Abstract
Because hip arthroscopic procedures are increasing in number, complications related to the operation itself are starting to emerge. Whereas the capsule has been recognized as an important static stabilizer for the hip, it has not been until recently that surgeons have realized the importance of its preservation and restoration. Disruption of the capsule during arthroscopic procedures is a potential contributor to postoperative iatrogenic hip instability. In cases of a symptomatic deficient capsule, a capsular reconstruction is mandatory because instability may lead to detrimental chondral and labral changes. The purpose of this report was to describe our technique for arthroscopic hip capsular reconstruction using dermal allograft.
Some authors have reported iatrogenic subluxation and dislocation events after hip arthroscopies.1, 2 The hip capsule is one of the most important static stabilizers of the hip joint,3 and disruption or debridement of the capsule during arthroscopy is a potential contributor to postoperative iatrogenic hip instability. Therefore, hip arthroscopists must be mindful of hip capsule management because hip arthroscopic procedures are increasing exponentially.4 Given the increased awareness of the importance of the hip capsule, many surgeons advocate performing either capsular closure or capsular plication at the end of arthroscopic surgery.5, 6
The extent of iatrogenic instability may be underestimated, because a previous study reported that 35% of patients who underwent revision hip arthroscopy were found to have undiagnosed direct observational instability.7 As a result, this could ultimately lead to progressive labral and chondral injury over time.6 Although indications have not been clearly identified, it is recommended that a capsular reconstruction be performed (1) in patients with symptomatic capsular deficiency, (2) when removal of adhesions results in capsule deficiency, or (3) in patients reporting pain and limited range of motion because of capsular adhesions. The purpose of this report is to describe our technique for arthroscopic hip capsular reconstruction using dermal allograft.
Surgical Technique
Anesthesia and Patient Positioning
The patient is placed in a modified supine position on a traction operating table. After induction of general anesthesia, a bilateral examination is performed to assess for hip range of motion. Traction is gently applied to the leg with 15° of internal rotation, 10° of lateral tilt, 10° of flexion, and neutral abduction. To prevent neurologic complications, an extra-wide perineal post is used to minimize pressure on the pudendal nerve and to force the femoral head laterally, shifting the vector of forces. Adequate traction is verified with the fluoroscope (confirmed with a “vacuum sign” and 1 cm of joint distraction).
Portal Placement
Access to the hip joint is accomplished through the anterolateral and midanterior portals. A 70° arthroscope is used to perform a diagnostic arthroscopy, with inspection of both the central and peripheral compartments. After intra-articular pathology is addressed, the traction is released and the capsular defect is sized with a probe.
Graft Preparation
After sizing of the capsular defect, the dermal allograft tissue (LifeNet Health, Bio-Implants Division, Virginia Beach, VA) can be prepared on the back table. For this purpose, a graft 20% larger than the sized capsular defect should be sectioned from the allograft tissue (Video 1). One end of the graft should be attached to the Graftmaster (Smith & Nephew Andover, MA) for better handling. On each corner of the graft, loops are made using No. 2 Vicryl (Ethicon, Somerville, NJ) and tied over a straight mosquito clamp with an overhand-loop knot. The loops will help with intra-articular handling of the graft and will be incorporated into the suture fixation. For increased fixation, an additional loop is placed on the acetabular side. To help with intra-articular identification of the loops, the graft is marked at the locations of the acetabular loops (1 purple point for the medial loop, 2 for the middle loop, and 3 for the lateral loop). Regarding the femoral side, the loops are entirely painted with purple ink to help with identification. Lastly, the graft is remeasured to confirm the desired size (Fig 1).
Fig 1.
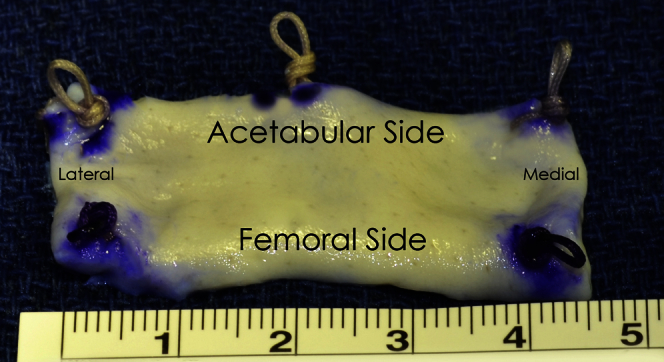
Prepared dermal allograft for capsular reconstruction. The acetabular loops are tagged with 1 (right side), 2 (middle), and 3 purple points (left side) to help with orientation once it is inside the joint. Femoral-sided loops (medial and lateral) are entirely painted with purple ink.
Arthroscopic Technique
After the graft preparation is complete, traction is re-established. Capsular adhesions should be released. Occasionally, the capsule can be attached to the labrum, in which case re-creation of the plane between the labrum and capsule should be performed (Fig 2). Placement of a 1.5-mm JuggerKnot anchor (Biomet, Warsaw, IN) at the 3-o'clock position on the acetabulum is performed. Then the medial corner loop of the graft is secured to the anchor in the 3-o'clock position, and the graft is passed in through a large cannula (Fig 3, Fig 4). An arthroscopic knot is tied, anchoring it medially. The graft is then deployed using a grasper to assess for coverage of the whole defect, up to the 10-o'clock position. Afterward, a 2.3-mm Osteoraptor anchor (Smith & Nephew) is placed at the 10-o'clock position and the sutures of the anchor are passed through the loop on the edge of the graft, securing the lateral position. Lastly, another 2.3-mm Osteoraptor anchor is positioned at the 1-o'clock position, where the center loop had been, and the sutures of the anchor are passed through the loop. An arthroscopic knot is then tied. Additional 1.5-mm JuggerKnot anchors can be placed through the graft to avoid capsular redundancy.
Fig 2.
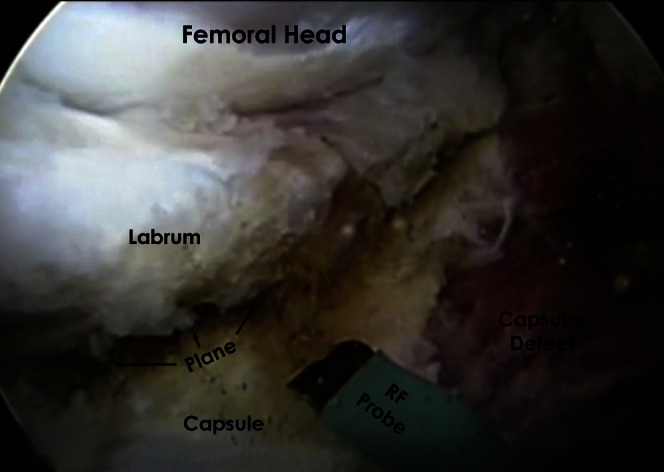
Release of capsular adhesions using a radiofrequency (RF) probe. A plane is created between the labrum and the remnant capsule.
Fig 3.
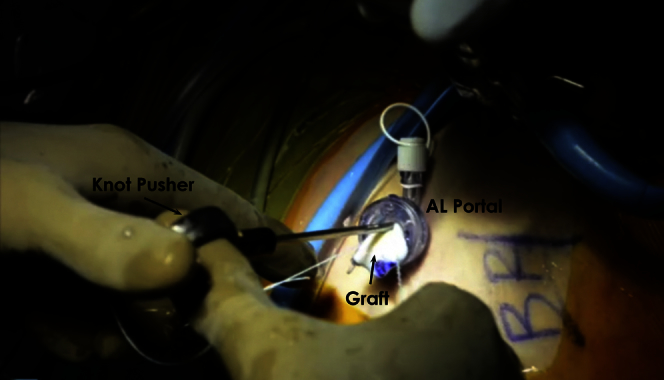
The dermal allograft is passed in through a large cannula in the anterolateral (AL) portal. A knot pusher is used to bring the graft down to the previously placed anchor.
Fig 4.
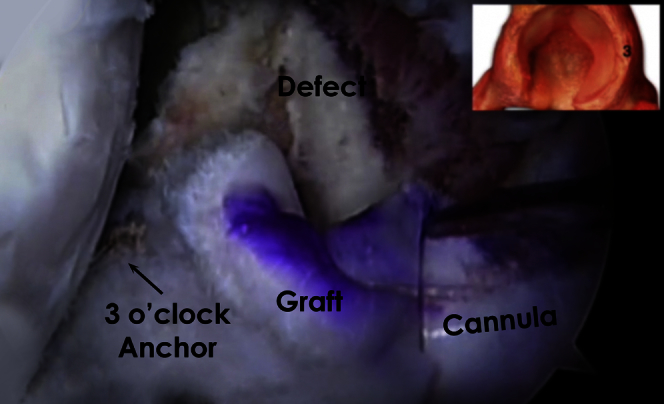
The medial corner loop of the graft is secured to the anchor in the 3-o'clock position that has been previously placed at the subspinal region.
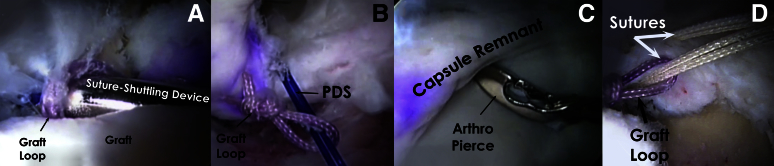
After adequate fixation of the graft to the acetabular side, traction is released and the hip is brought into flexion and internal rotation. Anastomosis of the allograft to the remnant native capsule is performed using a suture-shuttling device (SutureLasso; Arthrex, Naples, FL) through the suture loop of the graft, and a polydioxanone (PDS) wire is advanced through this loop and left in place. Next, an Arthro-Pierce device (Smith & Nephew, Andover, MA) is used to pierce the distal remnant capsule. The PDS wire is pulled out through the anterolateral portal and used to retrieve the sutures, which are then pulled through the remnant capsule and graft loop (Fig 5). To perform this side-to-side anastomosis, a No. 2 absorbable suture (Vicryl) is used. A double-limb suture configuration and racking half-hitch knots are used to secure both capsular limbs (Fig 6).
Fig 5.
(A) Anastomosis of the allograft to the remnant native capsule is performed using a suture-shuttling device (SutureLasso) through the suture loop of the graft, and (B) a polydioxanone (PDS) wire is advanced through this loop and left in place. (C) Next, an Arthro-Pierce device is used to pierce the distal remnant capsule. Then the PDS wire is pulled out through the anterolateral portal and used to retrieve the sutures, (D) which are then pulled through the remnant capsule and graft loop.
Fig 6.
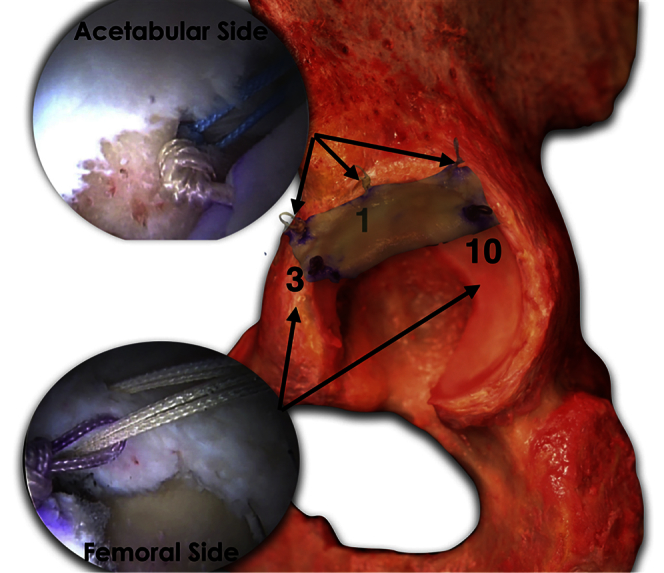
Right capsular reconstruction in a cadaveric pelvis. Three acetabular anchors are placed in the subspinal region at the 1-, 3-, and 10-o'clock positions. Additional anchors can be placed to further reinforce the graft if necessary. For the femoral side, a suture-shuttling device through the distal limb and an Arthro-Pierce device through the loops of the graft are used to perform the side-to-side suture placement.
Additional anastomotic stitches from medial to lateral should be placed. After completion of the capsular reconstruction, tension on the capsule and deployment (no significant redundancy) of the graft should be assessed throughout the complete range of motion (Fig 7). A depiction of the final capsular reconstruction is shown in Figure 8. Pearls and pitfalls of this procedure are listed in Table 1.
Fig 7.

Final result of capsular reconstruction in a right hip, showing the graft in position with the desirable tension.
Fig 8.
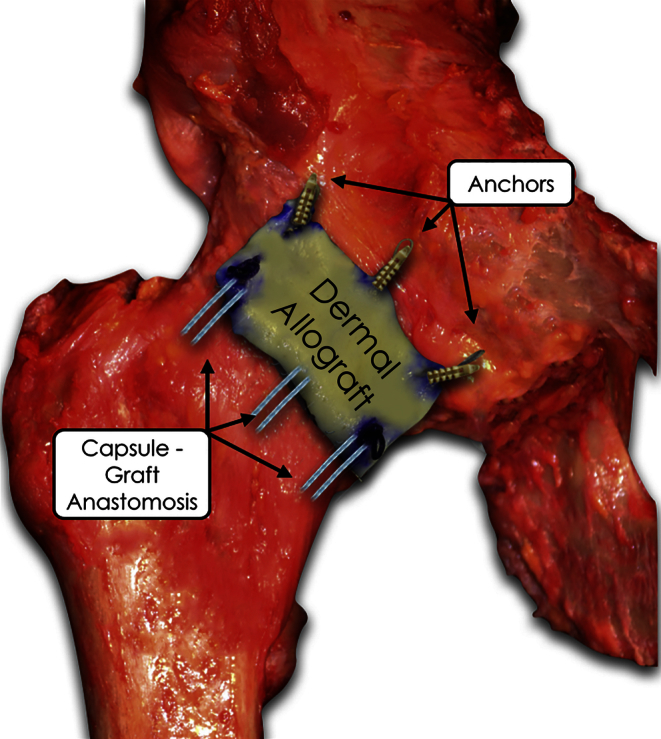
Construct after fixation of the graft into the acetabulum and anastomosis to the remnant capsule in a right cadaveric hip.
Table 1.
Pearls and Pitfalls
| Pearls |
| The patient should be positioned with 15° of internal rotation, 10° of lateral tilt, and 10° of flexion, and neutral abduction while in traction. |
| The dermal allograft should be 20% larger than the sized capsular defect. |
| To help with intra-articular identification of the loops, the graft is marked at the locations of the acetabular loops (1 purple point for the medial loop, 2 for the middle loop, and 3 for the lateral loop). For the femoral side, the loops are entirely painted with purple ink to help with identification. |
| After completion of the capsular reconstruction, tension on the capsule and deployment (no significant redundancy) of the graft should be assessed throughout the complete range of motion. |
| The following acetabular anchors are used: |
| 3-o'clock position, 1.5-mm JuggerKnot anchor |
| 10-o'clock position, 2.3-mm Osteoraptor anchor |
| 1-o'clock position, 2.3-mm Osteoraptor anchor |
| Pitfalls |
| Introducing the allograft into the joint before placing the proximal anchors in the subspinal region makes the procedure more challenging. |
| Failure to correctly measure the capsular defect can result in inappropriate graft size. |
| Not assessing complete range of motion after graft placement can result in failure to identify graft redundancy. |
Discussion
The hip capsule is an important static stabilizer of the hip joint. It is composed of the ilioischial, iliofemoral, and pubofemoral ligaments, as well as the zona orbicularis.8 The iliofemoral ligament is located between the 12- and 3-o'clock positions (thickest at the 2-o'clock position) on the acetabular clock-face anatomy and is the most important stabilizer for hip extension and external rotation.9 Moreover, it is the most commonly incised ligament to gain access to the joint during hip arthroscopy. If left unrepaired, the capsular defect can lead to direct observational instability, anterior hip pain, and in rare cases, subluxation or dislocation.10 In most cases, direct capsular repair or capsular plication can be performed after hip arthroscopy. However, larger defects in the capsule, whether from prior arthroscopy or not, require a reconstructive procedure to fully amend the defect.
Capsular reconstruction has been described with good results in cases of hip instability after hip arthroplasty.11 However, only 1 report exists regarding capsular reconstruction in the native hip.3 Recently, Trindade et al.3 described capsular reconstruction using the iliotibial band. Dermal allograft may more closely approximate the native hip capsule thickness and provide a stronger and more secure construct than the iliotibial band allograft. However, this remains to be examined clinically with a comparison study and long-term follow-up. The benefits of allograft use include reduced donor-site morbidity, the ability to tailor the size of the graft, and a theoretically reduced operating time.12 Advantages and limitations of our procedure can be found in Table 2.
Table 2.
Advantages and Limitations
| Advantages |
| Restoration of stability |
| Ability to use technique when defect is too large to perform direct repair of capsular plication |
| Ability to tailor size of graft |
| No donor-site morbidity and theoretical decreased operating time, as compared with autograft |
| Limitations |
| Technically challenging |
| Not ideal for small defects |
| Cost |
| Allograft availability |
| Limited outcome data |
This is the first description of hip capsular reconstruction using dermal allograft. Although the proposed technique using dermal allograft for hip capsule reconstruction has only recently been developed and implemented, short-term results appear promising. Subjective and objective patient outcome studies are needed to validate the results of capsular reconstruction. Given our promising early clinical results, we will continue to perform arthroscopic hip capsular reconstruction using dermal allograft in the setting of capsular deficiency. However, further biomechanical analysis and clinical study of the indications and outcomes relative to alternative methods are indicated.
Footnotes
The authors report the following potential conflict of interest or source of funding: M.J.P. receives support from Smith & Nephew, Ossur, Siemens, and Vail Valley Medical Center.
Supplementary Data
Capsular reconstruction technique using dermal allograft. First, a diagnostic arthroscopy is performed, with inspection of both the central and peripheral compartments. After intra-articular pathology is addressed, the traction is released and the capsular defect is sized with a probe. The dermal allograft tissue is then prepared on the back table. On each corner of the graft, loops are made using No. 2 Vicryl (Ethicon) and tied over a straight mosquito clamp with an overhand-loop knot. For increased fixation, an additional loop is placed on the acetabular side. To help with intra-articular identification of the loops, the graft is marked at the location of the acetabular loops. Lastly, the graft is remeasured to confirm the desired size. After the graft preparation is complete, traction is re-established. Capsular adhesions should be released. Placement of a 1.5-mm JuggerKnot (Biomet) anchor at the 3-o'clock position on the acetabulum is performed. Then the medial corner loop of the graft is secured to the anchor in the 3-o'clock position, and the graft is passed in through a large cannula. An arthroscopic knot is tied, anchoring it medially. The graft is then deployed using a grasper to assess for coverage of the whole defect, up to the 10-o'clock position. Afterward, a 2.3-mm Osteoraptor anchor (Smith & Nephew) is placed at the 10-o'clock position and the sutures of the anchor are passed through the loop on the edge of the graft, securing the lateral position. Lastly, another 2.3-mm Osteoraptor anchor is positioned at the 1-o'clock position, where the center loop had been, and the sutures of the anchor are passed through the loop. An arthroscopic knot is then tied. Additional 1.5-mm JuggerKnot anchors can be placed through the graft to avoid capsular redundancy. After adequate fixation of the graft to the acetabular side, traction is released and the hip is brought into flexion and internal rotation. Anastomosis of the allograft to the remnant native capsule can be achieved using a suture-shuttling device (SutureLasso; Arthrex) through the distal limb and an Arthro-Pierce device (Smith & Nephew) through the loops of the graft. To perform this side-to-side anastomosis, a No. 2 absorbable suture is used. A double-limb suture configuration and racking half-hitch knots are used to secure both capsular limbs. Additional anastomotic stitches from medial to lateral should be placed. After completion of the capsular reconstruction, tension on the capsule and deployment (no significant redundancy) of the graft should be assessed throughout the complete range of motion.
References
- 1.Benali Y., Katthagen B.D. Hip subluxation as a complication of arthroscopic debridement. Arthroscopy. 2009;25:405–407. doi: 10.1016/j.arthro.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 2.Matsuda D.K. Acute iatrogenic dislocation following hip impingement arthroscopic surgery. Arthroscopy. 2009;25:400–404. doi: 10.1016/j.arthro.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 3.Trindade C.A., Sawyer G.A., Fukui K., Briggs K.K., Philippon M.J. Arthroscopic capsule reconstruction in the hip using iliotibial band allograft. Arthrosc Tech. 2015;4:e71–e74. doi: 10.1016/j.eats.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McCormick F., Slikker W., III, Harris J.D. Evidence of capsular defect following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2014;22:902–905. doi: 10.1007/s00167-013-2591-z. [DOI] [PubMed] [Google Scholar]
- 5.Harris J.D., Slikker W., III, Gupta A.K., McCormick F.M., Nho S.J. Routine complete capsular closure during hip arthroscopy. Arthrosc Tech. 2013;2:e89–e94. doi: 10.1016/j.eats.2012.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Domb B.G., Philippon M.J., Giordano B.D. Arthroscopic capsulotomy, capsular repair, and capsular plication of the hip: Relation to atraumatic instability. Arthroscopy. 2013;29:162–173. doi: 10.1016/j.arthro.2012.04.057. [DOI] [PubMed] [Google Scholar]
- 7.Philippon M.J., Schenker M.L., Briggs K.K., Kuppersmith D.A., Maxwell R.B., Stubbs A.J. Revision hip arthroscopy. Am J Sports Med. 2007;35:1918–1921. doi: 10.1177/0363546507305097. [DOI] [PubMed] [Google Scholar]
- 8.Telleria J.J., Lindsey D.P., Giori N.J., Safran M.R. A quantitative assessment of the insertional footprints of the hip joint capsular ligaments and their spanning fibers for reconstruction. Clin Anat. 2014;27:489–497. doi: 10.1002/ca.22272. [DOI] [PubMed] [Google Scholar]
- 9.Philippon M.J., Michalski M.P., Campbell K.J. A quantitative analysis of hip capsular thickness. Knee Surg Sports Traumatol Arthrosc. 2015;26:2548–2553. doi: 10.1007/s00167-014-3030-5. [DOI] [PubMed] [Google Scholar]
- 10.Harris J.D., McCormick F.M., Abrams G.D. Complications and reoperations during and after hip arthroscopy: A systematic review of 92 studies and more than 6,000 patients. Arthroscopy. 2013;29:589–595. doi: 10.1016/j.arthro.2012.11.003. [DOI] [PubMed] [Google Scholar]
- 11.Fujishiro T., Nishikawa T., Takikawa S., Saegusa Y., Yoshiya S., Kurosaka M. Reconstruction of the iliofemoral ligament with an artificial ligament for recurrent anterior dislocation of total hip arthroplasty. J Arthroplasty. 2003;18:524–527. doi: 10.1016/s0883-5403(03)00073-1. [DOI] [PubMed] [Google Scholar]
- 12.Cvetanovich G.L., Mascarenhas R., Saccomanno M.F. Hamstring autograft versus soft-tissue allograft in anterior cruciate ligament reconstruction: A systematic review and meta-analysis of randomized controlled trials. Arthroscopy. 2014;30:1616–1624. doi: 10.1016/j.arthro.2014.05.040. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Capsular reconstruction technique using dermal allograft. First, a diagnostic arthroscopy is performed, with inspection of both the central and peripheral compartments. After intra-articular pathology is addressed, the traction is released and the capsular defect is sized with a probe. The dermal allograft tissue is then prepared on the back table. On each corner of the graft, loops are made using No. 2 Vicryl (Ethicon) and tied over a straight mosquito clamp with an overhand-loop knot. For increased fixation, an additional loop is placed on the acetabular side. To help with intra-articular identification of the loops, the graft is marked at the location of the acetabular loops. Lastly, the graft is remeasured to confirm the desired size. After the graft preparation is complete, traction is re-established. Capsular adhesions should be released. Placement of a 1.5-mm JuggerKnot (Biomet) anchor at the 3-o'clock position on the acetabulum is performed. Then the medial corner loop of the graft is secured to the anchor in the 3-o'clock position, and the graft is passed in through a large cannula. An arthroscopic knot is tied, anchoring it medially. The graft is then deployed using a grasper to assess for coverage of the whole defect, up to the 10-o'clock position. Afterward, a 2.3-mm Osteoraptor anchor (Smith & Nephew) is placed at the 10-o'clock position and the sutures of the anchor are passed through the loop on the edge of the graft, securing the lateral position. Lastly, another 2.3-mm Osteoraptor anchor is positioned at the 1-o'clock position, where the center loop had been, and the sutures of the anchor are passed through the loop. An arthroscopic knot is then tied. Additional 1.5-mm JuggerKnot anchors can be placed through the graft to avoid capsular redundancy. After adequate fixation of the graft to the acetabular side, traction is released and the hip is brought into flexion and internal rotation. Anastomosis of the allograft to the remnant native capsule can be achieved using a suture-shuttling device (SutureLasso; Arthrex) through the distal limb and an Arthro-Pierce device (Smith & Nephew) through the loops of the graft. To perform this side-to-side anastomosis, a No. 2 absorbable suture is used. A double-limb suture configuration and racking half-hitch knots are used to secure both capsular limbs. Additional anastomotic stitches from medial to lateral should be placed. After completion of the capsular reconstruction, tension on the capsule and deployment (no significant redundancy) of the graft should be assessed throughout the complete range of motion.