Abstract
A cornerstone of sexually transmitted infection (STI) prevention is the identification, tracing, and notification of sex partners of index patients. Although partner notification reduces disease burden and prevents new infections as well as reinfections, studies show that only a limited number of partners are ever notified. Electronic communication technologies, namely, the Internet, text messaging, and phone calls (i.e., e-notification), have the potential to expand partner services. We conducted a systematic review of studies that have investigated the acceptability and utility of e-notification. We identified 23 studies that met the following criteria: (a) 9 studies presented data on the acceptability of technology-based communications for contacting sex partner(s), and (b) 14 studies reported on the utilization of communication technologies for partner notification. Studies found high levels of interest in and acceptability of e-notification; however, there was little evidence for actual use of e-notification. Taken together, results suggest that electronic communications could have their greatest impact in notifying less committed partners who would otherwise be uninformed of their STI exposure. In addition, all studies to date have been conducted in resource-rich countries, although the low cost of e-notification may have its greatest impact in resource-constrained settings. Research is needed to determine the best practices for exploiting the opportunities afforded by electronic communications for expanding STI partner services.
Identifying, notifying, and treating sexually transmitted infection (STI) patients’ partners is the foundation of public health approaches aimed to stop the spread of STI. Treating sex partners prevents reinfection of index patients, decreases the disease burden in sexual networks, and prevents forward STI transmission. When performed by public health workers, partner notification requires index patients to confidentially reveal the names of recent partners, who are then traced and notified by health department workers. Although provider-initiated partner notification is the most reliable means of knowing whether partners are in fact informed, the costs associated with provider-initiated partner notification are prohibitive in resource-limited settings (Trelle, Shang, Nartey, Cassell, & Low, 2007). In addition, provider-initiated notification may not be preferred by patients and can result in uninformed partners. For example, Wohlfeiler and colleagues (2013) found that 2 out of 3 men sampled from a high-risk community did not endorse provider-initiated partner notification.
As a low-cost and potentially more acceptable alternative to provider-initiated partner notification, index patients themselves can be encouraged to notify their sex partners. Patient-initiated partner notification is therefore often encouraged and may be the only option for partner services in resource-limited settings. Although essential to reducing STI transmission, both provider- and patient-initiated partner notification inform less than 40% of sex partners (Trelle et al., 2007). Outcomes are even less encouraging in developing countries, where current partner notification and referral practices fail to reach the majority of partners.
Failure to inform partners of their exposure to STI leaves sexual network members potentially infectious. Furthermore, a significant number of uninformed and infected individuals remain asymptomatic and therefore untreated. One study showed that between 22% and 68% of men with gonorrhea who were notified by partners had asymptomatic infections (Klann et al., 2014). Increasing the capacity to detect and treat STI in sex partners of index patients can therefore impact entire sex networks and significantly reduce the rate of new infections (Fenton et al., 1997; Fenton & Peterman, 1997).
Standard practices of patient-initiated partner notification involve (a) brief educational messages delivered during clinical consultation and (b) the use of partner referral cards. Unfortunately, only a small fraction of partner notification cards are ever returned to clinics, suggesting that relatively few partners are ultimately treated (Steen & Dallabetta, 2003; Swendeman, Grusky, & Swanson, 2009). Because the STI reproductive rate is in part a function of contact frequency with infected partners, strategies to enhance partner notification will have greater public health significance than behavior change interventions that focus solely on index patients. Unfortunately, interventions designed to maximize the coverage of face-to-face patient-initiated partner notification services have had limited success (Udeagu et al., 2014).
Electronic communication technologies have the potential to reduce costs, expand coverage, and increase efficiency of both provider- and patient-initiated partner notification services. It is estimated that nearly half of the world’s population has access to the Internet (Internet Live Stats, 2015), and more than 3 out of 4 people in the world have cell phones (World Bank, 2012). The Internet affords index patients options to initiate partner notification while remaining anonymous through the use of Web-based portals and e-cards. Internet-based partner notification services may also fit the relationship context for partners who are met online. Providers and patients can use cell phones and text messaging services to contact partners in ways that were not possible prior to increased access to communication technologies.
In this article we review the empirical research on the acceptability and utilization of electronic communication technologies for STI partner notification. We conducted a systematic review that included provider and patient applications of Web-based and cell phone–based communications for tracing and notifying sex partners of STI index patients. We review studies that examined (a) the acceptability of and interest in using these technologies and (b) their actual utilization. We draw conclusions aimed toward exploiting the opportunities of communication technologies to expand partner notification services, particularly in resource-limited settings.
Methods
Literature Search
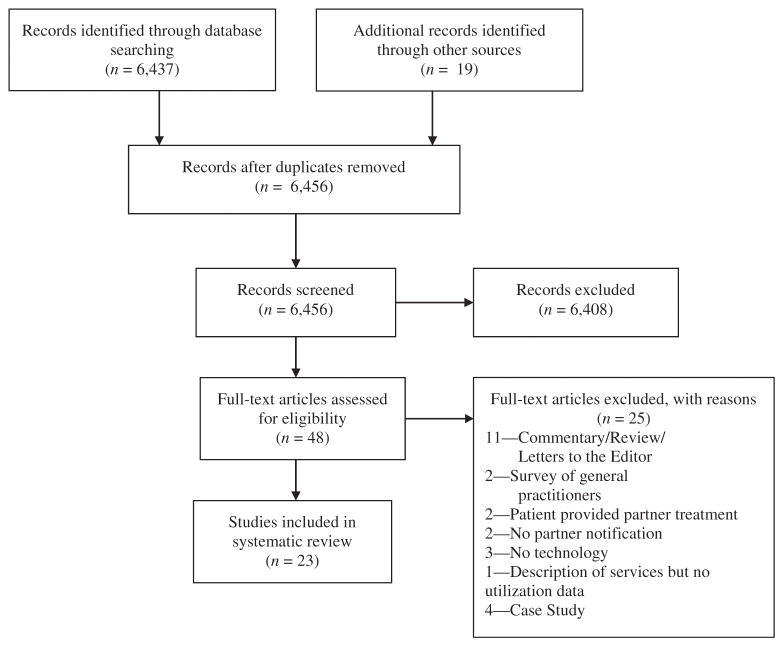
Relevant studies were located using the following search strategies. We first searched PubMed using Boolean operators: (partner notification) AND (short message service OR text message OR email OR Internet) AND (STI OR sexually transmitted infection OR STD OR sexually transmitted disease). The automated search was limited to the past 10 years because of the rapid evolution of communication technology. A total of 6,437 titles and abstracts were located (see Figure 1).
Fig. 1.
Search and retrieval strategies and results for the review of electronic communications for partner notification studies.
Following the automated searches, we performed manual searches of relevant journals (i.e., Sexually Transmitted Infections, Sexually Transmitted Diseases, Journal of Medical Internet Research, Preventive Medicine) for studies published over a 3-year period (2012 through 2014). Manual searches of journals and references identified an additional 19 studies. The search ended in December 2014. Duplicates of sources were removed, and a total of 6,456 titles and abstracts were examined to identify studies that met the following inclusion criteria: (a) presented data reporting participants’ willingness to use hypothetical or actual technology-based communication methods to contact sex partner(s) following a positive STI diagnosis; or (b) presented data on actual usage of communication technologies for partner notification, including websites and online partner notification services. Exclusion criteria included (a) reviews, opinions, or commentaries; (b) surveys of practitioners; (c) patient-delivered partner therapy (PDPT) without communication technology; (d) partner notification without communication technology; or (e) descriptions of communication technologies without data.
Results
Following a text-based screening strategy we retained 48 articles, 23 of which were eligible for inclusion. We identified nine studies that assessed acceptability of and interest in using communication technology-based methods to notify sex partners following an STI diagnosis (see Table 1) and 14 studies that examined actual utilization of these methods (see Table 2).
Table 1.
Studies on the acceptability of electronic communication technologies for partner notification
| Author (year) | Study sample | Race/ethnicity | Setting and research design | Technology | STI notification | Key findings |
|---|---|---|---|---|---|---|
| Kerani et al. (2013) | 182 MSM | NR | STI clinic, Seattle, Washington, USA; cross-sectional survey | Anonymous e-card (inSPOT Internet server) | HIV, STD | Receiving an e-card reduced the likelihood of seeking STI testing by 20% and HIV testing by 8%. |
| Wohlfeiler et al. (2013) | 3,050 MSM website users | 69% White, 13% Black, 8% Latino | Internet, USA; cross-sectional survey | Anonymous e-card | HIV, STD | A total of 67% of MSM website users indicated likely use of anonymous e-cards. |
| Mimiaga, Fair, et al. (2008), Mimiaga, Tetu, et al. (2008) | 1,848 MSM | 80% White, 4% Black, 8% Hispanic, 8% other | Internet, USA; cross-sectional survey | Personal e-mail | HIV, syphilis, gonorrhea, chlamydia | A total of 92% would use the Internet to notify a partner; 32% would have the health department notify and 38% would self-notify. Notification varied by HIV status, with HIV-positive men less inclined to notify partners via the Internet. |
| Apoola et al. (2006) | 1,055 men, 1,474 women clinic patients | 72% White, 13% Black, 15% other | Birmingham, Derby, Coventry, UK; cross-sectional survey | Text message, personal e-mail | STIs (general) | Text messaging and e-mail were not acceptable for partner notification. |
| Woodward et al. (2010) | 85 MSM, HIV positive | 80% White | Bloomsburg Clinic, Mortimer Market Centre, UK; cross-sectional survey | Clinic originating text message and personal e-mail, and anonymous e-cards | STIs (general) | Text messages and e-mails sent by the clinic and anonymous e-cards were similarly and moderately acceptable. |
| Clark et al. (2014) | 397 MSM HIV/STI patients | NR | STD clinic; Lima, Peru; cross-sectional survey | Anonymous e-cards | HIV, STIs (general) | A total of 59% anticipated the use of a Internet-based notification system: 57% for a main partner, 54% for casual partners, 23% for commercial partners. |
| Bilardi, Fairley, Hopkins, Hocking, Temple-Smith, et al. (2010) | 202 heterosexual men and women, and MSM STI patients | NR | Melbourne, Canberra, and Cairns, Australia; phone interview | Text message, e-mail | Chlamydia | A total of 47% expressed interest in notification via the Internet; 34% stated that they would have contacted more partners had technology-based tools been available. |
| Rietmeijer et al. (2011) | 481 men and women STI patients | 37% White, 29% Black, 27% Hispanic, | Denver, Colorado, USA; cross-sectional survey | e-card, Colorado inSPOT | Gonorrhea, chlamydia | A total of 89% said that they would notify partners in person, 37% by phone, 11% by text message, 4% by e-mail. |
| Hopkins et al., 2010 | 25 women and 15 men STI patients | NR | Victoria and Queensland, Australia; in-depth interviews | Phone calls, text messages, personal e-mail | Chlamydia | Patients most often contacted partners in person or phone; texting and e-mail were used when in-person or phone contacts were not feasible. |
Note. STI = sexually transmitted infection; MSM = men who have sex with men; NR = not reported; USA = United States of America; STD = sexually transmitted disease; UK = United Kingdom.
Table 2.
Studies on the utilization of electronic communication technologies for partner notification
| Author (year) | Study sample | Race/ethnicity | Setting and research design | Technology | STI notification | Key findings |
|---|---|---|---|---|---|---|
| Levine et al. (2008) | Data from more than 30,000 website visitors | NR | 17 U.S. cities; Ottawa and Toronto, Canada; and Romania. Implemented program evaluation | inSpot.org e-card delivery website | HIV, syphilis, gonorrhea, chlamydia | Daily use of inSpot.org exceeds 750 visits; 16,983 e-cards were sent in 1 year; 2%–4% of participants in the evaluation received or sent an e-card. |
| Rietmeijer et al. (2011) | 934 men and women STI clinic patients | 38% White, 27% Black, 30% Hispanic | Denver, Colorado, USA; two cross-sectional surveys | Colorado inSpot.org e-card delivery website | Gonorrhea, chlamydia | Use of e-cards increased significantly following implementation of an online banner ad. |
| Plant et al. (2012) | Baseline = 509 MSM STI clinic patients | 49% White, 13% Black, 28% Latino/Hispanic | Los Angeles, California, USA; cross-sectional surveys before and after an advertising campaign | inSPOTLA.org e-card delivery website | Gonorrhea, chlamydia, syphilis, genital herpes, HIV | A total of 15% were aware of the e-card website at baseline with no increase in advertising campaign; only 1% of patients reported sending an e-card to partners. |
| Kerani et al. (2011) | 75 MSM STI clinic patients | 76% White, 5% Black, 7% Hispanic, 12% other | Seattle, Washington, USA; randomized four-condition trial: (a) PDPT, (b) use of inSPOT, (c) PDPT and inSPOT, (d) standard clinic services | inSpot.org e-card delivery website | Gonorrhea, chlamydia | A total of 4% of the inSPOT condition used an e-card to notify a partner; inSPOT did not increase notification and had less partners receive HIV testing. |
| Bilardi, Fairley, Hopkins, Hocking, Sze, et al. (2010) | 5,785 heterosexual men and women new website users | NR | Australia; website utilization monitoring | letthemknow.org.au, e-mail, text message delivery website | Chlamydia | New users of the website service and e-mail and text messages sent through the service increased over the evaluation period. |
| Huffam et al. (2013) | 1,381 consecutive website users | NR | Australia; website utilization monitoring | letthemknow.org.au, e-mail, text message delivery website | Gonorrhea, chlamydia, syphilis, trichomonas | A total of 37% of website visitors sent messages to partners. |
| Tomnay et al. (2006) | 76 men and 29 women STI clinic patients | NR | Victoria; Australia; randomized two-condition trial: (a) access to a partner notification assistance website, (b) standard clinic services | Website designed to assist with partner notification | Chlamydia, non-gonoccocal urethritis | Access to the partner notification website did not increase partner notification. |
| Bourne et al. (2012) | 1,278 MSM recruited from community events and social venues | 73% Anglo-Australian, 27% other | Sydney, Australia; community-based cross-sectional surveys during website promotion | Whytest.org e-mail, text message delivery website | Gonorrhea, chlamydia, syphilis infection, and HIV | Website promotion significantly increased messages sent, with 96% of messages sent by text and 4% by e-card. |
| Gotz et al. (2014) | 988 STI clinic patients receiving a partner notification code | NR | Amsterdam and Rotterdam, The Netherlands; cross-sectional survey | Suggestatest.nl, e-mail, text message delivery website | Gonorrhea, chlamydia, syphilis, HIV | A total of 14% of patients used the system to notify partners; 84% used text messaging, 15% sent e-mail, 1% sent an anonymous e-card. |
| Vest et al. (2007) | 53 STI patients with partner e-mail as only contact information and 265 unmatched patient controls | 73% White, 9% Black, 13% Hispanic, 3% other | Austin, Texas, USA; case control study of provider notification by e-mail | Provider delivered notification to partner e-mail | HIV, syphilis | A total of 49% of the partners were notified using e-mail, 80% came for clinic services. |
| Bilardi, Fairley, Hopkins, Hocking, Temple-Smith, et al. (2010) | 202 heterosexual men, women, and MSM STI clinic patients | NR | Melbourne, Canberra, and Cairns, Australia; phone interview following diagnosis | Text message, personal e-mail | Chlamydia | A total of 8% used e-mail and 11% used text messaging to notify partners. |
| Udeagu et al. (2014) | 3,247 HIV partner services clients | 11% White, 43% Black, 34% Hispanic, 10% other | New York, USA; comparison of three services: (a) e-mail, (b) text messaging, (c) standard partner referral | Personal e-mail and text message | HIV | Group comparisons showed that 41% of partners in the e-mail service were notified; 77% of partners in the text message service were notified; 69% of partners in the standard services group were notified. |
| Hightow-Weidman et al. (2014) | 588 partner notification contacts made through STI clinic services | 23% White, 59% Black, 11% Hispanic | North Carolina, USA; evaluation of expanded partner services using e-mail and texting | Personal e-mail, text message | HIV, syphilis | Partner notification increased with the use of e-mail and texting from 26% notified to 63% notified; 29 partners who could not be notified otherwise were contacted by text message. |
| Ehlman et al. (2010) | 337 men and 24 women diagnosed with early-stage syphilis | 29% White, 61% Black, 2% Asian, 7% other | Washington, DC, USA; evaluation of health department use of the Internet | Online system: Internet-based partner notification program | Syphilis | A total of 43% of partners were traced using Internet service, resulting in an 83% increase in partners notified and a 26% increase in partners examined medically. |
Note. STI = sexually transmitted infection; NR = not reported; USA = United States of America; MSM = men who have sex with men; PDPT = patient-delivered partner therapy.
Acceptability of Communication Technology-Based Partner Notification
We reviewed studies of technology-based methods for partner notification that included acceptance of notifying partners and/or acceptance of being notified by partners. Studies assessed interest in using Web-based systems for notification, usually anonymously, or the use of personal contact with partners via e-mail or text messaging. In addition, we identified studies that focused on communicating with partners by phone rather than in person.
Sending Web-Based Partner Notification E-Cards
Web-based systems for partner notification generally involve entering an Internet portal to send anonymous e-cards. Studies that examined interest in and acceptability of sending e-cards to partners following an STI diagnosis were conducted in the United States, the United Kingdom, and Peru. One study of men who have sex with men (MSM) receiving STI clinic services in Seattle, Washington, found that 56% of patients indicated that they would use an anonymous e-card to notify sex partners, and 45% stated that they would be more likely to notify partners if this option were available (Kerani, Fleming, DeYoung, & Golden, 2011). A Web-based survey of MSM found that 70% preferred that a public health worker inform partners and 22% preferred to self-notify (Mimiaga, Tetu, et al., 2008). However, when e-mail was offered as an option, 37% of men would have a public health worker notify using e-mail compared to 32% who would use anonymous e-cards themselves. In contrast to MSM surveyed online, acceptance of anonymous e-cards was low among STI clinic patients, with less than 5% of patients indicating that they would use anonymous e-cards to notify partners (Rietmeijer et al., 2011).
Web-based partner notification is not necessarily acceptable for all types of partners but may be for those partners who would not otherwise be notified. One study of MSM in Lima, Peru, who had recently been diagnosed with an STI found that 88% were likely to notify their partners, especially their primary sex partners (Clark et al., 2014). Although men were inclined to personally notify their primary partners, they were less likely to notify other partners, for which using the Internet was seen as a viable option. Overall, 53% of the primary partners who would not be notified personally would receive an e-card if available.
Receiving Web-Based Partner Notification E-Cards
We identified one study that assessed the acceptability of receiving an e-card notification of exposure to an STI (Kerani, Fleming, & Golden, 2013). In this study men were asked “If you received an anonymous e-mail card saying that you might have been exposed to gonorrhea or chlamydia by a sex partner, would you go get tested?” Individuals were asked the same question regarding a partner telling them of the exposure face to face. Results showed that 64% said that they would get tested after receiving an e-card compared to 89% after being told face to face, a significant difference. Overall, 60% of participants indicated that the form of communication would not matter, but the anonymity of the e-card raised concerns about trusting the information; 77% of men would seek testing if the e-card was anonymous compared to 98% who would get tested after receiving a personal e-mail from a partner.
Text Messaging, Personal E-Mail, and Phone Calls
Unlike e-cards, text messages, e-mails, and phone calls are not anonymous. In a study conducted with recently diagnosed STI patients in Australia, Hopkins and colleagues (2010) found that nearly all patients had contacted their past partners, with half doing so face to face and slightly less than half calling partners on the phone. Most patients felt that sending a text message was too impersonal. Those few persons who did send a text message confirmed this sentiment, stating that they used text messaging because they did not know the partner well or did not particularly care for the partner. Some patients, however, followed phone conversations with text messages to provide information about where to receive services. In addition, patients sent text messages or personal e-mails when partners were away or unable to be reached by phone. Bilardi, Fairley, Hopkins, Hocking, Temple-Smith, and colleagues (2010) reported limited interest in another Australian sample, with 16% of MSM, 12% of women, and 4% of heterosexual men expressing interest in using e-mail or text messaging to notify partners.
Mimiaga, Fair, and colleagues (2008) found that 92% of MSM surveyed from websites on which men were seeking sex partners stated that they would use e-mail if available, sent either by himself or by the health department, to notify sex partners of an STI. However, men who had a previous STI were significantly less likely to self-notify and more likely to have the health department notify using e-mail. HIV-negative men were significantly more likely than HIV-positive men to indicate that information about having contracted the STI, links to educational materials, and details about how to contact the health department are important to include in e-mails. Other studies have reported that including links to STI information online along with notification e-mails is acceptable (Woodward, Roedling, Edwards, Armstrong, & Richens, 2010). Unfortunately, text messaging and e-mail notification have not received broad support. One study found that only 11% of STI clinic patients in Denver, Colorado, would use text messaging to notify partners (Rietmeijer et al., 2011). Another survey of men and women clinic patients in the United Kingdom found little support for the use of text messaging and e-mail for partner notification (Apoola et al., 2006). Approximately two thirds of survey participants believed that receiving a text message or e-mail informing them that they may have an STI was a bad method of notification, relative to two thirds of individuals believing that being directly informed by a partner is a good method.
Telephone calls represent the technological option that is closest to a face-to-face conversation. Calling on the phone may be particularly useful for geographically distant partners and as a means of reducing perceived physical risks conferred by a face-to-face meeting. One in three STI clinic patients have been found to be likely to use the phone to notify their partners of an STI (Rietmeijer et al., 2011). Another study found that 56% of MSM would be more likely to respond proactively if they received a phone message from a sex partner relative to anonymous e-cards (Kerani et al., 2013). When multiple options were presented from which patients could choose, 62% of patients preferred notifying partners by phone compared to 53% who preferred in person, 45% who preferred e-mail, and 39% who preferred anonymous e-cards.
Actual Use of Technology-Based Partner Notification
This group of studies examined the utilization of communication technologies for partner notification. The majority of studies focused on partner notification delivered via websites that allow users to send e-mails/e-cards or text messages to anonymously inform partners.
Web-Based Partner Notification
The most commonly studied Web-based platform for partner notification is the anonymous e-card system www.inSpot.org. In addition to providing information on local STI testing sites, individuals can send anonymous or confidential e-cards to notify partners of STI exposure. E-cards link the receiver to the inSpot.org webpage with disease-specific information and the location of STI service providers. Levine, Woodruff, Mocello, Lebrija, and Klausner (2008) evaluated inSpot.org in 10 cities in three countries (the United States, Canada, and Romania) and found that nearly 50,000 e-cards had been sent from more than 30,000 unique users. In just over 2 years, more than 29,000 people accessed STI testing information as a result of receiving an inSpot.org e-card.
An extensive evaluation of inSpot.org was conducted in Colorado with STI patients receiving services from a public health clinic (Rietmeijer et al., 2011). In the span of a year and a half, 1,885 e-cards were sent. Two cross-sectional surveys were also conducted that corresponded with before and after the launch of inSpot.org promotion campaigns. There was a significant increase in the number of users of the site following implementation of the campaign. There was also a slight increase in the number of participants who ever sent an e-card; however, this was not statistically significant. Following the campaign, 89% of respondents indicated that they would still most likely notify partners face to face.
inSpot.org has also been evaluated in Los Angeles, California, where the public’s awareness of www.inspot.org was assessed before and after a promotional campaign using cross-sectional surveys (Plant, Rotblatt, Montoya, Rudy, & Kerndt, 2012). The baseline survey indicated that 15% of participants were aware of the website, which did not change following advertisements in English and Spanish placed in local gay magazines, restaurants, and nightclubs. The number of participants who reported using the site increased slightly but not statistically significantly (baseline = 0.5%, follow-up = 1.3%).
Finally, the effects of inSpot.org were also tested in a randomized controlled trial. Kerani and colleagues (2011) assigned 75 MSM to one of four conditions: (a) PDPT, (b) inSpot.org, (c) combined PDPT and inSpot.org, or (d) standard services that sought to notify partners by the health department. Participants who were randomized to either the inSpot.org condition or the PDPT and inSpot.org condition were given the opportunity to use a clinic computer to visit the inSpot.org website. In addition, they received a card with the website address for inSpot.org to access the site at a later time. Results showed that 4% of participants randomized to an inSpot.org condition actually used the service to notify partners.
Studies have also examined the utilization of anonymous e-card systems other than inSpot.org. One such Web-based system is Letthemknow.org.au provided by the Melbourne (Australia) Sexual Health Centre. Letthemknow.org.au allows users to send anonymous e-mails or text messages for partner notification. This website also provides educational information about common STIs. One study found that during an 11-month period there was a significant increase in the number of new users and messages sent (Bilardi, Fairley, Hopkins, Hocking, Sze, et al., 2010). During this timeframe, the site was visited 6,481 times (5,785 new users), which resulted in 2,727 text messages and 108 e-mail messages being sent to partners. In a further evaluation of this website, another study found that more than one third of the website visits resulted in a text message being sent to a partner (Huffam et al., 2013).
Tomnay, Pitts, Kuo, and Fairley (2006) also conducted a randomized controlled trial in Australia to assess the utility of providing patients with a website in conjunction with standard partner services. The study found that patients who were provided with access to a website were no more likely to contact their partners than patients who only received the standard clinic services.
Whytest.org is also targeted toward gay men in Sydney, Australia, and provides information on HIV and other STIs as well as options to use a “Tell them” e-card and anonymous text messages. One evaluation of this program found that nearly 8,000 partner notification messages were sent from the website over a 3-year period (Bourne, Zablotska, Williamson, Calmette, & Guy, 2012). Of the messages sent, 4% were e-cards and 96% were text messages. The authors also conducted an online survey of MSM to assess awareness of the website. In this survey, 55% of the participants recognized the website’s images.
The final partner notification website that has been evaluated for utilization is The Netherlands–based Suggestatest.nl, designed for use within clinic settings. In this system the patient specifies his or her partner notification preferences, and anonymous cards can be created to inform partners. Notifications can be sent via e-mail, text message, a postal letter, or a private message on a dating website. The evaluation found that 46% of patients expressed the intention of using the Suggestatest.nl system to notify partners. However, only 14% ultimately used the system (Gotz et al., 2014). Of those who notified their partners via the system, 84% used text messaging, 15% used e-mail, and 1% mailed their partners postal letters.
Text Messaging and Personal E-Mail
One study examined the use of e-mail to notify partners who were only able to be contacted via their e-mail addresses (Vest, Valadez, Hanner, Lee, & Harris, 2007). Patients who used e-mail notified half of their partners, and of those 80% were examined for possible STI. However, the use of texting and e-mail was much lower in a smaller sample of men and women diagnosed with an STI in Australia, in which only six (17%) participants had sent their partners a text message as the means of notification (Hopkins et al., 2010).
A telephone-based survey of patients who were recently diagnosed with chlamydia found that of the patients who contacted their partners, 11% did so through text messages and 8% used personal e-mail (Bilardi, Fairley, Hopkins, Hocking, Temple-Smith, et al., 2010). The study also found that 47% of patients reported that they would have found a website to assist with e-mail or text message partner notification helpful. Furthermore, 34% of the patients who did not inform all of their partners said that they would have contacted more partners had Web-based tools been available.
Conclusions
Our review identified a relatively small and growing literature on the acceptability and utilization of partner notification strategies delivered through electronic communication technologies. When STI patients notify their partners face to face, the communication tends to occur soon after diagnosis, with the median time to notification occurring on the same day as the diagnosis, and 84% of patients who do notify their partners do so within 7 days of being diagnosed (Bilardi, Fairley, Hopkins, Hocking, Temple-Smith, et al., 2010). Thus, electronic communications may further enhance rapid notification. Studies reviewed found that electronic notification services are likely to be used with partners who may not be notified otherwise. Likewise, studies have found that individuals are more inclined to seek services when they are notified face to face rather than anonymously. A pattern that emerged across studies was that anonymity was less acceptable than the electronic delivery method itself. Thus, the use of open communication versus anonymity should be considered separately from the various delivery platforms when considering options for partner notification.
A crosscutting theme in the literature is the discordance between high levels of acceptability and low rates of utilization. Overall, the uptake of electronic partner notification has been slow, especially in settings where impact may be greatest. For example, patients at STI clinics, where partner notification services are often implemented, are less likely to use anonymous e-cards than individuals surveyed in communities and online. Campaigns to increase utilization of electronic notification systems have not significantly increased numbers of partners notified.
Several methodological limitations were identified in the studies reviewed. Much of the acceptability research relied on hypothetical scenarios of accessing options for partner notification. In addition, every study we identified had been conducted in resource-rich countries. With electronic communication now widely available, studies should be replicated and extended using websites and messaging services in resource-poor countries. Because electronic messages come at a low cost and can reach partners who may be geographically dispersed, these technologies may be positively received in developing countries. With global expansion of cellular services and Internet access, electronic partner notification technologies are realistic in resource-poor settings. Finally, it is important to recognize that with communication technologies rapidly improving and expanding in reach, much of the literature we reviewed is already out of date. Most of the studies we accessed had been published within 3 years of our search, but some had publication lags extending back just as long.
Electronic communications increase options for notifying partners of exposure to STI. Providing patients with more options for notification may empower them to choose a method that is best suited to their relationships and circumstances. Individuals diagnosed with an STI may choose to notify their closest partners without the use of technology, whereas they may choose to send an anonymous e-card to partners they may not otherwise notify at all. In addition, with electronic communications health departments in resource-limited settings now have access to low-cost tools for notifying partners. These new strategies offer the possibility of rendering provider referral a feasible option for resource-poor settings. Partner tracing, notification, and services that have typically been cost-prohibitive in resource-limited places may now be affordable using electronic communications. With growing concern that seeking sex partners on the Internet can amplify STI epidemics, the same advances in electronic communications can and should be enlisted as tools to reduce STI burden in sexual networks.
Acknowledgments
Funding
This research was supported by a grant from the National Institute of Child Health and Development, NIH, R01-HD074560.
References
- Apoola A, Radcliffe KW, Das S, Robshaw V, Gilleran G, Kumari BS, Rajakumar R. Patient preferences for partner notification. Sexually Transmitted Infections. 2006;82(4):327–329. doi: 10.1136/sti.2005.018119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilardi JE, Fairley CK, Hopkins CA, Hocking JS, Sze JK, Chen MY. Let Them Know: Evaluation of an online partner notification service for chlamydia that offers e-mail and SMS messaging. Sexually Transmitted Diseases. 2010;37(9):563–565. doi: 10.1097/OLQ.0b013e3181d707f1. [DOI] [PubMed] [Google Scholar]
- Bilardi JE, Fairley CK, Hopkins CA, Hocking JS, Temple-Smith MJ, Bowden FJ, Chen MY. Experiences and outcomes of partner notification among men and women recently diagnosed with chlamydia and their views on innovative resources aimed at improving notification rates. Sexually Transmitted Diseases. 2010;37(4):253–258. doi: 10.1097/OLQ.0b013e3181d012e0. [DOI] [PubMed] [Google Scholar]
- Bourne C, Zablotska I, Williamson A, Calmette Y, Guy R. Promotion and uptake of a new online partner notification and retesting reminder service for gay men. Sexual Health. 2012;9(4):360–367. doi: 10.1071/SH11132. [DOI] [PubMed] [Google Scholar]
- Clark JL, Segura ER, Perez-Brumer AG, Reisner SL, Peinado J, Salvatierra HJ, Lama JR. Potential impact and acceptability of Internet partner notification for men who have sex with men and transgender women recently diagnosed as having sexually transmitted disease in Lima, Peru. Sexually Transmitted Diseases. 2014;41(1):43–45. doi: 10.1097/OLQ.0000000000000068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlman DC, Jackson M, Saenz G, Novak DS, Kachur R, Heath JT, Furness BW. Evaluation of an innovative Internet-based partner notification program for early syphilis case management, Washington, DC, January 2007–June 2008. Sexually Transmitted Diseases. 2010;37(8):478–485. doi: 10.1097/OLQ.0b013e3181e212cb. [DOI] [PubMed] [Google Scholar]
- Fenton KA, Copas A, Johnson AM, French R, Petruckevitch A, Adler MW. HIV partner notification policy and practice within GUM clinics in England: Where are we now? Genitourinary Medicine. 1997;73(1):49–53. doi: 10.1136/sti.73.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenton KA, Peterman TA. HIV partner notification: Taking a new look. Aids. 1997;11(13):1535–1546. doi: 10.1097/00002030-199713000-00001. [DOI] [PubMed] [Google Scholar]
- Gotz HM, Van Rooijen MS, Vriens P, Op De Coul E, Hamers M, Heijman T, … Voeten HACM. Initial evaluation of use of an online partner notification tool for STI, called “suggest a test”: A cross sectional pilot study. Sexually Transmitted Infections. 2014;90(3):195–200. doi: 10.1136/sextrans-2013-051254. [DOI] [PubMed] [Google Scholar]
- Hightow-Weidman L, Beagle S, Pike E, Kuruc J, Leone P, Mobley V, … Gay C. “No one’s at home and they won’t pick up the phone”: Using the Internet and text messaging to enhance partner services in North Carolina. Sexually Transmitted Diseases. 2014;41(2):143–148. doi: 10.1097/OLQ.0000000000000087. [DOI] [PubMed] [Google Scholar]
- Hopkins CA, Temple-Smith MJ, Fairley CK, Pavlin NL, Tomnay JE, Parker RM, Chen MY. Telling partners about chlamydia: How acceptable are the new technologies? BMC Infectious Diseases. 2010;10:58. doi: 10.1186/1471-2334-10-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffam S, Fairley CK, Chung M, Sze JK, Bilardi J, Chen MY. Facilitating partner notification through an online messaging service: Let Them Know. Sexual Health. 2013;10(4):377–379. doi: 10.1071/SH13007. [DOI] [PubMed] [Google Scholar]
- Internet Live Stats. Internet users. 2015 Retrieved from http://www.inter-netlivestats.com/internet-users/
- Kerani RP, Fleming M, DeYoung B, Golden MR. A randomized, controlled trial of inSPOT and patient-delivered partner therapy for gonorrhea and chlamydial infection among men who have sex with men. Sexually Transmitted Diseases. 2011;38(10):941–946. doi: 10.1097/OLQ.0b013e318223fcbc. [DOI] [PubMed] [Google Scholar]
- Kerani RP, Fleming M, Golden MR. Acceptability and intention to seek medical care after hypothetical receipt of patient-delivered partner therapy or electronic partner notification postcards among men who have sex with men: The partner’s perspective. Sexually Transmitted Diseases. 2013;40(2):179–185. doi: 10.1097/OLQ.0b013e31827adc06. [DOI] [PubMed] [Google Scholar]
- Klann JG, Mendis M, Phillips LC, Goodson AP, Rocha BH, Goldberg HS, Murphy SN. Taking advantage of continuity of care documents to populate a research repository. Journal of the American Medical Informatics Association. 2014 doi: 10.1136/amiajnl-2014-003040. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levine D, Woodruff AJ, Mocello AR, Lebrija J, Klausner JD. inSPOT: The first online STD partner notification system using electronic postcards. PLoS Med. 2008;5(10):e213. doi: 10.1371/journal.pmed.0050213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga MJ, Fair AD, Tetu AM, Novak DS, Vanderwarker R, Bertrand T, Mayer KH. Acceptability of an Internet-based partner notification system for sexually transmitted infection exposure among men who have sex with men. American Journal of Public Health. 2008;98(6):1009–1011. doi: 10.2105/AJPH.2006.098467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mimiaga MJ, Tetu AM, Gortmaker S, Koenen KC, Fair AD, Novak DS, Mayer KH. HIV and STD status among MSM and attitudes about Internet partner notification for STD exposure. Sexually Transmitted Diseases. 2008;35(2):111–116. doi: 10.1097/OLQ.0b013e3181573d84. [DOI] [PubMed] [Google Scholar]
- Plant A, Rotblatt H, Montoya JA, Rudy ET, Kerndt PR. Evaluation of inSPOTLA.org: An Internet partner notification service. Sexually Transmitted Diseases. 2012;39(5):341–345. doi: 10.1097/OLQ.0b013e31824e5150. [DOI] [PubMed] [Google Scholar]
- Rietmeijer CA, Westergaard B, Mickiewicz TA, Richardson D, Ling S, Sapp T, McFarlane M. Evaluation of an online partner notification program. Sexually Transmitted Diseases. 2011;38(5):359–364. doi: 10.1097/OLQ.0b013e31820ef796. [DOI] [PubMed] [Google Scholar]
- Steen R, Dallabetta G. Sexually transmitted infection control with sex workers: Regular screening and presumptive treatment augment efforts to reduce risk and vulnerability. Reproductive Health Matters. 2003;11(22):74–90. doi: 10.1016/S0968-8080(03)02295-X. [DOI] [PubMed] [Google Scholar]
- Swendeman DT, Grusky O, Swanson AN. HIV partner notification: Predictors of discussion and agreements from provider reports. AIDS and Behavior. 2009;13(3):573–581. doi: 10.1007/s10461-009-9522-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomnay JE, Pitts MK, Kuo TC, Fairley CK. Does the Internet assist clients to carry out contact tracing? A randomized controlled trial using Web-based information. International Journal of STD & AIDS. 2006;17(6):391–394. doi: 10.1258/095646206777323391. [DOI] [PubMed] [Google Scholar]
- Trelle S, Shang A, Nartey L, Cassell JA, Low N. Improved effectiveness of partner notification for patients with sexually transmitted infections: Systematic review. British Medical Journal. 2007;334(7589):354. doi: 10.1136/bmj.39079.460741.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Udeagu CC, Bocour A, Shah S, Ramos Y, Gutierrez R, Shepard CW. Bringing HIV partner services into the age of social media and mobile connectivity. Sexually Transmitted Diseases. 2014;41(10):631–636. doi: 10.1097/OLQ.0000000000000181. [DOI] [PubMed] [Google Scholar]
- Vest JR, Valadez AM, Hanner A, Lee JH, Harris PB. Using e-mail to notify pseudonymous e-mail sexual partners. Sexually Transmitted Diseases. 2007;34(11):840–848. doi: 10.1097/OLQ.0b013e318073bd5d. [DOI] [PubMed] [Google Scholar]
- Wohlfeiler D, Hecht J, Volk J, Fisher Raymond H, Kennedy T, McFarland W. How can we improve online HIV and STD prevention for men who have sex with men? Perspectives of hook-up website owners, website users, and HIV/STD directors. AIDS and Behavior. 2013;17(9):3024–3033. doi: 10.1007/s10461-012-0375-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward CL, Roedling S, Edwards SG, Armstrong A, Richens J. Computer-assisted survey of attitudes to HIV and sexually transmissible infection partner notification in HIV-positive men who have sex with men. Sexual Health. 2010;7(4):460–462. doi: 10.1071/SH09146. [DOI] [PubMed] [Google Scholar]
- World Bank. Mobile phone access reaches three quarters of the planet’s population. 2012 Retrieved from http://www.worldbank.org/en/news/press-release/2012/07/17/mobile-phone-access-reaches-three-quarters-planets-population.