Abstract
The lateral meniscus plays a critical role in the stability and health of the knee. Treating patients who have undergone a total lateral meniscectomy or functional equivalent is challenging, especially young and active patients. Current literature regarding meniscal tears supports that repair should be the first surgical option. Moreover, it is recommended to preserve as much meniscal tissue as possible. In cases in which a total or functional meniscectomy is a pre-existing condition, a lateral meniscal allograft transplantation is a possible option. The purpose of this surgical technique description was to detail the method of lateral meniscal allograft transplantation using a bone trough.
Meniscal tears are one of the most common lesions in orthopaedics. Load absorption and distribution, as well as knee stability, are some of the most important functions of the menisci.1, 2 When a meniscectomy leads to symptoms that could indicate an imminent early onset of osteoarthritis, meniscal allograft transplantation (MAT) arises as a viable treatment option.
Patients who have undergone a lateral meniscectomy show worse clinical and radiographic outcomes than patients with a medial meniscectomy.3, 4 This may be a consequence of the less congruent articular surfaces of the lateral side and the greater degree of translation compared with the medial compartment.2 Moreover, the lateral meniscus absorbs 70% of the load whereas the medial meniscus only absorbs 50%.5
Several MAT techniques have been described to restore knee biomechanics and decrease the risk of osteoarthritis. This procedure can be performed using an open or arthroscopic technique. Three different fixation methods have been reported: soft-tissue, bone plug, or bone trough fixation. Regarding lateral meniscal allograft transplantation (LMAT), the bone trough technique is the most commonly used and has shown superior results.6, 7 LMAT has very precise indications, and therefore, patient selection is key to obtain good results. The purpose of this surgical technique description was to describe our method of LMAT using the bone trough method.
Surgical Technique
Objective Diagnosis
Imaging studies such as weight-bearing radiographs, long-standing radiographs, and magnetic resonance imaging (MRI) should be obtained. Partial or total meniscectomies can be evaluated on axial, coronal, and/or sagittal MRI views. The classic MRI presentation of a meniscectomy is seen as absence of an identifiable meniscus in the lateral compartment. An arthroscopic evaluation can be performed to determine whether the patient is a suitable candidate for LMAT.8, 9
Indications for Surgery
The criteria used as indications for LMAT include isolated lateral-compartment knee pain and post-activity effusion after a subtotal, total, or functionally equivalent meniscectomy in patients with closed physes in whom a trial of conservative therapy has failed (Video 1). The physes must be closed or closing to avoid physeal arrest and alignment deformities. The patient should be evaluated for valgus malalignment; this must be corrected to neutral alignment before or at the same time as the LMAT procedure. Obesity should be considered a relative contraindication to LMAT; some authors deem this procedure to be contraindicated in patients with a body mass index of more than 30 kg/m2 because it increases the loads on the knee compartments, thereby making the allograft more susceptible to failure.10 For more precise indications, a diagnostic arthroscopic evaluation is often performed to assess the current status of the lateral compartment and to determine whether the patient is suitable for this operation.8, 9
Patients with grade IV chondromalacia according to the Outerbridge classification, except for those who are candidates for a concurrent articular cartilage–resurfacing procedure, especially those with opposing cartilage surfaces with grade IV chondromalacia, should not be considered candidates for meniscal transplantation.8 Additional limb alignment or cartilage procedures can be performed concurrently or before LMAT if necessary.6, 11, 12 A summary of the indications and contraindications for our technique can be found in Table 1.
Table 1.
Indications and Contraindications
| Indications (must have all) |
| Unicompartmental knee pain |
| Post-activity effusion |
| Total or subtotal knee meniscectomy |
| Failure of conservative treatment |
| Contraindications |
| Open physes |
| BMI >35 kg/m2 |
| Noncorrectable grade IV chondromalacia∗ |
| Malalignment† |
BMI, body mass index.
Unless performed with concurrent articular cartilage–resurfacing procedure.
Unless performed with concurrent realignment procedure.
Graft Preparation and Selection
Fresh-frozen, non-irradiated or non–antigen-matched grafts are the preferred choice for MAT. Verdonk et al.13, 14 reported the use of viable grafts that can be maintained in culture for 2 weeks, which allows for testing of infectious diseases while preserving cell viability. Irradiation is no longer used because of its deleterious effect on graft survival, which negatively affects the long-term outcomes of the graft.10, 14, 15 Lyophilized meniscal grafts have higher reported failure rates, and their use has been abandoned.10, 14, 15, 16
Graft sizing is fundamental for a successful outcome of LMAT. One of the most widely used sizing methods is the one described by Pollard et al.,17 which incorporates radiographic measurements to improve graft sizing. Meniscal width is equal to the distance (coronal) from the peak of the lateral tibial eminence to the periphery of the tibial lateral compartment on anteroposterior films. Meniscal length is measured from lateral radiographs. The length can be calculated as 70% of the measured sagittal length of the tibial plateau, with a measurement error average of 7.8%.17
Patient Positioning and Anesthesia
The patient is placed in the supine position on the operating table. After induction of general anesthesia, a bilateral knee examination is performed to evaluate for any concurrent ligamentous instability and to assess for range of motion. A well-padded high-thigh tourniquet is subsequently placed on the operative leg, which is then placed into a leg holder (Mizuho OSI, Union City, CA) while the contralateral knee is placed into an abduction stirrup (Birkova Products, Gothenburg, NE). The leg holder should be placed proximal enough to allow exposure of the posterolateral corner for an inside-out meniscal repair. The foot of the operating table is then lowered, allowing for the surgeon to freely manipulate the knee as needed.
LMAT Procedure
Standard anterolateral and anteromedial portals are created adjacent to the patellar tendon and the joint is visualized with a 30° arthroscope (Smith & Nephew, Andover, MA) while the knee is insufflated with normal saline solution (Video 1). A diagnostic arthroscopy is performed to confirm the absence of significant chondral lesions. After the patient is confirmed to be a candidate for LMAT (if the diagnosis was not confirmed during a previous diagnostic arthroscopy), the meniscal allograft (JRF Ortho, Centennial, CO) is thawed in room-temperature saline solution.
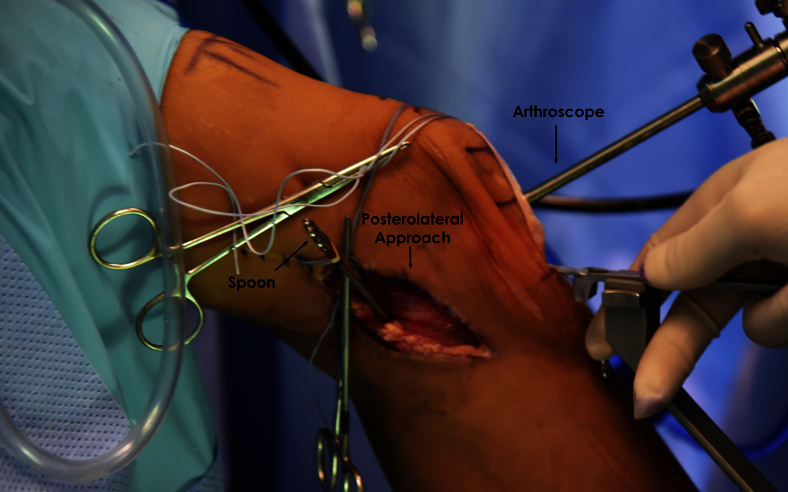
An arthroscopic shaver (Smith & Nephew) is inserted into the knee, and the remnants of the meniscal tissue are debrided to a bleeding rim of approximately 1 mm. The residual meniscal rim should not be completely removed because it prevents radial displacement of the allograft and fits as a firm bed for meniscal fixation.13, 18 The lateral incision for meniscal sutures is made over the joint line along the distal border of the superficial iliotibial band. Then the iliotibial band is incised approximately 5 mm anterior to the posterior margin of the superficial layer of the iliotibial band, and blunt dissection is performed toward the fibular head. To reach the posterolateral joint capsule and avoid injuring the peroneal nerve, dissection should be carefully performed superior to the biceps femoris complex and anterior to the lateral gastrocnemius tendon. An elevator is then used to release adhesions between the posterior capsule and the gastrocnemius. By use of the same interval, a spoon is inserted and used as a retractor; its placement will prevent injury to the neurovascular bundle posteriorly.
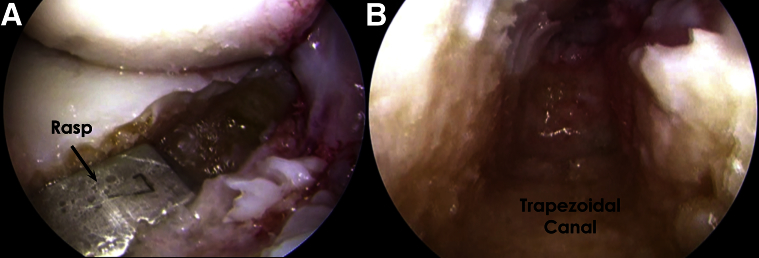
Next, both meniscal root attachments should be identified arthroscopically. With the aid of an arthroscopic shaver (Smith & Nephew) and a curette, the cartilage is decorticated down to bone and a straight line is created between these 2 structures, just lateral to the tibial attachment of the anterior cruciate ligament (ACL). A lateral parapatellar arthrotomy is created that incorporates the anterolateral portal to allow for the passage of the graft. An alignment rod (Biomet, Warsaw, IN) is positioned along the previously prepared decorticated zone between the anterior and posterior horn attachments. Then a trapezoidal osteotome (Biomet), with depth line and length markings, is oriented vertically just off the patellar tendon and advanced using a mallet into the tibial plateau to create a trapezoidal canal (Fig 1). The osteotome is advanced until a posterior cortical wall of 1 to 2 mm remains. The posterior bone trough should be set at the far medial edge of the lateral tibial plateau and just adjacent to the lateral edge of the ACL. A dilating rasp (Biomet) is used several times to achieve the desired dimensions (Fig 2). The trapezoidal canal should be measured to ensure a perfect fit to the allograft.
Fig 1.
Use of a bone-cutting device to create a trapezoidal bone canal on the lateral tibial plateau for bone block insertion (right knee). A spoon is placed into the posterolateral portal to protect the posterior neurovascular structures. After the bone-cutting device is aligned, a trapezoidal osteotome is oriented vertically just lateral to the patellar tendon and advanced using a mallet into the tibial plateau to create a canal for the bone block.
Fig 2.
(A) A 7-mm dilating rasp being used to expand the bone trough. (B) Trapezoidal shape of the slot that connects the anterior and posterior roots of the lateral meniscus.
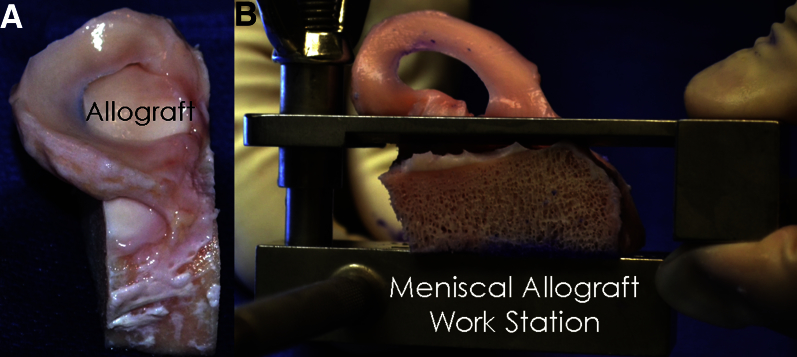
The preparation of the bone trough meniscal allograft (Fig 3) is divided into 2 stages. First, the bone graft should be measured and marked. The bone block is trimmed of excess bone and soft tissue to better identify the meniscal roots. This also allows for a better fit into the meniscal allograft workstation (Biomet). By use of this device, the allograft is cut into a trapezoid to fit the tibial canal previously made. It is important to size it precisely to have good bone-to-bone fixation and to avoid bone plug prominence (Fig 4).
Fig 3.
(A) Lateral meniscal allograft before preparation and (B) use of custom instruments to help with bone cutting during preparation (right knee).
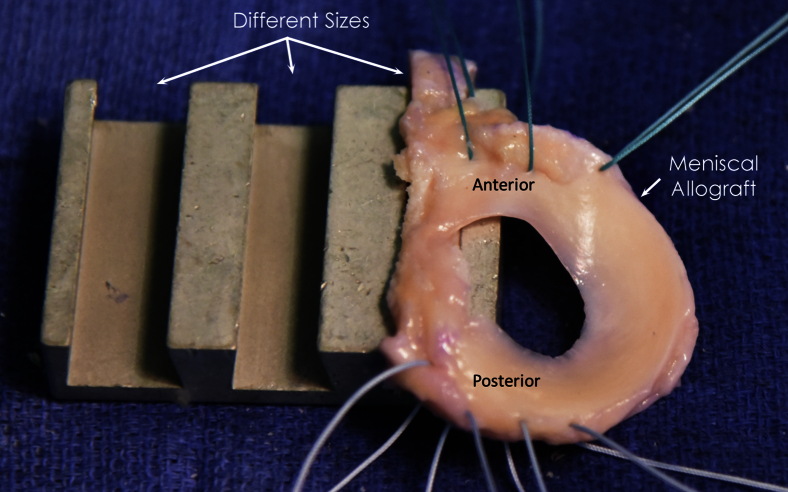
Fig 4.
Measurement of bone block of lateral meniscal allograft. Three sutures (green) have been placed through the anterior horn and 4 sutures through the posterior horn (white).
Then the meniscal portion of the allograft is prepared with 4 nonabsorbable sutures (No. 2 FiberWire; Arthrex, Naples, FL) placed in the posterior horn and 3 nonabsorbable sutures in the anterior horn (Fig 5). These sutures will be used for the intra-articular fixation of the graft. Marking the external border of the meniscal allograft with methylene blue is useful to differentiate it from the remaining meniscal rim when inserting the sutures arthroscopically (Fig 5).
Fig 5.
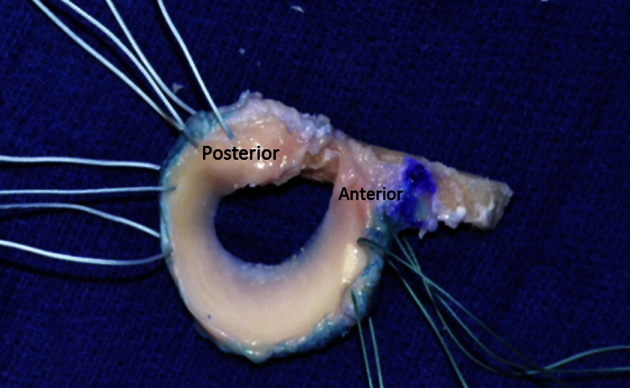
Prepared lateral meniscal allograft with 4 sutures (white) in posterior horn and 3 sutures (green) in anterior horn.
Four passing sutures are then passed through the posterior capsule in an inside-out fashion with the aid of the tip of a curved Adson pointed hemostat (Aesculap, Center Valley, PA) to bluntly pierce the capsule while the surgeon controls the exit point using his or her finger from the lateral incision. These passing sutures will match the location of the graft sutures in the posterior horn.
Before insertion of the bone trough of the graft into the trough, the passing sutures are used to pass the posterior horn meniscal allograft sutures out of the posterolateral capsule (Fig 6A). Then the allograft is inserted (Fig 6B), the trapezoidal bone plug is pushed into the tibial bone slot, and the posterior horn sutures are pulled through the posterior capsule. For graft reduction, a varus force should be applied to the knee with 30° of flexion to allow the allograft to pass under the lateral femoral condyle. The bony portion of the posterior horn of the lateral meniscus transplant graft should be placed as far posteriorly as possible to avoid graft impingement from the lateral femoral condyle. To achieve this, the graft can be gently impacted into the canal (Fig 7). Once the allograft is reduced, the knee is cycled several times to properly position the meniscus.
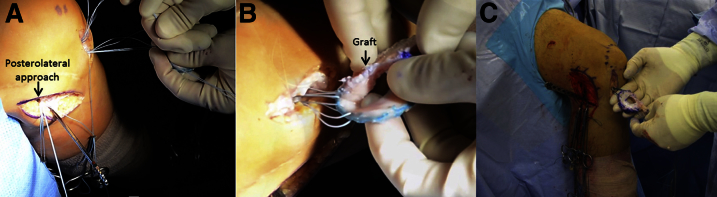
Fig 6.
(A) The previously placed posterior passing sutures are matched with the posterior horn meniscal sutures, and the passing sutures are then pulled through the posterolateral incision (B, C) to pull the allograft into the lateral compartment of the knee (right knee).
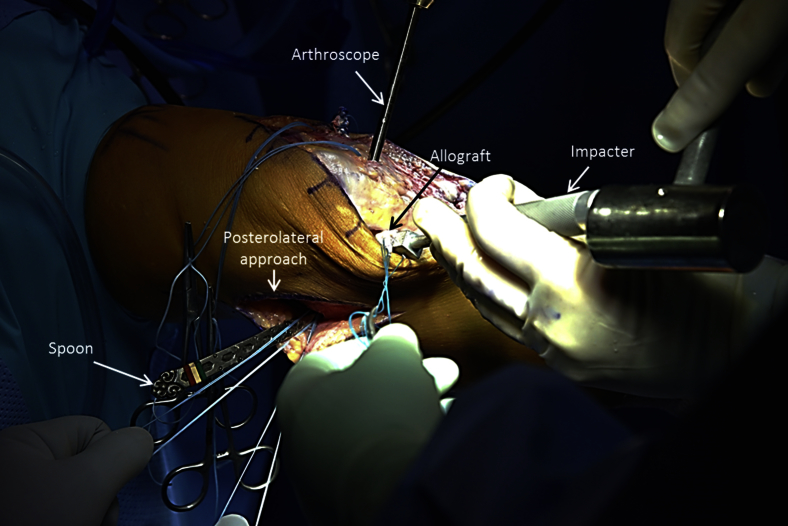
Fig 7.
After the meniscal allograft is inserted into the knee, it is gently impacted while being arthroscopically visualized through the anteromedial portal. Although mainly used for the posterior horn sutures, the spoon is left in place (in the posterolateral approach) to protect the posterior neurovascular structures (right knee).
The posterior sutures are tied in a cross-matched fashion (i.e., 1 arm of the first suture with 1 arm of the second suture) to make a stronger construct. Anteriorly placed sutures (3) are tied to the anterior capsule with a free needle. Finally, the rest of the meniscal allograft is secured with a total of 6 to 10 nonabsorbable vertical sutures placed 5 mm apart and distributed on both its superior and inferior surfaces (along the capsule) with an arthroscopically assisted inside-out technique. Table 2 summarizes the pearls and pitfalls of our technique.
Table 2.
Pearls, Pitfalls, and Risks
| Pearls |
| The posterolateral joint line should be identified with a probe through the regular portals to define the best location for the lateral approach. |
| During debridement of the remnant meniscus, the surgeon should leave a 1-mm rim of bleeding meniscal tissue to prevent displacement of the allograft. |
| A 90° curette should be used to detach the posterior horn attachment to improve visualization of the tibia's back wall. |
| The surgeon should use his or her finger to feel the posterior capsule while it is pierced by the hemostat. This aids in the precise placement of the passing sutures. |
| The edges of the meniscal allograft should be marked to help orientation. |
| The posterior sutures should be tied in a cross-matched fashion to create a stronger construct. |
| The distance between the sutures should be 3-5 mm. Usually 6 vertical mattress sutures are placed in the superior and inferior surfaces of the meniscus between the anterior and posterior fixations. |
| Pitfalls and risks |
| Failure to address concomitant conditions such as instability and malalignment may lead to poor results. |
| Patients with grade IV chondromalacia must be evaluated for a concomitant cartilage–resurfacing procedure. Otherwise, they are not good candidates for MAT. |
| MAT in patients with open physes can lead to growth arrest. |
| Injury to the common peroneal nerve is a risk in posterolateral approaches. The surgeon should keep the lateral dissection anterior to the biceps tendon and lateral head of the gastrocnemius to avoid the nerve. |
| Before creating the trapezoidal trough that will receive the bone portion of the graft, the surgeon should measure the length of the tibial plateau and use a calibrated device leaving a 2-mm posterior back wall to avoid posterior trough blowout. |
| Stiffness can occur if the patient is not able to follow the established rehabilitation protocol. Assisted mobilization should be initiated on the first day postoperatively and should be limited to 90° for the first 2 weeks. |
MAT, meniscal allograft transplantation.
Postoperative Rehabilitation
Postoperatively, weight bearing is not allowed until week 6. For the first 2 weeks, progressive assisted range of motion is allowed from 0° to 90°. Full range of motion is allowed from the third week onward. At week 6, patients are allowed to bear weight as tolerated and to wean off crunches progressively.
Thereafter stationary bike exercise and progressive low-impact rehabilitation are encouraged as tolerated. Deep squatting should be avoided until at least 4 months postoperatively. At 6 to 9 months postoperatively, the patient may return to full low-impact activities like walking, swimming, and elliptical machine use. High-impact activities are always discouraged, especially in patients with greater than grade I chondromalacia in the lateral compartment.
Discussion
LMAT has been shown to be a safe and successful procedure in patients who meet the indications. MAT results in reduced subjective pain, less activity-related effusion, and improved functional activities in patients with a previous meniscectomy.8, 11, 14, 19, 20 LaPrade et al.8 reported a significant improvement in symptoms after LMAT at a minimum 2-year follow-up, as measured by the Modified Cincinnati subjective outcome survey (57.8 preoperatively vs 77.9 postoperatively) and International Knee Documentation Committee (IKDC) subjective scores (52.3 preoperatively vs 73.2 postoperatively). Sekiya et al.6 reported that in 96% of patients, overall function and activity level were improved after isolated LMAT, with an average 3.3-year follow-up, as measured with Short Form 36, Lysholm, and IKDC scores. They have also suggested that earlier meniscal transplantation, before the onset of significant joint space narrowing, may result in improved outcomes.
The graft sizing method used by the senior author (R.F.L.) for MAT is the same one described by Pollard et al.17 With this method, they reported a size mismatch occurrence in fewer than 5% of cases. Concomitant procedures such as joint alignment, ligament stabilization, and cartilage resurfacing should improve the survival of the graft and should be performed during the same surgical procedure or before MAT.21
Cadaveric studies have shown bone fixation to more closely replicate normal meniscal function and to have a better chondroprotective effect.22 Sekiya et al.6 reported an increased range of motion with the use of bone fixation compared with soft-tissue fixation. Rodeo7 reported a success rate of 88% in patients who underwent MAT with bone fixation compared with a 44% success rate in patients who underwent only soft-tissue fixation, as measured with the Lysholm and IKDC scores.
A list of advantages and limitations of our procedure can be found on Table 3. One of the most frequent problems after LMAT is meniscal extrusion, which leads to a decrease in tibial coverage of the meniscus and results in a less chondroprotective effect.16 However, few studies have evaluated the relation between meniscal extrusion and clinical results. Verdonk et al.13 reported no significant difference in the progression of cartilage degeneration between patients with and patients without meniscal extrusion. However, no consensus exists for the management of patients with meniscal extrusion after MAT. Verdonk et al.13 also reported that meniscal extrusion might be a consequence of overstuffing caused by the remnant meniscal rim. Therefore, the functional area of the allograft should be equivalent to that of the normal meniscus.13, 18 It has been reported that patients with advanced osteoarthritis have a higher propensity for graft extrusion.7
Table 3.
Advantages and Limitations
| Advantages |
| Efficient placement of graft |
| Maintenance of native anterior-posterior distance between meniscal roots |
| Possibly less graft extrusion when compared with soft-tissue fixation |
| Enhanced chondroprotective effect when compared with soft-tissue fixation |
| Limitations |
| Risk of graft size mismatch if not precisely measured preoperatively |
| No possibility to change root insertions in case of mismatch |
| Requirement for larger parapatellar incision to allow for passage of graft into joint |
The degree of cartilage wear at the time of MAT is the most important variable of outcome prediction.11, 12 Von Lewinski et al.23 published a 20-year follow-up study showing no significant difference between the radiographic joint space of the affected knee and that of the uninvolved knee.
In conclusion, LMAT is a safe procedure that has shown good mid-term outcomes. All patients should be informed that LMAT is not a curative procedure but should be able to delay cartilage wear and preserve the knee joint. Few long-term studies have reported the chondroprotective effects of the LMAT procedure. However, because pain and swelling are decreased, we can infer that the progression rate of arthritis is slowed. We encourage other groups to perform this surgical procedure and report on long-term outcomes.
Footnotes
The authors report the following potential conflict of interest or source of funding: R.F.L. receives support from Arthrex, Smith & Nephew, Ossur, Health East Norway, and a National Institutes of Health R13 grant for biologics.
Supplementary Data
Surgical technique of lateral meniscal allograft transplantation with use of a bone trough. The patient is placed supine on the operating table, and standard anterolateral and anteromedial portals are created adjacent to the patellar tendon. Remnants of the lateral meniscal tissue are debrided to a bleeding rim of approximately 1 mm. The lateral incision for the meniscal repair is made over the joint line along the distal border of the superficial iliotibial band. Both meniscal root attachments are identified arthroscopically. An arthroscopic shaver and a curette are used to decorticate the cartilage down to bone, and a straight line is created between these 2 structures, just lateral to the tibial attachment of the anterior cruciate ligament. A lateral parapatellar arthrotomy is created to allow for the passage of the graft. A trapezoidal osteotome is oriented vertically just off the patellar tendon and advanced using a mallet into the tibial plateau to create a trapezoidal canal. The canal is then dilated to 7 mm. The bone block is trimmed of excess bone and soft tissue to better identify the meniscal roots. The allograft is cut into a trapezoid to fit the tibial canal previously made. The meniscal portion of the allograft is prepared with 4 nonabsorbable sutures placed in the posterior horn and 3 nonabsorbable sutures in the anterior horn. Four passing sutures are then passed through the posterior capsule in an inside-out fashion with the aid of the tip of a curved Adson pointed hemostat (Aesculap, Center Valley, PA) to bluntly pierce the capsule. These passing sutures are used to pass the posterior horn meniscal allograft sutures out of the posterolateral capsule before insertion of the graft. The allograft is inserted and the trapezoidal bone plug is pushed into the tibial bone slot. The posterior horn sutures are pulled through the posterior capsule. For graft reduction, a varus force should be applied to the knee with 30° of flexion to allow the allograft to pass under the lateral femoral condyle. Anteriorly placed sutures (3) are tied to the anterior capsule. Finally, the rest of the meniscal allograft is secured with a total of 6 to 10 nonabsorbable vertical mattress sutures placed 5 mm apart with an arthroscopically assisted inside-out technique.
References
- 1.Allen P.R., Denham R.A., Swan A.V. Late degenerative changes after meniscectomy. Factors affecting the knee after operation. J Bone Joint Surg Br. 1984;66:666–671. doi: 10.1302/0301-620X.66B5.6548755. [DOI] [PubMed] [Google Scholar]
- 2.Fairbank T.J. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30:664–670. [PubMed] [Google Scholar]
- 3.Raber D.A., Friederich N.F., Hefti F. Discoid lateral meniscus in children. Long-term follow-up after total meniscectomy. J Bone Joint Surg Am. 1998;80:1579–1586. doi: 10.2106/00004623-199811000-00003. [DOI] [PubMed] [Google Scholar]
- 4.McNicholas M.J., Rowley D.I., McGurty D. Total meniscectomy in adolescence. A thirty-year follow-up. J Bone Joint Surg Br. 2000;82:217–221. [PubMed] [Google Scholar]
- 5.Messner K., Gao J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat. 1998;193:161–178. doi: 10.1046/j.1469-7580.1998.19320161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sekiya J.K., West R.V., Groff Y.J., Irrgang J.J., Fu F.H., Harner C.D. Clinical outcomes following isolated lateral meniscal allograft transplantation. Arthroscopy. 2006;22:771–780. doi: 10.1016/j.arthro.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 7.Rodeo S.A. Meniscal allografts—Where do we stand? Am J Sports Med. 2001;29:246–261. doi: 10.1177/03635465010290022401. [DOI] [PubMed] [Google Scholar]
- 8.LaPrade R.F., Wills N.J., Spiridonov S.I., Perkinson S. A prospective outcomes study of meniscal allograft transplantation. Am J Sports Med. 2010;38:1804–1812. doi: 10.1177/0363546510368133. [DOI] [PubMed] [Google Scholar]
- 9.Brophy R.H., Matava M.J. Surgical options for meniscal replacement. J Am Acad Orthop Surg. 2012;20:265–272. doi: 10.5435/JAAOS-20-05-265. [DOI] [PubMed] [Google Scholar]
- 10.Abat F., Gelber P.E., Erquicia J.I., Pelfort X., Gonzalez-Lucena G., Monllau J.C. Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med. 2012;40:1591–1596. doi: 10.1177/0363546512446674. [DOI] [PubMed] [Google Scholar]
- 11.van Arkel E.R., de Boer H.H. Human meniscal transplantation. Preliminary results at 2 to 5-year follow-up. J Bone Joint Surg Br. 1995;77:589–595. [PubMed] [Google Scholar]
- 12.Garrett J.C., Steensen R.N. Meniscal transplantation in the human knee: A preliminary report. Arthroscopy. 1991;7:57–62. doi: 10.1016/0749-8063(91)90079-d. [DOI] [PubMed] [Google Scholar]
- 13.Verdonk P.C., Verstraete K.L., Almqvist K.F. Meniscal allograft transplantation: Long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc. 2006;14:694–706. doi: 10.1007/s00167-005-0033-2. [DOI] [PubMed] [Google Scholar]
- 14.Verdonk P.C., Demurie A., Almqvist K.F., Veys E.M., Verbruggen G., Verdonk R. Transplantation of viable meniscal allograft. Survivorship analysis and clinical outcome of one hundred cases. J Bone Joint Surg Am. 2005;87:715–724. doi: 10.2106/JBJS.C.01344. [DOI] [PubMed] [Google Scholar]
- 15.Vangsness C.T., Jr., Garcia I.A., Mills C.R., Kainer M.A., Roberts M.R., Moore T.M. Allograft transplantation in the knee: Tissue regulation, procurement, processing, and sterilization. Am J Sports Med. 2003;31:474–481. doi: 10.1177/03635465030310032701. [DOI] [PubMed] [Google Scholar]
- 16.Wirth C.J., Peters G., Milachowski K.A., Weismeier K.G., Kohn D. Long-term results of meniscal allograft transplantation. Am J Sports Med. 2002;30:174–181. doi: 10.1177/03635465020300020501. [DOI] [PubMed] [Google Scholar]
- 17.Pollard M.E., Kang Q., Berg E.E. Radiographic sizing for meniscal transplantation. Arthroscopy. 1995;11:684–687. doi: 10.1016/0749-8063(95)90110-8. [DOI] [PubMed] [Google Scholar]
- 18.Verdonk P., Depaepe Y., Desmyter S. Normal and transplanted lateral knee menisci: Evaluation of extrusion using magnetic resonance imaging and ultrasound. Knee Surg Sports Traumatol Arthrosc. 2004;12:411–419. doi: 10.1007/s00167-004-0500-1. [DOI] [PubMed] [Google Scholar]
- 19.Matava M.J. Meniscal allograft transplantation: A systematic review. Clin Orthop Relat Res. 2007;455:142–157. doi: 10.1097/BLO.0b013e318030c24e. [DOI] [PubMed] [Google Scholar]
- 20.Cole B.J., Carter T.R., Rodeo S.A. Allograft meniscal transplantation: Background, techniques, and results. Instr Course Lect. 2003;52:383–396. [PubMed] [Google Scholar]
- 21.Stone K.R., Adelson W.S., Pelsis J.R., Walgenbach A.W., Turek T.J. Long-term survival of concurrent meniscus allograft transplantation and repair of the articular cartilage: A prospective two- to 12-year follow-up report. J Bone Joint Surg Br. 2010;92:941–948. doi: 10.1302/0301-620X.92B7.23182. [DOI] [PubMed] [Google Scholar]
- 22.Chen M.I., Branch T.P., Hutton W.C. Is it important to secure the horns during lateral meniscal transplantation? A cadaveric study. Arthroscopy. 1996;12:174–181. doi: 10.1016/s0749-8063(96)90007-9. [DOI] [PubMed] [Google Scholar]
- 23.von Lewinski G., Milachowski K.A., Weismeier K., Kohn D., Wirth C.J. Twenty-year results of combined meniscal allograft transplantation, anterior cruciate ligament reconstruction and advancement of the medial collateral ligament. Knee Surg Sports Traumatol Arthrosc. 2007;15:1072–1082. doi: 10.1007/s00167-007-0362-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical technique of lateral meniscal allograft transplantation with use of a bone trough. The patient is placed supine on the operating table, and standard anterolateral and anteromedial portals are created adjacent to the patellar tendon. Remnants of the lateral meniscal tissue are debrided to a bleeding rim of approximately 1 mm. The lateral incision for the meniscal repair is made over the joint line along the distal border of the superficial iliotibial band. Both meniscal root attachments are identified arthroscopically. An arthroscopic shaver and a curette are used to decorticate the cartilage down to bone, and a straight line is created between these 2 structures, just lateral to the tibial attachment of the anterior cruciate ligament. A lateral parapatellar arthrotomy is created to allow for the passage of the graft. A trapezoidal osteotome is oriented vertically just off the patellar tendon and advanced using a mallet into the tibial plateau to create a trapezoidal canal. The canal is then dilated to 7 mm. The bone block is trimmed of excess bone and soft tissue to better identify the meniscal roots. The allograft is cut into a trapezoid to fit the tibial canal previously made. The meniscal portion of the allograft is prepared with 4 nonabsorbable sutures placed in the posterior horn and 3 nonabsorbable sutures in the anterior horn. Four passing sutures are then passed through the posterior capsule in an inside-out fashion with the aid of the tip of a curved Adson pointed hemostat (Aesculap, Center Valley, PA) to bluntly pierce the capsule. These passing sutures are used to pass the posterior horn meniscal allograft sutures out of the posterolateral capsule before insertion of the graft. The allograft is inserted and the trapezoidal bone plug is pushed into the tibial bone slot. The posterior horn sutures are pulled through the posterior capsule. For graft reduction, a varus force should be applied to the knee with 30° of flexion to allow the allograft to pass under the lateral femoral condyle. Anteriorly placed sutures (3) are tied to the anterior capsule. Finally, the rest of the meniscal allograft is secured with a total of 6 to 10 nonabsorbable vertical mattress sutures placed 5 mm apart with an arthroscopically assisted inside-out technique.