Abstract
We describe a middle aged previoulsy healthy female patient who presented with clinical features suggestive of acute heart failure. Investigations revealed very high NT pro-BNP, right heart enlargement, bilateral pulmonary alveolar edema and bilateral pleural effusion. In view of falling platelet counts and exudative pleural effusion inflammatory/infective causes were considered. Her Weil Felix test was strongly positive and IgM for scrub typhus also returned positive. She was started on doxycycline to which there was dramatic improvement. Thus in this case scrub typhus infection presented as acute right heart failure and the cause seemed elusive at the outset. We also systematically reviewed the existing literature on cardio-pulmonary manifestations of scrub typhus infection.
KEY WORDS: Acute corpulmonale, acute heart failure, afebrile, scrub typhus
INTRODUCTION
Scrub typhus infection is a common febrile disorder presenting in the tropical region with propensity to involve different systems. Amongst them the cardio-respiratory system is involved in a significant proportion resulting in various manifestations. Herein we describe a case of scrub typhus presenting as acute right sided heart failure and also discuss the different aspects of cardio-pulmonary manifestations in this rickettsial infection.
CASE REPORT
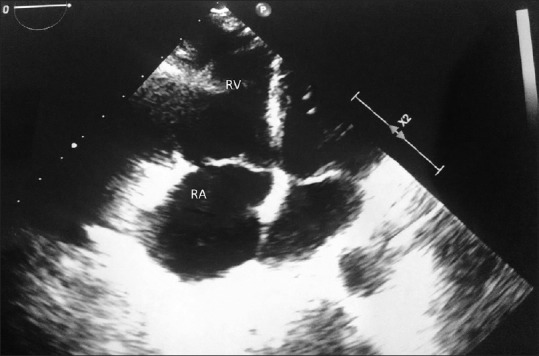
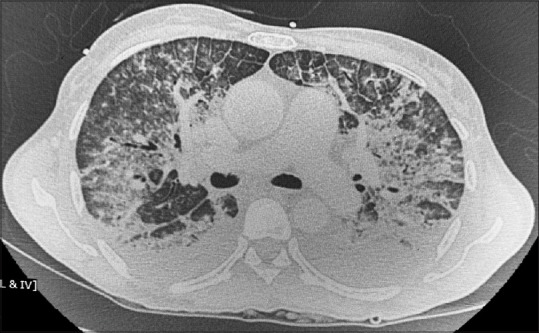
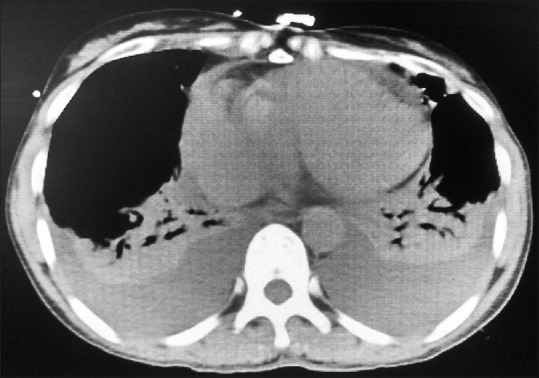
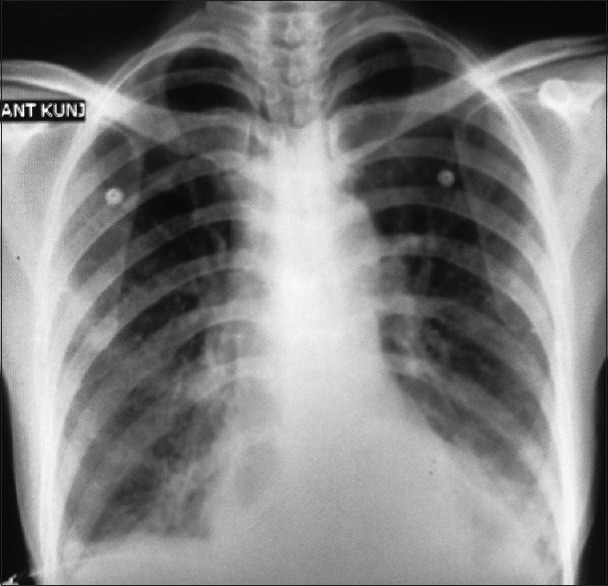
A 40-year-old female who was previously well-presented to us with complaints of shortness of breath and cough with scanty expectoration for the last 7 days. On examination, she had a heart rate of 132 beats/min, respiratory rate 44 breaths/min, blood pressure 114/82 mm of Hg, SpO2 of 80% (on room air). Systemic examination revealed raised jugular venous pressure (JVP), mild hepatomegaly, and coarse crepitations in bilateral lung bases. Chest X-ray revealed bilateral patchy nonhomogenous infiltrates in the mid and lower zones [Figure 1]. Routine investigations revealed mild leukocytosis and mild hyperbilirubinemia [Table 1]. NT-proBNP done in the emergency was >20,000 pg/ml with normal cardiac enzymes and without any significant electrocardiography (ECG) changes. Two-dimensional (2D) echocardiography showed normal left atrium/ventricle but enlarged right atrium/ventricle (RA/RV) with shifting of interventricular septum towards left and the presence of moderate pulmonary hypertension (RV systolic pressure = 43 + right atrial pressure) [Figure 2]. A provisional diagnosis of acute cor-pulmonale with pulmonary edema was made. Computed tomography (CT) pulmonary angiography was done which did not show any pulmonary embolism. Bilateral pleural effusion was seen along with interlobular septal thickening and ground glass opacities in both lung fields with sparing of periphery of lung fields [Figures 3 and 4]. Ultrasonography of abdomen showed mild ascites. Ventilation-perfusion scan done was also negative for thromboembolism.
Figure 1.
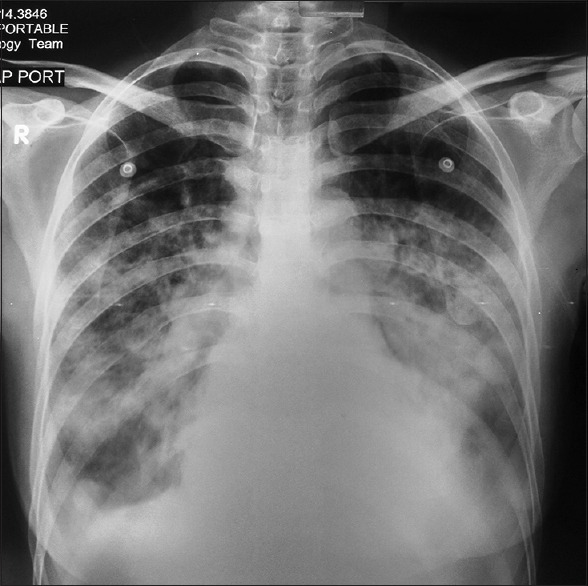
Chest X-ray of the patient at presentation
Table 1.
Investigations of the patient
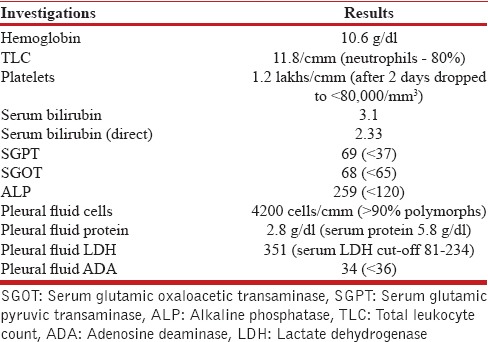
Figure 2.
Two-dimensional echocardiography (apical view) showing marked right atrial and ventricular enlargement
Figure 3.
Computed tomography thorax (mediastinal window) showing bilateral pleural effusion
Figure 4.
Computed tomography thorax (lung window) showing bilateral pulmonary alveolar edema
Initially, she was treated symptomatically with oxygen, noninvasive ventilation, fluid restriction and diuretics. However, her symptoms worsened, oxygen requirement increased along with a drop in platelets (80,000/mm3).
In view of multi-organ involvement and newly developing thrombocytopenia, other possible causes were looked into. Immunological workup (anti-nuclear antibody, anti-double-stranded deoxyribonucleic acid, anti-cyclic citrullinated peptide, and anti-neutrophil cytoplasmic antibody) were negative. Ultrasound guided pleural fluid aspiration was done which revealed exudative effusion [Table 1]. Dengue serology, malarial antigen, and procalcitonin was negative. Cultures from blood and urine were sterile. Weil-Felix test was positive and IgM antibody for scrub typhus was strongly positive (by ELISA).
She was started on doxycycline (100 mg twice a day). She responded to doxycycline and within 48 h her symptoms decreased significantly and her vitals steadily improved. Within another 48 h, her hemoglobin oxygen saturation improved to 95% (on room air) and tachypnea and tachycardia resolved and her NT-proBNP fell to <3000 pg/ml. Chest X-ray repeated after a week revealed significant improvement [Figure 5] and a repeat 2D echo after 2 weeks revealed resolution of RA/RV enlargement [Figure 6].
Figure 5.
Chest X-ray of the patient showing marked improvement after completion of therapy
Figure 6.

Two-dimensional echo of the patient (apical view) showing resolution of right heart enlargement after completion of therapy
DISCUSSION
This case presents several unique features. A patient having scrub typhus, presented with features of acute right heart failure (acute cor-pulmonale) and ARDS. ARDS has been rarely described in cases of scrub typhus but scrub typhus presenting as acute cor-pulmonale has not been described in literature to the best of our knowledge. The fact that the patient was afebrile was another uncommon feature in this case. As the patient was afebrile and did not have eschar mark or history of any insect bite the diagnosis of scrub typhus was not suspected initially and infective conditions were not investigated at the outset.
Scrub typhus is a Rickettsial disease caused by Orientia tsutsugamushi which commonly leads to the features of fever, rash, and eschar. In some cases, especially where early treatment is not instituted complications may arise such as meningitis, liver dysfunction, acute kidney injury, and disseminated intravascular coagulation which might lead to multi-organ dysfunction syndrome.[1] ARDS has been reported sparingly in cases of scrub typhus. Heart failure due to scrub typhus patients has been rarely reported[1,3] where myocarditis has been implicated in the causation of the same. Acute myocardial infarction due to scrub typhus has been reported.[4] In our case, the full-blown picture of heart failure was manifested by raised JVP, hepatomegaly, raised NT-proBNP, and right heart enlargement on echocardiography. However, the left ventricular ejection fraction was preserved. The pulmonary edema seen on chest X-ray appeared to be due to ARDS – the indirect evidence was provided by the exudative nature of the effusions. The occurrence of acute cor-pulmonale in this case was probably due to ARDS and associated severe pulmonary vaso-constriction induced increased pressure load on the right ventricle. Alternatively, the interventricular septum might have been pushed to the left with an increase in the RV pressure and corresponding compromise of the left ventricular output. However, this seems less likely as the pleural effusions in the latter scenario would be expected to be transudative. A right heart catheterization and pressure studies would have been conclusive but could not be done as the patient was severely hypoxemic and required continuous noninvasive ventilator support.
Thus, this case brings forward some important points. Scrub typhus in severe cases can lead to complications involving vital organs such as lungs and heart as was evident in this case. Sometimes the classical features of fever, rash, and eschar might all be missing as in our case. However scrub typhus presenting as ARDS without much fever has been documented by Ichimura et al.[18] Hence, having a high index of suspicion is important in cases of lung and/or heart involvement especially in endemic areas. In patients with multi-organ failure, the possibility of scrub typhus infection should be borne in mind and investigated if the cause is otherwise not apparent.
Systematic review of literature
A systematic review of literature was done to evaluate the nature of involvement of cardiorespiratory system in scrub typhus infection. Search was done in PubMed with the following questions with respect to cardiopulmonary involvement in scrub typhus.
Symptomatology
Chest X-ray and CT imaging features
Different type of diseases caused
Complications encountered.
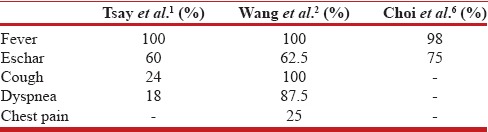
The common symptoms have been enumerated in Table 2. Fever was seen in 100% of patients in all the series. Eschar which is said to be pathognomic of scrub typhus were seen in 43.5–86.3% patients, cough in 13.7–38% patients and dyspea in 18–49% patients.
Table 2.
Frequencies of the common symptoms related to the cardio-pulmonary system
The X-ray features have been tabulated in Table 3. The incidence of X-ray abnormalities have been described by Qu[11] to be around 44% and 59.4% by Song et al.[9] among patients with scrub typhus. Interstitial pneumonia appears to be the most common radiological feature (ranging from 40% to 51.4%). On CT scan of thorax, the most common features were ground glass opacities and mediastinal lymphadenopathy (91% each) [Table 4] while interlobular septal thickening has been noticed in up to 82% patients. The complications related to the cardiopulmonary system have been enumerated in Tables 5 and 6. Septic shock has been described in 3-65.6% patients and ARDS in 11.1-33.7% patients.
Table 3.
Frequencies of Chest X-ray findings in scrub typhus infection
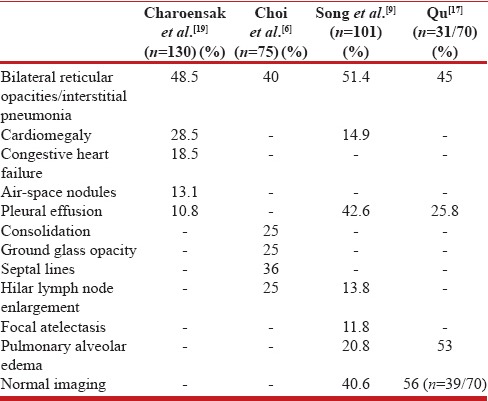
Table 4.
Frequencies of computed tomography thorax findings in scrub typhus infection
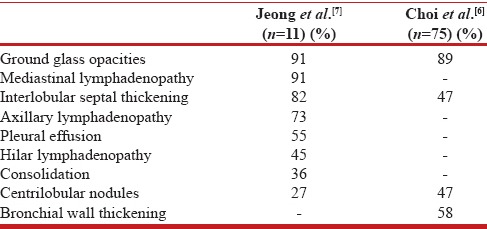
Table 5.
Frequencies of cardiac involvement in scrub typhus infection
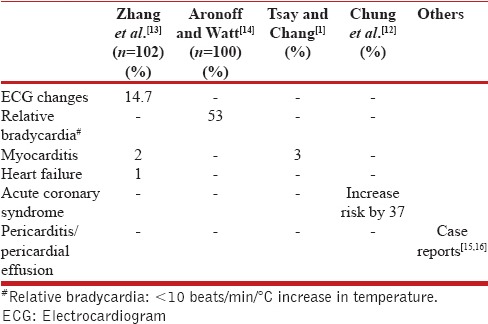
Table 6.
Frequencies of different cardiopulmonary complications in scrub typhus infection
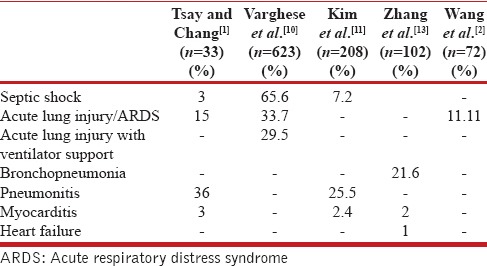
Wang et al.[2] has described the complication of ARDS in association with scrub typhus patients. 8 out of 72 (11.1%) patients studied were seen to develop ARDS and 25% of patients with ARDS succumbed. Initial presentations of dyspnea and cough, white blood cell count, hematocrit, total bilirubin, and delayed use of appropriate antibiotics were independent predictors of ARDS.
Settle et al.[5] in their series describing autopsy findings of scrub typhus patients concluded that interstial pneumonia is present in almost all patients with scrub typhus. On chest radiograph abnormalities are present in 59–72% patients.[6,7,8,9] Zhang et al. noted the involvement of respiratory system in around 25.5% of cases.[13] Reticulonodular infiltrates, hilar lymph node enlargement and septal lines are the most common findings while consolidation is relatively uncommon and generally appears in the lower zone of lungs.[6] Pleural effusion and unilateral/bilateral hilar enlargement are found in 12–43% and 25–27% patients respectively.
In more than 50% patients abnormal chest radiographs were observed in the 1st week and progressive changes were frequently observed also in the 1st week.[8]
Fifty-three percent of infected patients have been seen to have relative bradycardia as described by Aronoff and Watt.[14] Scrub typhus increases the risk of acute coronary syndrome by around 37%, and the prominent effect was seen within 1 year of infection.[12] ECG changes have been seen in 14.7% patients and the common changes describe 12 were T wave changes (33.3%), ST-T changes (26.7%), partial or complete bundle branch block (26.7%), sinus bradycardia (13.3%), ventricular extrasystoles (6.7%), and abnormal Q wave (6.7%).19
CONCLUSION
Cardiopulmonary involvement is not so uncommon in scrub typhus infections and needs to be duly considered when treating such patients.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Tsay RW, Chang FY. Serious complications in scrub typhus. J Microbiol Immunol Infect. 1998;31:240–4. [PubMed] [Google Scholar]
- 2.Wang CC, Liu SF, Liu JW, Chung YH, Su MC, Lin MC. Acute respiratory distress syndrome in scrub typhus. Am J Trop Med Hyg. 2007;76:1148–52. [PubMed] [Google Scholar]
- 3.Ganjoo RK, Sharma SN, Roy AK. Typhus myocarditis. J Assoc Physicians India. 1989;37:357. [PubMed] [Google Scholar]
- 4.Kim DG, Kim JW, Choi YS, Kim SH, Kim SM, Park CG, et al. Acute myocardial infarction following scrub typhus infection. Int J Cardiol. 2007;114:e18–20. doi: 10.1016/j.ijcard.2006.07.131. [DOI] [PubMed] [Google Scholar]
- 5.Settle EB, Pinkerton H, Corbett AJ. A pathologic study of tsutsugamushi disease (scrub typhus) with notes on clinicopathologic correlation. J Lab Clin Med. 1945;30:639–61. [Google Scholar]
- 6.Choi YH, Kim SJ, Lee JY, Pai HJ, Lee KY, Lee YS. Scrub typhus: Radiological and clinical findings. Clin Radiol. 2000;55:140–4. doi: 10.1053/crad.1999.0336. [DOI] [PubMed] [Google Scholar]
- 7.Jeong YJ, Kim S, Wook YD, Lee JW, Kim KI, Lee SH. Scrub typhus: Clinical, pathologic, and imaging findings. Radiographics. 2007;27:161–72. doi: 10.1148/rg.271065074. [DOI] [PubMed] [Google Scholar]
- 8.Chen HC, Chang HC, Chang YC, Liu SF, Su MC, Huang KT, et al. Chest radiographic presentation in patients with scrub typhus. Trans R Soc Trop Med Hyg. 2012;106:48–53. doi: 10.1016/j.trstmh.2011.09.005. [DOI] [PubMed] [Google Scholar]
- 9.Song SW, Kim KT, Ku YM, Park SH, Kim YS, Lee DG, et al. Clinical role of interstitial pneumonia in patients with scrub typhus: A possible marker of disease severity. J Korean Med Sci. 2004;19:668–73. doi: 10.3346/jkms.2004.19.5.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Varghese GM, Trowbridge P, Janardhanan J, Thomas K, Peter JV, Mathews P, et al. Clinical profile and improving mortality trend of scrub typhus in South India. Int J Infect Dis. 2014;23:39–43. doi: 10.1016/j.ijid.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 11.Kim DM, Kim SW, Choi SH, Yun NR. Clinical and laboratory findings associated with severe scrub typhus. BMC Infect Dis. 2010;10:108. doi: 10.1186/1471-2334-10-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chung WS, Lin CL, Hsu WH, Kao CH. Scrub typhus increases the risk of developing acute coronary syndrome: A nationwide cohort study. Heart. 2014;100:1844–50. doi: 10.1136/heartjnl-2014-306181. [DOI] [PubMed] [Google Scholar]
- 13.Zhang M, Zhao ZT, Wang XJ, Li Z, Ding L, Ding SJ. Scrub typhus: Surveillance, clinical profile and diagnostic issues in Shandong, China. Am J Trop Med Hyg. 2012;87:1099–104. doi: 10.4269/ajtmh.2012.12-0306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aronoff DM, Watt G. Prevalence of relative bradycardia in Orientia tsutsugamushi infection. Am J Trop Med Hyg. 2003;68:477–9. [PubMed] [Google Scholar]
- 15.Chang JH, Ju MS, Chang JE, Park YS, Han WS, Kim IS, et al. Pericarditis due to Tsutsugamushi disease. Scand J Infect Dis. 2000;32:101–2. doi: 10.1080/00365540050164344. [DOI] [PubMed] [Google Scholar]
- 16.Bosch T, Hacker H, Höfling B, Löscher T. Fever, pericardial and pleural effusion in a 27-year-old patient following a stay in Thailand. Internist (Berl) 1990;31:291–4. [PubMed] [Google Scholar]
- 17.Qu Y. A clinical analysis of 31 cases with pulmonary damage caused by scrub typhus. Zhonghua Jie He He Hu Xi Za Zhi. 2000;23:98–100. [PubMed] [Google Scholar]
- 18.Ichimura K, Uchida Y, Arai K, Nakazawa K, Sasaki J, Kobayashi K, et al. Afebrile scrub typhus (Tsutsugamushi disease) with acute respiratory distress syndrome. Intern Med. 2002;41:667–70. doi: 10.2169/internalmedicine.41.667. [DOI] [PubMed] [Google Scholar]
- 19.Charoensak A, Chawalparit O, Suttinont C, Niwattayakul K, Losuwanaluk K, Silpasakorn S, et al. Scrub typhus: Chest radiographic and clinical findings in 130 Thai patients. J Med Assoc Thai. 2006;89:600–7. [PubMed] [Google Scholar]


