Abstract
Open reduction internal fixation of proximal humerus fractures is often accomplished with proximal humerus locking plates. While these plates have a good track record, they can become symptomatic and require removal once the fracture has healed. Open hardware removal is associated with a number of additional risks to the patient, including infection, scarring, nerve damage, and blood loss. In addition, the recovery time after open hardware removal may be prolonged, thereby predisposing the patient to postoperative stiffness. The purpose of this article is to describe a technique for removing proximal humerus locking plates arthroscopically. Although technically demanding, the benefits of this technique include smaller incisions, quicker recovery time, decreased risk of infection, and reduced blood loss. Arthroscopy also provides the surgeon with the ability to address concomitant intra-articular pathology at the time of surgery. Additionally, we use a bone-void filler to reduce the risk of fracture through stress caused by previous screw holes.
Proximal humerus fractures are the third most commonly encountered fracture in patients over the age of 65, and the annual incidence is increasing at rates as high as 15% per year.1 Although a number of treatment options exist, proximal humeral locking plates remain the predominant surgical treatment used. Despite the significant advances that have been made in plate osteosynthesis of proximal humerus fractures, the complication rate remains high. In fact, up to 25% of patients require revision surgery, most of which is related to persistent pain and dysfunction secondary to symptomatic hardware.2 Prior work has demonstrated improvement in patient outcomes after removal of symptomatic plates and screws through an open approach; however, revision surgery is certainly not without risks.2, 3 Known risks of open revision surgery include but are not limited to infection, stiffness, scarring, neurovascular injury, refracture, and blood loss.3, 4, 5, 6, 7
In an attempt to minimize these risks in patients with symptomatic hardware after locking plate fixation of proximal humerus fractures, a few reports of arthroscopic hardware removal have been published.4, 5, 7 These studies have demonstrated the feasibility of these techniques and improved patient symptoms postoperatively. Potential benefits of arthroscopic plate removal include decreased soft-tissue dissection, decreased stiffness, reduced bleeding, less pain, and quicker recovery than with open surgery. Additionally, arthroscopy allows full visualization of the glenohumeral joint for treatment if indicated and the axillary nerve for protection during the procedure. The purpose of this work is to describe an efficient, safe, and reliable technique for arthroscopic proximal humerus plate and screw removal with bone-void filler. The procedure is described in detail here and in the accompanying video (Video 1, Tables 1 and 2).
Table 1.
Key Points
| • Good preoperative radiographs are necessary to ensure that the appropriate number of screws are removed from the plate. |
| • Precise portal placement is critical in terms of minimizing the number of portals necessary to remove all screws. |
| • Several screws may be removed from a single portal by abducting and adducting the arm to achieve the appropriate axis on the driver-screw complex. |
| • Intraoperative fluoroscopy should be used as needed to aid in portal localization and to confirm screw and plate removal. |
| • Meticulous care must be taken around the motor branch of the axillary nerve and the posterior humeral circumflex artery with a low threshold to convert to an open procedure should visualization of these neurovascular structures be limited. |
Table 2.
Equipment Required
| • Trimano arm holder (Arthrex, Naples, FL, U.S.A.) |
| • PassPort cannulas (Arthrex) |
| • ArthroCare wand (ArthroCare Corporation, Austin, TX, U.S.A.) |
| • Standard screw removal set |
| • QuickSet Injectable Macroporous Calcium Phosphate (Arthrex) |
Surgical Technique
After administration of regional anesthesia, the patient is placed in the beach chair position with all bony prominences well padded. An examination under anesthesia of bilateral shoulders is performed with emphasis on range of motion of the glenohumeral joint. The operative extremity is then prepped and draped in standard fashion. A Trimano arm holder (Arthrex, Naples, FL) is used to facilitate intraoperative shoulder positioning.
Diagnostic arthroscopy is performed through a standard portal posterior to the glenohumeral joint (Fig 1). If intra-articular work, such as loose body removal or capsular release, is indicated, an anterior portal through the rotator interval is established using a spinal needle for localization. If no intra-articular work is indicated, the anterior portal may be avoided, thus decreasing the risk of postoperative scarring in the rotator interval.
Fig 1.
With the patient in the beach chair position, key anatomical landmarks are identified and drawn. Care should be taken to identify the transverse path of the axillary nerve approximately 5 to 7 cm from the lateral border of the acromion. The camera is placed in the standard posterior portal, and a diagnostic arthroscopy is performed.
The arthroscope is then repositioned into the subacromial space through the posterior portal. A lateral portal is established under needle localization; this portal can be maintained with a PassPort cannula (Arthrex). Scar tissue between the plate and the undersurface of the deltoid is removed with an ArthroCare wand (ArthroCare Corporation, Austin, TX), thereby exposing the proximal (or paddle) portion of the plate and the sutures through the rotator cuff (Fig 2A). A meniscal biter or grasper is used to remove the sutures, using care to protect the rotator cuff.
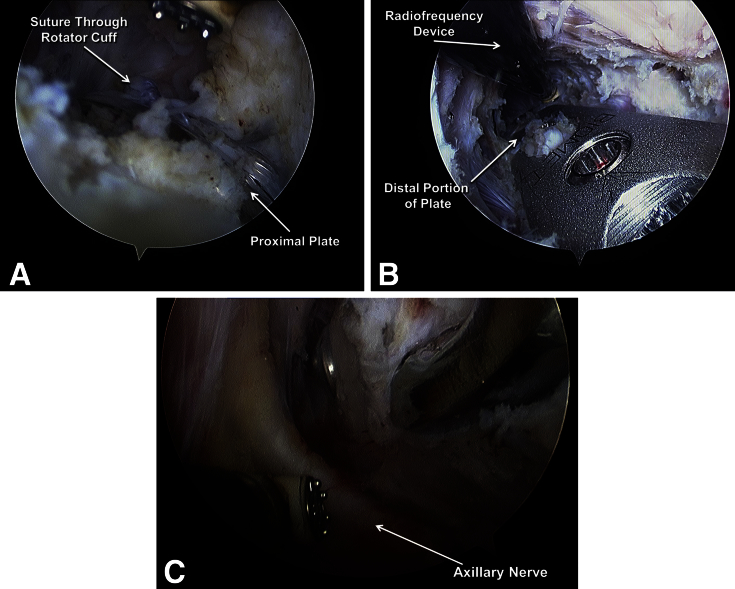
Fig 2.
(A) When viewing from a posterior portal, a radiofrequency device is used to expose the proximal portion of the locking plate. Here a suture that was used for rotator cuff repair is easily identified. (B) Dissection is carried out along the length of the plate using the radiofrequency device until the plate and all screws are fully visualized. (C) Care is taken to identify, protect, and preserve the axillary nerve and posterior circumflex humeral artery along the undersurface of the deltoid.
The plane between the plate and the deltotrapezial fascia is then further developed distally with a radiofrequency device (Fig 2B). Care is taken to stay medial to the motor branch of the axillary nerve and the posterior humeral circumflex artery (Fig 2C). These structures typically cross ∼6.5 cm distal to the lateral aspect of the acromion.8 Intraoperative fluoroscopy should also be used as a guide, as the axillary nerve typically crosses the first hole just distal to the paddle portion of the plate. A radiofrequency device is preferred over a shaver as it provides feedback as the dissection proceeds closer to the nerve.
A single distal lateral portal is then established for removal of the screws in the shaft of the plate. This portal is typically made at the distal-most aspect of the previous anterolateral incision, but the precise location of the portal can be determined with fluoroscopic guidance and needle localization. The distal screws are then removed arthroscopically through the distal lateral portal (Fig 3A). A hand screwdriver is first used to initiate screw removal from the plate; a power screwdriver may then be used to complete the extraction. Use of a PassPort cannula (Arthrex) in the distal lateral portal prevents dissociation of the screw and the driver as the screws are extracted through the deltoid. Abduction and adduction of the arm help to ensure that the driver approaches the screw at the correct angle. A radiofrequency device is then used to dissect the distal edge of the plate free from scar tissue.
Fig 3.
(A) When viewing the distal part of the plate from the posterior portal, the distal-most screws are removed arthroscopically through a PassPort cannula (Arthrex) so that they are not lost in the soft tissues. (B) Once all screws are removed, the bone-void filler (QuickSet Injectable Macroporous Calcium Phosphate; Arthrex) is arthroscopically injected through the PassPort cannula. (C) The proximal screws may be easier to inject in an open fashion through the same small incision that will be used to remove the plate. The plate is left in place during injection of the bone-void filler as this facilitates identifying all screw holes. Once all holes have been filled, the plate is removed.
After removal of the distal screws, attention is turned proximally to the multiple locking screws in the paddle portion of the plate. These screws may be removed arthroscopically, using the proximal lateral portal with the arm in abduction. The lateral portal is then extended, allowing open removal of any screws that were difficult to remove arthroscopically, as well as any remaining sutures in the rotator cuff. Fluoroscopy is used to confirm extraction of all screws. Prior to plate removal, the empty screw holes are filled with QuickSet Injectable Macroporous Calcium Phosphate (Arthrex), which acts as a bone-void filler (Fig 3 B and C). Finally, the plate is gently elevated from the bone and extracted through the extended lateral portal. The incisions are thoroughly irrigated and closed in standard layered fashion.
Postoperatively, the patient is placed in a sling and is restricted from weight bearing for 6 weeks. Range of motion exercises are initiated immediately to prevent postoperative stiffness. Patients typically return to full activity at 12 weeks after surgery.
Discussion
Symptomatic hardware is a complication after open reduction internal fixation of proximal humerus fractures with locking plates. Removal of the plate and screws through an open incision poses an increased risk of infection, stiffness, scarring, neurovascular injury, and blood loss.3, 4, 5, 6, 7
The described arthroscopic technique for removal of proximal humerus locking plates offers numerous potential benefits relative to open surgery. The significantly reduced soft-tissue dissection leads to decreased postoperative stiffness and pain and quicker recovery from surgery. Furthermore, the risks of infection and blood loss are diminished with arthroscopic surgery. An arthroscopic technique additionally affords full visualization of the glenohumeral joint, thereby allowing concomitant treatment of intra-articular pathology, such as loose bodies or a tight capsule. Since the axillary nerve is well visualized in this technique, the procedure can be performed safely with minimal risk to the nerve. By filling the screw holes with bone-void filler (Quickset), we theoretically decrease the risk of postoperative fracture. This technique has been successfully performed by the senior author (J.S.D.) on 94 patients with no reports of postoperative axillary nerve palsy or refracture.
In conclusion, our technique for arthroscopic removal of proximal humerus locking plates is an efficient, safe, and reliable method for treating symptomatic hardware and any concomitant intra-articular pathology status after locking plate fixation of proximal humerus fractures.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
Cadaveric demonstration of arthroscopic removal of proximal humerus locking plate. The specimen is a right shoulder positioned in the beach chair position. The technique can be performed with small incisions, minimal blood loss, and excellent visualization. It also permits concomitant treatment of intra-articular pathology. Initially, an intra-articular diagnostic arthroscopy of the glenohumeral joint is performed. Once completed, the camera is moved to the subacromical position. Debridement of the subacromical space and hardware is performed as needed. Once fully visualized, screws are removed under either direct or arthroscopic visualization. Finally, all screw holes are filled with a bone-void filler, and the plate is removed.
References
- 1.Roux A., Decroocq L., El Batti S. Epidemiology of proximal humerus fractures managed in a trauma center. Orthop Traumatol Surg Res. 2012;98:715–719. doi: 10.1016/j.otsr.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 2.Jost B., Spross C., Grehn H., Gerber C. Locking plate fixation of fractures of the proximal humerus: Analysis of complications, revision strategies and outcome. J Shoulder Elb Surg. 2013;22:542–549. doi: 10.1016/j.jse.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 3.Kirchhoff C., Braunstein V., Kirchhoff S. Outcome analysis following removal of locking plate fixation of the proximal humerus. BMC Musculoskelet Disord. 2008;9:138. doi: 10.1186/1471-2474-9-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maqdes A., Levy B., Klouche S., Hardy P. The feasibility and results of an arthroscopic removal of humeral locking plates and glenohumeral arthrolysis after proximal humeral fractures. Knee Surg Sport Traumatol Arthrosc. 2014;22:456–461. doi: 10.1007/s00167-013-2437-8. [DOI] [PubMed] [Google Scholar]
- 5.Voigt C., Geisler A., Lill H. Arthroscopic locking plate removal after proximal humeral fractures. Arch Orthop Trauma Surg. 2010;130:391–395. doi: 10.1007/s00402-009-0882-0. [DOI] [PubMed] [Google Scholar]
- 6.Katthagen J.C., Hennecke D., Jensen G., Ellwein A., Voigt C., Lill H. Arthroscopy after locked plating of proximal humeral fractures: Implant removal, capsular release, and intra-articular findings. Arthrosc J Arthrosc Relat Surg. 2014;30:1061–1067. doi: 10.1016/j.arthro.2014.04.092. [DOI] [PubMed] [Google Scholar]
- 7.Dines J.S., Hettrich C.M., Kelly B.T., Savoie F.H., Lorich D.G. Arthroscopic removal of proximal humerus locking plates. Knee Surg Sport Traumatol Arthrosc. 2010;18:409–411. doi: 10.1007/s00167-009-0991-x. [DOI] [PubMed] [Google Scholar]
- 8.Gardner M.J., Griffith M.H., Dines J.S., Briggs S.M., Weiland A.J., Lorich D.G. The extended anterolateral acromial approach allows minimally invasive access to the proximal humerus. Clin Orthop Relat Res. 2005;434:123–129. doi: 10.1097/01.blo.0000152872.95806.09. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Cadaveric demonstration of arthroscopic removal of proximal humerus locking plate. The specimen is a right shoulder positioned in the beach chair position. The technique can be performed with small incisions, minimal blood loss, and excellent visualization. It also permits concomitant treatment of intra-articular pathology. Initially, an intra-articular diagnostic arthroscopy of the glenohumeral joint is performed. Once completed, the camera is moved to the subacromical position. Debridement of the subacromical space and hardware is performed as needed. Once fully visualized, screws are removed under either direct or arthroscopic visualization. Finally, all screw holes are filled with a bone-void filler, and the plate is removed.