Sir,
A 46-year-old male presented with cough of one and half months duration and fever of 3-weeks duration. Cough was productive with mucoid expectoration. There was no diurnal variation. Fever was of low grade and not associated with chills or rigors. There was one episode of hemoptysis of 15 ml. He also complained of pain abdomen and burning micturition.
On examination he was a moderately built male. Chest examination revealed diminished breath sounds in the basal areas with monophonic wheeze more on left side. There was guarding, tenderness and fullness in the left loin. His hematological investigations revealed neutrophilic leucocytosis. His routine biochemical parameters were normal. He was HIV, HBsAg and HCV non-reactive. Urine culture was negative. Gram stain of bronchial wash revealed Gram-positive cocci.
CT chest revealed a homogenously enhancing mass in the left hilum extending into middle lobe bronchus. Bronchoscopy revealed an endobronchial mass lesion occluding the entire lower lobe bronchus [Figure 1]. Bronchial biopsy showed mild chronic inflammation. CT abdomen revealed a well-defined lobulated mass lesion in the left kidney in the upper pole [Figure 1].
Figure 1.
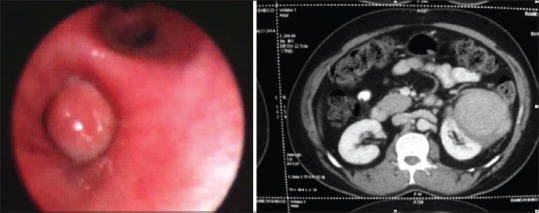
Bronchoscopic picture showing endobronchial mass. CT abdomen showing left renal mass
With a provisional diagnosis of a renal mass with probable lung metastasis, patient underwent left radical nephrectomy and left lower lobectomy. He had an uneventful per operative and post-operative course.
Macroscopic findings
Radical nephrectomy specimen measured 13 × 8 × 8 cms. Upper pole of the kidney showed a lobulated mass measured 10 × 8 cms. External surface revealed grey white nodular areas. Cut section revealed a yellowish firm mass [Figure 2b].
Figure 2.
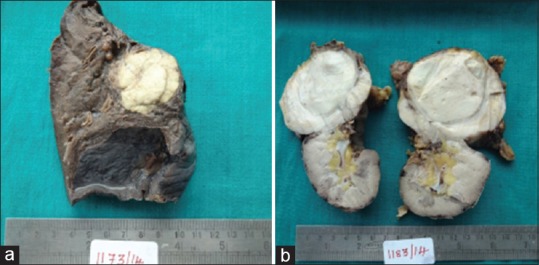
Specimen photographs of lung (a) and kidney (b) showing grey white lesions with yellowish areas
Lobectomy specimen measured 12 × 7 × 6 cms. A nodular mass seen close to the bronchus measured 4.5 cms. Cut surface of the mass was yellowish white [Figure 2a] and firm in consistency.
Microscopic findings
Multiple sections are studied from the specimen, sections revealed renal tissue with an inflammatory lesion. This is composed of an admixture of lymphocytes, plasma cells and few neutrophils. Sheets of foam cells and focal multinucleate giant cell reaction were seen [Figure 3a]. Stains for AFB and fungus were negative. Foam cells were CD68 positive [Figure 3b] and EMA and cytokeratin negative.
Figure 3.
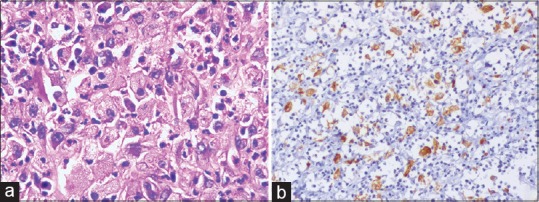
(a) Section of kidney lesion shows lymphocytes and plasma cells (H and E x200) (b) Foam cells showing CD68 positivity (x200)
Sections from the lung lesion revealed chronic inflammatory cells, foam cells and granulomas, Features similar to that seen in the kidney. A diagnosis of XGPN with extension beyond the renal capsule and septic lung metastasis was made.
Six months after the surgery, patient was readmitted with complaints of backache of 2-months duration associated with malaise. Ultrasonography revealed a mass in the left renal fossa. Mass was excised. He recovered completely and was discharged.
Histological examination of the mass revealed Xanthogranulomatous inflammation.
The present case had stage-3 XPGN with septic metastasis to lung, treated with lobectomy and nephrectomy. Patient developed recurrence in left renal fossa which was excised. He is on regular follow-up and was symptom free during the last visit.
Xanthogranulomatous pyelonephritis is an uncommon severe chronic inflammatory disorder of the kidney associated with the indolent bacterial infection. XGPN was first described in 1916 by Schlagenhaufer and the term was suggested by Osterline in 1935.[1] It is characterized by destruction of renal parenchyma and replacement by chronic inflammatory cells, lipid laden macrophages. Exact etiology is not known. It is associated with chronic urinary tract infection, urinary tract obstruction and nephrolithiasis. It is common in immunosuppressed patients and other risk factors are diabetes and hyperlipidemia. This is an uncommon infection with an incidence of 1% of renal infections.[2] It can occur in any age group from 11 months to 89 years. Women are affected more than men in a ratio of 2:1 and rarely bilateral. Schlagenhaufer described it as Staphylomycosis due to the presence of staphylococci. Various organisms are implicated in the pathogenesis like Escherichia coli, Proteus mirabilis, Klebsiella, Enterococcus, Pseudomonas and Streptococcus.
XGPN can be localized, focal or segmental in 15% of cases, diffuse or global in 85% of cases. Diffuse XGPN can be staged as stage-1 when involvement is limited to kidney, stage-2 lesion extends to renal pelvis or peri-renal fat and stage-3 extension into retroperitoneum.[3] This disease is called a great imitator as it is difficult to differentiate clinically and radiologically from other lesions especially renal cell carcinoma.
Fistulisation is a rare complication.[4] Nephro-bronchial, nephro-cutaneous, colonic, gastric and jejunal fistulas are described. Fistulas can also occur to psoas muscle, flank and gluteal region. It can spread to lungs and form lung abscess. The case under discussion is XGPN with septic spread to lung. The tendency of peri-renal inflammation spreading superiorly was described by Evans et al.[5] The lumbocostal triangle is a relatively weak area of diaphragm and can transmit infection into thoracic cavity.
CONCLUSIONS
Xanthogranulomatous pyelonephritis is a rare chronic infection. Local infiltration and spread to other organs is rare. It is common in patients with recurrent urinary tract infection, diabetics and nephrolithiasis. This case is XGPN in a diabetic with peri-renal infiltration and extension to lungs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ramos LD, Lima Mde M, Carvalho Md, Silva Junior GB, Daver Ede F. Emphysematous and xanthogranulomatous pyelonephritis: Rare diagnosis. Braz J Infect Dis. 2010;14:374–6. [PubMed] [Google Scholar]
- 2.Eastham J, Ahlering T, Skinner E. Xanthogranulomatous pyelonephritis: Clinical findings and surgical considerations. Urology. 1994;43:295–9. doi: 10.1016/0090-4295(94)90069-8. [DOI] [PubMed] [Google Scholar]
- 3.Hendrickson RJ, Lutfiyya WL, Karrer FM, Furness PD, 3rd, Mengshol S, Bensard DD. Xanthogranulomatous pyelonephritis. J Pediatr Surg. 2006;41:e15–7. doi: 10.1016/j.jpedsurg.2005.11.030. [DOI] [PubMed] [Google Scholar]
- 4.Parsons MA, Harris SC, Grainger RG, Ross B, Smith JA, Williams JL. Fistula and sinus formation in xanthogranulomatous pyelonephritis. A clinicopathological review and report of four cases. Br J Urol. 1986;58:488–93. doi: 10.1111/j.1464-410x.1986.tb05452.x. [DOI] [PubMed] [Google Scholar]
- 5.Evans JA, Meyers MA, Bosniak MA. Acute renal and perirenal infections. Semin Roentgenol. 1971;6:276–91. doi: 10.1016/0037-198x(71)90039-3. [DOI] [PubMed] [Google Scholar]


