Abstract
Objectives:
International guidelines on infant feeding for HIV- positive mothers promote Exclusive Replacement Feeding (ERF) (infant formula or animal milk) or exclusive breastfeeding (with no supplements of any kind). A mixed feeding pattern, where breastfeeding is combined with other milks, liquid foods or solids, has been shown to increase the risk of transmission of HIV and is strongly discouraged. However, little is known about the ability of women to adhere to recommended feeding strategies to prevent mother-to-child transmission (MTCT) of HIV from breast milk. The objective of this study was to assess the individual and community-level factors that affect perspectives, attitudes and practices of HIV-positive mothers on MTCT and infant feeding in sub-Saharan Africa as documented in peer-reviewed and grey literature.
Methods:
This work is based on an extensive review of peer-reviewed articles and grey literature from the period 2000-2012. The literature search was carried out using electronic databases like Medline Ovid, Google Scholar, PubMed and EBSCOhost. Both quantitative and qualitative studies written in English language on HIV and infant feeding with particular emphasis on Sub-Saharan Africa were included.
Results:
The review found low adherence to the chosen infant feeding method by HIV-positive mothers. The following factors emerged as influencing infant feeding decisions: cultural and social norms; economic conditions; inadequate counselling; and mother’s level of education.
Conclusions and Public Health Implications:
Unless local beliefs and customs surrounding infant feeding is understood by policy makers and program implementers, Prevention of Mother-to-Child Transmission (PMTCT) programs will only be partially successful in influencing feeding practices of HIV-positive women. Hence programs should provide affordable, acceptable, feasible, safe and sustainable feeding recommendations that do not erode strong cultural practices. Advice to HIV-positive mothers should be based on local conditions that are acceptable to the community.
Keywords: mother-to-child-transmission, PMTC and infant feeding, Cultural and social norms, HIV/AIDS, Sub-Saharan Africa, Ghana
Background
Globally, of the 33.3 million individuals infected with HIV,[1] 22.5 million live in sub-Saharan Africa (SSA).[1, 2] Sub-Saharan Africa remains the region most heavily affected by HIV, accounting for approximately 69 per cent of people living with HIV globally.[3] Over the past decade, HIV prevalence among women attending antenatal clinics has unprecedentedly risen leading to an increase in HIV-positive children born to HIV-infected mothers’ worldwide.[4] According to Illiff and colleagues, 30-50% of women will pass the virus to their infants; and more than a third of all transmissions will occur during breastfeeding without appropriate interventions.[5]
In 2010, an estimated 390, 000 [340, 000–450, 000] children were newly infected with HIV of which more than 90% were living in Sub-Saharan Africa.[3] In 2008, of the 430,000 paediatric HIV infections worldwide, between 129,000 and 194,000 were attributable to breastfeeding.[4] In the absence of any interventions, the rate of Mother to Child Transmission (MTCT) in developing countries can be as high as 45 per cent with prolonged breastfeeding of up to 24 months.[5] Post-natal transmission of HIV, predominantly through breastfeeding accounts for approximately half of all MTCT in Sub-Saharan Africa where breastfeeding is prolonged.[5] In this region, HIV/AIDS accounted for 7.7 per cent of deaths of children under five years.[6]
Several studies have tried to estimate the net effect of HIV/AIDS on child mortality in Africa.[7-10] One of such studies by Adetunji in 2000, provided an overview by comparing point estimates of under-five mortality in the late 1980’s and early 1990’s, using published estimates from Demographic and Health Surveys (DHS). The study found that in Africa, HIV mortality accounted from 13% to 61% of under-five mortality depending on the country, demonstrating that the HIV/AIDS epidemic is reversing many of the gains made in child survival.[8]
Over the past decade, the WHO in partnership with other UN agencies has issued several guidelines in relation to the PMTCT and infant feeding. While each successive guideline has varied in light of evidence, a common recommendation for the prevention of transmission has been the avoidance of breastfeeding and replacement with infant formulae when possible and considered adequately safe, and discouraging of mixed feeding (combining breastfeeding with other fluids and solids). While this has clearly been successful in developed countries, this is often not been the case in developing countries and much of Sub-Saharan Africa,[11] more specifically, with regards to infant feeding. Although formula is the recommended infant feeding option for HIV-infected mothers in developed countries, this may not be a feasible or preferred choice for women in resource-poor communities and developing countries for many reasons. These include the prohibitive cost, poor infrastructure to ensure consistent availability and cultural beliefs that may compel mothers to continue breastfeeding. These socially and culturally embedded practices need to be understood and taken into account when designing and implementing infant feeding programs in the context of MTCT of HIV.
Breastfeeding is the norm in most of the world, and for good reasons such as the best nutrition for babies, protection against deadly childhood diseases, delay return to fertility, being costless, and promotion of bonding and social/emotional development in babies.[12-14] Other benefits of the promotion of Exclusive Breastfeeding (EBF) include: a healthful behavior for HIV-unexposed infants and their mothers, requires minimal preparation, is not dependent upon outside materials[4] and among other benefits which are incalculable. Yet, in today’s society, breastfeeding is often thought of as unnecessary due to diseases. The HIV epidemic coupled with the assumed benefits of infant formula for the children of all HIV-infected mothers have in complex ways, changed public ideas about infant feeding and represents a threat to well established breastfeeding practices.[15] The rise in HIV/AIDS cases puts new focus on breastfeeding as a route of transmission from mother to child especially in Africa.
Infants across all regions of the world are breastfed, although not always exclusively and there is significant variation in the percentage of infants who are ever breastfed among regions and among countries within a region.[16] According to Young and colleagues, current rates of EBF are well below targeted levels in both HIV-affected and unaffected populations around the world though increasing rates of EBF is one of the most powerful interventions to save child lives.[4] The promotion of breastfeeding could prevent 13–15% of child deaths in low-income countries.[17] In Sub-Saharan Africa, the issue of HIV transmission through breastfeeding is of public health importance particularly in countries where HIV affects significant proportion of the population and where breastfeeding is the cultural norm.[18] Studies have confirmed that about a third of HIV transmission from mother to child occurs through breastfeeding.[19, 5] This is as a result of inappropriate infant feeding practices.
According to WHO, appropriate feeding practices play a crucial role in preventing mortality and in achieving optimal health outcomes for infants and young children during the first 6 months of life.[20] Despite, the many advantages of EBF and ERF, a woman’s initial decision to EBF or ERF can be hindered by a range of societal, household, and individual factors. In light of the gap between policy and practice, the purpose of this review is to deepen our understanding of why this gap exists. We examined the evidence in terms of factors affecting perspectives, attitudes and practices of HIV-positive mothers and communities on mother-to-child-transmission and infant feeding in Sub-Saharan Africa region.
Methods
This work is based on an extensive review of peer-reviewed articles and grey literature based on the aim and objectives of the study, covering the period 2000-2012 (12 years). The literature search for peer-reviewed articles were carried out using electronic databases like, Medline Ovid, Google scholar, Pubmed and EBSCOhost, keeping in mind the fact that different authors use different terminologies. Key words and phrases like “HIV” “HIV and infant feeding”, “infant feeding practices,” “influence of breastfeeding duration,” “replacement feeding or alternative feeding”, “international infant feeding guidelines”, “WHO infant feeding guidelines”, “developing countries”, “low-income countries”, “middle-income countries”, “sub-Saharan Africa”, “resource poor settings”, “socio-economic status”, “educational status”, “counseling”, “cultural norms and practices”, “stigma” PMTCT, were used to identify the relevant literature after which duplicate records and irrelevant titles were removed. Both quantitative and qualitative studies on HIV and infant feeding with particular emphasis on sub-Saharan Africa were included. Only papers written in English which met the inclusion criteria were selected for this review.
In all, a total of 215 articles were identified through the searching. After articles excluded based on region, study subjects and year of publication, 34 articles both quantitative and qualitative English language studies met the inclusion criteria. Figure 1 presents a flowchart representing the overall selection process for the studies reviewed in this paper. This paper is based on a review of existing literature and did not require ethical approval.
Figure 1.
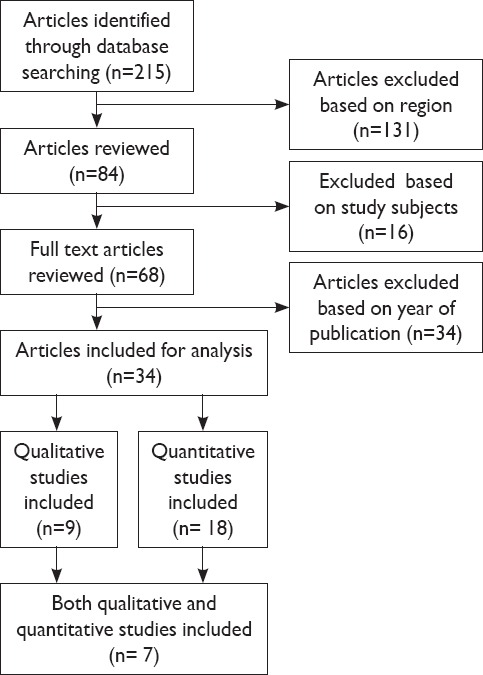
Process for searching the relevant literature.
Results
For the review, 34 articles comprising of 9 qualitative, 18 quantitative and 7 both quantitative and qualitative studies were analyzed. The results were categorized based on the following attributes: socio-economic, PMTCT and infant feeding counseling and cultural and social norms. Based on information gathered from the study findings, we developed a conceptual framework (figure 2) that demonstrated the interrelationships between the attributes that affect breastfeeding among mothers who are positive for HIV/AIDS. These factors influence considerations of and the relative importance of affordability, feasibility, acceptability, and sustainability of feeding options recommended for HIV-Positive mothers and the decision by the mother to adopt a particular option or combination thereof.
Figure 2.
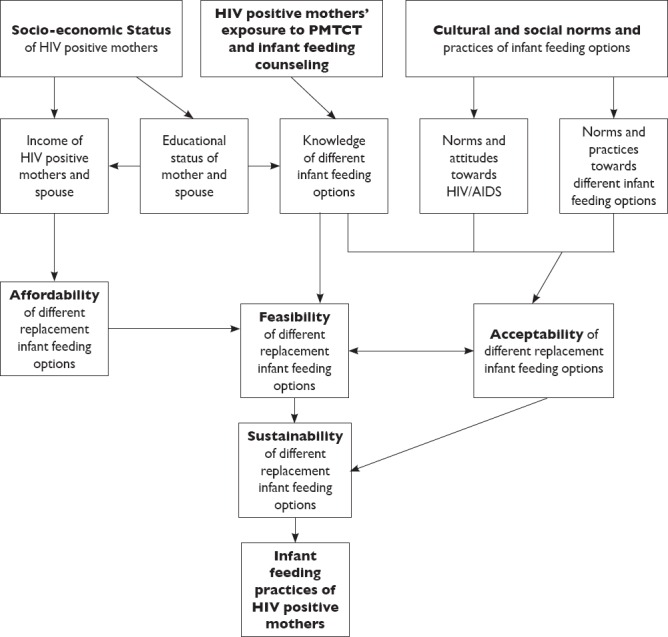
Conceptual framework
HIV-positive Mothers’ Exposure to PMTCT and Infant Feeding Counseling.
Infant feeding counseling based on international guidelines is considered a basis in the prevention of MTCT of HIV in Sub-Saharan Africa. In this setting, the quality of the infant feeding counseling and the knowledge and practices of nurses or PMTCT counsellors providing the services have been called into question.
An increasing body of research documents the shortcomings of infant feeding counseling particularly in terms of counsellors’ knowledge about PMTCT and counseling skills.[21-23] A qualitative study in Moshi, Kilimanjaro region investigating counsellors’ infant feeding advice to HIV-positive women, reported that infant feeding options were not accurately explained and that informed choice of infant feeding method, as recommended in the guidelines, was seriously compromised by inadequate information leading to directive counseling.[24] In that same Kilimanjaro Region of Tanzania, a study which evaluated HIV-positive women’s knowledge following infant feeding counseling showed that the women demonstrated a good understanding of HIV transmission through breastfeeding and recommended infant feeding options.[25]
One of such studies conducted in Zambia, assessed the knowledge and understanding of HIV-positive mothers who had received pre and post-test HIV counseling of the WHO recommended infant feeding guideline reported that 35 percent of the women surveyed, understood the risk of transmission of HIV through breastfeeding.[26] This knowledge was a key factor in them opting to exclusively breastfeed in order to avoid transmitting HIV to their infants. Similarly a study conducted in Harare, Zimbabwe demonstrated that women’s knowledge of HIV and infant feeding options had improved with increased exposure to counselling.[27] Moreover, counselled mothers were 8.4 times more likely to uptake EBF than the mothers who were not exposed to counselling.[27]
In South Africa, it was reported that despite receiving counseling, knowledge and understanding of feeding options was poor.[28] This was demonstrated by the fact that 85 percent of the women who had been counselled could not define the term EBF. A Tanzanian study came out with similar findings.[29] In addition, the women’s knowledge on safe preparation of infant formula was poor and this was attributed to the fact that this had not been demonstrated to them by counsellors. The problem of poor quality counseling was also reported in a study of nurse counsellors in northern Tanzania where cousellors were not able to give quality and relevant advice to HIV-positive women on how best to feed their infants.[30] According to Ehrnst and Zetterstrm, the recommendations given and the way in which counseling is performed are the most important determinants of a mother’s decision about how to feed her infant.[31]
In Eastern Uganda, a study, which assessed how infant feeding counseling was done and experienced by counsellors and mothers in the context of infant feeding guidelines and its implications for implementation, found the counseling sessions often improvised and the tendency to simplify messages giving one-sided information was seen.[32] In that same study, different health workers presented contradicting simplified perspectives in some cases. Chopra et al. report that counseling is central to preparing mothers for making a proper informed choice about adequate feeding practices to prevent their infants from acquiring HIV infection.[28]
Socio-economic Status of HIV-positive Mothers
For mothers in Sub-Saharan Africa, an appropriate choice of infant feeding is fundamental to optimizing infant survival and minimizing infant morbidity and mortality. A woman’s socio-economic status may well be predictive of her acceptance of PMTCT of HIV care, and likely infant feeding behaviors.
The guidelines on HIV and infant feeding needs to be cognizant of and reflective of the fact that HIV/AIDS and poverty are inextricably linked.[33] In a context of HIV/AIDS and poverty, women are particularly vulnerable as they are among the poorest in most sub-Saharan African societies.[34] This is illustrated in the following country studies across Sub-Saharan Africa. A study in Kilimanjaro (Tanzania) on recommended replacement infant feeding options, reported that women considered formula as unaffordable but if the formula was distributed free of charge, the majority of them (82 percent) would choose this option.[35] In a Ugandan study, it was reported that HIV-positive mothers started breastfeeding their babies once UNICEF stopped donating free infant formula, suggesting issues of cost (affordability) influencing their shift.[36] Similarly in South Africa, HIV-positive women opted for replacement feeding when formula milk was provided free. Moreover, women of lower socio-economic status found it difficult to continue formula feeding when there was an interruption in the supply of free formula.[37] Similar results were reported from Kenya[38] and Nigeria.[39] Taken together, all these studies are unanimous in reinforcing that socio-economic factors are critical influences in the choices women make with regard to infant feeding.
Besides the cost of formula, other socio-economic considerations including access to clean water, electricity, and other infrastructure necessary for the safe and hygienic preparation of formula milk needs to be considered. In the Nigerian study, poor access to clean water for the preparation of formula milk was an important barrier to replacement feeding.[39] In South Africa, it was found that women who possessed a kettle, flask and electricity found it easier to feed their infants with formula milk during the night.[37] Still in South Africa, in the province of KwaZulu Natal, it was reported that women who intended to use replacement feeding were more likely to have access to clean water and a regular income.[40] Similarly, in a cross-sectional study in Eastern Uganda, the higher the educational levels and socio-economic status of women, the more likely they were to adopt appropriate infant feeding practices.[41] In a rural Kisumu District, in Kenya, higher socioeconomic status was significantly associated with lower risks of premature cessation of EBF.[42]
Cultural and Social Norms and Practices of Infant Feeding Options
International guidelineson infant feeding for HIV-positive mothers promote replacement feeding (infant formula or animal milk) or exclusive breastfeeding (with no supplements of any kind). A mixed feeding pattern, where breastfeeding is combined with other milks, liquid foods or solids, has been shown to increase the risk of transmission and is strongly discouraged. Mothers’ adoption of and adherence to the recommended feeding methods is an issue.[43, 29] In the region of Sub-Saharan Africa, infant feeding practices are linked directly to a mother’s social and cultural norms.[44] Studies of feeding practices in different countries have shown a large variety of beliefs and traditions related to infant feeding. While some of these can encourage EBF or ERF others may discourage it. There are many cultural and practical obstacles to the practice of EBF.[45] Evidence has shown that some traditional beliefs, practices and rites encourage use of pre-lacteal feeds, as well as giving extra water, herbs and “teas” to breastfeeding babies.[46, 47] Moreover, feeding the infant water is also regarded as cultural gesture to welcome the child into the world.[48]
The influence that families and communities exert is the same irrespective of the HIV status of the women. Breastfeeding is seen as the only acceptable infant feeding method and the only way to fulfil ideals of a cultural norm and being a good mother.[25, 49] In a qualitative study in South Africa which examined infant feeding decision making and practices among HIV-positive women, it was found that key characteristics of women who achieved success in exclusivity (either in their breastfeeding or formula feeding) included the ability to resist pressure from the family to introduce other fluids and to recall key messages on MTCT risks and mixed feeding.[50]
In addition, societal expectations and norms also exert a powerful influence. In Botswana, it was found that although formula feeding among HIV-positive women was strongly encouraged by counsellors and formula was provided by the clinic, women went home only to practice mixed feeding.[51] This was attributed to influences from extended families and the community members. Similarly, Omari et al. reported in Zambia that HIV-positive women changed to mixed feeding although having started out with ERF. Once again, reasons included socio-cultural and expectations of family members (partners and mothers-in-law, extended families) and community members.[52] In Tanzania, HIV-positive mothers who were not able to do exclusively replacement feeding continued mixed feeding since they believed their milk was not enough to make the baby grow ‘fat and shiny’ as expected by kin and neighbors.[53]
A study which investigated infant feeding choices and experiences of HIV-positive mothers from two Ghanaian Districts, found social pressure and local norms as factors that influenced mothers decisions to mixed feed their children.[54] From the review, it is clear that in all cultures there are a number of factors that affect women’s decisions on how to feed their children.
Discussion
From this review, it is clear that in many African settings breastfeeding initiation is near universal, and early mixed feeding patterns are deeply entrenched. Adopting either EBF or ERF represents departures from the social norms. While counseling is important and a necessary condition for improved feeding choices for HIV-positive mothers, the impact of counseling about breastfeeding risks and alternative feeding methods has also not been adequate. Furthermore, the influence of socio-economic factors, family and community members often result in women not being able to adhere to the recommended infant feeding options.[49, 53]
Infant feeding represents a great challenge in the prevention of MTCT of HIV in Sub-Sahara Africa. Based on the review of the literature, we hypothesized that decisions by HIV-positive mothers with regards to infant feeding is influenced by three important sets of factors. These include knowledge of the feeding guidelines for infants born to HIV-positive mothers, socio-economic status of HIV-positive mothers and cultural norms and practices. Not only that, but also influences by their spouses/partners, family members and the community at large. These factors are linked to the issues of affordability, availability, acceptability, and sustainability of different feeding options and finally the decision by the mother to adopt a particular option or combination thereof.
Socio-economic status of HIV-positive mothers more specifically is determined by a range of factors including the mothers’ and their spouses’ professional status, Socio-economic status of her family[37-39] and educational levels.[41] Education also impacts positively on employment and income with implications for issues of affordability.[24, 55] Mothers with higher educational levels are more likely to be socio-economically better off, are more likely to adopt healthy infant feeding practices.[56] It is not surprising then that infant feeding options which often include financial considerations (e.g. cost of formula) and require access to clean water and sanitation need to be considered as important influences on the decision-making process of HIV-positive mothers. It is obvious that the socio-economic position of HIV-positive women is an important factor which influences the infant feeding decision-making process and can often explain why women who indicate their intention to replacement feed, change their decisions postpartum because of the financial challenges they face. This underscores the importance of counseling and support which extends beyond the antenatal period. In a global context of widespread impoverishment especially in developing countries, there is the need for countries to re-examine their infant-feeding policies in relation to broader socioeconomic issues and realities facing women and families.[57]
From this review, it is clear that infant feeding counseling is an important intervention for the prevention of PMTCT of HIV. PMTCT interventions include HIV testing and counseling, antiretroviral prophylaxis or treatment for mother and infant, modified obstetric practices, and support for infant-feeding practices.[5] The World Health Organization advises that HIV-positive mothers should be offered nondirective counseling on various infant feeding options that are feasible, affordable, safe, sustainable, and effective in the local context. Comprehensive PMTCT of HIV programs have nearly eliminated MTCT in developed countries.[58] However, progress in implementing PMTCT interventions in resource-limited countries has been slow.[59] It is against this background that Coutsoudis and colleagues recommend investments in high-quality, widely available HIV counseling support for choice of feeding methods for HIV-positive mothers.[60]
Clearly, counseling in the context of MTCT calls for adequate training of health workers and lay counsellors in infant feeding counseling skills, followed by monitoring and supervision which can lead to effective support to mothers in areas of high HIV prevalence. Such efforts have resulted in reduced mixed feeding and increased EBF and ERF. Counseling approaches need to effectively guide women to informed choices with support available to make these choices viable and sustainable. Reducing transmission of HIV through breast milk is dependent on the knowledge and understanding of these mothers and the quality of counseling information given to them by PMTCT counsellors or health workers. Poor quality of counseling is likely to reduce the effectiveness of these programs on infant feeding interventions in the context of HIV/AIDS. Therefore it is important that HIV-positive mothers are provided with correct information during counseling on infant feeding options to enable them choose a feeding option and adhere to it. To support counseling on HIV and infant feeding as a routine part of Maternal and Child Health, health workers and PMTCT counsellors need to be trained to provide culturally compatible counseling support that improves self-esteem and confidence and corresponds with the social norms and perceptions of mothers.
As noted earlier in this review, mixed-feeding and not exclusive breast-feeding is the norm in many cultures across the sub-Saharan Africa region. These practices are also embedded within cultural norms where communities, husbands and other significant family members play a decisive role in infant feeding decisions. Understanding and addressing local beliefs and customs can help counsellors to provide more culturally appropriate counseling about breastfeeding. Therefore, unless local beliefs and customs surrounding infant feeding and the socio-cultural aspects of HIV/AIDS is understood by policy makers and program implementers, PMTCT programs will only be partially successful in influencing feeding practices of HIV-positive women.
Conclusion and Global Health Implication
In conclusion, guidelines for infant feeding options among HIV-positive mothers are changing with informative research. Cultural factors, socialization processes, gender dimensions and socio-economic status within communities and families should be considered in recommending feasible and sustainable options. Hence, the need to take into account the social, cultural and psychological complexity of infant feeding practices when advocating appropriate infant feeding options. The need for further research into infant feeding in the context of HIV to ascertain the safety of using animal’s milk (cow’s milk), expressed heat-treated human milk and wet-nursing as infant feeding options. Finally, development of appropriate, locally produced, feasible, sustainable and affordable local nutritive foods for children in Sub-Saharan Africa.
Acknowledgements:
The authors wish to express their sincere gratitude to Swedish International Development Agency (SIDA) for the scholarship granted to the corresponding author to pursue the masters’ program.
References
- 1.UNAIDS. UNAIDS Report on the Global AIDS Epidemic. 2010. [Accessed September 13 2012]. Available at: http://www.unaids.org/en/dataanalysis/knowyourepidemic/epidemiologypublications/2009 aid sepidemicupdate/
- 2.UNAIDS/WHO. Sub-Saharan Africa AIDS epidemic update regional summary. 2007. [Accessed November 5 2012]. Available at: http://data.unaids.org/pub/Report/2008/JC1526_epibriefs_sub saharan africa_en.pdf .
- 3.UNAIDS.ReportsonGlobalAIDSEpidemic. 2012. [Accessed March 4, 2013]. Availableat: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/20121120_UNAIDS_Global_Report_2012_en.pdf .
- 4.Young SL, Mbuya NNM, Chantry JC. Current Knowledge and Future Research on Infant Feeding in the Context of HIV Basic Clinical Behavioral and Programmatic. Perspectives Advances in Nutrition. 2011;2:225–243. doi: 10.3945/an.110.000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Cock KM, Fowler MG, Mercier E, de Vencenzi I, Saba J, Hoff E, et al. Prevention of mother-to-child HIV transmission in resource-poor countries: translating research into policy and practice. Journal of the American Medical Association. 2000;283(9):1175–1182. doi: 10.1001/jama.283.9.1175. [DOI] [PubMed] [Google Scholar]
- 6.Walker N, Schwartländer B, Bryce J. Meeting international goals in child survival and HIV/AIDS. The Lancet. 2002;360(9329):284–289. doi: 10.1016/S0140-6736(02)09550-8. [DOI] [PubMed] [Google Scholar]
- 7.Garenne M. The Impact of HIV/AIDS on the Health Transition among Under-Five Children in Africa. [Accessed March 8 2013];Social and Psychological Aspects of HIV/AIDS and their Ramifications. 2011 DOI:10.5772/19330. [Google Scholar]
- 8.Adetunji J. Trends in under-5 mortality rates and the HIV/AIDS epidemic. Bulletin of the World Health Organisation. 2000;78(10):1200–1206. [PMC free article] [PubMed] [Google Scholar]
- 9.Mahy M. Measuring child mortality in AIDS-affected countries. United Nations, Population Division. Doc. UN/POP/MORT/2003/15 (paper presented to the workshop on HIV/AIDS and adult mortality in developing countries) 2003. [Accessed January 2 2013]. Available at: http://www.unorg/esa/population/publications/adultmort/UNICEF_Paper15.pdf .
- 10.Korenromp EL, Arnold F, Williams BG, Nahlen BL, Snow RW. Monitoring trends in under-5 mortality rates through national birth history surveys. International Journal of Epidemiology. 2004;33(6):1293–1301. doi: 10.1093/ije/dyh182. [DOI] [PubMed] [Google Scholar]
- 11.UNAIDS/WHO. AIDS epidemic update. UNAIDS/05.19E. Geneva: UNAIDS; 2005. [Accessed March 8 2013]. Available at: http://www.unaids.org/en/media/unaids/contentassets/dataimport/publications/irc-pub06/epi_update2005_en.pdf . [Google Scholar]
- 12.Leon-Cava N, Lutter C, Ross J, Martin L. Quantifying the benefits of breastfeeding: a summary of the evidence. Washington DC: Pan American Health Organization; 2002. [Accessed March 23 2012]. Available at: http://www1.paho.org/english/ad/fch/bob-main.htm . [Google Scholar]
- 13.WHO. Infant and young child model picture for textbooks for medical students and allied health professionals. Geneva Switzerland: 2009. [Accessed February 12 2013]. Available at: http://www.ncbi.nlm.nih.gov/books/NBK148965/ [Google Scholar]
- 14.Stuebe A. The Risk of Not Breastfeeding for Mothers and Infants. Reviews in Obstetrics Gynecology. 2009;2(4):222–231. [PMC free article] [PubMed] [Google Scholar]
- 15.Moland IMK, Esterik VP, Sellen WD, De Paoli MM, Leshabari SC, Blystad A. Ways ahead: protecting, promoting and supporting breast feeding in the context of HIV. International Breastfeeding Journal. 2010;5:19. doi: 10.1186/1746-4358-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marriott MB, Campbell L, Hirsch E, Wilson D. Preliminary Data from Demographic and Health Surveys on Infant Feeding in 20 Developing Countries. Journal of Nutrition. 2007;137:518S–523S. doi: 10.1093/jn/137.2.518S. [DOI] [PubMed] [Google Scholar]
- 17.WHO. Community-based strategies for breast feeding promotion and support in developing countries. Maternal, newborn, child and adolescent health. 2003. [Accessed April 3 2013]. ISBN:9241591218. Availableat: http://www.who.int/maternal_child_adolescent/documents/9241591218/en/
- 18.UNAIDS. UNAIDS report on the global AIDS epidemic. 2012. [Accessed August 20 2013]. Available at: http://www.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/20121120_UNAIDS_Global_Report_2012_en.pdf .
- 19.Coutsoudis A. Breast-feeding and HIV transmission. Nutrition Research reviews. 2001;14(2):191–206. doi: 10.1079/NRR200123. [DOI] [PubMed] [Google Scholar]
- 20.WHO. Infant and young child feeding Media Centre Fact sheet N°342. 2011. [Accessed April 10 2012]. Available at http://www.who.int/mediacentre/factsheets/fs342/en/
- 21.Chopra M, Rollins N. Infant feeding in the time of HIV: Assessment of infant feeding policy and programs in four African countries scaling up prevention of mother to child transmission programs. Global Health Sciences Literature Digest. 2007. [Accessed September 15 2013]. Available at: http://hivinsite.ucsf.edu/InSite?page=jl-20-02 .
- 22.Shah S, Rollins NC, Bland R. Breastfeeding knowledge among health workers in rural South Africa. Journal of Tropical Paediatric. 2005;51:33–38. doi: 10.1093/tropej/fmh071. [DOI] [PubMed] [Google Scholar]
- 23.Doherty T, Chopra M, Colvin M. Counselling on infant feeding choice: Some practical realities from South Africa. Health System Trust. 2006;29:26–28. [Google Scholar]
- 24.De Paoli MM, Manongi R, Kleep KI. Factors influencing acceptability of voluntary counselling and HIV-testing among pregnant women in Northern Tanzania. AIDS Care. 2004;16(4):411–25. doi: 10.1080/09540120410001683358. [DOI] [PubMed] [Google Scholar]
- 25.Leshabari SC, Koniz-Booher P, Astrom AN, De Paoli MM, Moland KM. Translating global recommendations on HIV and infant feeding to the local context: the development of culturally sensitive counselling tools in the Kilimanjaro Region Tanzania. [Accessed January 1 2013];Implementation Science. 2006 1:22. doi: 10.1186/1748-5908-1-22. doi:10.1186/1748-5908-1-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aika AAO, Luo C, Kankasa C, Bhat GJ, Bunn J. Infant-feeding practices of mothers of known HIV status in Lusaka Zambia. Health Policy and Planning. 2003;18:156–162. doi: 10.1093/heapol/czg020. [DOI] [PubMed] [Google Scholar]
- 27.Piwoz EG, Iliff PJ, Tavengwa N, Gavin L, Marinda E, Lunney K, et al. An education and counseling programme for preventing breast-feeding-associated HIV transmission in Zimbabwe: design and impact on maternal knowledge and behaviour. Journal of Nutrition. 2005;135(4):950–955. doi: 10.1093/jn/135.4.950. [DOI] [PubMed] [Google Scholar]
- 28.Chopra M, Doherty T, Jackson D. Preventing HIV transmission to children: quality of counselling of mothers in South Africa. Acta Paediatrica. 2005;94:357–363. doi: 10.1111/j.1651-2227.2005.tb03080.x. [DOI] [PubMed] [Google Scholar]
- 29.De Paoli IMM, Manongi R, Klepp K-I. Counsellors’perspectives on antenatal HIV testing and infant feeding dilemmas facing women with HIV in northern Tanzania. Reproductive Health Matters. 2002;10:144–156. doi: 10.1016/s0968-8080(02)00088-5. [DOI] [PubMed] [Google Scholar]
- 30.Leshabari SC, Blystad A, De Paoli M, Moland KM. HIV and infant feeding counselling: challenges faced by nurse-counsellors in northern Tanzania. [Accessed March 4 2012];Human Resources for Health. 2007 5:18. doi: 10.1186/1478-4491-5-18. doi:10.1186/1478-4491-5-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ehrnst A, Zetterstrom R. Feeding practices of HIV-1-infected mothers: The role of counselors. Acta Paediatrica. 2005;94:263–265. doi: 10.1111/j.1651-2227.2005.tb03066.x. [DOI] [PubMed] [Google Scholar]
- 32.Fadnes LT. Counselling, child growth and feeding of children in Uganda in the era of HIV Contexts and consequences. The University of Bergen. 2011. [Accessed February 15 2013]. Available at: http://hdl.handle.net/1956/4785 .
- 33.Whiteside A. ‘Poverty and HIV/AIDS in Africa’. Third World Quarterly. 2002;23:313–332. [Google Scholar]
- 34.WHO. Integrating gender into HIV/AIDS programmes, review paper for expert consultation. Geneva: WHO; 2003. [Accessed March 8 2013]. Available at http://www.unfpa.org/hiv/docs/rp/integrating-gender.pdf . [Google Scholar]
- 35.De Paoli MM, Manongi R, Klepp K-I. Are infant feeding options that are recommended for mothers with HIV acceptable, feasible, affordable, sustainable and safe?Pregnant women’s perspectives. Public Health Nutrition. 2004;7:611–619. doi: 10.1079/phn2003596. [DOI] [PubMed] [Google Scholar]
- 36.Wendo C. HIV-positive mothers in Uganda resort to breastfeeding. The Lancet. 2003;16(362 (9383)):542. doi: 10.1016/S0140-6736(03)14154-2. [DOI] [PubMed] [Google Scholar]
- 37.Doherty T, Chopra M, Nkonki L, Jackson D, Persson L. A Longitudinal Qualitative Study of Infant-Feeding Decision Making and Practices among HIV-Positive Women in South Africa. Journal of Nutrition. 2006;136:2421–2426. doi: 10.1093/jn/136.9.2421. [DOI] [PubMed] [Google Scholar]
- 38.Kiarie JN, Richardson BA, Mbori-Ngacha D, Nduati RW, John-Stewart GC. Infant feeding practices of women in a perinatal HIV-1 prevention study in Nairobi Kenya. Journal of Acquired Immune Deficiency Syndrome. 2004;35:75–81. doi: 10.1097/00126334-200401010-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sadoh E, Adeniran A, Abhulimhen-Iyoha I. Infant-feeding Practices among HIV-infected Mothers in an HIV-treatment Programme. Health Population & nutrition Journal. 2008;26:463–467. doi: 10.3329/jhpn.v26i4.1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bland RM, Rollins NC, Coovadia HM, Coutsoudis A, Newell ML. Infant feeding counseling for HIV-infected and uninfected women: appropriateness of choice and practice. Bulletin of World Health Organization. 2007;85(4):289–296. doi: 10.2471/BLT.06.032441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Fadnes LT, Engebretsen IMS, Wamani H, Semiyaga NB, Tylleskar T, Tumwine JK. Infant feeding among HIV-positive mothers and the general population mothers: comparison of two cross-sectional surveys in Eastern Uganda. [Accessed December 21 2012];BioMed Central Public Health. 2009 9:124. doi: 10.1186/1471-2458-9-124. doi:10.1186/1471-2458-9-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gewa AC, Oguttu M, Savaglio L. Determinants of Early Child-Feeding Practices among HIV-Infected and Non- infected Mothers in Rural Kenya. Journal of Human Lactation. 2011;27:239–249. doi: 10.1177/0890334411403930. [DOI] [PubMed] [Google Scholar]
- 43.WHO. Guidelines on HIV and infant feeding. Principles and recommendations for infant feeding in the context of HIV and a summary of evidence. 2010. [Accessed January 25 2012]. Available at http://www.who.int/maternal_child_adolescent/documents/9789241599535/en/ [PubMed]
- 44.Titus RR. HIV and child nutrition: A qualitative study on mothers’ narratives on exclusivity in infant feeding practices in Ravensmead and Elsies River, Western Cape, South Africa. International AIDS Conference: Abstract no. D12537 [Google Scholar]
- 45.Nankunda J, Tumwine JK, Solvedt A, Semiyaga N, Ndeezi G, Tylleskar T. Community based peer counsellors for support of exclusive breastfeeding: experiences from rural Uganda. International Breastfeeding Journal. 2006;1:19. doi: 10.1186/1746-4358-1-19. doi:10.1186/1746-4358-1-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shirima R, Gebre-Medhin M, Greiner T. Information and socioeconomic factors associated with early breastfeeding practices in rural and urban Morogoro Tanzania. Acta Paediatrica. 2001;90:936–942. [PubMed] [Google Scholar]
- 47.Nwankwo BO, Brieger WR. Exclusive breastfeeding is undermined by use of other liquids in rural south western Nigeria. Journal Tropical Pediatrica. 2002;48:109–112. doi: 10.1093/tropej/48.2.109. [DOI] [PubMed] [Google Scholar]
- 48.Davis P, Tagoe-Darko E, Mukuria A. Water Koko and Complementary Feeding Practices in Kumasi Ghana. ORC Macro Calverton Maryland (MEASURE DHS) 2003 [Google Scholar]
- 49.Njunga J. Infant Feeding Experiences of HIV positive mothers enrolled in Prevention of Mother -to -Child Transmission (PMTCT) programmes. The case for Rural Malawi. Medical School of Densitory Norway University of Bergin, UniversitetetiBergen(UiB) 2008. [Accessed June 6 2012]. Available at: https://bora.uib.no/bitstream/handle/1956/2883/47446228.pdf?sequence=1 .
- 50.Doherty T, Chopra M, Nkonki L, Jackson D, Greiner T. “Effect of the HIV epidemic on infant feeding in South Africa:” when they see me coming with the tins they laugh at me. Bulletin of World Health Organisation. 2006;84(2):90–96. doi: 10.2471/blt.04.019448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shapiro RL, Lockman S, Thior I, Stocking L, Kebaabetswe P, Wester C. Low adherence to recommended infant feeding strategies among HIV-infected women: results from the pilot phase of a randomized trial to prevent mother-to-child transmission in Botswana. AIDS Education & Prevention. 2003;15:221–230. doi: 10.1521/aeap.15.4.221.23830. [DOI] [PubMed] [Google Scholar]
- 52.Omari AA, Luo C, Kankasa C, Bhat GJ, Bunn J. Infant-feeding practices of mothers of known HIV status in Lusaka Zambia. Health Policy Plan. 2003;18(2):156–162. doi: 10.1093/heapol/czg020. [DOI] [PubMed] [Google Scholar]
- 53.Leshabari SC, Blystad A, Moland K. Difficult choices: infant feeding experiences of HIV-positive mothers in northern Tanzania Social Aspects of HIV and AIDS. Research Alliance Journal. 2007;4:544–555. doi: 10.1080/17290376.2007.9724816. [DOI] [PubMed] [Google Scholar]
- 54.Laar AK, Ampofo W, Tuakli JM, Quakyi A. I Infant feeding choices and experiences of HIV-positive mothers from two Ghanaian districts. Journal of AIDS and HIV Research. 2009;1:008–017. [Google Scholar]
- 55.Abiona TC, Onayade AA, Ijadunola KT, Obiajunwa PO, Aina OI, Thairu LN. Acceptability feasibility and affordability of infant feeding options for HIV-infected women: a qualitative study in south-west Nigeria. Maternal and Child Nutrition. 2006;2:135–144. doi: 10.1111/j.1740-8709.2006.00050.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Swarts S, Kruger HS, Dolman RC. ‘Factors affecting mothers’ choice of breastfeeding vs. formula feeding in the lower Umfolozi district war memorial, KwaZulu-Natal. Journal of Interdisciplinary Health Sciences. 2010;15(1):1–8. [Google Scholar]
- 57.Coutsoudis A, Coovadia HM, Wilfert CM. HIV infant feeding and more perils for poor people: new WHO guidelines encourage review of formula milk policies. Bulletin of World Health Organization. 2008;86(3):210–4. doi: 10.2471/BLT.07.041673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.WHO/UNAIDS/UNICEF. GLOBAL HIV/AIDS RESPONSE-Epidemic update and health sector progress towards Universal Access-Progress Report 2011. [Accessed December 10 2012]. Available at http://www.unaids.org/en/media/unaids/contentassets/documents/unaids publication/2011/201111 30_ua_report_en.pdf .
- 59.Dabis F, Ekpin E. HIV-1/AIDS and maternal and child health in Africa. Lancet. 2002;359:2097–2104. doi: 10.1016/S0140-6736(02)08909-2. [DOI] [PubMed] [Google Scholar]
- 60.Coutsoudis A, Goga AE, Rollins N, Coovadia HM, Child Health Group Free Formula milk for infants of HIV-infected women: blessing or curse? Health Policy Plan. 2002;17(2):154–60. doi: 10.1093/heapol/17.2.154. [DOI] [PubMed] [Google Scholar]


