Abstract
Objectives
To evaluate the impact of dietary sodium and potassium (Na–K) ratio on mortality from total and subtypes of stroke, cardiovascular disease (CVD) and all causes, using 24-year follow-up data of a representative sample of the Japanese population.
Setting
Prospective cohort study.
Participants
In the 1980 National Cardiovascular Survey, participants were followed for 24 years (NIPPON DATA80, National Integrated Project for Prospective Observation of Non-communicable Disease And its Trends in the Aged). Men and women aged 30–79 years without hypertensive treatment, history of stroke or acute myocardial infarction (n=8283) were divided into quintiles according to dietary Na–K ratio assessed by a 3-day weighing dietary record at baseline. Age-adjusted and multivariable-adjusted HRs were calculated using the Mantel-Haenszel method and Cox proportional hazards model.
Primary outcome measures
Mortality from total and subtypes of stroke, CVD and all causes.
Results
A total of 1938 deaths from all causes were observed over 176 926 person-years. Na–K ratio was significantly and non-linearly related to mortality from all stroke (p=0.002), CVD (p=0.005) and total mortality (p=0.001). For stroke subtypes, mortality from haemorrhagic stroke was positively related to Na–K ratio (p=0.024). Similar relationships were observed for men and women. The observed relationships remained significant after adjustment for other risk factors. Quadratic non-linear multivariable-adjusted HRs (95% CI) in the highest quintile versus the lowest quintile of Na–K ratio were 1.42 (1.07 to 1.90) for ischaemic stroke, 1.57 (1.05 to 2.34) for haemorrhagic stroke, 1.43 (1.17 to 1.76) for all stroke, 1.39 (1.20 to 1.61) for CVD and 1.16 (1.06 to 1.27) for all-cause mortality.
Conclusions
Dietary Na–K ratio assessed by a 3-day weighing dietary record was a significant risk factor for mortality from haemorrhagic stroke, all stroke, CVD and all causes among a Japanese population.
Keywords: sodium, potassium, cardiovascular disease, prospective cohort, NUTRITION & DIETETICS
Strengths and limitations of this study.
Studies on the relationships of dietary sodium-to-potassium (Na–K) ratio with stroke or cardiovascular disease (CVD) mortality have been sparse.
This report showed that a higher dietary Na–K ratio was associated with higher mortality risk from stroke, CVD and all causes, in a representative sample of the Japanese population.
Strengths include the use of a 3-day weighing dietary record method from the National Nutritional Survey data, in assessing Na–K ratio.
A limitation is that dietary habits and CVD risk factors were assessed only once at the baseline survey, and their changes during the follow-up period were not accounted for.
Introduction
Dietary sodium and potassium intake have been found to be related to hypertension,1 and moderate dietary salt reduction causes significant reductions in blood pressure (BP),2 reducing the risk of cardiovascular disease (CVD). Also, increase in potassium intake has been shown to reduce BP.3
The Japanese diet has been characterised by high sodium intake. In 1975, the average sodium intake was 240 mmol (5520 mg) per day and although it has markedly decreased over the years, it still remains high at around 175 mmol (4025 mg) per day in 2010.4 In addition, a low intake of potassium has been reported in Japan, contributing to a high sodium-to-potassium (Na–K) ratio.5 6 The effects of high sodium and low potassium intake on BP levels are synergic, and thus the Na–K ratio may be a strong indicator for risk of CVD mortality.7–9 Recent reports from the USA have addressed the significant relationship of dietary Na–K ratio with CVD and ischaemic heart disease.10–12 These relationships, as well as the relationship of Na–K ratio with stroke, should be investigated in Japan. This is important as mortality from stroke in Japan is higher than that of ischaemic heart disease. Furthermore, Japanese diets are considerably different from those in Western countries; for example, they are higher in sodium and lower in potassium intake, as well as higher in fish and lower in fat consumption.13
In this study, we combined the follow-up data of participants in the National Cardiovascular Survey Japan (NCSJ) and the dietary estimates from the National Nutrition Survey (NNS), in which a 3-day weighing dietary records was carried out for the same participants at baseline. We examined the relationships of dietary Na–K ratio with mortality from stroke, stroke subtypes, CVD and all causes in this 24-year follow-up of a representative Japanese population.
Methods
Cohort studies of the NCSJ are known as NIPPON DATA (National Integrated Project for Prospective Observation of Non-communicable Disease And its Trends in the Aged). The present study analysed data from NIPPON DATA80, in which baseline surveys had been performed in 1980. Three hundred survey districts throughout Japan were randomly selected, and a total of 13 771 people aged 30 years and over were eligible and invited to participate in the study. The participation rate was 76.6% (10 546 people) before exclusion criteria were implemented for this present study.
The survey of participants consisted of history of CVD, physical examinations, blood tests and a self-administered questionnaire. In the lifestyle questionnaire, participants were asked about their habits of alcohol drinking (every day, sometimes, seldom or ex-drinker) and smoking (current, non-smoker or ex-smoker). Trained observers measured BP for each participant, using a standard mercury sphygmomanometer. Non-fasting blood samples were drawn and centrifuged within 60 min of collection. Serum total cholesterol was analysed in an auto-analyser (SMA12/60; Technicon, Tarrytown, New York, USA) at one specific laboratory (Center for Adult Diseases, Osaka). This laboratory has been certified since 1975 by the CDC-NHLBI Lipid Standardization Program of the Center for Disease Control and Prevention, Atlanta, Georgia, USA. Serum glucose was measured by the cupric-neocuproine method, using an auto-analyser. Since blood glucose levels are now widely measured by the hexokinase method, serum glucose levels were adjusted using a formula ((0.047×(glucose concentration in mg/dL))−0.541) previously reported by the same laboratory, which provides levels in mmol/L.14 Diabetes was defined as serum glucose of 11.1 mmol/L or higher, history of diabetes, or both.
The NNS in 1980 was conducted for the same participants who were in the NCSJ. Dietary intakes were assessed for each household, using a 3-day weighing dietary record method. Trained dieticians reviewed dietary records with the participants and edited them as necessary. Survey data were processed centrally to calculate total energy intake and intake of nutrients, including sodium and 84 food groups.15 Since potassium intake was not calculated in the original survey results,16 we calculated it from the 84 food groups intake, using the food database developed for the INTERMAP Study (international study of macronutrients and micronutrients and BP).17
Nutrient intake of each household member was estimated by dividing household intake data of NNS in 1980 proportionally with average intake as categorised by sex and age group calculated for the 1995 NNS. The detailed procedure and results of validation for these estimations have been reported elsewhere.18 19 Per cent energy intake from protein and total fat were calculated as follows: the amounts of intake for protein and total fat were multiplied by 4 and 9, respectively, and the sum of the two products was divided by total energy intake. We combined the nutritional data with the follow-up database of NIPPON DATA80, obtaining data for 10 422 eligible participants.
For the present study, participants were followed until 2004 (NIPPON DATA80, 1980–2004). We used computerised vital statistics data to identify the underlying causes of death with the permission of the Management and Coordination Agency, Japan. At follow-up, we obtained information on 9550 participants (a follow-up rate of 91.6%), and a total of 2278 deaths were identified. The procedure used for end point determination in our study has been reported elsewhere.15 Definitions of underlying cause of death for Japan's National Vital Statistics using International Classification of Disease (ICD) are shown in online supplementary table S1. Of the 9550 participants, we excluded 1267 individuals who met the following conditions at baseline: those with a history of myocardial infarction (n=45) or stroke (n=109); those aged 80 years or older (n=150), as their estimated nutrient intake may be inaccurate; those who reported use of antihypertensive medication (n=1079; the total did not add up to 1267 due to overlap). We, therefore, analysed the remaining 8283 participants for this report (see online supplementary figure for participant flow).
bmjopen-2016-011632supp.pdf (180.5KB, pdf)
Regular drinking was defined as drinking alcohol every day. Participants were divided into sex-specific quintiles of dietary Na–K ratio (mmol/mmol). We performed analyses of covariance and trend analyses for continuous variables including age and sex as covariates. We conducted the χ2 test to examine independence and the linearity of trends for categorical variables across quintiles of the Na–K ratio. Using a person-year method of analysis, age-adjusted mortality rates were calculated according to the standard population of Japan in 1985. Age-adjusted relative risks and 95% CIs were calculated using the Mantel-Haenszel procedure. The test for linear and quadratic non-linear trends was used to assess dietary Na–K ratio categories in terms of the relative risk.
The Cox proportional hazards model was used to calculate multivariable-adjusted HRs across the quintiles of dietary Na–K ratio, using quadratic non-linear regression. In model I, sex, age (years), body mass index (BMI; kg/m2), smoking habit and drinking habit were adjusted. In model II, diabetes (yes/no) and serum total cholesterol (mg/dL) were adjusted in addition to variables in model I. Further adjustment was made for per cent energy intake from protein and total fat in model III. Hypothesis testing was two-sided, with a 0.05 level of significance. SPSS V.21.0 for Windows (IBM Corporation, Chicago, Illinois, USA) was used for all analyses.
Results
Table 1 shows the baseline characteristics according to sex-specific quintiles of dietary Na–K ratio. Median values of dietary Na–K quintiles were similar in both sexes. Both sodium and potassium intake were significantly related to dietary Na–K ratio (p trend <0.001). Significantly higher per cent energy intake from protein (p trend <0.001) and significantly lower intake from total fat (p trend <0.001) were also observed with higher category of dietary Na–K ratio in both sexes. Moving from low to high Na–K ratio quintiles, average systolic BP (p trend <0.001) and average BMI (p trend <0.049) significantly increased in men, but not in women, and serum cholesterol levels decreased (p trend <0.001) in both sexes. Prevalence rate of current drinking and current smoking rose with increasing dietary Na–K ratio in men.
Table 1.
Baseline characteristics of participants according to the quintiles of dietary sodium-to-potassium ratio among participants of NIPPON DATA80 (National Integrated Project for Prospective Observation of Non-communicable Disease And its Trends in the Aged) aged 30–79 years without antihypertensive treatment
| Q1 | Q2 | Q3 | Q4 | Q5 | p Value* | p Trend† | |
|---|---|---|---|---|---|---|---|
| Men | |||||||
| Sodium-to-potassium ratio (mol/mol) | 1.30 (0.18) | 1.64 (0.07) | 1.90 (0.08) | 2.19 (0.10) | 2.81 (0.49) | – | – |
| (Range) | (0.55) (1.51) | (1.51) (1.77) | (1.77) (2.03) | (2.04) (2.37) | (2.37) (6.13) | ||
| Number | 696 | 736 | 749 | 752 | 749 | ||
| Age (years) | 49.6 (12.5) | 48.4 (12.2) | 48.4 (12.1) | 48.4 (12.0) | 49.3 (12.7) | 0.178 | 0.724 |
| Sodium intake (mmol/day) | 179.4 (56.0) | 221.9 (52.7) | 252.2 (68.1) | 285.2 (70.3) | 356.8 (109.8) | <0.001 | <0.001 |
| (mg/day) | 4127 (1289) | 5103 (1211) | 5801 (1567) | 6559 (1617) | 8206 (2526) | – | – |
| Potassium intake (mmol/day) | 81.4 (22.6) | 79.7 (18.6) | 78.3 (20.7) | 76.8 (18.7) | 75.1 (20.1) | <0.001 | <0.001 |
| (mg/day) | 3174 (882) | 3109 (727) | 3054 (809) | 2996 (731) | 2928 (784) | – | – |
| Protein intake (energy per cent) | 14.9 (2.3) | 15.0 (2.0) | 15.0 (2.1) | 15.1 (1.9) | 15.2 (2.2) | <0.001 | <0.001 |
| Total fat intake (energy per cent) | 21.1 (5.1) | 20.6 (5.0) | 20.2 (5.2) | 20.2 (5.0) | 19.1 (5.5) | <0.001 | <0.001 |
| Systolic blood pressure (mm Hg) | 134.4 (18.6) | 135.0 (19.4) | 134.9 (19.3) | 136.5 (18.8) | 139.0 (20.8) | <0.001 | <0.001 |
| Diastolic blood pressure (mm Hg) | 82.2 (11.7) | 82.1 (12.4) | 82.5 (11.7) | 82.9 (12.0) | 83.4 (11.7) | 0.160 | 0.015 |
| Body mass index (kg/m2) | 22.5 (2.9) | 22.4 (2.8) | 22.6 (2.8) | 22.5 (2.8) | 25.1 (50.6) | 0.100 | 0.049 |
| Serum cholesterol (mg/dL) | 190.3 (32.8) | 184.7 (31.6) | 188.0 (33.0) | 184.9 (32.9) | 181.5 (32.7) | <0.001 | <0.001 |
| Serum creatinine (mg/dL) | 1.066 (0.389) | 1.050 (0.151) | 1.060 (0.290) | 1.038 (0.136) | 1.027 (0.182) | 0.021 | 0.003 |
| Regular drinking (%) | 43.1 | 47.5 | 48.8 | 51.3 | 50.5 | 0.041 | 0.010 |
| Current smoking (%) | 60.8 | 61.5 | 63.1 | 66.5 | 70.8 | <0.001 | <0.001 |
| Diabetes‡ (%) | 8.3 | 5.4 | 4.7 | 6.5 | 6.8 | 0.049 | 0.049 |
| Hypertension§ (%) | 43.2 | 40.2 | 45.3 | 45.7 | 48.6 | 0.020 | 0.004 |
| Women | |||||||
| Sodium-to-potassium ratio (mol/mol) | 1.22 (0.16) | 1.55 (0.07) | 1.80 (0.07) | 2.08 (0.09) | 2.65 (0.44) | – | – |
| (Range) | (0.59) (1.42) | (1.42) (1.67) | (1.67) (1.93) | (1.93) (2.25) | (2.25) (5.83) | ||
| Number | 885 | 916 | 936 | 932 | 932 | ||
| Age (years) | 50.2 (12.0) | 48.7 (11.8) | 48.2 (12.1) | 47.9 (12.3) | 49.0 (12.9) | 0.001 | 0.015 |
| Sodium intake (mmol/day) | 155.5 (44.7) | 190.9 (48.9) | 215.9 (59.6) | 247.2 (63.1) | 300.0 (91.7) | <0.001 | <0.001 |
| (mg/day) | 3575 (1027) | 4392 (1124) | 4966 (1372) | 5685 (1452) | 6900 (2110) | – | – |
| Potassium intake (mmol/day) | 75.2 (20.1) | 72.6 (18.2) | 70.9 (19.4) | 70.2 (17.9) | 67.1 (18.3) | <0.001 | <0.001 |
| (mg/day) | 2933 (784) | 2833 (710) | 2764 (757) | 2739 (699) | 2617 (712) | – | – |
| Protein intake (energy per cent) | 15.4 2.2 | 15.3 2.0 | 15.3 1.9 | 15.5 2.0 | 15.5 2.2 | <0.001 | <0.001 |
| Total fat intake (energy per cent) | 22.9 5.5 | 22.6 5.8 | 22.1 5.7 | 21.9 5.5 | 20.9 6.0 | <0.001 | <0.001 |
| Systolic blood pressure (mm Hg) | 131.7 (20.2) | 130.9 (19.5) | 129.5 (19.1) | 129.7 (18.0) | 131.3 (19.0) | 0.044 | 0.342 |
| Diastolic blood pressure (mm Hg) | 78.7 (11.4) | 78.6 (11.4) | 77.7 (11.0) | 78.1 (10.6) | 78.5 (11.2) | 0.196 | 0.453 |
| Body mass index (kg/m2) | 22.6 (3.4) | 22.7 (3.3) | 22.6 (3.2) | 22.7 (3.3) | 22.7 (3.2) | 0.932 | 0.572 |
| Serum cholesterol (mg/dL) | 195.5 (33.1) | 189.6 (34.1) | 188.8 (34.1) | 185.7 (32.0) | 184.9 (33.6) | <0.001 | <0.001 |
| Serum creatinine (mg/dL) | 0.847 (0.241) | 0.833 (0.123) | 0.832 (0.121) | 0.825 (0.115) | 0.829 (0.122) | 0.031 | 0.008 |
| Regular drinking (%) | 3.5 | 2.1 | 3.6 | 2.4 | 2.9 | 0.063 | 0.152 |
| Current smoking (%) | 9.0 | 8.1 | 8.7 | 8.4 | 10.2 | 0.535 | 0.545 |
| Diabetes‡ (%) | 4.3 | 3.8 | 3.5 | 2.9 | 4.5 | 0.388 | 0.376 |
| Hypertension§ (%) | 35.6 | 33.1 | 31.3 | 32.3 | 34.7 | 0.290 | 0.290 |
| Men and women combined | |||||||
| Sodium-to-potassium ratio (mol/mol) | 1.25 (0.17) | 1.59 (0.09) | 1.84 (0.09) | 2.13 (0.11) | 2.72 (0.47) | – | – |
| (Range) | (0.55) (1.51) | (1.42) (1.77) | (1.67) (2.03) | (1.93) (2.37) | (2.25) (6.13) | ||
| Number | 1581 | 1652 | 1685 | 1684 | 1681 | ||
| Age (years) | 49.9 (12.2) | 48.6 (12.0) | 48.3 (12.1) | 48.1 (12.2) | 49.1 (12.8) | <0.001 | 0.042 |
| Sodium intake (mmol/day) | 166.0 (51.3) | 204.7 (52.9) | 232.1 (66.1) | 264.2 (69.0) | 325.3 (104.1) | <0.001 | <0.001 |
| (mg/day) | 3818 (1181) | 4709 (1216) | 5337 (1519) | 6076 (1588) | 7482 (2394) | – | – |
| Potassium intake (mmol/day) | 77.9 (21.5) | 75.8 (18.7) | 74.2 (20.3) | 73.2 (18.6) | 70.7 (19.5) | <0.001 | <0.001 |
| (mg/day) | 3039 (837) | 2956 (730) | 2893 (793) | 2854 (725) | 2755 (761) | – | – |
| Protein intake (energy per cent) | 15.2 2.2 | 15.2 2.0 | 15.2 2.0 | 15.4 2.0 | 15.4 2.2 | <0.001 | <0.001 |
| Total fat intake (energy per cent) | 22.1 5.4 | 21.7 5.6 | 21.3 5.6 | 21.1 5.4 | 20.1 5.8 | <0.001 | <0.001 |
| Systolic blood pressure (mm Hg) | 132.9 (19.5) | 132.7 (19.5) | 131.9 (19.4) | 132.7 (18.7) | 134.8 (20.2) | 0.001 | 0.012 |
| Diastolic blood pressure (mm Hg) | 80.2 (11.6) | 80.2 (12.0) | 79.8 (11.5) | 80.2 (11.5) | 80.7 (11.7) | 0.248 | 0.241 |
| Body mass index (kg/m2) | 22.6 (3.2) | 22.6 (3.1) | 22.6 (3.0) | 22.6 (3.0) | 23.8 (33.8) | 0.100 | 0.042 |
| Serum cholesterol (mg/dL) | 193.3 (33.1) | 187.4 (33.1) | 188.4 (33.6) | 185.3 (32.4) | 183.4 (33.3) | <0.001 | <0.001 |
| Serum creatinine (mg/dL) | 0.944 (0.333) | 0.930 (0.174) | 0.933 (0.241) | 0.920 (0.163) | 0.917 (0.181) | 0.006 | 0.008 |
| Regular drinking (%) | 20.9 | 22.3 | 23.7 | 24.2 | 24.1 | 0.111 | 0.011 |
| Current smoking (%) | 30.0 | 30.2 | 31.0 | 32.9 | 35.0 | 0.008 | <0.001 |
| Diabetes‡ (%) | 11.3 | 10.7 | 9.4 | 9.3 | 11.8 | 0.057 | 0.852 |
| Hypertension§ (%) | 40.4 | 37.9 | 39.2 | 40.0 | 43.0 | 0.046 | 0.057 |
Values are means (SD), numbers or percentages.
*p Values obtained by analysis of variance for continuous values and by χ2 test for categorical values.
†p Trend was obtained by trend analysis for continuous variables, and χ2 test for trend for categorical variables.
‡History of diabetes and/or non-fasting blood glucose of 11.1 mmol/L or higher.
§Systolic blood pressure ≥140 mm Hg and/or diastolic blood pressure ≥90 mm Hg.
A total of 176 926 person-years were studied during the 24-year follow-up. Table 2 shows age-adjusted mortality rates according to quintiles of dietary Na–K ratio. Mortality rates from ischaemic stroke, haemorrhagic stroke, all stroke, CVD and all causes were highest in the highest Na–K quintile (Q5), while mortality rates did not appear to be higher for either Q2 or Q3 in reference to Q1. Mortality rates (per 100 000 person-years) for all stroke were 58 for Q1, and 101 for Q5. For ischaemic stroke, the rates were 30 for Q1, and 48 for Q5.
Table 2.
Person-years, mortality numbers and age-adjusted mortality rate (per 100 000 person-years) according to quintiles of dietary sodium-to-potassium ratio for deaths from all causes, CVDs, all stroke and stroke subtypes in a 24-year follow-up of the participants of NIPPON DATA80
| Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | N | (Rate) | N | (Rate) | N | (Rate) | N | (Rate) | N | (Rate) | |
| Person-years | 176926 | 33581 | 35 983 | 35 949 | 36 122 | 35 291 | |||||
| All causes | 1938 | 381 | (502) | 365 | (521) | 368 | (493) | 388 | (568) | 436 | (640) |
| CVD | 579 | 110 | (132) | 114 | (152) | 100 | (116) | 113 | (152) | 142 | (189) |
| Stroke | 273 | 45 | (58) | 46 | (63) | 55 | (65) | 53 | (76) | 74 | (101) |
| Ischaemic stroke | 150 | 29 | (30) | 27 | (29) | 30 | (27) | 26 | (33) | 38 | (48) |
| Haemorrhagic stroke | 67 | 8 | (17) | 12 | (18) | 14 | (25) | 13 | (17) | 20 | (31) |
Values in parentheses are age-adjusted mortality rates per 100 000 person-years for each cause of death.
CVD, cardiovascular disease; NIPPON DATA, National Integrated Project for Prospective Observation of Non-communicable Disease And its Trends in the Aged.
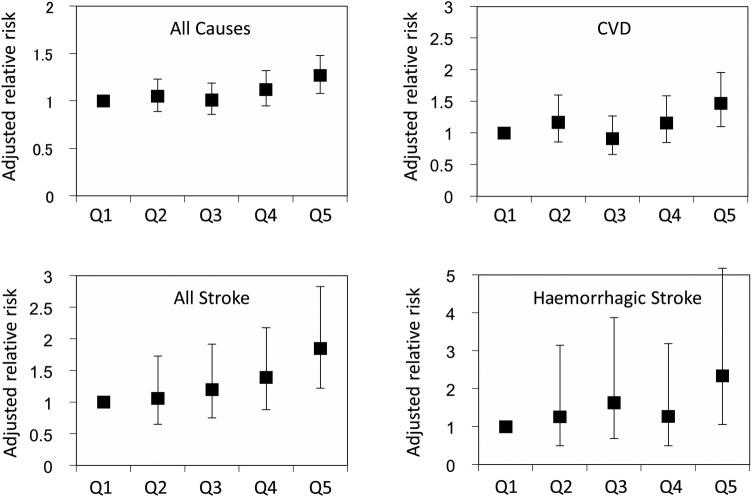
Age-adjusted relative risks and 95% CIs for cause-specific deaths from linear and quadratic regression are shown in table 3 and figure 1. Significantly higher relative risk was observed for deaths from all stroke, CVD and all causes in the highest quintile in total participants for both regression models. p Values obtained by quadratic non-linear regression tended to be lower than those for linear regression. Among stroke subtypes, a significant positive relationship was observed for mortality from haemorrhagic stroke (p=0.024) but not for ischaemic stroke (p=0.099; table 3).
Table 3.
Age-adjusted relative risks and 95% CIs for deaths from all causes, CVDs, stroke and stroke subtypes, according to dietary sodium-to-potassium ratio quintiles using the Mantel-Haenszel method for 24-year follow-up of NIPPON DATA80
| Q1 | Q2 | Q3 | Q4 | Q5 | p Value* | p Value** | |
|---|---|---|---|---|---|---|---|
| All causes | 1 | 1.05 (0.89 to 1.23) | 1.01 (0.86 to 1.19) | 1.12 (0.95 to 1.32) | 1.27 (1.08 to 1.48) | 0.005 | 0.001 |
| CVD | 1 | 1.17 (0.86 to 1.60) | 0.91 (0.66 to 1.27) | 1.16 (0.85 to 1.59) | 1.47 (1.10 to 1.96) | 0.032 | 0.005 |
| Stroke | 1 | 1.06 (0.65 to 1.73) | 1.20 (0.75 to 1.92) | 1.39 (0.88 to 2.18) | 1.85 (1.22 to 2.83) | 0.009 | 0.002 |
| Ischaemic stroke | 1 | 0.96 (0.50 to 1.84) | 0.90 (0.46 to 1.74) | 1.09 (0.58 to 2.06) | 1.57 (0.89 to 2.78) | 0.266 | 0.099 |
| Haemorrhagic stroke | 1 | 1.26 (0.50 to 3.15) | 1.63 (0.69 to 3.88) | 1.27 (0.50 to 3.19) | 2.34 (1.06 to 5.18) | 0.039 | 0.024 |
*p Values of the test for linear trends were calculated using Cox proportional hazards model.
**p Values of the test for quadratic non-linear trends were calculated using Cox proportional hazards model.
CVD, cardiovascular disease; NIPPON DATA, National Integrated Project for Prospective Observation of Non-communicable Disease And its Trends in the Aged.
Figure 1.
Age-adjusted relative risks and 95% CIs for deaths from all causes, CVDs, all stroke and haemorrhagic stroke according to quintiles of dietary sodium-to-potassium ratio by using the Mantel-Haenszel method in a 24-year follow-up of NIPPON DATA80. CVD, cardiovascular disease; NIPPON DATA, National Integrated Project for Prospective Observation of Non-communicable Disease And its Trends in the Aged.
Table 4 shows the quadratic non-linear multivariable-adjusted HRs and 95% CIs in the highest quintile in reference to the lowest quintile of dietary Na–K ratio. In models adjusted for lifestyle factors (model I) and further adjusted for coexistent morbidity (model II), a significant positive relationship was observed for mortality from ischaemic stroke, haemorrhagic stroke, all stroke, CVD and all causes. After further adjustment for per cent energy intake from protein and total fat (model III), the HRs were almost similar to those of model II. The associations were generally similar both in men and women (see online supplementary tables S2 and S3).
Table 4.
Quadratic non-linear multivariate-adjusted HR and 95% CI for deaths from all causes, CVDs, stroke and stroke subtypes, for the highest quintile versus the lowest quintile of dietary sodium-to-potassium ratio in total participants
| HR | (95% CI) | |
|---|---|---|
| Model I | ||
| All causes | 1.18 | (1.08 to 1.29) |
| CVD | 1.35 | (1.17 to 1.56) |
| Stroke | 1.42 | (1.17 to 1.74) |
| Ischaemic stroke | 1.42 | (1.08 to 1.88) |
| Haemorrhagic stroke | 1.55 | (1.05 to 2.27) |
| Model II | ||
| All causes | 1.16 | (1.06 to 1.27) |
| CVD | 1.38 | (1.20 to 1.59) |
| Stroke | 1.44 | (1.18 to 1.76) |
| Ischaemic stroke | 1.42 | (1.08 to 1.88) |
| Haemorrhagic stroke | 1.56 | (1.06 to 2.30) |
| Model III | ||
| All causes | 1.16 | (1.06 to 1.27) |
| CVD | 1.39 | (1.20 to 1.61) |
| Stroke | 1.43 | (1.17 to 1.76) |
| Ischaemic stroke | 1.42 | (1.07 to 1.90) |
| Haemorrhagic stroke | 1.57 | (1.05 to 2.34) |
Model I was adjusted for age, sex, BMI, smoking and drinking habits.
Model II was adjusted for variables in model I plus diabetes and serum total cholesterol.
Model III was adjusted for variables in model II plus per cent energy intake from protein and total fat.
BMI, body mass index; CVD, cardiovascular disease.
Similar but less significant relationships were observed when we used dietary Na–K ratios that were calculated from household intake per 1000 kcal (density value) of sodium and potassium. Significantly higher HRs were also observed for mortality from haemorrhagic stroke, all stroke, CVD and all causes in all models (see online supplementary tables S4–S6).
Discussion
These results demonstrate a positive quadratic non-linear relationship of dietary Na–K ratio with long-term mortality risk from haemorrhagic stroke, all stroke, CVD, as well as all causes, in a representative Japanese population. While stroke mortality has been previously reported to have a positive relationship with dietary sodium and an inverse relationship with dietary potassium in other Japanese studies, these findings were obtained using food frequency questionnaires (FFQs).20 21
Since quantitative estimation of sodium and potassium intake is necessary to calculate dietary Na–K ratio, only a few reports have addressed its relationship with CVD mortality.10–12 22 Cook et al10 reported that lower dietary Na–K ratio was significantly related to decreased stroke mortality in a long-term lifestyle modification study, using 24-hour urine samplings. They also reported an effect of decreased CVD mortality from dietary salt reduction.22 Yang et al11 reported a significant relationship of dietary Na–K ratio to cardiovascular risk, using 1-day (24-hour) dietary recall data obtained for the National Health and Nutrition Examination Survey (NHANES) III, with a 14-year follow-up. This study also supports that higher Na–K ratio is significantly related to higher mortality from all causes, as well as CVD, for both sexes. Judd et al12 reported that high Na–K ratio was significantly related to all-cause mortality among Americans.
Dietary intake of sodium and potassium is predominantly assessed by their excretion in 24-hour urine collection. Estimated dietary intake assessed by FFQs yields low correlation coefficients with those of 24-hour urine.23 However, in previous large-scale prospective studies,20 21 24 sodium and potassium intake was assessed by FFQs rather than the time-consuming 24-hour urine method. Dietary records and the 24-hour recall method are also used for the estimation of salt intake and yield better correlation with those of 24-hour urinary excretion.25 26 However, since the diet of an individual changes day to day, dietary records for several days would be more appropriate for estimation of habitual intake.27 In the present study, we used data from NNS, assessed by a 3-day weighing dietary record that was reviewed by trained dieticians. Dietary Na–K ratio estimated in this cohort study, therefore, would be more suitable for evaluating the relationship with CVD mortality.
The baseline characteristics of participants with higher dietary Na–K ratio included higher per cent intake from protein, lower intake from total fat, higher BP, lower cholesterol levels and higher prevalence of smoking. These factors may have had a confounding effect on the results. Higher total fat intake in lower Na–K categories (reflecting Westernised dietary habits) may influence all-cause and cause-specific mortalities. HRs did not change substantially after the adjustment for percentage intake from protein and total fat (model III), nor did they change after the adjustment for other possible confounding factors (model II).
The strength of using the Na–K ratio as an index of sodium and potassium intake is due to the nature of this measurement being independent from total energy intake. Both dietary sodium and potassium intake have strong relationships with total energy intake.28 In the report by Cohen et al,29 the average energy intake for the lower salt intake group was much lower than what would be expected from the body weight values. Such participants may, thus, have had an insufficient diet. This may also be true when evaluating dietary potassium intake.
In the analyses for stroke subtypes, the Na–K ratio was positively associated with haemorrhagic stroke, but was borderline significant for ischaemic stroke. Haemorrhagic stroke has been reported to be more strongly related to BP than has ischaemic stroke;30 higher Na–K ratio may lead to higher BP during follow-up, and consequently to higher risk of haemorrhagic stroke. Lower numbers of deaths from haemorrhagic stroke (67 deaths) and ischaemic stroke (150 deaths) may also have caused insufficient statistical power for these subanalyses.
This study has some limitations. First, dietary habits and CVD risk factors were assessed only once, at the baseline survey, and may have changed during the follow-up period. Second, dietary intake of individual participants was obtained from a consecutive 3-day weighing record method for each household. This method to estimate sodium intake would be less accurate compared with the 24-hour urine collection method, which is considered the gold standard in estimating sodium intake. Also, because diets naturally vary from weekdays to weekends,17 the 3-day weighing record method may not reflect average dietary habits throughout the week. Thus, estimated dietary values may be overestimated or underestimated and may attenuate the true relationships between Na–K ratio and our outcomes of interest. Third, we used underlying cause of death by ICD 9 and 10 as outcome. The diagnostic accuracy of underlying cause of death may differ from what was registered in the medical record31 and diagnostic criteria have changed through ICD 9 and 10. Last, the statistical power may not be sufficient in the subanalyses on stroke subtypes.
Through public health policy and a national movement for lifestyle change, salt intake has been declining in the Japanese population over the past decades. Because of this, BP levels and stroke mortality have substantially decreased in Japan.32 Recently, we reported sources of dietary sodium in the Japanese diet,33 with soy sauce, miso (fermented soybean seasoning), salted fish and salted pickles being the main sources. Although varieties of salt-reduced soy sauce and miso have been produced,34 trends for both salt intake and stroke mortality have recently reached a plateau.35 Electrolyte intake among Japanese people is also characterised by lower potassium intake than that of Western countries and it has essentially not changed during the past 20 years, leading to a high Na–K ratio level.4 Individual sources of potassium intake could not be identified in this study since all dietary data used in the study were aggregated to 84 food categories. However, we have previously reported that intake of more fruit and vegetable, which are major sources of potassium, had lower risk of CVD mortality.36 Since considerable amounts of dietary vegetable are consumed as salted pickles among Japanese people,33 a decrease in dietary sodium by reducing the intake of these pickles may not give enough of a beneficial effect on lowering Na–K ratio. A high Na–K ratio has also been observed in Korea and China.8
In conclusion, we should bear in mind that lowering dietary Na–K ratio may be a useful, alternative indicator in reducing cardiovascular risk. A recent intervention study to decrease dietary Na–K ratio among the elderly has showed a significant decrease in CVD mortality.37 The combination of salt reduction and potassium increase in the diet could lead to a further decline of BP, and thus of CVD risk, in Japan and in the rest of world.
Footnotes
Collaborators: NIPPON DATA80/90 Research Group Chairpersons: HU (Center for Epidemiologic Research in Asia, Shiga University of Medical Science, Otsu, Shiga), AO (Research Institute of Strategy for Prevention, Tokyo) for the NIPPON DATA80; HU, TOk (Department of Preventive Medicine and Public Health, Keio University, Tokyo) for the NIPPON DATA90. Research members: SS (School of Health Sciences, Sapporo Medical University, Sapporo, Hokkaido), Kiyomi Sakata (Department of Hygiene and Preventive Medicine, Iwate Medical University, Morioka, Iwate), Atsushi Hozawa (Department of Preventive Medicine and Epidemiology, Tohoku Medical Megabank Organization, Tohoku University, Sendai, Miyagi), TH (Department of Hygiene and Preventive Medicine, Fukushima Medical University, Fukushima), Yosikazu Nakamura (Department of Public Health, Jichi Medical University, Shimotsuke, Tochigi), Nobuo Nishi (Center for International Collaboration and Partnership, National Institute of Health and Nutrition, Tokyo), NO (Department of Health and Nutrition, University of Human Arts and Sciences, Saitama), TOh (Department of Hygiene and Public Health Teikyo University School of Medicine, Tokyo), Fumiyoshi Kasagi (Institute of Radiation Epidemiology, Radiation Effects Association, Tokyo), Yoshitaka Murakami (Department of Medical Statistics, Toho University, Tokyo), Toru Izumi (Department of Cardio-Angiology Kitasato University School of Medicine, Sagamihara, Kanagawa), Yasuhiro Matsumura (Faculty of Health and Nutrition, Bunkyo University, Chigasaki, Kanagawa), Toshiyuki Ojima (Department of Community Health and Preventive Medicine, Hamamatsu University School of Medicine, Hamamatsu, Shizuoka), Koji Tamakoshi (Department of Public Health and Health Information Dynamics, Nagoya University Graduate School of Medicine, Nagoya, Aichi), Hideaki Nakagawa (Department of Epidemiology and Public Health, Kanazawa Medical University, Kanazawa, Ishikawa), Yoshikuni Kita (Faculty of Nursing Science, Tsuruga Nursing University, Tsuruga, Fukui), KM (Director of the Center for Epidemiologic Research in Asia, Department of Public Health, Shiga University of Medical Science, Otsu, Shiga), Aya Kadota (Center for Epidemiologic Research in Asia, Shiga University of Medical Science, Otsu, Shiga), AF (Department of Public Health, Shiga University of Medical Science, Otsu, Shiga), Naomi Miyamatsu (Department of Clinical Nursing, Shiga University of Medical Science, Otsu, Shiga), Yasuyuki Nakamura (Department of Food Science and Human Nutrition, Ryukoku University, Otsu, Shiga), KY (Osaka City University Graduate School of Human Life Science, Osaka), Yoshihiro Miyamoto (Department of Preventive Cardiology, National Cerebral and Cardiovascular Center, Suita, Osaka), Kazunori Kodama (Radiation Effects Research Foundation, Hiroshima) and YK (Department of Environmental Medicine, Kyushu University, Fukuoka).
Contributors: AO and HU conceived and designed the study; AO, HU, NO, KM, TOk, TH, HA, SS, YK, NT and KY contributed to collection and assembling of the data. AO analysed the data and wrote the draft of the manuscript, having primary responsibility for the final content. All the authors critically reviewed and approved the final version of the manuscript.
Funding: This study was supported by a Grant-in-Aid from the Ministry of Health, Labour and Welfare under the auspices of the Japanese Association for Cerebro-cardiovascular Disease Control, a Research Grant for Cardiovascular Diseases (7A-2) from the Ministry of Health, Labour and Welfare, and Health and Labour Sciences Research Grants, Japan (Comprehensive Research on Aging and Health (H11-Chouju-046, H14-Chouju-003, H17-Chouju-012, H19-Chouju-Ippan-014) and Comprehensive Research on Life-Style Related Diseases including Cardiovascular Diseases and Diabetes Mellitus (H22-Junkankitou-Seishuu -Sitei-017, H25-Junkankitou-Seishuu-Sitei-022)).
Competing interests: None declared.
Ethics approval: Approval for this study was obtained from the Institutional Review Board of Shiga University of Medical Science.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
Contributor Information
Collaborators: Kiyomi Sakata, Atsushi Hozawa, Yosikazu Nakamura, Nobuo Nishi, Fumiyoshi Kasagi, Yoshitaka Murakami, Toru Izumi, Yasuhiro Matsumura, Toshiyuki Ojima, Koji Tamakoshi, Hideaki Nakagawa, Yoshikuni Kita, Aya Kadota, Naomi Miyamatsu, Yasuyuki Nakamura, Yoshihiro Miyamoto, and Kazunori Kodama
References
- 1.Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ 1988;297:319–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. BMJ 2013;346:f1325 10.1136/bmj.f1325 [DOI] [PubMed] [Google Scholar]
- 3.Binia A, Jaeger J, Hu Y et al. Daily potassium intake and sodium-to-potassium ratio in the reduction of blood pressure: a meta-analysis of randomized controlled trials. J Hypertens 2015;33:1509–20. 10.1097/HJH.0000000000000611 [DOI] [PubMed] [Google Scholar]
- 4.Ministry of Health, Labour and Welfare, ed National Nutrition and Health Survey, 2010. Tokyo: Daiichi Shuppan, 2012. [Google Scholar]
- 5.Rose G, Stamler J. The INTERSALT study: background, methods and main results. INTERSALT Co-operative Research Group. J Hum Hypertens 1989;3:283–8. [PubMed] [Google Scholar]
- 6.Stamler J, Elliott P, Dennis B et al. INTERMAP: background, aims, design, methods, and descriptive statistics (nondietary). J Hum Hypertens 2003;17:591–608. 10.1038/sj.jhh.1001603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geleijnse JM, Witteman JC, Stijnen T et al. Sodium and potassium intake and risk of cardiovascular events and all-cause mortality: the Rotterdam Study. Eur J Epidemiol 2007;22:763–70. 10.1007/s10654-007-9186-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stamler J, Rose G, Stamler R et al. INTERSALT study findings. Public health and medical care implications. Hypertension 1989;14:570–7. [DOI] [PubMed] [Google Scholar]
- 9.Whelton PK. Sodium, potassium, blood pressure, and cardiovascular disease in humans. Curr Hypertens Rep 2014;16:465 10.1007/s11906-014-0465-5 [DOI] [PubMed] [Google Scholar]
- 10.Cook NR, Obarzanek E, Cutler JA et al. Joint effects of sodium and potassium intake on subsequent cardiovascular disease: the Trials of Hypertension Prevention follow-up study. Arch Intern Med 2009;169:32–40. 10.1001/archinternmed.2008.523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang Q, Liu T, Kuklina EV et al. Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey. Arch Intern Med 2011;171:1183–91. 10.1001/archinternmed.2011.257 [DOI] [PubMed] [Google Scholar]
- 12.Judd SE, Aaron KJ, Letter AJ et al. High sodium:potassium intake ratio increases the risk for all-cause mortality: the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. J Nutr Sci 2013;2:e13 10.1017/jns.2013.4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ueshima H, Iida M, Shimamoto T et al. Dietary intake and serum total cholesterol level: their relationship to different lifestyles in several Japanese populations. Circulation 1982;66:519–26. 10.1161/01.CIR.66.3.519 [DOI] [PubMed] [Google Scholar]
- 14.Iso H, Imano H, Kitamura A et al. Type 2 diabetes and risk of non-embolic ischaemic stroke in Japanese men and women. Diabetologia 2004;47:2137–44. 10.1007/s00125-004-1587-0 [DOI] [PubMed] [Google Scholar]
- 15.Lida M, Ueda K, Okayama A et al. , Nippon Data 80 Research Group. Impact of elevated blood pressure on mortality from all causes, cardiovascular diseases, heart disease and stroke among Japanese: 14 year follow-up of randomly selected population from Japanese—NIPPON DATA80. J Hum Hypertens 2003;17:851–7. 10.1038/sj.jhh.1001602 [DOI] [PubMed] [Google Scholar]
- 16.Ministry of Health and Welfare, ed National Nutrition Survey, 1980. Daiichi Shuppan, 1982. [Google Scholar]
- 17.Dennis B, Stamler J, Buzzard M et al. , INTERMAP Research Group. INTERMAP: the dietary data—process and quality control. J Hum Hypertens 2003;17:609–22. 10.1038/sj.jhh.1001604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Okuda N, Miura K, Yoshita K et al. Integration of data from NIPPON DATA80/90 and National Nutrition Survey in Japan: for cohort studies of representative Japanese on nutrition. J Epidemiol 2010;20(Suppl 3):S506–14. 10.2188/jea.JE20090218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nakamura Y, Okuda N, Turin TC et al. , NIPPON DATA80/90 Research Group. Comparison of the National Nutritional Survey in Japan estimated individual-based nutritional data and NIPPON DATA80 food frequency questionnaires. J Epidemiol 2010;20(Suppl 3):S582–6. 10.2188/jea.JE20090228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nagata C, Takatsuka N, Shimizu N et al. Sodium intake and risk of death from stroke in Japanese men and women. Stroke 2004;35:1543–7. 10.1161/01.STR.0000130425.50441.b0 [DOI] [PubMed] [Google Scholar]
- 21.Umesawa M, Iso H, Date C et al. , JACC Study Group. Relations between dietary sodium and potassium intakes and mortality from cardiovascular disease: the Japan Collaborative Cohort Study for Evaluation of Cancer Risks. Am J Clin Nutr 2008;88:195–202. [DOI] [PubMed] [Google Scholar]
- 22.Cook NR, Cutler JA, Obarzanek E et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ 2007;334:885–8. 10.1136/bmj.39147.604896.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Toft U, Kristoffersen L, Ladelund S et al. Relative validity of a food frequency questionnaire used in the Inter99 study. Eur J Clin Nutr 2008;62:1038–46. 10.1038/sj.ejcn.1602815 [DOI] [PubMed] [Google Scholar]
- 24.Iso H, Stampfer MJ, Manson JE et al. Prospective study of calcium, potassium, and magnesium intake and risk of stroke in women. Stroke 1999;30:1772–9. 10.1161/01.STR.30.9.1772 [DOI] [PubMed] [Google Scholar]
- 25.Sasaki S, Ishihara J, Tsugane S. Validity of a self-administered food frequency questionnaire in the 5-year follow-up survey of the JPHC Study Cohort I to assess sodium and potassium intake: comparison with dietary records and 24-hour urinary excretion level. J Epidemiol 2003;13:S102–5. 10.2188/jea.13.1sup_102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Murakami K, Sasaki S, Uenishi K et al. The degree of misreporting of the energy-adjusted intake of protein, potassium, and sodium does not differ among under-, acceptable, and over-reporters of energy intake. Nutr Res 2012;32:741–50. 10.1016/j.nutres.2012.09.001 [DOI] [PubMed] [Google Scholar]
- 27.Tsubono Y, Fahey MT, Takahashi T et al. Interpopulation and intrapopulation variability of nutrient intake in five regions of Japan. Eur J Clin Nutr 1998;52:176–9. 10.1038/sj.ejcn.1600531 [DOI] [PubMed] [Google Scholar]
- 28.Cobb LK, Anderson CA, Elliott P et al. Methodological issues in cohort studies that relate sodium intake to cardiovascular disease outcomes: a science advisory from the American Heart Association. Circulation 2014;129:1173–86. 10.1161/CIR.0000000000000015 [DOI] [PubMed] [Google Scholar]
- 29.Cohen HW, Hailpern SM, Fang J et al. Sodium intake and mortality in the NHANES II follow-up study. Am J Med 2006;119:275.e7–14. 10.1016/j.amjmed.2005.10.042 [DOI] [PubMed] [Google Scholar]
- 30.Zia E, Hedblad B, Pessah-Rasmussen H et al. Blood pressure in relation to the incidence of cerebral infarction and intracerebral hemorrhage. Hypertensive hemorrhage: debated nomenclature is still relevant. Stroke 2007;38:2681–5. [DOI] [PubMed] [Google Scholar]
- 31.Saito I, Ozawa H, Aono H et al. Trends in fatal coronary heart disease among people aged 25-74 years in Oita City, Japan, from 1987-1998. J Clin Epidemiol 2002;55:469–76. 10.1016/S0895-4356(01)00516-9 [DOI] [PubMed] [Google Scholar]
- 32.Ueshima H, Tatara K, Asakura S et al. Declining trends in blood pressure level and the prevalence of hypertension, and changes in related factors in Japan, 1956-1980. J Chronic Dis 1987;40:137–47. 10.1016/0021-9681(87)90065-8 [DOI] [PubMed] [Google Scholar]
- 33.Okuda N, Okayama A, Miura K et al. Food sources of dietary sodium in the Japanese adult population: the international study of macro-/micronutrients and blood pressure (INTERMAP). Eur J Nutr 2016. 10.1007/s00394-016-1177-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kilcast D, Angus F, eds. Reducing salt in foods-practical strategies. Cambridge, UK: Woodhead Publishing, 2007. [Google Scholar]
- 35.Ministry of Health, Labour and Welfare. Vital Statistics. Department of Statistics and Information, Ministry of Health, Labour and Welfare, Tokyo, 2014:227. [Google Scholar]
- 36.Okuda N, Miura K, Okayama A et al. Fruit and vegetable intake and mortality from cardiovascular disease in Japan: a 24-year follow-up of the NIPPON DATA80 Study. Eur J Clin Nutr 2015;69:482–8. 10.1038/ejcn.2014.276 [DOI] [PubMed] [Google Scholar]
- 37.Chang HY, Hu YW, Yue CS et al. Effect of potassium-enriched salt on cardiovascular mortality and medical expenses of elderly men. Am J Clin Nutr 2006;83:1289–96. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-011632supp.pdf (180.5KB, pdf)