Abstract
Phrenic nerve palsy causing hemidiaphragm paralysis is a very uncommon feature of thoracic aortic aneurysm. In one case, a 30 year male complained of chronic dull aching chest pain, and hoarseness of voice; posteroanterior view chest radiograph revealed large spherical radiopacity on the left upper lung zone with smooth lobulated margin with elevated left hemidiaphragm. On Colour Doppler sonography, lesion was anechoic on gray scale sonography but on Doppler analysis revealed intense internal vascularity within it with characteristic “Ying Yang” sign. The finding favor the vascular origin of the lesion and a diagnosis of an arterial aneurysm was made Contrast-enhanced computed tomography (CT) of the thorax revealed a large well defined spherical lesion of 8 × 10 cm size with smooth well defined margin arising from the aortic arch and attenuation of impending rupture or dissection were lesion on immediate post contrast and delayed scan was similar to that of aorta. Left hemidiaphragm elevation was explained by the gross mass effect of the aneurysm causing right phrenic nerve palsy.
KEY WORDS: Hoarseness, phrenic nerve palsy, thoracic aortic aneurysm
INTRODUCTION
Thoracic aortic aneurysms are usually asymptomatic[1] and the chest pain is most commonly reported symptom. Left hemidiaphragm paralysis, because of left phrenic nerve palsy, is a very rare presentation of thoracic aortic aneurysm. Here, we present a case of a thoracic aortic aneurysm in a patient presented to us complaining of chest pain and hoarseness of voice, and featuring elevated left hemidiaphragm observed on posteroanterior view chest radiograph. Further investigations revealed aortic aneurysm causing left phrenic nerve palsy. The patient was referred to cardiothoracic-vascular surgery unit for surgical correction of the aneurysm. The patient recovered postoperatively. This report describes an unusual presentation of a thoracic aortic aneurysm.
CASE REPORT
A 30-year-old male presented with symptoms of hoarseness of voice for the last 1 year and dull aching chest pain on the left side since 1 year. There was no history of occurrence of fever, cough, hemoptysis, dysphagia, dyspnea, weight loss, and neuromuscular disorders. On physical examination, his vitals were within the normal limit. There was no lymphadenopathy and engorged neck vein present, and on examination of cardiovascular system and abdomen did not reveal any abnormality. On examination of respiratory system, there was decreased excursion of left lower chest and decreased movement of abdomen in left upper quadrant. Vocal fremitus was decreased in left parasternal region. On percussion dullness was present on left infraclavicular and parasternal area in 1st and 2nd intercostal space (ICS), diaphragm at the level of 4th ICS in midclavicular line on left side. There was decreased breath sound in left parasternal and lower axillary and infrascapular area, vocal resonance was bilaterally equal except in left lower axillary and infrascapular areas. There were no other predisposing risk factors found upon examination for aortic aneurysm. There were nothing significant medical or surgical history in past. Patient was nonsmoker and shopkeeper by occupation.
On laboratory examination, his complete blood count, renal function tests, liver functions tests, and lipid profile were within the normal limits. A posteroanterior view chest radiograph revealed a large spherical radiopacity on the left upper lung zone with smooth lobulated margin which appeared to merge medially forming an obtuse angle. The lesion silhouetted with aortic arch medially, along with elevated left hemidiaphragm [Figure 1]. Left lateral view chest radiograph showed sharply demarcated opacity in anterior and middle mediastinum with elevated left hemidiaphragm [Figure 1]. Ultrasonography of the abdomen was normal. Color Doppler sonography of the patient was performed using 7.5 MHZ linear array transducer. The lesion was anechoic on gray scale sonography but on Doppler analysis revealed intense internal vascularity within it with characteristic “Ying Yang” sign [Figure 2]. The findings favored the vascular origin of the lesion and a diagnosis of an arterial aneurysm was made. Contrast-enhanced computed tomography of the thorax revealed a large well defined spherical lesion of 8 cm × 10 cm size with smooth well defined margin arising from the aortic arch and attenuation of impending rupture or dissection were lesion on immediate postcontrast and delayed scan was similar to that of aorta. Thus the lesion was confirmed as saccular aneurysm of aortic arch and extending into the aortic arch with no extension into the descending aorta. No intramural thrombus was seen [Figure 3]. The patient was referred to cardiothoracic-vascular surgery unit for surgical repair of the aortic aneurysm. The patient recovered postoperatively.
Figure 1.
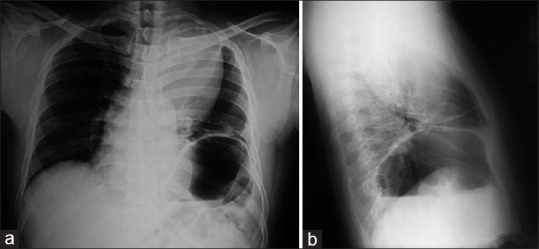
(a) X-ray chest posterioranterior view showing homogeneous opacity with well demarcated sharp interface in left upper zone merging with mediastinum and hilum overlay sign along with elevated left hemidiaphragm. (b) X-ray chest left lateral view showing sharply demarcated homogenous opacity in anterior and middle mediastinum along with elevated left hemidiaphragm
Figure 2.
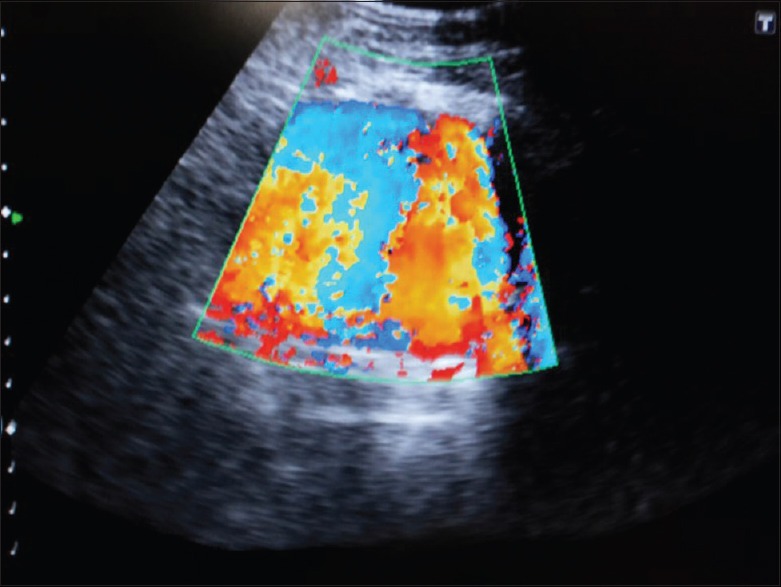
Colour Doppler sonography showing lesion was anechoic on gray scale sonography with mosaic pattern suggesting intense internal vascularity. Thus confirming the diagnosis of saccular aneurysm of descending thoracic aorta
Figure 3.
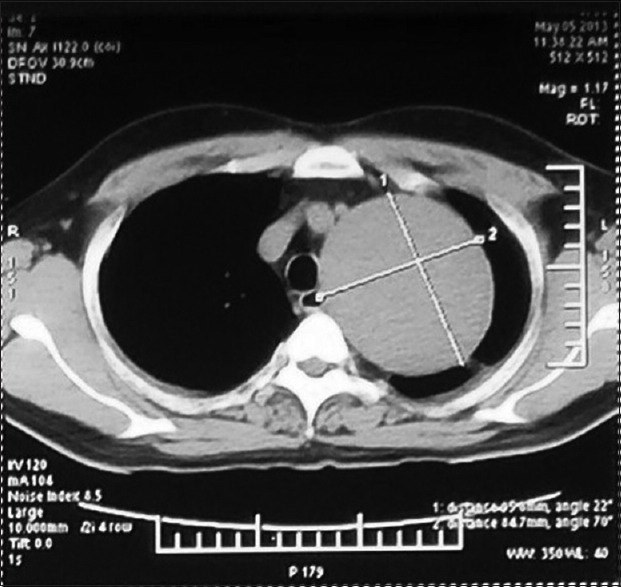
Contrast-enhanced computed tomography thorax shows smoothly rounded opacity with fluid density abutting mediastinum with no contrast enhancement
DISCUSSION
Most aortic aneurysm are asymptomatic and are found as a mediastinal mass during routine noninvasive exploration.[1,2] An aortic aneurysm is a permanent localized dilatation having diameter at least 1.5 times greater than the normal diameter of that portion of the aorta.[3] Based on its shape, the aortic aneurysm is classified as either saccular or fusiform. The most common cause of aneurysm is atherosclerosis. It is also associated with hypertension, smoking and advanced age, usually in the sixth and seventh decades of life. It can also occur due to weakening of the aortic wall associated with connective tissue disorders such as the Marfan and Ehler-Danlos syndromes. Inflammation of the aorta and injury from falls or motor vehicle accidents are other potential contributing factors. The symptoms and signs of a thoracic arteriosclerotic aneurysm depend on its location. Chest pain, due to compression or erosion of surrounding structures, is the most common symptom. Acute, sudden onset of severe pain in the back or abdomen may represent rupture and is a life-threatening medical emergency. Thoracic aortic aneurysm may present atypical symptoms such as dysphagia due to compression of the esophagus; hoarseness due to vocal cord paralysis or compression of the recurrent laryngeal nerve; superior vena cava syndrome due to compression of the superior vena cava; cough, dyspnea or both due to tracheal compression; hemoptysis due to rupture of the aneurysm into a bronchus; and shock due to rupture of the aneurysm. Thoracic or lumbar vertebral body erosion may cause back pain, spinal instability, and neurologic deficits from spinal cord compression; this is particularly the case with mycotic aneurysms. A large aneurysm of the descending thoracic aorta can compress the recurrent laryngeal nerve and cause hoarseness.[4]
Phrenic nerve palsy appear to be unusual manifestations of a thoracic aortic aneurysm. In a case reported by Rαbago et al., a patient with a descending thoracic aortic aneurysm presented left hemidiaphragmatic paralysis consistent with left phrenic nerve palsy.[4] Common causes of phrenic nerve palsy include malignancy such as bronchogenic carcinoma, as well as mediastinal and neck tumors. Phrenic nerve palsy can also occur due to a penetrating injury or due to iatrogenic causes arising, for example, during cardiac surgery and central venous catheterization. Many cases or phrenic nerve palsy are idiopathic.
Criteria of unilateral diaphragmatic paralysis[5] clinically unilateral diaphragmatic paralysis may be suspected but cannot be diagnosed with certainty. Physical signs, occasionally striking, are more often so insignificant as to be easily missed or overshadowed by coexisting processes, and when present are not usually diagnostic. The following criteria were therefore adopted in the cases described.[1] Elevation of the diaphragm 1.5 inch (about 4 cm.) or more above the normal position: The extent of the elevation was determined by comparison with the sound side. For purposes of measurement, the right dome was arbitrarily taken as being normally 1 inch (1.25 cm) higher than the left.[2] Paradoxical movement, especially noticeable on sniffing, the sound side descends on inspiration while the paralyzed side rises by a smaller amount. This phenomenon is rendered more obvious when the subject sniffs sharply. The latter test is a severe one, and may be positive with incompletely paralyzed diaphragms. A-positive response to the sniff test was not therefore taken by itself as the only criterion. Direct stimulation of the phrenic nerve with simultaneous radiographic control would have been crucial, but was scarcely practicable under circumstances of acute illness.
The phrenic nerves take a long course through the thorax and throughout that course they are situated immediately under the mediastinal pleura, where they are liable to damage by toxins present in the pleural cavity. There is also a possibility that, where the nerves pass in front of the respective lung hila, they would be exposed to toxins travelling in the bronchial lymphatics. The left recurrent laryngeal nerve fibers before they leave the vagus trunk are likewise situated subpleurally. Their shorter subpleural course corresponds to the lower incidence of paralysis (1 in 6). Unilateral diaphragmatic paralysis in itself causes very little disability. There would appear to be no practicable form of treatment for the one patient with apparently permanent paralysis, nor is it necessary, since he is not conscious of any disability.
Kienbock (1898) phenomenon is often associated elevation of diaphragm. Kienbock attributed the phenomenon to phrenic palsy. However, the term Kienbock phenomenon is often, but erroneously, used to describe the paradoxical movement of phrenic paralysis. Kienbock's description referred to the occurrence of this movement in the fluid level of hydropneumothorax.[6]
In diagnosing a case of phrenic palsy of recent onset, it is, therefore, desirable if possible to exclude eventration.[6]
In our case, there is aortic arch aneurysm with left hemidiaphragm elevation suggestive of left phrenic nerve palsy, due to the pressure effect of an aneurysm. Hoarseness of voice was also present in our patient, which are uncommon symptoms of thoracic aortic aneurysm. Hoarseness is due to the left recurrent laryngeal nerve palsy, caused by a specific cardiovascular pathology such as an aortic aneurysm, called cardio-vocal syndrome or Ortner's syndrome.
Surgical correction of thoracic aortic aneurysms is advised on the basis of its size or growth rate and symptoms. Elective repair of ascending aneurysms should be performed if the size is >5.5 cm, or >6.5 cm in the case of descending aneurysms, in the absence of any familial disorders.[7] Patients with aneurysms as well as a history of familial disorders such as Marfan syndrome should be surgically corrected earlier, particularly if the ascending aorta is more than 5.0 cm, or the descending aorta more than 6.0 cm. A rapid increase in size is also an indicator for surgical correction. An increase in size of 1 cm or more per year is an indication of the need for elective surgical repair.[8] Symptomatic patients should undergo surgical resection regardless of size because of the risk of rupture, as in our case. Acutely symptomatic patients require an emergent operation. The emergent operation is also indicated in cases of acute rupture.
Surgical correction can be done by open surgical repair in which an aneurysm is removed and replaced with a tube graft. A new modality for surgery is endovascular stent graft aneurysm repair.[5]
CONCLUSION
This case reports a rare involvement of left phrenic nerve palsy due to aortic arch aneurysm.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Earnest F, 4th, Muhm JR, Sheedy PF., 2nd Roentgenographic findings in thoracic aortic dissection. Mayo Clin Proc. 1979;54:43–50. [PubMed] [Google Scholar]
- 2.Harris RD, Usselman JA, Vint VC, Warmath MA. Computerized tomographic diagnosis of aneurysms of the thoracic aorta. Comput Tomogr. 1979;3:81–91. doi: 10.1016/0363-8235(79)90002-4. [DOI] [PubMed] [Google Scholar]
- 3.Lavall D, Schäfers HJ, Böhm M, Laufs U. Aneurysms of the ascending aorta. Dtsch Arztebl Int. 2012;109:227–33. doi: 10.3238/arztebl.2012.0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rábago G, Martín-Trenor A, López-Coronado JL. Chronic aneurysm of the descending thoracic aorta presenting with right pleural effusion and left phrenic paralysis. Tex Heart Inst J. 1999;26:96–8. [PMC free article] [PubMed] [Google Scholar]
- 5.Bavaria JE, Appoo JJ, Makaroun MS, Verter J, Yu ZF, Mitchell RS. Gore TAG Investigators. Endovascular stent grafting versus open surgical repair of descending thoracic aortic aneurysms in low-risk patients: A multicenter comparative trial. J Thorac Cardiovasc Surg. 2007;133:369–77. doi: 10.1016/j.jtcvs.2006.07.040. [DOI] [PubMed] [Google Scholar]
- 6.Freedman B. Unilateral paralysis of the diaphragm and larynx associated with inflammatory lung disease. Thorax. 1950;5:169–82. doi: 10.1136/thx.5.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davies RR, Gallo A, Coady MA, Tellides G, Botta DM, Burke B, et al. Novel measurement of relative aortic size predicts rupture of thoracic aortic aneurysms. Ann Thorac Surg. 2006;81:169–77. doi: 10.1016/j.athoracsur.2005.06.026. [DOI] [PubMed] [Google Scholar]
- 8.Elefteriades JA. Natural history of thoracic aortic aneurysms: Indications for surgery, and surgical versus nonsurgical risks. Ann Thorac Surg. 2002;74:S1877–80. doi: 10.1016/s0003-4975(02)04147-4. [DOI] [PubMed] [Google Scholar]


