117. doi: 10.1016/0022-3956(88)90075-1. [DOI] [PubMed] [Google Scholar]
- Riddle JR, Smith TC, Smith B, Corbeil TE, Engel CC, Wells TS, Hoge CW, Adkins J, Zamorski M, Blazer D, T. Millennium Cohort Study Millennium Cohort: the 2001–2003 baseline prevalence of mental disorders in the U. S. military. J. Clin. Epidemiol. 2007;60:192–201. doi: 10.1016/j.jclinepi.2006.04.008. [DOI] [PubMed] [Google Scholar]
- Rosner B. Fundamentals of Biostatistics. Duxbury; Belmont, CA: 2006. [Google Scholar]
- Rutter ML. Relationships between child and adult psychiatric disorders. Some research considerations. Acta Psychiatr. Scand. 1972;48:3–21. doi: 10.1111/j.1600-0447.1972.tb04346.x. [DOI] [PubMed] [Google Scholar]
- Schoenbaum M, Kessler RC, Gilman SE, Colpe LJ, Heeringa SG, Stein MB, Ursano RJ, Cox KL, S.C. for the Army Predictors of suicide and accident death in the army study to assess risk and resilience in servicemembers (Army STARRS): results from the army study to assess risk and resilience in service-members (Army STARRS) JAMA Psychiatry. 2014 doi: 10.1001/jamapsychiatry.2013.4417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenbaum M, Kessler RC, Gilman SE, Colpe LJ, Heeringa SG, Stein MB, Ursano RJ, Cox KL, S.C. for the Army Predictors of suicide and accident death in the army study to assess risk and resilience in servicemembers (Army STARRS): results from the army study to assess risk and resilience in service-members (Army STARRS) JAMA Psychiatry. 2014 doi: 10.1001/jamapsychiatry.2013.4417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, Hoge CW. Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Arch. Gen. Psychiatry. 2010;67:614–623. doi: 10.1001/archgenpsychiatry.2010.54. [DOI] [PubMed] [Google Scholar]
- Warner CH, Appenzeller GN, Grieger T, Belenkiy S, Breitbach J, Parker J, Warner CM, Hoge C. Importance of anonymity to encourage honest reporting in mental health screening after combat deployment. Arch. Gen. Psychiatry. 2011;68:1065–1071. doi: 10.1001/archgenpsychiatry.2011.112. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: a review of the first ten years of research. Depress Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Wilson J, Jones M, Fear NT, Hull L, Hotopf M, Wessely S, Rona RJ. Is previous psychological health associated with the likelihood of Iraq war deployment? An investigation of the “healthy warrior effect”. Am. J. Epidemiol. 2009;169:1362–1369. doi: 10.1093/aje/kwp044. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Skodol AE, Bender D, Dolan R, Sanislow C, Schaefer E, Morey LC, Grilo CM, Shea MT, McGlashan TH, Gunderson JG. The collaborative longitudinal personality disorders study: reliability of axis I and II diagnoses. J. Personal. Disord. 2000;14:291–299. doi: 10.1521/pedi.2000.14.4.291. [DOI] [PubMed] [Google Scholar]