Sir,
We read with great pleasure the recent article by Aagre et al. published in your esteemed journal. We would like to share a similar experience from our institute.[1]
A 65-year-old female presented to ENT surgeon for the symptoms of difficulty in eating for the 3 months. She noticed dysphagia for solid food more than the liquid items. There was no history of fever, loss of weight or appetite. There was no lump sensation anywhere else in the body. Oral examination showed a mass of approximately 3 cm × 3 cm size hanging from the hard palate. On palpation, the mass was firm to feel, nontender, and nonfriable. Magnetic resonance imaging of head and neck was done which showed mass to be limited to the hard palate without erosion of adjacent bone [Figure 1a–c]. Core biopsy confirmed the diagnosis of diffuse large B-cell lymphoma stage IAE and she was started on RCHOP-21 regimen. She completed three cycles uneventfully. Seventh-day onward following the fourth RCHOP, patient started developing breathlessness. On auscultation, there were bilateral coarse crackles throughout the lung fields. There was no history of fever or worsening pallor. Hemogram showed normal counts and Hb levels. High-resolution computed tomography (HRCT) of the chest showed interstitial infiltrates with patchy ground glass opacities involving the whole lung field bilaterally [Figures 2a, 3a and 3b]. Sputum examination and BAL fluid cultures were negative for tuberculosis, fungi, and pneumocystis. Other more common causes of interstitial lung disease (ILD) such as eosinophilic pneumonia, hypersensitive pneumonitis etc were ruled out. Considering the diagnosis of rituximab induced-ILD (RI-ILD), she was started on oral wysolone 1 mg/kg. She showed dramatic improvement with resolution of symptoms within 2 weeks of starting steroids. Subsequently, slow tappering of steroids by 0.25mg/kg was done every fortnightly to which patient tolerated well without any recurrence of breathlessness. Repeat HRCT chest was done which showed drastic improvement in lung findings [Figures 2b, 3c and d]. Follow-up positron emission tomography-CT showed complete resolution of hard palate swelling. In view of rituximab induced fatal lung complication and malignancy being in complete remission, it was decided by treating team not to give further chemotherapy and to keep her under regular follow up.
Figure 1.
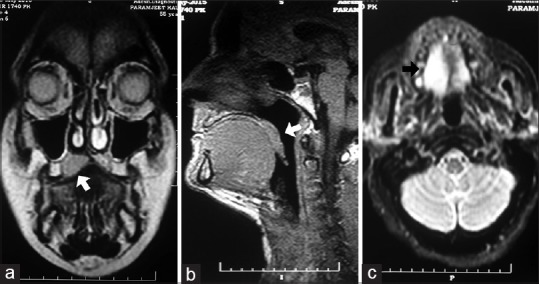
Magnetic resonance imaging head and neck (T1 sequence) showing mild widening and signal alterations in hard palate appearing mildy hypointense to isointense (white arrow) in (a) coronal section (b) sagittal section. (c) Magnetic resonance imaging head and neck T2 sequence showing hyperintense signal in right side of hard palate (black arrow) in axial view
Figure 2.
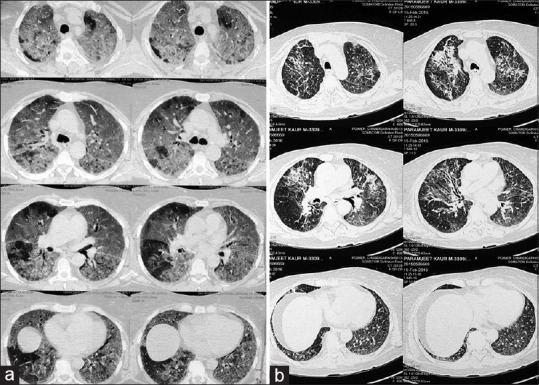
(a) Baseline high-resolution computed tomography cuts showing showed interstitial infiltrates with bilateral patchy ground glass opacities involving the whole lung field bilaterally. (b) Follow-up images showing dramatic resolution of lung shadows after steroid therapy
Figure 3.
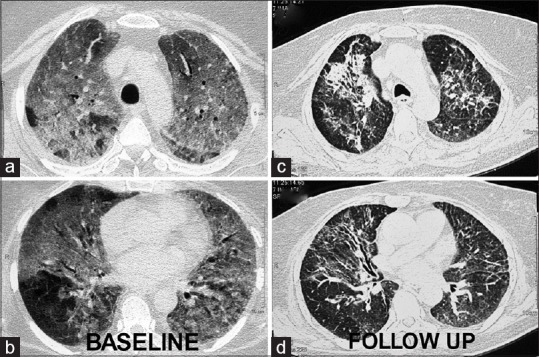
Comparative images in high-resolution showing (a and b) extensive interstitial involvement at baseline. (c and d) With resolution of opacities at follow-up
As mentioned by Aagre et al., incidence of RI-ILD is extremely rare with high frequency in an elderly male.[1] Although exact pathophysiology is not known till now, few authors have suggested a role of dysregulation of cellular cytotoxicity and NLRP3-related lung injury.[2] Maximum incidence of ILD is commonly noted after a cumulative dose of 1500 mg which usually peaks after the fourth cycle. There is no gold standard imaging or invasive investigation of choice for accurate diagnosis. It is rare and hence should only be considered after ruling out the more common infective causes of ILD. Considering the potential fatality, a lower threshold of suspicion with prompt diagnosis and treatment can be rewarding in most cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Aagre S, Patel A, Kendre P, Anand A. Rituximab-induced interstitial lung disease in a patient with follicular lymphoma: A rare case report. Lung India. 2015;32:620–3. doi: 10.4103/0970-2113.168135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Naqibullah M, Shaker SB, Bach KS, Bendstrup E. Rituximab-induced interstitial lung disease: Five case reports. Eur Clin Respir J. 2015;21:2. doi: 10.3402/ecrj.v2.27178. [DOI] [PMC free article] [PubMed] [Google Scholar]


