Abstract
Background
The social network of those treated for alcohol use disorder can play a significant role in subsequent drinking behavior, both for better and worse. Network Support treatment was devised to teach ways to reconstruct social networks so that they are more supportive of abstinence and less supportive of drinking. For many patients this may involve engagement with AA, but other strategies are also used.
Purpose
The current trial of Network Support treatment, building on our previous work, was intended to further enhance the ability of patients to construct abstinence-supportive social networks, and to test this approach against a strong control treatment.
Methods
Patients were 193 men and women with alcohol use disorder recruited from the community and assigned to either 12 weeks of Network Support (NS) or Packaged Cognitive-Behavioral Treatment (PCBT), and followed for 27 months.
Results
Results of multilevel analyses indicated that NS yielded better posttreatment results in terms of both proportion of days abstinent and drinking consequences, and equivalent improvements in 90-day abstinence, heavy drinking days and drinks per drinking day. Mediation analyses revealed that NS treatment effects were mediated by pre-post changes in abstinence self-efficacy and in social network variables, especially proportion of non-drinkers in the social network and attendance at Alcoholics Anonymous.
Conclusion
It was concluded that helping patients enhance their abstinent social network can be effective, and may provide a useful alternative or adjunctive approach to treatment.
ClinicalTrials.gov Identifier: NCT01129804.
Keywords: Alcohol Treatment, Network Support, Treatment Mechanisms, Self-efficacy, Alcoholics Anonymous
1. INTRODUCTION
Social network support for drinking has been found to be predictive of poor outcomes in treatment-seeking patients (Beattie and Longabaugh, 1997; Beattie et al., 1992; Havassy et al., 1991; Longabaugh et al., 1993; Project MATCH Research Group, 1997). On the other hand, social networks that support sobriety tend to yield greater abstinence from drinking and less relapse after treatment (Beattie and Longabaugh, 1999; Havassy et al., 1991; Longabaugh et al., 1995). The net effect of social networks is large. Stout et al. (2012) noted that the effect size for social network measures on drinking was over and above the effects of contemporaneous AA involvement.
The exact mechanisms of drinking-related social support are not known. It has been suspected that the effects of social support on outcomes may be mediated by cognitive mechanisms such as self-efficacy (Davis and Jason, 2005; Worley et al., 2014) or motivation (Hunter-Reel et al., 2010; Morgenstern et al., 1997). Possible behavioral mechanisms include reinforcement for abstinence and modeling of abstinent behavior, which may account for the effect of abstinence-related models on reduction of posttreatment drinking (Litt et al., 2009c; Zywiak et al., 2002). The absence of these reinforcers, as well as the presence of drinking models, may help to speed relapse (Vuchinich and Tucker, 1996).
Social anxiety has also been recognized as a significant factor in drinking and relapse (Morris et al., 2005). One benefit of adaptive social networks is that they can buffer the effects of social anxiety, and thereby reduce or delay relapse (Pattison et al., 1979). Coping skills, along with self-efficacy, may also be enhanced when persons are exposed to non-drinkers in their social networks. Litt et al. (2009c) reported that abstinence-related network support, as well as AA attendance, were predictive of increased use of coping skills, as well as abstinence self-efficacy. It seems likely that being in the presence of non-drinkers should normalize the experience of functioning without drinking, and help patients adjust cognitively to the idea of not drinking, thereby increasing self-efficacy for abstinence.
Given the potential power of social networks, we devised the Network Support (NS) Project to study the building of social networks supportive of sobriety and to teach patients how to change their own social network (Litt et al., 2007, 2009c). Alcoholics Anonymous (AA) was employed as the basic infrastructure for NS treatment, and NS was based to some extent on the Project MATCH Twelve-step Facilitation intervention (TSF; Nowinski et al., 1992). AA had a number of advantages in this regard: AA meetings are held frequently in a variety of locales, and they form a ready-made network of individuals devoted to helping others stay abstinent.
In our initial study of NS, therapists engaged in problem solving with patients to enable them to make new non-drinking friends as a way to enhance sober social networks. The two NS conditions in our initial study (NS with and without Contingency Management) were compared to a manualized Case Management condition (CaseM). Results from a 27-month follow-up (24 months posttreatment) indicated that both Network Support conditions yielded better outcomes than the CaseM condition.
Despite our efforts, however, a large number of patients in the NS conditions were never able to change their social networks, in part because of deep dislike of AA and difficulty establishing social relationships (almost 30% had 2 or fewer abstinent friends throughout the 2 years of the study). Additionally, the absence of a coping skills based control group left open the possibility that specific network building activities may not be needed: that is, people may increase their sober social network simply as a function of developing relapse prevention skills.
Given these issues, the present second test of NS treatment incorporated an enhanced social skills training component added to NS to improve the ability of patients to engage in new social networks. And in this study NS treatment was tested against a manualized, individual, cognitive-behavioral coping skills-based treatment (Packaged CBT or PCBT; Litt et al., 2009b), in a two-group, randomized design. This comparison treatment tested the specific significance of social network building compared to general relapse prevention skills training, in the context of a registered clinical trial (ClinicalTrials.Gov NCT01129804).
It was hypothesized that the network support intervention would result in a social network that was more supportive of abstinence than would a PCBT intervention, and that NS would result in better long-term outcomes. This result would be expected if a durable supportive network served to help patients forestall relapse and heavy drinking over time. We employed mediational analyses to test whether previous findings regarding the roles of self-efficacy, coping, and readiness to change, as well as social network variables, would be replicated in this study. Finally, given the enhanced attention to social skills-building in this project, it was hoped that NS would result in reduced social anxiety, and thus would yield more network contacts with less attendant distress.
2. METHODS
2.1 Participants
Participants were 127 men and 66 women recruited from the greater Hartford, CT, area from June, 2010 through March, 2012 using newspaper and radio advertisements. To be eligible individuals had to be at least 18 years old, meet DSM-IV criteria for Alcohol Dependence, and be willing to accept random assignment to either of the two treatment conditions. Individuals were excluded from participation if they had acute medical or psychiatric problems requiring inpatient treatment (e.g., acute psychosis, or suicide/homicide risk), current dependence on drugs (except nicotine and marijuana), recent intravenous drug use, tested reading ability below the fifth grade level, lack of reliable transportation to the treatment site, or excessive commuting distance. Individuals were also excluded if they were already engaged in substance abuse treatment elsewhere, if they denied any drinking in the 60 days prior to intake, or if they had attended more than three AA meetings in the month prior to intake.
Of the 266 persons who responded to advertisements and were screened, 193 were eligible according to the criteria described. Most (48) of the 73 excluded had lost interest in seeking treatment. The remainder were excluded because of other drug addiction or lack of transportation and/or stable residence, or did not attend the diagnostic interview. The remaining 193 participants were assigned to the two treatment conditions: PCBT (n=97) and NS (n=96). Based on our earlier results, a between-treatments effect size for change in PDA from baseline to 15 month follow-up was estimated as d=.23 (Hedges bias-corrected). Given this effect size, an N of 75 per cell would be required to detect a difference in PDA at 15 months posttreatment significant at the alpha = .05 level with a power of .81. Thus the present study was sufficiently powered.
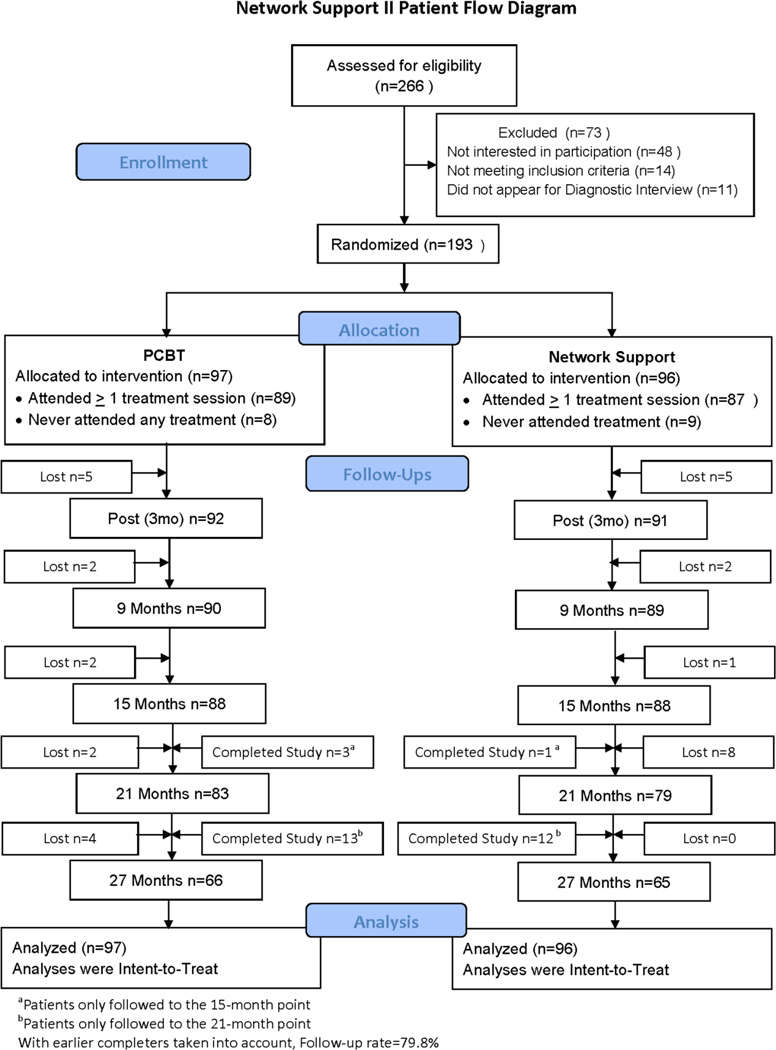
Of the 193 participants randomized, a total of 29 were recruited late in the study period for the purpose of obtaining supplemental data on attentional biases and were not followed for the entire 27 months (25 followed only to 21 months, 4 followed only to 15 months). These persons were nevertheless included in the data analyses, following an intent-to-treat approach in which all persons randomized to treatment were included in analyses. A diagram showing the flow of participants through the study recruitment and treatment stages is shown in Figure 1.
Figure 1.
Flow of patients in the Network Support II project. Only in-person follow-ups are shown here.
Participants were 66% male, with a mean age of 46 years (SD = 10.5), and were 93% White, 3% Black, 3% Hispanic, and 1% other. Their mean years of schooling was 14.3 (SD = 2.0), 78% were employed at least part time outside the home, and 53% were living with a spouse or partner. Participants had a mean AUDIT score of 25.8 (SD=5.4), drank on a mean of 77% of days in the 3 months prior to intake, and had a mean of 1.2 prior treatments for alcohol dependence (SD = 2.1). Table 1 shows the distribution of baseline characteristics by treatment condition, along with results of between-treatment tests (F-test or chi-square). No significant between-treatment differences were seen on any baseline variable.
Table 1.
Demographic and Baseline Characteristics of Sample. N=193.
| Total | Treatment |
Fa or χ2 |
|||||
|---|---|---|---|---|---|---|---|
| PCBT | NS | ||||||
| Variable | Mean | SD | Mean | SD | Mean | SD | |
| Gender (% Male) | 65.8% | 70.1% | 61.5% | 1.60 | |||
| Age (Years) | 46.0 | 10.5 | 45.1 | 9.8 | 47.2 | 11.2 | 1.88 |
| Race/Ethnicity | 1.20 | ||||||
| White | 92.7% | 92.8% | 92.7% | ||||
| Black | 2.6% | 2.1% | 3.1% | ||||
| Hispanic | 3.1% | 3.1% | 3.1% | ||||
| Other | 1.6% | 2.0% | 1.0% | ||||
| Education (Years) | 14.3 | 2.0 | 14.1 | 2.1 | 14.5 | 1.9 | 2.46 |
| Marital Status (% Married or Cohabiting) | 53.4% | 56.7% | 50.0% | 0.87 | |||
| Employed (% Employed Full or Part Time) | 77.7% | 82.5% | 72.9% | 2.55 | |||
| AUDIT Score (0 – 40) | 25.8 | 5.4 | 25.5 | 5.6 | 25.9 | 5.2 | 0.22 |
| Alcohol Treatments Lifetime | 1.0 | 2.0 | 1.0 | 1.6 | 1.1 | 2.5 | 0.31 |
| Proportion Drinking Days in Last 90 | .77 | .22 | .78 | .20 | .75 | .23 | 0.59 |
| Drinks per Drinking Day Last 90 Days | 8.6 | 5.4 | 8.1 | 4.0 | 8.9 | 6.5 | 1.10 |
| AA Meetings Last 90 Days | 0.8 | 2.5 | 0.8 | 2.7 | 0.7 | 2.4 | 0.09 |
| ASI Alcohol Composite Score (0 – 1) | .72 | .14 | .73 | .13 | .71 | .13 | 0.68 |
| ASI Drug Composite Score (0 – 1) | .01 | .05 | .02 | .06 | .01 | .03 | 3.27 |
| ASI Psychiatric Severity Score (0 – 1) | .23 | .21 | .23 | .21 | .23 | .21 | 0.01 |
| Brief Symptom Inventory Score (0 – 72) | 17.77 | 12.93 | 18.23 | 13.22 | 16.88 | 12.38 | 0.52 |
| Treatment Goal (% Abstinence as Goal v. Controlled Drinking) |
71.5% | 71.1% | 71.9% | 0.01 | |||
df for F-tests =1/187
2.2 Measures and Instruments
2.2.1 Diagnostic Interview
The Structured Clinical Interview for DSM-IV Axis I Disorders, Patient edition, version 2.0 (SCID-I/P; First et al., 1996), was used to determine whether subjects met inclusion/exclusion criteria for alcohol abuse or dependence, drug dependence, and psychotic symptoms in the 90 days prior to the interview. The Alcohol Use Disorders Identification Test (AUDIT; Saunders et al, 1993) was also used to characterize severity of drinking in our sample.
2.2.2 Drinking and drug use outcome data
Drinking and drug use data at baseline and at follow-ups were collected using the Form-90 (Miller and Del Boca, 1994). A telephone version of the Form-90 was used for follow-ups that did not take place in person. Three continuously scaled outcome variables were derived from the daily Form-90 data: Proportion Days Abstinent (PDA) in the 90 days prior to intake and prior to each follow-up period (considered the primary drinking outcome); Proportion Heavy Drinking Days (PHD) in the previous 90 days, with a heavy drinking day defined as 4 drinks/day for women and 5 drinks/day for men; and Drinks per Drinking Day (DDD) in each 90-day period, a measure of drinking intensity (log-transformed to correct for skewness). In addition, we also calculated 90-day abstinence status prior to each of the follow-up points.
2.2.3 Psychosocial Outcome
The Drinker Inventory of Consequences (DrInC; Miller et al., 1995), was used to assess problems related to drinking in the domains of health; legal difficulties; and social relations, and was administered at baseline, posttreatment, and every six months thereafter. The DrInC Total score had an internal reliability α = .85.
2.2.4 Treatment process variables: Network support
Network support for drinking or abstinence was measured using the Important People and Activities Instrument (IPA; Clifford and Longabaugh, 1991), administered at baseline, posttreatment, and every 6 months thereafter. The IPA is a structured interview that asks patients to identify up to 10 most important people in their social network, the drinking behavior of each person (frequency and quantity), and the person’s behavior with respect to the patient’s drinking (supportive of drinking, supportive of abstinence). Five summary variables assessing various aspects of network support for abstinence and drinking were used in the present study as the primary social network outcomes: Social Support for Drinking, Attitudinal Support for Drinking, Behavioral Support for Drinking, Attitudinal Support for Abstinence, and Behavioral Support for Abstinence.
Social Support for Drinking was comprised of the mean of the current drinking status (from 1 = abstainer to 5 = heavy drinker) of the persons named in the participant’s social network, plus the mean of those persons’ reactions to the participant’s drinking (from 1 = left the room to 5 = encouraged drinking) (α= .75 t intake). Behavioral Support for Drinking was the proportion of people in the participant’s social network who were classified as heavy drinkers. Attitudinal Support for Drinking was calculated as the mean of the reactions to drinking of those in the social network (α=.70 at intake). Behavioral Support for Abstinence was the proportion of people in the participant’s social network who were abstinent. Attitudinal Support for Abstinence was calculated as the mean of the reactions to not drinking of those in the social network (α= .68 at intake). The intercorrelations of all five of the network support variables were in the range of .3 to .6, indicating that these variables represented related, but not redundant, constructs. Because the network-support treatment in the current study focused on using AA as a social support network, self-reports of number of AA meetings attended prior to intake and at posttreatment and follow-ups were also used as process variables. An additional social network variable, number of close abstinent friends met via AA, was also examined, but this number was so low in both treatments that it was not used in analyses.
2.2.5 Cognitive and behavioral process variables
The Coping Strategies Scale (CSS; Litt et al., 2003) is composed of 59 items scored from 1 to 4 intended to tap potential coping strategies that might be used by a person to remain abstinent (α = .93 at intake). The CSS was administered at pretreatment, posttreatment, 9 months, 15 months and 27 months.
The Alcohol Abstinence Self-Efficacy Scale (AASE; DiClemente et al., 1994) was used to assess self-efficacy in this study. The AASE asks subjects how “tempted” and “confident” they would be in 20 different drinking situations. A total score was computed by subtracting the temptation score from the confidence score (internal reliability α = .92). It was administered at pretreatment, posttreatment, 9 months and 15 months, 21 months, and 27 months.
The Readiness to Change Questionnaire (RTCQ; Rollnick et al., 1992) was designed to assess stages of change in substance abusers. A total score was computed by subtracting the precontemplation score from the sum of the scores of the Contemplation and Action subscales. The internal reliability of this score was borderline, at α = .65. The RTCQ was administered at pretreatment, posttreatment, 9 months, 15 months and 27 months.
2.2.6 Emotional distress/anxiety variables
The Brief Symptom Inventory-18 total score (BSI-18; Derogatis, 2000) was used to measure overall distress (anxiety, depression and somatization), which has been shown to increase risk of relapse (Marlatt, 1985). It was administered at intake, biweekly during treatment, and at the in-person follow-ups (α = .92 at intake). The 19-item Social Interaction Anxiety Scale (SIAS; Mattick and Clarke, 1998) was used to measure social anxiety, specifically anxiety related to fear of meeting new people and engaging in social interactions (α = .93 at intake).
2.3 Procedure
2.3.1 Initial evaluation, informed consent, and identification of collaterals
Prospective subjects were evaluated through a telephone screening procedure and were either excluded (and referred elsewhere for treatment appropriate to their needs), or scheduled for an intake interview with a research assistant. The final decision about eligibility was made at the intake interview, after completion of the SCID-I/P (to determine presence of DSM-IV alcohol dependence and any of the exclusionary diagnoses). Those who were eligible for the research and agreed to be randomly assigned to treatment reviewed the informed consent form and completed the intake assessment. Potential participants were randomly assigned to treatment using a computerized urn randomization procedure (Stout et al., 1994) that balanced the two treatment groups for gender, age, ethnicity, and current involvement with AA. Given the procedures used in each treatment, neither participants, therapists, nor research assistants could be blinded as to treatment condition.
2.3.2 Data collection procedures
Follow-up assessments occurred at posttreatment and at three-month intervals thereafter for the next 24 months (27 months post-intake). In-person interviews were conducted at months 3 (posttreatment), 9, 15, 21, and 27, and took about 1 hour to complete. The intervening assessments at months 6, 12, 18 and 24 were conducted by telephone, during which only the telephone version of the Form-90 was administered, and took about 25 minutes. Participants were compensated $40 for the initial intake assessment, $50 for each in-person follow-up assessment, and $25 for the telephone follow-ups.
2.4 Treatments
Treatment in both conditions was conducted in 12 weekly 60-minute outpatient sessions, employing detailed manuals that provided specific guidelines to therapists. Treatment was provided free of charge in order to maximize subject recruitment. Prior to all evaluations and treatment sessions an alcohol reading was taken via breathalyzer. Any subjects with a blood alcohol level above .05 was asked to wait until the level declined or to return at a later date.
2.4.1 Packaged Cognitive-Behavioral Treatment (PCBT)
PCBT was chosen as a comparison treatment condition because it is a manualized skills-based cognitive-behavioral treatment like those being used in many treatment facilities. PCBT was designed to remediate deficits in skills for coping with interpersonal (e.g., social pressure, conflict with others) and intrapersonal (e.g., craving, anger) antecedents to drinking. The treatment was presented in packaged modules, and was based on manuals developed for our previous clinical research (Kadden et al., 1992; Litt, Kabela-Cormier and Kadden, 2009b). PCBT provided a structured experience using didactic presentations, behavioral rehearsal, and homework practice exercises. Skills training assignments (homework) relevant to the material covered in that session were prescribed at the end of every session. Although material dealing with social networks per se was never part of PCBT, explicit references to the social support network were nevertheless avoided, and social skills relating to changing one’s social network were not discussed. Attendance at AA was neither encouraged nor discouraged in PCBT.
2.4.2 Network Support Treatment (NS)
The NS treatment was intended to help the patient change his or her social support network to be more supportive of abstinence and less supportive of drinking (Litt et al., 2009a). Because AA is a ubiquitous source of social support, and one that is already tapped by most treatment services, it was thought that encouraging AA attendance would be an efficient way to quickly engage patients in a supportive, abstinence-oriented social network.
As in our first NS trial, core topics were based on topics presented in Project MATCH TSF. AA-specific dogma and focus on a higher power were downplayed. Attendance at AA was presented as a way to avoid drinking, to make new acquaintances, and to derive enjoyment (reinforcement) from activities other than drinking. If a patient was adamantly opposed to attending AA, another formalized social network was explored (e.g., Rational Recovery, other social groups).
Recovery tasks, or homework, were assigned weekly. Recovery tasks took the form of going to AA meetings and exploring ways to change one’s network of support. These included activities that were not necessarily AA-related but that had the potential for building non-drinking social networks. These activities might involve education (e.g., obtaining information about a course at a community college), employment (e.g., searching for and applying for a job in a non-drinking environment), family (e.g., family outing or family therapy), and social activities/recreation (e.g., re-establishing contact with non-drinking friends and relatives).
The most significant change from our first trial was that additional time and emphasis were placed on social skills training, after our first study indicated that a significant proportion of patients (30%) were unwilling or unable to meet new people and develop a new support structure. The enhanced social skills section focused particularly on devising ways to meet and interact with new non-drinking persons, including finding venues to meet people, role-playing introductions, and practicing making plans to interact further, with the aim being to make lasting acquaintances.
2.5 Therapists
The four therapists were Masters-level nurse practitioners, psychologists, or social workers working part-time at community substance abuse programs or psychotherapy practices, and with experience using manualized treatments for addictions. All were experienced practitioners of CBT and also proponents of AA. All therapists delivered both of the treatments, in order to eliminate the confound of therapy with therapist (see Project MATCH Research Group, 1998b). Therapists were trained in the protocols through the use of treatment manuals, didactic seminars, and discussion of case examples with the investigators and Project Coordinator. Therapists were not made aware of study hypotheses.
2.6 Treatment Integrity
Therapists were required to follow detailed treatment outline checklists and check off topics covered as the session proceeded. A typical checklist consisted of 4 main topics (e.g., did patient attend AA or other non-drinking social events; skills to discuss that day), each with 4 to 8 subtopics. The requirement to adhere to the session outlines and record progress reduced the likelihood of extraneous or tangential discussions. In addition the Project Coordinator (PC) listened to all session recordings during therapist training, and provided bi-weekly supervision with the therapists, and made sure that elements unique to one treatment were not employed in the other. Following therapist training, 33% of all session tapes were monitored to assess fidelity to the treatment, using the same fidelity checklists used by the therapists. Adherence to treatment among the four therapists ranged from 86% to 91% of checklist topics covered, on average, with no treatment overlaps noted.
2.7 Patient Adherence to Treatment
Participants in PCBT attended a mean of 7.5 sessions versus a mean of 7.4 sessions for those in Network Support (F 1,192 = 0.87). In each treatment condition therapists recorded completion of assigned activities. Patients in the PCBT condition completed 75% of assignments, and those in NS condition completed 70% (Z = 0.76; p=0.44).
3. RESULTS
3.1 Effects of Treatment on Drinking-Related Outcomes Over Time
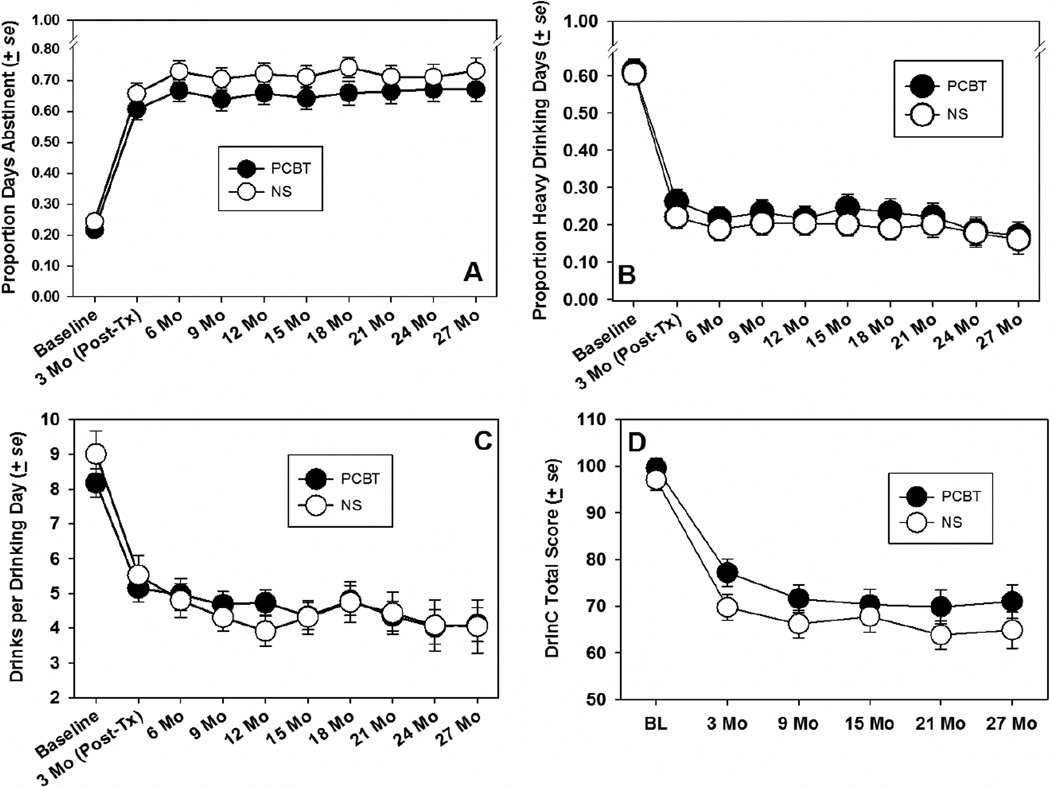
Multilevel modeling (MLM) with random effects and maximum likelihood estimation (Proc MIXED; SAS Institute, 1999) was used to evaluate the effects of treatment over time for each of the continuously scaled outcome variables described above. The MLM approach was used because it employs maximum likelihood estimation of covariance matrices rather than raw data, allowing us to take advantage of all data collected for anyone randomized to treatment. Each repeated dependent variable was analyzed as a function of treatment condition, time since intake (in months), and the interaction of treatment condition by time. No covariates were employed in these analyses, due to the overall equivalence of the treatment groups (see Table 1), and because these initial analyses were intended to present overall between-treatment effects. Treatment condition was treated as a fixed effect and time was treated as a continuous, random effect, with an autoregressive covariance structure. Figure 2 shows the means for each continuous outcome variable by treatment condition. Table 2 shows the summary of the multilevel analyses of these outcomes. As seen in the figure, significant improvements in all outcome measures were seen at posttreatment in both treatment conditions. Main effects for treatment condition were seen on the PDA and the DrInC variables, with the Network Support treatment yielding slightly better outcomes than PCBT over the 24 months of follow-up (27 months post-intake).
Figure 2.
Means of continuous drinking-related outcome variables by treatment condition and by time.
Table 2.
Summary of Tests of Treatment Effects on Outcome Variables. Values Shown are Parameter Estimates from Multilevel Models (for Continuous Outcome Measures) or Estimates and χ2 Values from a Generalized Estimating Equations Analysis (for the Binary 90-Day Abstinence Measure).
| Dependent Variable | Treatmenta (df=1, 1481) |
Timeb (df=1,181) |
Treatment X Time (df=1, 1498) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| B | se | t | B | se | t | B | se | t | |
| Proportion Days Abstinent (PDA) | .054 | .022 | 2.42* | .012 | .002 | 5.76*** | .001 | .003 | 0.15 |
| Proportion Heavy Drinking Days (PDH) | −.027 | .022 | 1.24 | −.010 | .002 | −5.51*** | −.000 | .003 | −0.13 |
| Drinks/Drinking Dayc (DDD) | −.055 | .056 | 0.98 | −.025 | .005 | −4.87*** | −.001 | .007 | −0.10 |
| DrINC Scored | −4.451 | 2.266 | −1.96* | −.864 | .164 | −5.26*** | .080 | .233 | −0.35 |
| B | se | χ2 | B | se | χ2 | B | se | χ2 | |
| 90-Day Abstinence e,f | .332 | .308 | 1.20 | .027 | .011 | 12.25*** | −.010 | .017 | 0.37 |
B=unstandardized estimate; se=standard error; t= t statistic
Treatment coded: PCBT=-1; NS= 1.
Time effect refers to change per month during period from baseline to 27 months.
Drinks/Drinking Day was log transformed
The DrINC was administered on fewer occasions than the other instruments: dfTreatment=1, 606; dfTime=1, 169; dfTreatment X Time= 1, 606.
Baseline PDA used as a covariate in this model.
Only numerator df applies in this analysis.
Note:
p < .05;
p < .001. df = degrees of freedom.
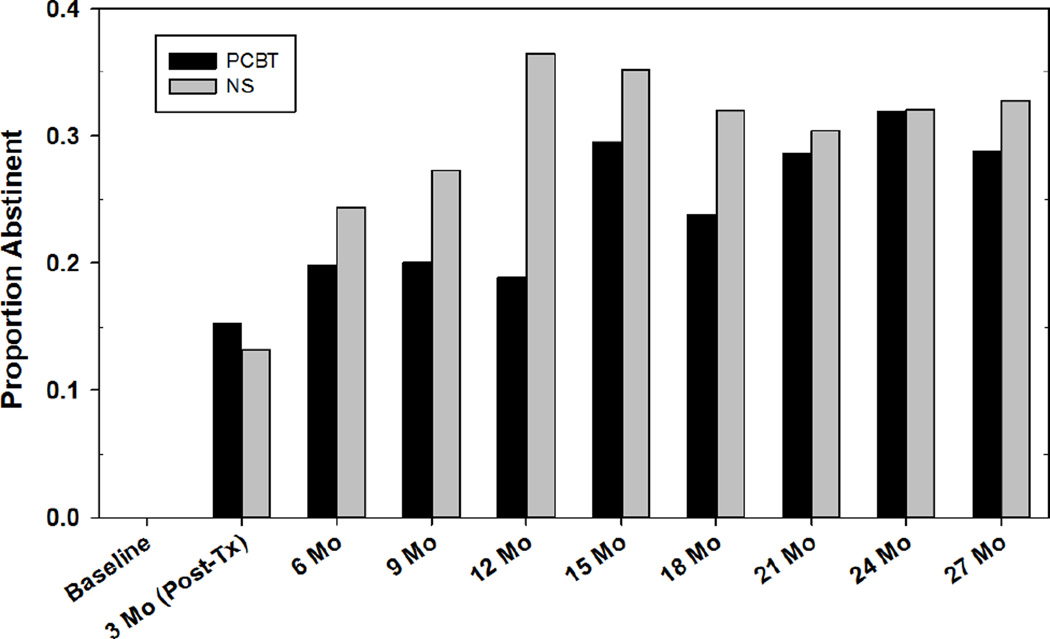
A generalized estimating equations (GEE; Proc GENMOD, SAS Institute, 1999) model was used to analyze the effect of treatment on the dichotomously scaled 90-day abstinence status variable prior to each of the follow-up points, with pretreatment PDA entered as a covariate. GEE uses the “all available pairs” method, in which all non-missing pairs of data are used in the estimating the working correlation parameters. Thus we lose only those individual observations that a given subject has missing, rather than losing the entire subject. The results of the GEE analysis are also seen in Table 2. Abstinence rates by treatment condition are seen in Figure 3. The NS treatment yielded higher abstinence rates overall than the PCBT treatment, particularly near the 12-month follow-up point. By the end of the last follow-up, however, there were no significant differences between treatments.
Figure 3.
Proportion of patients abstinent in each 90-day period by treatment condition.
3.2 Effects of Treatment on Social Network and Cognitive Process Variables, and Distress
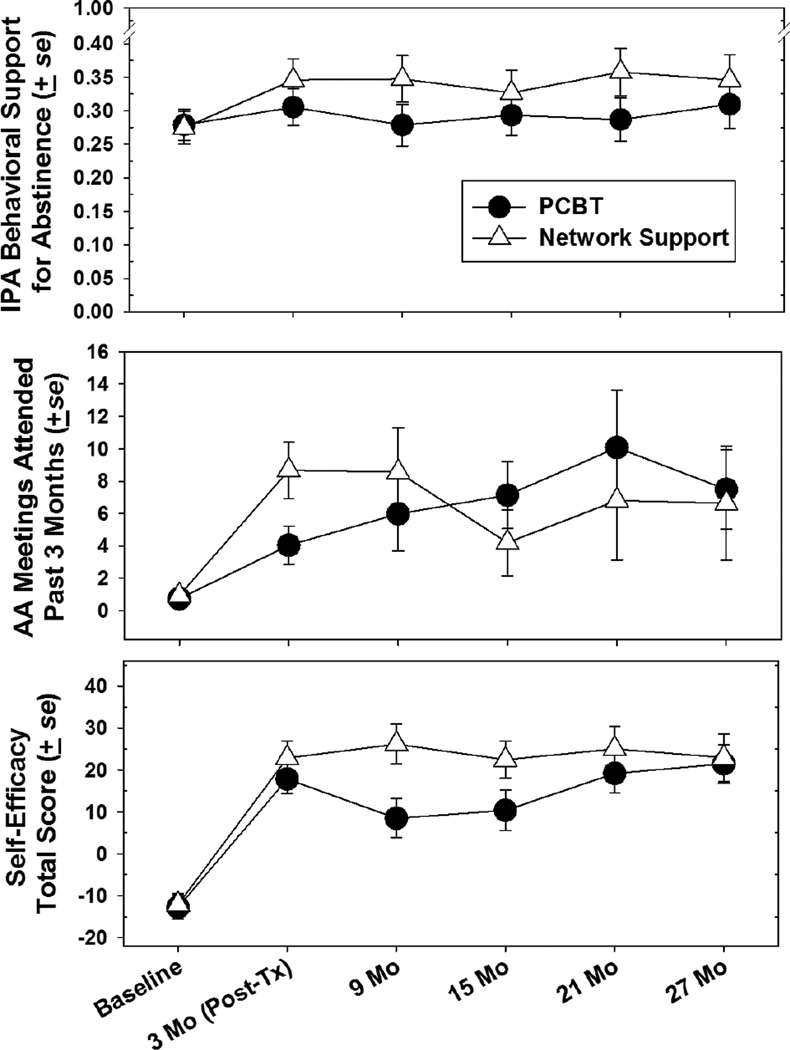
Results of MLM analyses on process measures are summarized in Table 3. Of the IPA social network variables, only behavioral support for abstinence showed an effect of treatment. Patients in the NS treatment tended to increase the proportion of their social network that was abstinent (from roughly 27% to about 35% from baseline to posttreatment), whereas those in the PCBT condition did not (See Figure 4). AA attendance was also sensitive to treatment effects, such that NS yielded increased AA attendance in the first 9 months, which dropped somewhat thereafter, whereas those in PCBT tended to increase AA attendance gradually over time. Despite the influences of treatment, however, 47% of NS patients and 58% of PCBT patients never attended AA during the 27 months of the study. NS patients did find some other means to increase their exposure to non-drinking associates, increasing the proportion of non-drinkers in their network by about 8% (which amounts to a mean of about one-half person) versus 0% for PCBT patients.
Table 3.
Summary of Tests of Treatment Effects on Outcome Variables. Values Shown are Parameter
| Treatment (df=1, 268) |
Timea (df=1,147) |
Treatment X Time (df=1, 268) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| B | se | t | B | se | t | B | se | t | |
| Social Support for Drinking | −.053 | .129 | −0.41 | −.005 | .007 | −0.77 | .003 | .010 | 0.35 |
| Attitudinal Support for Drinking | −.158 | .095 | −1.67 | −.007 | .005 | −1.39 | .002 | .007 | 0.25 |
| Attitudinal Support for Abstinence |
.127 | .082 | 1.55 | −.002 | .004 | −0.54 | .004 | .006 | 0.71 |
| Behavioral Support for Drinking | −.022 | .019 | −1.18 | −.001 | .000 | −0.62 | −.000 | .001 | −0.27 |
| Behavioral Support for Abstinence |
.065 | .032 | 1.92* | .000 | .002 | .27 | .002 | .002 | .72 |
| AA Meeting in Past 90 Daysb | 4.636 | 1.940 | 2.39* | −.093 | .131 | −0.71 | −.268 | .184 | −1.46 |
| Readiness to Change | .443 | .918 | 0.48 | −.205 | 0.52 | −3.91*** | −.049 | .073 | −0.66 |
| Abstinence Self-Efficacy Score | 11.465 | 4.126 | 2.78** | .146 | .241 | 0.61 | .304 | .341 | 0.89 |
| Coping Strategies Scale | −.054 | .057 | −0.95 | −.006 | .004 | −1.46 | .000 | .005 | 0.06 |
| BSI-18 Distress | −1.337 | 1.334 | −1.00 | .060 | .075 | 0.80 | −.014 | .107 | −0.13 |
| Social Interaction Anxiety Scale | −1.292 | 1.370 | −0.94 | .110 | .090 | 1.22 | .127 | .128 | 1.00 |
Note: B=unstandardized estimate; se=standard error; t=t statistic
Time effect refers to change per month during period from baseline to 27 months.
Variable was log transformed
p < .05;
p < .01;
p< .001; df = degrees of freedom
Figure 4.
Means of selected social network variables by treatment condition and by time.
Analyses of readiness to change, abstinence self-efficacy, and coping skills scores showed a main effect for treatment condition only for the self-efficacy measure. Self-efficacy for abstinence increased in both treatment conditions at posttreatment, but maintained a higher level in the NS condition over the follow-up period (see Figure 4, bottom panel). There was no significant treatment effect on BSI distress over time, and, contrary to expectations, no significant treatment effect on social interaction anxiety scale (SIAS) scores.
3.3 Mediators of Treatment Effects
Tests of mediation were conducted to determine what variables might account for differential effects of treatment on outcome. For these analyses PDA over time was used as the dependent variable. The tests of mediation were conducted using a procedure described by Krull and MacKinnon (2001), which employs the unstandardized estimates from MLM analyses as the coefficients for the direct and indirect paths from independent variables and mediators to the outcome. The mediation effect is estimated using a product of coefficients approach adapted by MacKinnon for use with longitudinal data, and evaluated for significance as a Z score. In these analyses the mediator variables were calculated as difference scores from pre- to posttreatment, in order to reflect the direct effects of treatment on the mediator variables.
Mediators were chosen for their apparent sensitivity to treatment effects and/or for their theoretical importance. Three social network variables were chosen: Behavioral Support for Abstinence (proportion of the social network that does not drink) and Social Support for Drinking have both been influential in past studies (e.g., Litt et al., 2009c; Longabaugh et al., 2010); number of AA meetings attended was also used as a mediating social network variable. The cognitive-behavioral process variables examined as mediators were self-efficacy, coping strategies, and readiness to change. Finally, the emotional distress variables from the BSI-18 and from the SIAS were evaluated as mediating variables.
Results of the mediation analyses are shown in Table 4. The effects of Network Support treatment on PDA over time were significantly mediated by pre-post changes in Behavioral Support for Abstinence, i.e., by the proportion of the social network that was non-drinking, by AA meeting attendance, and by abstinence self-efficacy. In each case the Network Support treatment resulted in higher levels of each variable than did PCBT, and these in turn accounted for some of the treatment effect on PDA. The far right column of the table indicates the proportion of the total Treatment effect that was mediated by that variable (MacKinnon, 2008). (Because each analysis was run separately, these proportions do not take into account the other mediators. Thus the total of the mediation effects exceeds 100% of the treatment effect. These proportions are best considered here as relative effect sizes.).
Table 4.
Results from Multilevel Mediation Analyses of PDA Over Time as a Function of Treatment Condition. N = 193.
| Mediator | A-Path | B-Path | Indirect Effect | ||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | B | SE | B | Z | 95% CI | Proportion of Total Effect |
||
| Lower | Upper | ||||||||
| Social Network Variables | |||||||||
| Behavioral Support for Abstinence | 0.057*** | 0.012 | 0.287* | 0.084 | 0.012 | 2.175* | 0.004 | 0.019 | .30 |
| Social Support for Drinking | 0.040 | 0.054 | −0.012 | 0.019 | 0.000 | 0.481 | −0.007 | 0.008 | .00 |
| AA Meetings | 4.822*** | 0.653 | 0.004* | 0.001 | 0.019 | 3.517*** | 0.015 | 0.024 | .32 |
| Cognitive-Behavioral Processes | |||||||||
| Abstinence Self-Efficacy | 5.471** | 1.989 | 0.002** | 0.001 | 0.011 | 2.266* | 0.004 | 0.018 | .70 |
| Coping Strategies | 0.030 | 0.028 | 0.046 | 0.037 | 0.001 | 0.819 | −0.006 | 0.009 | .30 |
| Readiness to Change | 0.935* | 0.410 | 0.002 | 0.002 | 0.002 | 0.916 | −0.004 | 0.008 | .44 |
| Emotional Distress Variables | |||||||||
| Brief Symptom Inventory Distress | −3.551*** | 0.644 | −0.003* | 0.001 | 0.014 | 1.880† | −0.005 | 0.024 | .34 |
| Social Interaction Anxiety Scale | 0.458 | 0.461 | −0.003 | 0.002 | 0.001 | 0.828 | −0.005 | 0.008 | .38 |
Note: A-Path: Effect of Treatment Condition on the mediator. B-path: Effect of mediator on outcome (PDA over time). Indirect effect: The effect of Treatment on PDA over time that is accounted for by the mediator variable. Proportion of Total Effect: Proportion of the total effect of treatment on PDA outcome that is attributable to the mediator variable. Treatment Condition was coded as PCBT= −.5; NS = .5.
p < .10
p < .05.
p < .01.
p < .001.
In a sub-analysis we explored whether network members were acquired via AA, but this distinction made no difference in outcomes. The addition of abstinent network members yielded the same benefit, regardless of whether they were acquired via AA or not.
4. DISCUSSION
The literature convincingly demonstrates that social networks are influential in both the initiation and maintenance of drinking (e.g., Havassy et al., 1991; Longabaugh et al., 1993, 1998; Project MATCH Research Group, 1997, 1998a; Wu and Witkiewitz, 2008). Our group was among the first to try to leverage these findings by devising a treatment approach to help patients actively manage their social networks so that they would be less supportive of drinking and more supportive of abstinence (Litt et al., 2007, 2009c).
To some extent, Network Support in this trial performed as expected. It yielded significantly higher PDA over time, and significantly lower DrInC scores, than PCBT. However, 90-day abstinence rates, proportion of heavy drinking days, and drinks per drinking day were equivalent between the two conditions. Furthermore, our efforts to encourage patients to use AA as a mechanism by which to change their social network were largely unsuccessful, as in our first NS trial. As indicated above, 47% of NS patients never attended AA. Nonetheless, NS patients on average did increase their exposure to non-drinking associates, resulting in improved outcomes. Proportion of non-drinkers in the social network was a significant mediator of NS treatment effects.
Despite the low overall attendance at AA in this study, those in NS did attend significantly more meetings than the PCBT patients, especially at the time of the posttreatment assessment. Attendance at AA at posttreatment was the strongest mediator of NS treatment effects on PDA outcome, along with self-efficacy change, which was also a significant mediator of NS treatment effects. The picture that emerges is that both treatments resulted in increased AA attendance (though more slowly in the case of PCBT), and also increased self-efficacy (more so in NS than in PCBT).
The fact that the mediating variables, as assessed at posttreatment, had an enduring influence on treatment outcomes out to 27 months suggests that treatment had effects that lasted at least 2 years after treatment was finished. Even AA attendance, which peaked among NS patients at the posttreatment time point and then dropped off somewhat, nevertheless persisted throughout the follow-up period well above the baseline level. It is possible that the NS patients got much of what they needed in AA by the time treatment ended, and no longer felt a need to maintain their earlier levels of attendance.
Another goal of this trial was to help patients lower their social interaction anxiety, and thus be more comfortable about expanding their social networks. This did not happen. SIAS scores did not change significantly over time (see Table 3), nor were these scores predictive of drinking outcomes. It appears that our patient sample did not have very high social anxiety to begin with: the mean score was comparable to the scores of average undergraduate women (see Mattick and Clarke, 1998). This low level of social interaction anxiety may not be enough to impede the enhancement of social networks.
Despite the problems detailed above, the current study does offer some hope that treatment and outcomes can be improved. Network Support treatment resulted in outcomes equivalent to or better than those produced by a well-established and effective cognitive-behavioral treatment. It did this by helping people expand their social networks and increase their exposure to non-drinking models in a way that the relapse prevention-based program did not. NS also prompted increased attendance at AA, which itself was a significant contributor to improved outcomes.
Network Support treatment also had significant effects on some other key mediating processes. Abstinence self-efficacy is one of the most influential constructs in the substance abuse literature (Kadden and Litt, 2011). In the present study abstinence self-efficacy was the most powerful mediator of treatment effects. NS was superior to PCBT at increasing abstinence self-efficacy, which in turn translated into long-term treatment gains. NS also had significantly greater effects than PCBT on reducing distress, and on increasing readiness to change, though these did not end up as mediators of treatment effects. These various findings can serve as the basis for further refining and improving NS treatment, to enhance treatment outcomes.
There were some limitations to this study. In particular, our eligibility criteria may have resulted in a more functional sample than might usually be the case in the community, possibly reducing generalizability of this study. Additionally, as indicated above, the level of social anxiety was not high. And the relatively low number of minority patients may also have altered the outcome. Research assistants could not be blinded to treatment condition, and the small number of therapists used might have reduced generalizability. It is not likely, however, that these issues would have favored one treatment over another. Nevertheless, future studies should include a broader cross-section of the alcohol use disorder population.
Network support can be an effective strategy to help change the environment that maintains drinking and interferes with sobriety in some patients, and can contribute to our strategies for behavior change in substance use disorder patients. Network support–based treatment may be a useful alternative for the coping skills-based treatments that are now ubiquitous, or it may serve as an adjunct to coping skills treatments. Additional research regarding who would benefit most from Network Support will help to sort out these possibilities.
Supplementary Material
Highlights.
Patients can change their social networks to be more supportive of abstinence
Social networks that are more supportive of abstinence yielded reduced drinking
Network support treatment was effective for most patients
Network support treatment effects were mediated by self-efficacy, network variables
Acknowledgments
The authors would like to acknowledge Eileen Leonard, William Blakey, Kara Dion, Abigail Young, Christine Calusine and Jane Harrison for their hard work and dedication in the conduct of this work.
Role of funding source
The study on which this paper is based, Network Support II, was sponsored by Grant R01-AA012827 from the National Institute on Alcohol Abuse and Alcoholism, and in part by General Clinical Research Center Grant M01-RR06192 from the National Institutes of Health, US Department of Health and Human Services. No office or personnel of the NIH had any role in study design, data collection, data analysis of interpretation of the data.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Drs. Litt and Kadden conceptualized the study and wrote the grant application that outlined its design. Drs. Litt & Kabela-Cormier wrote the treatment manuals, and Dr. Kabela-Cormier supervised the clinical interventions. Dr. Litt designed and implemented data analysis including statistical analysis, wrote the primary draft, and edited all subsequent drafts. Drs. Kadden, Tennen, and Kabela-Cormier provided critical interpretation of the results and edited the manuscript. All authors approved the final manuscript.
Conflict of interest
None of the authors has any financial conflict of interest to report.
REFERENCES
- Beattie MC, Longabaugh R. Interpersonal factors and post-treatment drinking and subjective wellbeing. Addiction. 1997;92:1507–1521. [PubMed] [Google Scholar]
- Beattie MC, Longabaugh R. General and alcohol-specific social support following treatment. Addict. Behav. 1999;24:593–606. doi: 10.1016/s0306-4603(98)00120-8. [DOI] [PubMed] [Google Scholar]
- Beattie MC, Longbaugh R, Fava J. Assessment of alcohol-related workplace activities: development and testing of “Your Workplace”. J. Stud. Alcohol. 1992;53:469–475. doi: 10.15288/jsa.1992.53.469. [DOI] [PubMed] [Google Scholar]
- Clifford PR, Longabaugh R. Manual for the Important People and Activities Instrument. Providence, RI: Center for Alcohol and Addiction Studies, Brown University; 1991. [Google Scholar]
- Davis MI, Jason LA. Sex differences in social support and self-efficacy within a recovery community. Am. J. Community Psychol. 2005;36:259–274. doi: 10.1007/s10464-005-8625-z. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. BSI-18: Administration, Scoring and Procedures Manual. Minneapolis, MN: National Computer Systems - Pearson; 2000. [Google Scholar]
- DiClemente CC, Carbonari JP, Montgomery RP, Hughes SO. The Alcohol Abstinence Self-Efficacy scale. J. Stud. Alcohol. 1994;55:141–148. doi: 10.15288/jsa.1994.55.141. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders - Patient Edition (SCID-I/P, Version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Havassy BE, Hall SM, Wasserman DA. Social support and relapse: commonalities among alcoholics, opiate users, and cigarette smokers. Addict. Behav. 1991;16:235–246. doi: 10.1016/0306-4603(91)90016-b. [DOI] [PubMed] [Google Scholar]
- Hunter-Reel D, McCrady BS, Hildebrandt T, Epstein EE. Indirect effect of social support for drinking on drinking outcomes: the role of motivation. J. Stud. Alcohol Drugs. 2010;71:930–937. doi: 10.15288/jsad.2010.71.930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadden RM, Carroll K, Donovan D, Cooney NL, Monti P, Abrams D, Litt MD, Hester R. NIAAA Project MATCH Monograph. Washington, D.C.: U.S. Government Printing Office; 1992. Cognitive-Behavioral Coping Skills Therapy Manual: A Clinical research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. [Google Scholar]
- Kadden RM, Litt MD. The role of self-efficacy in the treatment of substance use disorders. Addict. Behav. 2011;36:1120–1126. doi: 10.1016/j.addbeh.2011.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krull JL, MacKinnon DP. Multilevel modeling of individual and group level mediated effects. Multivariate Behav. Res. 2001;36:249–277. doi: 10.1207/S15327906MBR3602_06. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kabela-Cormier E, Kadden R. Netwrok Support Treatment Manual. Farmington, CT: University of Comnnecticut Health Center; 2009a. [Google Scholar]
- Litt MD, Kabela-Cormier E, Kadden RM. Packaged Cognitive-Behavioral Treatment Manual. Farmington, CT: University of Connecticut Health Center; 2009b. [Google Scholar]
- Litt MD, Kadden RM, Cooney NL, Kabela E. Coping skills and treatment outcomes in cognitive-behavioral and interactional group therapy for alcoholism. J. Consult. Clin. Psychol. 2003;71:118–128. doi: 10.1037//0022-006x.71.1.118. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry N. Changing network support for drinking: initial findings from the network support project. J. Consult. Clin. Psychol. 2007;75:542–555. doi: 10.1037/0022-006X.75.4.542. [DOI] [PubMed] [Google Scholar]
- Litt MD, Kadden RM, Kabela-Cormier E, Petry NM. Changing network support for drinking: network support project 2-year follow-up. J. Consult. Clin. Psychol. 2009c;77:229–242. doi: 10.1037/a0015252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Longabaugh R, Beattie M, Noel N, Stout R, Malloy P. The effect of social investment on treatment outcome. J. Stud. Alcohol. 1993;54:465–478. doi: 10.15288/jsa.1993.54.465. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW, Beattie MC, Noel N, Stout R. Matching treatment focus to patient social investment and support: 18-month follow-up results. J. Consult. Clin. Psychol. 1995;63:296–307. doi: 10.1037//0022-006x.63.2.296. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW, Zweben A, Stout RL. Network support for drinking, Alcoholics Anonymous and long-term matching effects. Addiction. 1998;93:1313–1333. doi: 10.1046/j.1360-0443.1998.93913133.x. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Wirtz PW, Zywiak WH, O’Malley SS. Network support as a prognostic indicator of drinking outcomes: the COMBINE study. J. Stud. Alcohol Drugs. 2010;71:837–846. doi: 10.15288/jsad.2010.71.837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction To Statistical Mediaiton Analysis. Mahwah, N.J: Erlbaum; 2008. [Google Scholar]
- Marlatt GA. Situational determinants of relapse and skill training interventions. In: Marlatt GA, Gordon JR, editors. Relapse Pprevention: Maintenance Strategies In The Treatment Of Addictive Behaviors. New York: Guilford Press; 1985. pp. 71–127. [Google Scholar]
- Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behav. Res. Ther. 1998;36:455–470. doi: 10.1016/s0005-7967(97)10031-6. [DOI] [PubMed] [Google Scholar]
- Miller WR, Del Boca FK. Measurement of drinking behavior using the Form 90 family of instruments. J. Stud. Alcohol Suppl. 1994;12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC) Rockville, MD: NIAAA Monograph U.S. Government Printing Office; 1995. [Google Scholar]
- Morgenstern J, Labouvie E, McCrady BS, Kahler CW, Frey RM. Affiliation with Alcoholics Anonymous after treatment: a study of its therapeutic effects and mechanisms of action. J. Consult. Clin. Psychol. 1997;65:768–777. doi: 10.1037//0022-006x.65.5.768. [DOI] [PubMed] [Google Scholar]
- Morris EP, Stewart SH, Ham LS. The relationship between social anxiety disorder and alcohol use disorders: a critical review. Clin. Psychol. Rev. 2005;25:734–760. doi: 10.1016/j.cpr.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Nowinski J, Baker S, Carroll K. Twelve Step Facilitation Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. Washington, D.C: U.S. Government Printing Office; 1992. [Google Scholar]
- Pattison EM, Llamas R, Hurd G. Social network mediation of anxiety. Psychiatr. Ann. 1979;9:474–482. [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J. Stud. Alcohol Suppl. 1997;58:7–29. [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to patient heterogeneity: Project MATCH three-year drinking outcomes. Alcohol. Clin. Exp. Res. 1998a;22:1300–1311. doi: 10.1111/j.1530-0277.1998.tb03912.x. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. Therapist effects in three treatments for alcohol problems. Psychothera. Res. 1998b;8:455–474. [Google Scholar]
- Rollnick S, Heather N, Gold R, Hall W. Development of a short ‘readiness to change’ questionnaire for use in brief, opportunistic interventions among excessive drinkers. Br. J. Addict. 1992;87:743–754. doi: 10.1111/j.1360-0443.1992.tb02720.x. [DOI] [PubMed] [Google Scholar]
- SAS Institute. SAS/STAT Software: Changes And Enhancements Through V7 And V8. Cary, NC: 1999. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption--II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Stout RL, Kelly JF, Magill M, Pagano ME. Association between social influences and drinking outcomes across three years. J. Stud. Alcohol Drugs. 2012;73:489–497. doi: 10.15288/jsad.2012.73.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. J. Stud. Alcohol Suppl. 1994;12:70–75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Vuchinich RE, Tucker JA. Alcoholic relapse, life events, and behavioral theories of choice: a prospective analysis. Exp. Clin. Psychopharmacol. 1996;4:19–28. [Google Scholar]
- Worley MJ, Trim RS, Tate SR, Roesch SC, Myers MG, Brown SA. Self-efficacy and social networks after treatment for alcohol or drug dependence and major depression: disentangling person and time-level effects. Psychol. Addict. Behav. 2014;28:1220–1229. doi: 10.1037/a0037901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu J, Witkiewitz K. Network support for drinking: an application of multiple groups growth mixture modeling to examine client-treatment matching. J. Stud. Alcohol Drugs. 2008;69:21–29. doi: 10.15288/jsad.2008.69.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zywiak WH, Longabaugh R, Wirtz PW. Decomposing the relationships between pretreatment social network characteristics and alcohol treatment outcome. J. Stud. Alcohol. 2002;63:114–121. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.