Abstract
Purpose of review
Melatonin is a neuroendocrine hormone synthesized primarily by the pineal gland. Numerous studies have suggested that melatonin plays an important role in various cardiovascular diseases. In this article, recent progress regarding melatonin's effects on cardiovascular diseases is reviewed.
Recent findings
In the past year, studies have focused on the mechanism of protection of melatonin on cardiovascular diseases, including myocardial ischemia-reperfusion injury, myocardial hypoxia-reoxygenation injury, pulmonary hypertension, hypertension, atherosclerosis, valvular heart diseases, and other cardiovascular diseases.
Summary
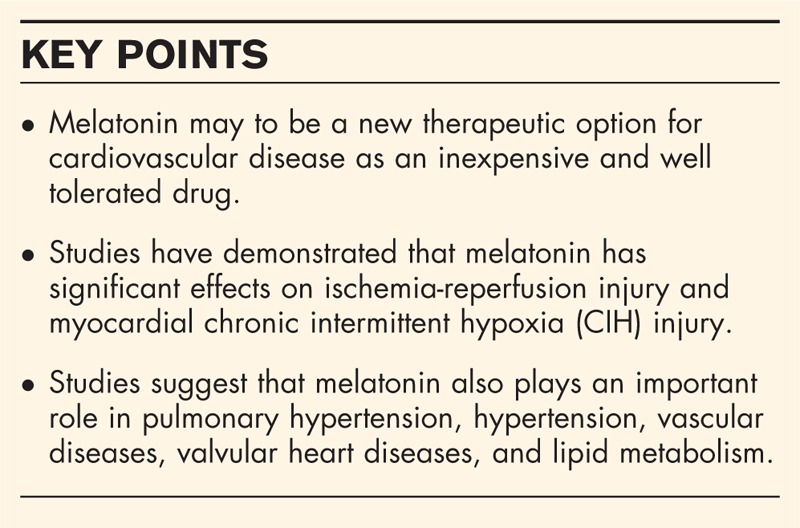
Studies have demonstrated that melatonin has significant effects on ischemia-reperfusion injury, myocardial chronic intermittent hypoxia injury, pulmonary hypertension, hypertension, valvular heart diseases, vascular diseases, and lipid metabolism. As an inexpensive and well tolerated drug, melatonin may be a new therapeutic option for cardiovascular disease.
Keywords: cardiovascular diseases, melatonin, myocardial ischemia-reperfusion injury
INTRODUCTION
Melatonin (N-acetyl-5-methoxytryptamine) is a neuroendocrine hormone, which is synthesized primarily by the pineal gland [1]. The synthesis and secretion of melatonin are regulated by light intensity [2]. It was found that melatonin functions to regulate the sleep cycle in the early study [3]. Further investigation revealed that melatonin also has antioxidant and anti-inflammatory functions [4]. It has also been shown to regulate lipid and glucose metabolism [5,6]. Importantly, recent research suggests that melatonin plays an important role in various cardiovascular diseases, including myocardial ischemia-reperfusion injury [7,8], atherosclerosis [9,10], hypertension [11,12], heart failure [13,14], and drug-induced myocardial injury [15,16]. In the past year, several studies have focused on the mechanism of the protection of melatonin on cardiovascular diseases. In this article, we review the recent progress in the understanding of melatonin's effects on cardiovascular disease.
Box 1.
no caption available
MELATONIN AND MYOCARDIAL ISCHEMIA-REPERFUSION INJURY
Melatonin confers profound protective effects against ischemia-reperfusion injury in various organs, including the heart [7,8], liver [17], and kidney [18]. However, the mechanisms by which it affords protection remain incompletely understood. Ghaeli et al.[19] reported that in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention, administration of melatonin plus standard treatment significantly reduced the level of creatine kinase-MB compared with the control group, receiving only standard therapy. However, in a porcine closed-chest reperfusion infarct model, intracoronary or intravenous melatonin administration did not reduce myocardial reperfusion injury [20]. The lack of effect may be because of the ineffective dose and route of administration. It was found that melatonin may protect against ischemia-reperfusion injury by activating silent information regulator 1 (SIRT1) signaling in a receptor-dependent manner [21]. Another study found that melatonin could protect adipose-derived mesenchymal stem cells (ADSCs) against hypoxia/serum deprivation injury by modulating the SIRT1 signaling pathway. Melatonin treatment also reduced the expression of the apoptotic proteins acetylated forkhead box protein O1 (Ac-Fox01), acetylated p53 (Ac-p53), acetylated nuclear factor kappa-light-chain-enhancer of activated B cells (Ac-NF-kB), and B-cell lymphoma 2 (BCL2)-associated X protein (BAX), while increasing the expression of the antiapoptotic protein B-cell lymphoma 2 (BCL-2) [22▪]. Similarly, melatonin improved the survival and function of ADSCs in a rat model of myocardial infarction [23]. Its protective effects were due to increased expression of Cu/Zn superoxide dismutase (SOD-1) and other antioxidant enzymes, basic fibroblast growth factor, insulin-like growth factor 1, epidermal growth factor, and hepatocyte growth factor. Melatonin also protected mesenchymal stem cells (MSCs) against reactive oxygen species (ROS)-induced apoptosis by stimulating phosphorylated protein kinase B (p-Akt) and inhibiting activation of the caspase cascade [23]. Yu et al.[24] studied the effect and mechanism of melatonin on myocardial ischemia-reperfusion (MI/R) by modulating Notch1/Hairy and enhancer of split 1 (Hes1) and phosphatase and tensin homolog (PTEN)/Akt signaling pathways. In an in-vivo study, prophylactic use of melatonin before myocardial ischemia-reperfusion surgery significantly improved cardiac function, reduced oxidative damage, and decreased myocardial apoptosis [24]. In an in-vitro study of H9C2 cardiomyocytes, melatonin treatment increased Notch1, Notch1 intracellular domain, BCL-2, and Hes1 expression and the ratio of phosphorylated to unphosphorylated Akt, while reducing caspase-3, PTEN, and BAX expression [24]. Another study showed that melatonin significantly inhibited myocardial apoptosis during myocardial ischemia-reperfusion in rats [25]. Melatonin also preserves the structural integrity of mitochondria in myocardiocytes, promoting adenosine triphosphate synthesis and preserving cardiac function [25]. In a rat model of ischemia/reperfusion injury, administration of melatonin reduced infarct size by inhibiting the mitochondrial permeability transition pore [26]. In a model of diet-induced obesity utilizing Wistar rats, melatonin treatment reduced serum insulin levels, homeostatic model assessment index and myocardial infarct volume, while increasing serum adiponectin levels and activating baseline myocardial extracellular signal-regulated kinases 42/44 (ERK 42/44), glycogen synthase kinase-3 beta (GSK-3 β), signal transducer and activator of transcription 3 (STAT-3), and Protein Kinase B (PKB/Akt) during reperfusion [27]. In another rat model of high-fat diet-fed streptozotocin induced diabetes [28▪], treatment with melatonin suppressed protein kinase ribonucleic acid-like endoplasmic reticulum kinase (PERK)/eukaryotic initiation factor 2 alpha kinase/activating transcription factor 4 (ATF4) signaling, reduced myocardial oxidative damage, and up-regulated SIRT1 expression. Endoplasmic reticulum stress is considered to be an important contributing factor in cardiovascular diseases [29]. Melatonin was also found to modulate endoplasmic reticulum stress by suppressing PERK/eIF2α/ATF4 signaling after ischemia reperfusion in H9C2 cardiomyocytes [28▪]. A recent study also implicated Toll-like receptor 4 (TLR4) signaling in the protective effects of melatonin [30▪]. In isolated hearts, melatonin treatment was shown to protect against ischemia/reperfusion injury through increased TLR4 signaling and also increased mitochondrial STAT-3 expression, leading to subsequent activation of the survivor activating enhancement pathway [30▪].
MELATONIN AND MYOCARDIAL CHRONIC INTERMITTENT HYPOXIC INJURY
Obstructive sleep apnea is associated with CIH and increases myocardial injury contributing to ischemic heart disease [31]. Yeung et al.[32▪] reported that melatonin protected against CIH-induced myocardial inflammation, fibrosis, and ischemia-reperfusion injury. In this study, treatment with melatonin significantly reduced the expression of inflammatory cytokines [tumor necrosis factor-α (TNF-α) and IL-6] and markers of fibrosis [PC1 and transforming growth factor β (TGFβ)]. Furthermore, melatonin treatment decreased infarct size in isolated hearts with regional ischemia reperfusion by mitigating sarcoplasmic reticulum calcium (2+) [SR-Ca(2+)] homeostasis in cardiomyocytes and reducing the expression of nicotinamide adenine dinucleotide phosphate oxidase (p22 and NOX2) and antioxidant enzymes [catalase (CAT) and manganese-superoxide dismutase (MnSOD)]. Xie et al.[33] reported that melatonin decreased CIH-induced myocardial hypertrophy and cardiomyocyte apoptosis by modulating the adenosine monophosphate-activated protein kinase pathway and autophagy-regulated apoptosis. Using a melatonin receptor agonist, Neu-p11, Yu et al.[34] demonstrated that downstream signaling protected myocardial cells from hypoxia-reoxygenation injury. Administration of Neu-p11 reduced cardiomyocyte apoptosis and also significantly decreased levels of creatine kinase, lactate dehydrogenase (LDH), and methane dicarboxylic aldehyde. Cardiovascular diseases have been associated with mitochondrial dysfunction [35]. Importantly, Neu-p11 also protected mitochondria from ischemia-reperfusion-mediated injury and modulated lipid peroxidation. Ortiz et al.[36] found that melatonin treatment inhibited iNOS/i-mtNOS (iNOS, inducible nitric oxide synthase; i-mtNOS, inducible mitochondrial nitric oxide synthase) induction, restored myocardial mitochondrial homeostasis and preserved the activity of nNOS/c-mtNOS (nNOS, neuronal nitric oxide synthase; c-mtNOS, constitutive mitochondrial nitric oxide synthase). Additionally, a study using chick embryos showed that melatonin (1 mg/kg/day) rescued hypoxia-induced cardiovascular dysfunction [37].
MELATONIN AND PULMONARY HYPERTENSION
Pulmonary hypertension is a disease characterized by elevated pulmonary arterial pressure, which leads to right ventricular hypertrophy and failure [38]. Maarman et al.[39] reported that treatment with melatonin alleviated right ventricular hypertrophy and dysfunction, and also reduced interstitial fibrosis and plasma oxidative stress in a rat model of pulmonary hypertension. Torres et al.[40] found that melatonin reduced pulmonary artery pressure and resistance and improved vasodilation of small pulmonary arteries in newborn sheep with pulmonary hypertension. In addition, melatonin increased nitric oxide bioavailability and reduced markers of pulmonary oxidative stress. Jin et al.[41▪] reported that melatonin attenuated hypoxic pulmonary hypertension. Chronic hypoxia elevates the ratio of the weights of the right ventricle to left ventricle plus intraventricular septum (RV/LV+S), right ventricular systolic pressures (RVSP), and median width of pulmonary arterioles. Treatment with melatonin reduced the elevation of RV/LV+S and RVSP and also inhibited pulmonary vascular remodeling. Additionally, melatonin reduced levels of hypoxia-inducible factor-1α, proliferating cell nuclear antigen, and nuclear factor-κB (NF-κB). In an in-vitro study, it was found that melatonin inhibited the proliferation of pulmonary artery smooth myocytes and reduced the expression of extracellular signal-regulated kinases1/2 (ERK1/2) and phosphorylation of Akt.
MELATONIN AND HYPERTENSION
Several studies have demonstrated that melatonin has an antihypertensive effect [42,43]. Simko et al.[44] found that melatonin alleviated hypertension is induced by continuous light exposure (24 h/day). Continuous light leads to hypertension, increased oxidative stress in the left ventricle and aorta, left ventricle hypertrophy, and left ventricle fibrosis. Melatonin treatment alleviated these pathological changes. İlhan et al.[45] also reported that melatonin alleviated 2,3,7,8-tetrachlorodibenzo-p-dioxin-induced hypertension by decreasing renal oxidative stress and vascular reactivity. A recently published review has confirmed the blood pressure (BP) lowering effects of melatonin [46]. It was shown that patients treated with melatonin (2–5 mg/day for 7–90 days) had a decrease in nocturnal SBP as well as DBP [46]. Additionally, it was demonstrated that the effect of melatonin on decreasing BP were most pronounced from 3:00 am to 8:00 am [47].
MELATONIN AND VASCULAR DISEASES
Recent studies have shown that melatonin is associated with atherosclerosis [48,49]. Cheng et al.[50] reported that melatonin reduced the number and area of atheromatous plaques in a rabbit model of atherosclerosis by modulating mitogen-activated protein kinase (MAPK) pathway signal transduction. In addition to MAPK signaling, a recent study showed that melatonin decreased aortic endothelial permeability and atherosclerosis in a mouse model of diabetes by decreasing the expression of myosin light chain kinase (MLCK), myosin phosphatase-targeting subunit phosphorylation, and myosin light-chain phosphorylation. Melatonin also decreased upstream expression of extracellular signal-related kinase (ERK) and p38 [51]. Zhu et al.[52] found that micro ribonucleic acid-29b (miR-29b) promotes endothelial permeability and apoptosis in high-fat diet-fed apoE knock-out mice by down-regulating the expression of MT1, which is a melatonin receptor. Yang et al.[53] reported that the anti-inflammatory effects of melatonin improved cigarette smoke-induced restenosis in rat carotid arteries after balloon injury. Melatonin may improve vascular dysfunction by affecting epigenetic regulation. In mice generated with assisted reproductive technologies, treatment with melatonin resulted in decreased arterial hypertension, which was thought to be due to its effects on normalizing nitric oxide levels by preventing impaired methylation of endothelial nitric oxide synthase [54]. It was also shown that melatonin may improve macrovascular and microvascular diseases [55–58]. Melatonin administration to high-fat diet and streptozotocin-induced diabetic rats restored endothelial function and vascular responses [59].
MELATONIN AND VALVULAR HEART DISEASE
It has been demonstrated that melatonin reduces flow shear stress-induced bone marrow mesenchymal stem cells injury by acting on melatonin receptors and the adenosine monophosphate-activated protein kinase/acetyl-CoA carboxylase signaling pathway [60▪]. In this study, melatonin reduced the expression of caspase 3, p53 upregulated modulator of apoptosis, and BAX, while inducing the expression of basic fibroblast growth factor, TGFβ, vascular endothelial growth factor, (BCL-2), and platelet-derived growth factor [60▪]. These findings suggest that targeting melatonin relating signaling in tissue-engineered heart valves may be an effective strategy in treating valvular heart disease.
MELATONIN AND LIPID METABOLISM
Early experiments showed that treatment with melatonin can improve dyslipidemia [4]. In patients with nonalcoholic fatty liver disease, treatment with melatonin (2 × 5 mg/day) for 14 months significantly reduced levels of triglycerides and LDL cholesterol (LDL-C) compared with controls treated with Essentiale [61]. Treatment with melatonin for 2 weeks significantly reduced free fatty acids compared with placebo in cigarette smokers [62]. A study on aluminum-induced toxicity in a rat model found that melatonin protected against toxic dyslipidemia by alleviating the aluminum induced increase in total cholesterol, LDL-C, triglycerides, oxidized LDL and apolipoprotein B100 [63]. In unpublished results, we have demonstrated that melatonin administration can improve lipid metabolism and reduce weight. Melatonin treatment reduced body weight, body fat, and waist circumference in obese patients with acanthosis nigricans. We also found that melatonin could decrease LDL and body weight in high-fat diet-induced nonalcoholic fatty liver disease mice. Dyslipidemia is an important risk factor of cardiovascular diseases [64], and melatonin's beneficial effects on lipid metabolism may reduce the incidence of cardiovascular diseases.
CONCLUSION
In conclusion, studies have demonstrated that melatonin has significant effects on ischemia-reperfusion injury, myocardial CIH injury, pulmonary hypertension, hypertension, vascular diseases, valvular heart diseases, and lipid metabolism (Table 1). As an inexpensive and well tolerated drug, melatonin may be a new therapeutic option for cardiovascular disease.
Table 1.
The effects of melatonin on various cardiovascular diseases
| Function | Factor/pathway/action | References |
| Melatonin and myocardial ischemia-reperfusion injury | ||
| Induce/activate | SIRT1 | [21,22▪,28▪] |
| NOTCH1, NICD, HES1, p-Akt/Akt ratio | [24] | |
| BCL-2, | [22▪,24] | |
| SOD-1, HFG | [23] | |
| Adiponectin, ERK42/44, GSK-3β, STAT-3, PKB/Akt | [27] | |
| TLR4, STAT3, SAFE | [30▪] | |
| Reduce/inhibit | CK-MB | [19] |
| BAX | [21,22▪] | |
| Ac-FoxO1, Ac-p53, Ac-NF-κB | [22▪] | |
| Caspase, ROS | [23] | |
| Caspase-3, PTEN, | [24] | |
| Serum insulin, HOMA index | [27] | |
| PERK/eIF2α/ATF4 signaling pathway | [28▪] | |
| Melatonin and myocardial chronic intermittent hypoxia injury | ||
| Reduce/inhibit | TNF-α, IL-6, COX-2; PC1, TGF-β; P22, NOX2; CAT, MnSOD | [32▪] |
| CK, LDH, MDA | [35] | |
| iNOS/i-mtNOS, nNOS/c-mtNOS | [36] | |
| Melatonin and pulmonary hypertension | ||
| Induce/activate | Nitric oxide | [41▪] |
| Reduce/inhibit | RV hypertrophy and dysfunction, interstitial fibrosis | [39] |
| Pulmonary artery pressure and resistance | [40] | |
| RV/LV+S, RVSP, HIF-1α, PCNA, NF-κb, ERK1/2, p-Akt | [41▪] | |
| Melatonin and hypertension | ||
| Reduce/inhibit | Oxidative load in the LV, aorta and LV hypertrophy, LV fibrosis | [44] |
| Renal oxidative stress and vascular reactivity | [45] | |
| Melatonin and vascular diseases | ||
| Reduce/inhibit | Number and areas of atheromatous plaques | [50] |
| MLCK, p-MYPT, p-MLC, ERK, p-38 | [51] | |
| eNOS | [54] | |
| Melatonin and valvular heart disease | ||
| Induce/activate | bFGF, BCL-2, PDGF | [60▪] |
| Reduce/inhibit | Caspase 3, PUMA, BAX | [60▪] |
| Melatonin and lipid metabolism | ||
| Reduce/inhibit | TG, LDL-C | [61,63] |
| FFA | [62] | |
| TC, oxidized LDL-C, apoB100 | [63] | |
Ac-FoxO1, acetylated forkhead box protein O1; Ac-p53,acetylated p53; Ac-NF-κB, acetylated nuclear factor kappa-light-chain-enhancer of activated B cells; ATF4, activating transcription factor 4; BCL-2, B-cell lymphoma 2; CAT, catalase; ERK42/44, extracellular signal-regulated kinases 42/44; GSK-3 β, glycogen synthase kinase-3 beta; LDH, lactate dehydrogenase; MnSOD, manganese-superoxide dismutase; p-Akt, phosphorylated protein kinase B; PKB, Protein Kinase B; PERK, protein kinase ribonucleic acid-like endoplasmic reticulum kinase; SIRT1, silent information regulator 1; TNF-α: tumor necrosis factor-α; bFGF, basic fibroblast growth factor; CK-MB, creatine kinase-MB; HIF-1α, hypoxia-inducible factor-1α; NICD, NOTCH1 intracellular domain; PCNA, proliferating cell nuclear antigen; PUMA, p53 upregulated modulator of apoptosis; PDGF, platelet-derived growth factor; RV/LV+S, right ventricle to left ventricle plus intraventricular septum; ROS, reactive oxygen species; SOD-1, superoxide dismutase; STAT-3, signal transducer and activator of transcription 3; TLR4, toll-like receptor 4; TGF-β transforming growth factor β; TG, triglycerides.
A summary of the mechanistic effects of melatonin on myocardial ischemia-reperfusion injury, myocardial hypoxia-reoxygenation injury, pulmonary hypertension, hypertension, and vascular diseases. (original).
Acknowledgements
H.S. wrote the manuscript, A.M.G. and S.Q. were involved in editing the manuscript.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Hardeland R, Pandi-Perumal SR, Cardinali DP. Melatonin. Int J Biochem Cell Biol 2006; 38:313–316. [DOI] [PubMed] [Google Scholar]
- 2.Skene DJ, Arendt J. Human circadian rhythms: physiological and therapeutic relevance of light and melatonin. Ann Clin Biochem 2006; 43:344–353. [DOI] [PubMed] [Google Scholar]
- 3.Arendt J, Bojkowski C, Folkard S, et al. Some effects of melatonin and the control of its secretion in humans. Ciba Found Symp 1985; 117:266–283. [DOI] [PubMed] [Google Scholar]
- 4.Sun H, Huang FF, Qu S. Melatonin: a potential intervention for hepatic steatosis. Lipids Health Dis 2015; 14:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agil A, Navarro-Alarcon M, Ruiz R, et al. Beneficial effects of melatonin on obesity and lipid profile in young Zucker diabetic fatty rats. J Pineal Res 2011; 50:207–212. [DOI] [PubMed] [Google Scholar]
- 6.Espino J, Pariente JA, Rodriguez AB. Role of melatonin on diabetes-related metabolic disorders. World J Diabetes 2011; 2:82–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tan DX, Manchester LC, Reiter RJ, et al. Ischemia/reperfusion-induced arrhythmias in the isolated rat heart: prevention by melatonin. J Pineal Res 1998; 25:184–191. [DOI] [PubMed] [Google Scholar]
- 8.Yang Y, Sun Y, Yi W, et al. A review of melatonin as a suitable antioxidant against myocardial ischemia-reperfusion injury and clinical heart diseases. J Pineal Res 2014; 57:357–366. [DOI] [PubMed] [Google Scholar]
- 9.Hu ZP, Fang XL, Fang N, et al. Melatonin ameliorates vascular endothelial dysfunction, inflammation, and atherosclerosis by suppressing the TLR4/NF-kappaB system in high-fat-fed rabbits. J Pineal Res 2013; 55:388–398. [DOI] [PubMed] [Google Scholar]
- 10.Favero G, Rodella LF, Reiter RJ, et al. Melatonin and its atheroprotective effects: a review. Mol Cell Endocrinol 2014; 382:926–937. [DOI] [PubMed] [Google Scholar]
- 11.Benova T, Viczenczova C, Radosinska J, et al. Melatonin attenuates hypertension-related proarrhythmic myocardial maladaptation of connexin-43 and propensity of the heart to lethal arrhythmias. Can J Physiol Pharmacol 2013; 91:633–639. [DOI] [PubMed] [Google Scholar]
- 12.Hung MW, Kravtsov GM, Lau CF, et al. Melatonin ameliorates endothelial dysfunction, vascular inflammation, and systemic hypertension in rats with chronic intermittent hypoxia. J Pineal Res 2013; 55:247–256. [DOI] [PubMed] [Google Scholar]
- 13.Sehirli AO, Koyun D, Tetik S, et al. Melatonin protects against ischemic heart failure in rats. J Pineal Res 2013; 55:138–148. [DOI] [PubMed] [Google Scholar]
- 14.Dominguez-Rodriguez A, Abreu-Gonzalez P, Reiter RJ. The potential usefulness of serum melatonin level to predict heart failure in patients with hypertensive cardiomyopathy. Int J Cardiol 2014; 174:415–417. [DOI] [PubMed] [Google Scholar]
- 15.Liu X, Chen Z, Chua CC, et al. Melatonin as an effective protector against doxorubicin-induced cardiotoxicity. Am J Physiol Heart Circ Physiol 2002; 283:H254–H263. [DOI] [PubMed] [Google Scholar]
- 16.Mukherjee D, Ghosh AK, Bandyopadhyay A, et al. Melatonin protects against isoproterenol-induced alterations in cardiac mitochondrial energy-metabolizing enzymes, apoptotic proteins, and assists in complete recovery from myocardial injury in rats. J Pineal Res 2012; 53:166–179. [DOI] [PubMed] [Google Scholar]
- 17.Kang JW, Lee SM. Melatonin inhibits type 1 interferon signaling of toll-like receptor 4 via heme oxygenase-1 induction in hepatic ischemia/reperfusion. J Pineal Res 2012; 53:67–76. [DOI] [PubMed] [Google Scholar]
- 18.Cetin N, Suleyman H, Sener E, et al. The prevention of ischemia/reperfusion induced oxidative damage by venous blood in rabbit kidneys monitored with biochemical, histopatological and immunohistochemical analysis. J Physiol Pharmacol 2014; 65:383–392. [PubMed] [Google Scholar]
- 19.Ghaeli P, Vejdani S, Ariamanesh A, et al. Effect of melatonin on cardiac injury after primary percutaneous coronary intervention: a randomized controlled trial. Iran J Pharm Res 2015; 14:851–855. [PMC free article] [PubMed] [Google Scholar]
- 20.Ekelof SV, Halladin NL, Jensen SE, et al. Effects of intracoronary melatonin on ischemia-reperfusion injury in ST-elevation myocardial infarction. Heart Vessels 2016; 31:88–95. [DOI] [PubMed] [Google Scholar]
- 21.Yu L, Sun Y, Cheng L, et al. Melatonin receptor-mediated protection against myocardial ischemia/reperfusion injury: role of SIRT1. J Pineal Res 2014; 57:228–238. [DOI] [PubMed] [Google Scholar]
- 22▪.Han D, Huang W, Li X, et al. Melatonin facilitates adipose-derived mesenchymal stem cells to repair the murine infarcted heart via the SIRT1 signaling pathway. J Pineal Res 2016; 60:178–192. [DOI] [PubMed] [Google Scholar]; Han et al. found that melatonin could protect ADSCs against hypoxia/serum deprivation injury by modulating the SIRT1 signaling pathway. Combined melatonin–AD-MSC to the convention therapy treatment was suggested to be a potential therapy for patients with MI.
- 23.Zhu P, Liu J, Shi J, et al. Melatonin protects ADSCs from ROS and enhances their therapeutic potency in a rat model of myocardial infarction. J Cell Mol Med 2015; 19:2232–2243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yu L, Liang H, Lu Z, et al. Membrane receptor-dependent Notch1/Hes1 activation by melatonin protects against myocardial ischemia-reperfusion injury: in vivo and in vitro studies. J Pineal Res 2015; 59:420–433. [DOI] [PubMed] [Google Scholar]
- 25.Liu LF, Qin Q, Qian ZH, et al. Protective effects of melatonin on ischemia-reperfusion induced myocardial damage and hemodynamic recovery in rats. Eur Rev Med Pharmacol Sci 2014; 18:3681–3686. [PubMed] [Google Scholar]
- 26.Liu LF, Qian ZH, Qin Q, et al. Effect of melatonin on oncosis of myocardial cells in the myocardial ischemia/reperfusion injury rat and the role of the mitochondrial permeability transition pore. Genet Mol Res 2015; 14:7481–7489. [DOI] [PubMed] [Google Scholar]
- 27.Nduhirabandi F, Huisamen B, Strijdom H, et al. Short-term melatonin consumption protects the heart of obese rats independent of body weight change and visceral adiposity. J Pineal Res 2014; 57:317–332. [DOI] [PubMed] [Google Scholar]
- 28▪.Yu L, Liang H, Dong X, et al. Reduced SIRT1 signaling exacerbates myocardial ischemia reperfusion injury in type 2 diabetic rats and the protective effect of melatonin. J Pineal Res 2015; 59:376–390. [DOI] [PubMed] [Google Scholar]; Yu et al. found that melatonin could modulate ER stress by suppressing PERK/eIF2α/ATF4 signaling pathway. This work provided novel insights into the etiogenesis of diabetic cardiovascular complications, highlighting melatonin's cardio protective effect for the type 2 diabetic patients with ischemic heart disease.
- 29.Fernandez A, Ordonez R, Reiter RJ, et al. Melatonin and endoplasmic reticulum stress: relation to autophagy and apoptosis. J Pineal Res 2015; 59:292–307. [DOI] [PubMed] [Google Scholar]
- 30▪.Nduhirabandi F, Lamont K, Albertyn Z, et al. Role of toll-like receptor 4 in melatonin-induced cardioprotection. J Pineal Res 2016; 60:39–47. [DOI] [PubMed] [Google Scholar]; Nduhirabandi implicated Toll-like receptor 4 (TLR4) signaling in the protective effects of melatonin, supporting melatonin as a safe and effective therapy against cardiovascular disease.
- 31.Levy P, Ryan S, Oldenburg O, et al. Sleep apnoea and the heart. Eur Respir Rev 2013; 22:333–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32▪.Yeung HM, Hung MW, Lau CF, et al. Cardioprotective effects of melatonin against myocardial injuries induced by chronic intermittent hypoxia in rats. J Pineal Res 2015; 58:12–25. [DOI] [PubMed] [Google Scholar]; Yeung et al. reported that melatonin protected against CIH-induced myocardial inflammation, fibrosis, and ischemia-reperfusion injury. Melatonin is supportive on the prophylactic usage of melatonin in obstructive sleep apnea patients.
- 33.Xie S, Deng Y, Pan YY, et al. Melatonin protects against chronic intermittent hypoxia-induced cardiac hypertrophy by modulating autophagy through the 5’ adenosine monophosphate-activated protein kinase pathway. Biochem Biophys Res Commun 2015; 464:975–981. [DOI] [PubMed] [Google Scholar]
- 34.Yu J, Wei J, Ji L, et al. Exploration on mechanism of a new type of melatonin receptor agonist Neu-p11 in hypoxia-reoxygenation injury of myocardial cells. Cell Biochem Biophys 2014; 70:999–1003. [DOI] [PubMed] [Google Scholar]
- 35.Paradies G, Paradies V, Ruggiero FM, et al. Protective role of melatonin in mitochondrial dysfunction and related disorders. Arch Toxicol 2015; 89:923–939. [DOI] [PubMed] [Google Scholar]
- 36.Ortiz F, Garcia JA, Acuna-Castroviejo D, et al. The beneficial effects of melatonin against heart mitochondrial impairment during sepsis: inhibition of iNOS and preservation of nNOS. J Pineal Res 2014; 56:71–81. [DOI] [PubMed] [Google Scholar]
- 37.Itani N, Skeffington KL, Beck C, et al. Melatonin rescues cardiovascular dysfunction during hypoxic development in the chick embryo. J Pineal Res 2016; 60:16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vonk-Noordegraaf A, Haddad F, Chin KM, et al. Right heart adaptation to pulmonary arterial hypertension: physiology and pathobiology. J Am Coll Cardiol 2013; 62 (25 Suppl):D22–33. [DOI] [PubMed] [Google Scholar]
- 39.Maarman G, Blackhurst D, Thienemann F, et al. Melatonin as a preventive and curative therapy against pulmonary hypertension. J Pineal Res 2015; 59:343–353. [DOI] [PubMed] [Google Scholar]
- 40.Torres F, Gonzalez-Candia A, Montt C, et al. Melatonin reduces oxidative stress and improves vascular function in pulmonary hypertensive newborn sheep. J Pineal Res 2015; 58:362–373. [DOI] [PubMed] [Google Scholar]
- 41▪.Jin H, Wang Y, Zhou L, et al. Melatonin attenuates hypoxic pulmonary hypertension by inhibiting the inflammation and the proliferation of pulmonary arterial smooth muscle cells. J Pineal Res 2014; 57:442–450. [DOI] [PubMed] [Google Scholar]; Jin et al. reported that melatonin attenuated hypoxic pulmonary hypertension. It is the first report that provides clues that melatonin might be a potential therapy for patients with hypoxic pulmonary hypertension.
- 42.Pechanova O, Paulis L, Simko F. Peripheral and central effects of melatonin on blood pressure regulation. Int J Mol Sci 2014; 15:17920–17937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Simko F, Paulis L. Melatonin as a potential antihypertensive treatment. J Pineal Res 2007; 42:319–322. [DOI] [PubMed] [Google Scholar]
- 44.Simko F, Pechanova O, Repova Bednarova K, et al. Hypertension and cardiovascular remodelling in rats exposed to continuous light: protection by ACE-inhibition and melatonin. Mediators Inflamm 2014; 2014:703175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ilhan S, Atessahin D, Atessahin A, et al. 2,3,7,8-Tetrachlorodibenzo-p-dioxin-induced hypertension: the beneficial effects of melatonin. Toxicol Ind Health 2015; 31:298–303. [DOI] [PubMed] [Google Scholar]
- 46.Borghi C, Cicero AF. Nutraceuticals with clinically detectable blood pressure lowering effect: a review of available randomized clinical trials and their meta-analyses. Br J Clin Pharmacol 2016; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gubin DG, Gubin GD, Gapon LI, et al. Daily melatonin administration attenuates age-dependent disturbances of cardiovascular rhythms. Curr Aging Sci 2016; 9:5–13. [DOI] [PubMed] [Google Scholar]
- 48.Broncel M, Kozirog-Kolacinska M, Chojnowska-Jezierska J. Melatonin in the treatment of atherosclerosis. Pol Merkur Lekarski 2007; 23:124–127. [PubMed] [Google Scholar]
- 49.Rodella LF, Favero G, Foglio E, et al. Vascular endothelial cells and dysfunctions: role of melatonin. Front Biosci (Elite Ed) 2013; 5:119–129. [DOI] [PubMed] [Google Scholar]
- 50.Cheng X, Wan Y, Xu Y, et al. Melatonin alleviates myosin light chain kinase expression and activity via the mitogen-activated protein kinase pathway during atherosclerosis in rabbits. Mol Med Rep 2015; 11:99–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tang ST, Su H, Zhang Q, et al. Melatonin attenuates aortic endothelial permeability and arteriosclerosis in streptozotocin-induced diabetic rats: possible role of MLCK- and MLCP-dependent MLC phosphorylation. J Cardiovasc Pharmacol Ther 2016; 21:82–92. [DOI] [PubMed] [Google Scholar]
- 52.Zhu HQ, Li Q, Dong LY, et al. MicroRNA-29b promotes high-fat diet-stimulated endothelial permeability and apoptosis in apoE knock-out mice by down-regulating MT1 expression. Int J Cardiol 2014; 176:764–770. [DOI] [PubMed] [Google Scholar]
- 53.Yang GH, Li YC, Wang ZQ, et al. Protective effect of melatonin on cigarette smoke-induced restenosis in rat carotid arteries after balloon injury. J Pineal Res 2014; 57:451–458. [DOI] [PubMed] [Google Scholar]
- 54.Rexhaj E, Pireva A, Paoloni-Giacobino A, et al. Prevention of vascular dysfunction and arterial hypertension in mice generated by assisted reproductive technologies by addition of melatonin to culture media. Am J Physiol Heart Circ Physiol 2015; 309:H1151–H1156. [DOI] [PubMed] [Google Scholar]
- 55.Tang ST, Su H, Zhang Q, et al. Melatonin attenuates aortic endothelial permeability and arteriosclerosis in streptozotocin-induced diabetic rats: possible role of MLCK- and MLCP-dependent MLC phosphorylation. J Cardiovasc Pharmacol Ther 2016; 21:82–92. [DOI] [PubMed] [Google Scholar]
- 56.Jing Y, Wu Q, Yuan X, et al. Microvascular protective role of pericytes in melatonin-treated spinal cord injury in the C57BL/6 mice. Chin Med J (Engl) 2014; 127:2808–2813. [PubMed] [Google Scholar]
- 57.Wiggins-Dohlvik K, Han MS, Stagg HW, et al. Melatonin inhibits thermal injury-induced hyperpermeability in microvascular endothelial cells. J Trauma Acute Care Surg 2014; 77:899–905. [DOI] [PubMed] [Google Scholar]
- 58.Ozdemir G, Ergun Y, Bakaris S, et al. Melatonin prevents retinal oxidative stress and vascular changes in diabetic rats. Eye (Lond) 2014; 28:1020–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Salmanoglu DS, Gurpinar T, Vural K, et al. Melatonin and L-carnitin improves endothelial disfunction and oxidative stress in Type 2 diabetic rats. Redox Biol 2016; 8:199–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60▪.Yang Y, Fan C, Deng C, et al. Melatonin reverses flow shear stress-induced injury in bone marrow mesenchymal stem cells via activation of AMP-activated protein kinase signaling. J Pineal Res 2016; 60:228–241. [DOI] [PubMed] [Google Scholar]; Yang et al. suggested that targeting melatonin relating signaling in tissue-engineered heart valves may be an effective strategy in treating valvular heart disease.
- 61.Celinski K, Konturek PC, Slomka M, et al. Effects of treatment with melatonin and tryptophan on liver enzymes, parameters of fat metabolism and plasma levels of cytokines in patients with nonalcoholic fatty liver disease--14 months follow up. J Physiol Pharmacol 2014; 65:75–82. [PubMed] [Google Scholar]
- 62.Wang Z, Ni L, Wang J, et al. The protective effect of melatonin on smoke-induced vascular injury in rats and humans: a randomized controlled trial. J Pineal Res 2016; 60:217–227. [DOI] [PubMed] [Google Scholar]
- 63.Allagui MS, Hachani R, Saidi S, et al. Pleiotropic protective roles of melatonin against aluminium-induced toxicity in rats. Gen Physiol Biophys 2015; 34:415–424. [DOI] [PubMed] [Google Scholar]
- 64.Sniderman AD, Pencina M, Thanassoulis G. Limitations in the conventional assessment of the incremental value of predictors of cardiovascular risk. Curr Opin Lipidol 2015; 26:210–214. [DOI] [PubMed] [Google Scholar]


