Abstract
Racial and ethnic disparities have been previously reported in acute stroke care. We sought to determine the effect of telemedicine (TM) on access to acute stroke care for racial and ethnic minorities in the state of Texas. Data were collected from the US Census Bureau, The Joint Commission and the American Hospital Association. Access for racial and ethnic minorities was determined by summing the population that could reach a primary stroke centre (PSC) or telemedicine spoke within specified time intervals using validated models. TM extended access to stroke expertise by 1.5 million residents. The odds of providing 60-minute access via TM were similar in Blacks and Whites (prevalence odds ratios (POR) 1.000, 95% CI 1.000–1.000), even after adjustment for urbanization (POR 1.000, 95% CI 1.000–1.001). The odds of providing access via TM were also similar for Hispanics and non-Hispanics (POR 1.000, 95% CI 1.000–1.000), even after adjustment for urbanization (POR 1.000, 95% CI 1.000–1.000). We found that telemedicine increased access to acute stroke care for 1.5 million Texans. While racial and ethnic disparities exist in other components of stroke care, we did not find evidence of disparities in access to the acute stroke expertise afforded by telemedicine.
Keywords: Teleneurology, tele-stroke, healthcare access, racial minorities, ethnic minorities, telemedicine
Introduction
Stroke is the fourth leading cause of death in the United States.1 Currently, tissue plasminogen activator (tPA) is the only approved medical therapy for acute ischaemic stroke (AIS) patients.2 Although some patients may be eligible to receive this therapy up to 4.5 hours from symptom onset,3 tPA utilization remains below 10%.4,5 Barriers to tPA usage may include limited access to acute stroke resources (neurological expertise, primary stroke centres), drug label contraindications and provider reluctance.6–8 Patients evaluated at primary stroke centres (PSCs) are more likely to receive tPA and have better outcomes, yet many patients in the country do not have access to these hospitals in a time window in which thrombolysis is recommended.9–11 It is estimated that only 55–66% of Americans have 60-minute ground access to a Joint Commission Primary Stroke Centre.12,13,14
Telemedicine (TM) has been proposed as a mechanism to improve access to acute stroke care. Originally developed in the 1990s, TM for stroke uses video teleconferencing to remotely examine a patient and facilitate treatment decisions.15 Hospital emergency departments without on-call neurological expertise are often equipped with mobile devices that include remote control cameras and display monitors, allowing a neurologist to remotely interact with the patient and their family members.16 TM for acute ischaemic stroke has been demonstrated to be safe and effective17,18 and increases both tPA utilization and accuracy of treatment decisions.19,20
In the United States, racial and ethnic minorities have a higher burden of cerebrovascular disease than non-minorities.21 The age adjusted incidence and prevalence of ischaemic stroke is substantially higher in non-Hispanic Black Americans compared to White Americans.22,23 Hispanic Americans, the fastest growing minority group in the United States, also have a higher burden of stroke morbidity when compared to Whites.22,23 Although the incidence of ischaemic stroke appears to be declining in Whites, the incidence has remained the same among Blacks.24
In addition to increased morbidity in racial and ethnic minorities, there is some evidence to suggest that disparities exist in access to acute stroke care.25,26 Reasons for these disparities are complex and are not isolated to one link in the stroke chain of survival.27 In addition to reduced or delayed activation of emergency medical services,28 previous studies have shown that once minority patients arrive at the hospital, they face longer wait times until initial evaluation and neurologic consultation.29,30 As a consequence of this, fewer racial and ethnic minorities receive tPA.31
As PSCs expand and comprehensive stroke centres (CSCs) develop, TM is likely to play a critical role in expanding these systems of care to smaller, outlying hospitals. In addition to improving access to centres with neurological expertise, TM has the potential to narrow the racial and ethnic disparities gap in access to acute stroke care. The aim of this study was to determine if there were racial or ethnic differences in access to acute stroke care in systems with and without telemedicine. This study focuses on the state of Texas, which can serve as a model for determining if other regional differences exist.
Methods
Data sources
We obtained 2010 population data from the US Census Bureau and the Neilson Claritas Demographic Estimation Program.32 Block groups, defined by the US Census Bureau as 600 to 3000 adults and not crossing county lines, were used as the primary geographic unit of analysis. A point (centroid) closest to the home address of most residents was assigned within each block group and used for point to point access calculations. The racial and ethnic composition of each block group was determined. For the purpose of this study, the population was divided into three racial groups: Caucasian/White, African American/Black, and other. Ethnicity was divided into Hispanic and non-Hispanic. Urbanization was defined according to a modification of the rural–urban continuum classification (mRUC) scheme.33–36
The details of the survey methodology have been previously described in a related study examining the impact of telemedicine for the entire population of Texas and resource allocation.37 Briefly, hospitals in Texas were identified from the American Hospital Association (AHA).38 Acute care facilities were defined as hospitals with emergency departments which manage adult patients. Within this group, we identified hospitals certified as stroke centres. The Texas Department of State Health Services accepts comprehensive or primary stroke centre certification issued by either The Joint Commission (TJC) or Det Norske Veritas (DNV) Healthcare to receive CSC and PSC state designation.39,40 These hospitals meet guidelines set forth by the Brain Attack Coalition and American Stroke Association for acute stroke management.41 For the purposes of this study, CSCs and PSCs were combined into a single category – PSC. We did not inquire about other strategies utilized to deliver tPA such as ‘drip and ship’ or translation service at each emergency department.
Access calculations
Our primary analysis focused on calculating the population that was able to reach acute stroke care within 60 minutes. To do this, we created 60 minute travel sheds around each hospital in Texas. We first identified each hospital and located it in space using the hospital’s latitudinal and longitudinal coordinates. Next we subtracted a number of empirically derived fixed pre-hospital time intervals from the pre-determined travel shed time interval of 60 minutes, as previously described.42,43 These included: (a) the time from 911 activation to ambulance dispatch (activation interval) of 1.4 and 2.9 minutes for urban and rural areas, respectively; (b) the time spent on scene stabilizing the patient and preparing for transport (on-scene time of 13.5 and 15.1 minutes for urban and rural areas, respectively).43 We then used the road travel network and the posted drive speeds to determine which block groups were able to travel to the hospital within the remaining time. A block group was considered to have access to care if the block group’s population-weighted centre point (centroid) was within the travel shed. As this travel time only represents the second half of the journey (from the patient’s home to the hospital), we added 5.28 and 7.86 minutes for urban and rural areas respectively to account for the time for the ambulance to travel from the depot to the patient. Finally, we summed the population of all block groups that could reach each hospital in the specified travel time. For calculations to determine distances to each hospital, we used US Census Bureau block groups based on the 2000 census. Using the network analyst functionality in ESRI ArcMap 10.1, the shortest Euclidean (straight line) road network distances were determined between each population-weighted centroid and the nearest hospital.44,45 Each block group was linked exclusively to the nearest hospital and no group was counted more than once. We did not allow for crossing of state lines.
Determination of telemedicine use and access
As previously described,37 all acute care hospitals in Texas were contacted by telephone. Each hospital’s stroke coordinator or emergency department charge nurse was interviewed using a standardized questionnaire. Interviewees were asked if their hospital was (a) an acute care hospital, (b) a TJC, DNV or the state of Texas certified stroke centre, or (c) utilizing TM to provide acute stroke care. After verification of the stroke centre status obtained from the telephone survey, hospitals were designated into four categories: stand-alone PSCs (PSCs: hospitals that were PSCs but were not using TM for acute stroke care); PSCs using TM (PSC-TM: hospitals that were PSCs and were using TM for acute stroke care); TM for stroke care (TM: hospitals that were not PSCs but were using TM for acute stroke care) or none (hospitals that were not PSCs and were not using TM for acute stroke care). We calculated the difference between the population who could reach a PSC within 60 minutes (60-minute access) and the population who could reach a TM spoke (PSC-TM or TM-only) within 60 minutes, to determine the contribution of TM to access to acute stroke care. Using census data, we were then able to determine if racial or ethnic differences exist in access to acute stroke care through TM.
Statistics
Given the proportion with access to a stand-alone PSC was greater than 20% in all groups, we elected to use modified Poisson regression to produce prevalence odds ratios (POR) to illustrate the association between race and ethnicity and access to acute stroke care.46 This decision was made in an attempt to prevent the overestimation often seen when using logistic regression (odds ratios) in situations with prevalent outcomes.46 In addition to crude models, models were adjusted for urbanization.
Results
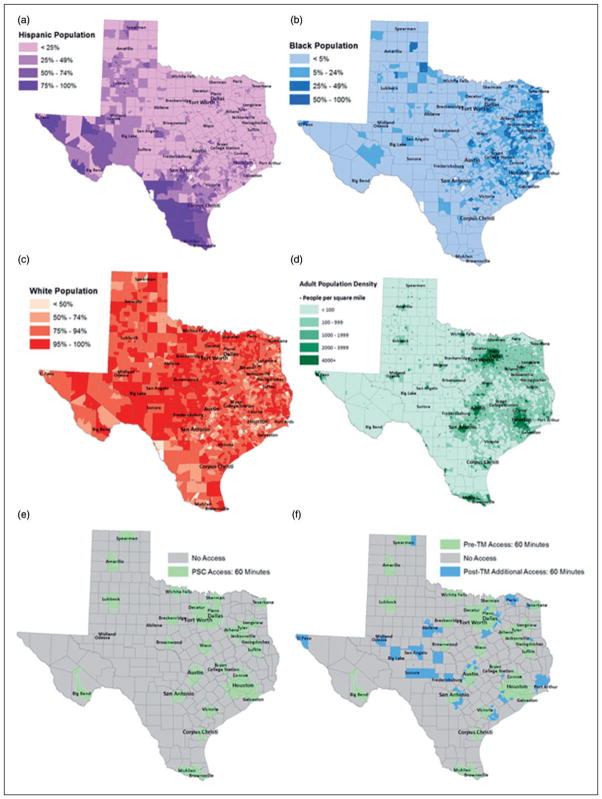
In 2009, the population of Texas was 23.8 million residents.32 Of these patients, 17 million were Caucasian/ White, 2.7 million were African American/Black and 4 million were classified as other (Figure 1A–D). The most common races included in the other category were American Indian, Asian, and Native Hawaiian. Nearly 8.6 million (36%) residents were Hispanic.
Figure 1.
The effects of telemedicine on primary stroke centre access in Texas.
A: Hispanic population
B: Black population
C: White population
D: Adult population density
E: 60 minute primary stroke centre access
F: 60 minute access afforded by telemedicine
PSC: primary stroke centre; TM: telemedicine
Maps were generated using ESRI ArcMap 10.1.
We identified 578 Texas hospitals in the AHA database, of which 96% (556/578) participated in the survey. Of the 22 hospitals who did not participate, seven could not be reached by phone (no answer, automated line), four declined participation and 11 had an inactive phone number. Of the participating hospitals, 395 identified themselves as acute care facilities (71%). Over 26% of acute care facilities (103/395) identified themselves as PSCs. While the majority of PSCs reported not using TM for acute stroke care, 21% (22/103) were using TM to deliver acute stroke care (PSC-TM). Only 9% (26/292) of non-PSCs were using TM for acute stroke care (TM).
We found that 18 million (75%) of the Texas population had 60-minute access to a stand-alone PSC (PSC). By including PSC-TM, 60-minute access increased to 19.5 Million (82%; Figure 1E–F). An additional 478,000 patients (2%) could access a hospital which has TM capabilities but that has not been PSC designated (TM). Nearly 4 million Texans (16%) do not have 60-minute access to acute stroke care.
Broken down by racial groups, Blacks had similar odds of having 60-minute access to acute stroke care when compared to Whites (POR 0.998, 95% CI 0.998–0.999). This finding remained after adjustment for urbanization (POR 0.997, 95% CI 0.995–0.998). We found that 83% of Black patients had 60 minute access to a stand-alone PSC compared to 73% of Whites (Table 1). Including PSC-TM expanded this access to an additional 5% of Blacks and nearly 7% of Whites for a combined total of 88% and 80% respectively. Residents of other racial background had access similar to Black residents (Table 1). TM hospitals provided 60-minute access for an additional 1.3% of Black residents and an additional 2.3% of White residents. The odds of providing 60-minute access to acute stroke care via existing TM sites were similar in Blacks and Whites (POR 1.000, 95% CI 1.000–1.000), even after adjustment for urbanization (POR 1.000, 1.000–1.001).
Table 1.
Current access to acute stroke care in Texas by race.
| Race
|
|||
|---|---|---|---|
| White (n =17,096,097) | Black (n =2,738,429) | Other (n =3,966,914) | |
| PSC | 12,431,953 (72.7%) | 2,270,715 (82.9%) | 3,251,664 (82.0%) |
| PSC-TM | 1,169,987 (6.8%) | 135,951 (5.0%) | 241,430 (6.1%) |
| TM | 397,961 (2.3%) | 35,789 (1.3%) | 44,898 (1.1%) |
| Non-PSC/No TM | 3,096,126 (18.1%) | 295,974 (10.8%) | 428,922 (10.8%) |
PSC: primary stroke centre; PSC-TM: primary stroke centre using telemedicine; TM: telemedicine.
Access to acute stroke care for Hispanic residents did not differ from non-Hispanic residents (Table 2). Nearly 75% of Hispanics could access a stand-alone PSC within 60 minutes compared to 76% of non-Hispanics. PSC-TM expanded this access by an additional 10% in Hispanics and 5% in non-Hispanics. Overall, Hispanics had similar odds of having 60-minute access to acute stroke care when compared to non-Hispanics (POR 1.000, 95% CI 1.000–1.000). This finding remained even adjusting for urbanization (POR 1.000, 95% CI 1.000–1.001). TM hospitals provided additional access to 1.1% of Hispanics and 2.5% of non-Hispanics. The odds of providing access to acute stroke care via TM were similar for Hispanics and their non-Hispanic counterparts (POR 1.000, 95% CI 1.000–1.000), even after adjustment for urbanization (POR 1.000, 95% CI 1.000–1.000).
Table 2.
Current access to acute stroke care in Texas by ethnicity.
| Ethnicity
|
||
|---|---|---|
| Hispanic (n =8,550,214) | Non-Hispanic (n =15,251,226) | |
| PSC | 6,402,169 (74.9%) | 11,552,233 (75.7%) |
| PSC-TM | 835,549 (9.8%) | 711,819 (4.7%) |
| TM | 95,972 (1.1%) | 382,676 (2.5%) |
| Non-PSC/No TM | 1,216,524 (14.2%) | 2,604,498 (17.1%) |
PSC: primary stroke centre; PSC-TM: primary stroke centre using telemedicine; TM: telemedicine.
Discussion
Our study is one of the first to investigate the impact of TM for stroke on racial and ethnic minorities. Our previous work has found that the addition of PSC-TM to traditional face-to-face neurologic consultation (PSC) provided an additional 1.5 million Texans access to the acute stroke expertise.37 Further, there were no significant differences in access to acute stroke care via PSC, PSC-TM, or TM among racial and ethnic minority groups. This is critical since these populations carry a higher burden of cerebrovascular disease. While disparities have been reported in other components of stroke care (differences in disease awareness and differences in attitudes, beliefs and compliance),27 our observations suggest that TM systems do not widen the disparity gap.
Over the last decade, stroke systems of care in the United States have focused on the establishment and certification of PSCs. Despite this, many people still do not have timely access to PSCs.13 Although systems of care are being developed to improve delivery of tPA, becoming a PSC does not require a certificate of need and as a result many PSCs are found in urban areas, leaving a substantial population underserved.47 In addition, many PSCs are geographically clustered, in part as a result of competitive market forces, creating what may be redundancy in the system. TM has emerged as a potential bridge in the system to help expand access to stroke care by virtually delivering sub-specialty expertise to hospitals, particularly those in rural areas. It seems, however, that only a small percentage of non-PSC hospitals are using this technology. Policy initiatives encouraging the incorporation of TM into regional planning for stroke could serve to advance population access to stroke care.48
Currently, racial and ethnic disparities exist in stroke prevalence, acute stroke care, and stroke related mortality.27 Our study provides reassurance that implementation of a TM system does not adversely impact access to care for racial and ethnic minorities. It has been well established that Black and Hispanic Americans have a disproportionally higher incidence of stroke22 and have delays at several points in the chain of survival for acute stroke care.27 One component of this is delayed evaluation in the emergency department and delayed neurological consultation.29,30 Equipping hospitals with TM capabilities can potentially improve this element of the disparity. While hospitals and city centres are clearly fixed, TM allows for innovated systems to be designed that are not constrained by traditional geographic limits.
Our study has several limitations. First, drive times calculations are based on data from trauma systems.43 While these are reasonable approximations, some data suggest that drive times for stroke patients may be six to 11 minutes longer.49,50 These calculations also do not account for geographic boundaries such as mountains, rivers and weather, nor do they account for traffic. Second, our analysis did not allow for patients to be transported across state lines. Third, our estimates are based on where people live, not necessarily where their strokes occur. We do know, however, that most strokes occur at home.51 Fourth, while our definition of a stand-alone PSC included both PSCs and CSCs certified by TJC, DNV, and the state of Texas, centres certified by national quality improvement projects were not included in this definition.52 Further, PSC credentialing is a dynamic process, and thus our inventory may underestimate the current number of credentialed centres.39,40 Fifth, our study only accounts for access to thrombolysis at PSCs, PSC-TM, or TM facilities and does not account for each individual hospital’s capability and/ or comfort in delivering tPA or employing other strategies such as ‘drip and ship’.53,54 This study is population based and does not account for the role that language barriers may play in individual treatment decisions using TM. Our study does not look at how the additional access provided by TM affects outcomes in racial and ethnic minorities. Finally, this is an ecological study. Observations at the aggregate level do not necessarily represent associations at the individual level.
Current access to in-person neurological expertise for acute stroke care is limited throughout the country and may disproportionally affect minority groups. Our findings suggest that the use of TM coupled with free standing PSCs can be used as part of a comprehensive strategy to address disparities in access to care. Although there are still barriers to the use of TM (reimbursement, privacy laws, fear of malpractice), the benefits of this model can be seen in all races and ethnicities without leading to any increases in the existing disparities in stroke care.
Acknowledgments
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Dr. Albright is supported by award numbers 5 T32 HS013852-10 from the Agency for Healthcare Research and Quality (AHRQ), 3 P60 MD000502-08S1 for the National Institute on Minority Health and Health Disparities (NIMHD), National Institutes of Health (NIH). Dr. Boehme is supported by award 13PRE13830003 from the American Heart Association (AHA). The content is solely the responsibility of the authors and does not necessarily represent the official views of the AHRQ, AHA or the NIH.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Towfighi A, Saver JL. Stroke declines from third to fourth leading cause of death in the United States: Historical perspective and challenges ahead. Stroke. 2011;42:2351–2355. doi: 10.1161/STROKEAHA.111.621904. [DOI] [PubMed] [Google Scholar]
- 2.Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA stroke study group. N Engl J Med. 1995;333:1581–1587. doi: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 3.Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359:1317–1329. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 4.Reeves MJ, Arora S, Broderick JP, et al. Acute stroke care in the US: Results from 4 pilot prototypes of the Paul Coverdell national acute stroke registry. Stroke. 2005;36:1232–1240. doi: 10.1161/01.STR.0000165902.18021.5b. [DOI] [PubMed] [Google Scholar]
- 5.Kleindorfer D, Lindsell CJ, Brass L, et al. National US estimates of recombinant tissue plasminogen activator use: ICD-9 codes substantially underestimate. Stroke. 2008;39:924–928. doi: 10.1161/STROKEAHA.107.490375. [DOI] [PubMed] [Google Scholar]
- 6.Hills NK, Johnston SC. Why are eligible thrombolysis candidates left untreated? Am J Prev Med. 2006;31:S210–216. doi: 10.1016/j.amepre.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Meurer WJ, Majersik JJ, Frederiksen SM, et al. Provider perceptions of barriers to the emergency use of tPA for acute ischemic stroke: A qualitative study. BMC Emerg Med. 2011;11:5. doi: 10.1186/1471-227X-11-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bambauer KZ, Johnston SC, Bambauer DE, et al. Reasons why few patients with acute stroke receive tissue plasminogen activator. Arch Neurol. 2006;63:661–664. doi: 10.1001/archneur.63.5.661. [DOI] [PubMed] [Google Scholar]
- 9.Lichtman JH, Jones SB, Wang Y, et al. Outcomes after ischemic stroke for hospitals with and without joint commission-certified primary stroke centers. Neurology. 2011;76:1976–1982. doi: 10.1212/WNL.0b013e31821e54f3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prabhakaran S, McNulty M, O’Neill K, et al. Intravenous thrombolysis for stroke increases over time at primary stroke centers. Stroke. 2012;43:875–877. doi: 10.1161/STROKEAHA.111.640060. [DOI] [PubMed] [Google Scholar]
- 11.Mullen MT, Kasner SE, Kallan MJ, et al. Joint commission primary stroke centers utilize more rt-PA in the nationwide inpatient sample. J Am Heart Assoc. 2013;2:e000071. doi: 10.1161/JAHA.112.000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Albright KC, Branas CC, Meyer BC, et al. Access: Acute cerebrovascular care in emergency stroke systems. Arch Neurol. 2010;67:1210–1218. doi: 10.1001/archneurol.2010.250. [DOI] [PubMed] [Google Scholar]
- 13.Carr BG, Branas CC. [accessed 9 August 2013];Strokemaps.Org stroke center maps. 2010 www.strokemaps.org.
- 14.Branas C. Stroke center access. [accessed 5 December 2013];Optimization modeling and comparative effectiveness of regionalized stroke care. 2010 www.collectiveip.com/grants/NIH:8512583.
- 15.Levine SR, Gorman M. “Telestroke”: The application of telemedicine for stroke. Stroke. 1999;30:464–469. doi: 10.1161/01.str.30.2.464. [DOI] [PubMed] [Google Scholar]
- 16.Hess DC, Wang S, Gross H, et al. Telestroke: Extending stroke expertise into underserved areas. Lancet Neurol. 2006;5:275–278. doi: 10.1016/S1474-4422(06)70377-5. [DOI] [PubMed] [Google Scholar]
- 17.Switzer JA, Hall C, Gross H, et al. A web-based telestroke system facilitates rapid treatment of acute ischemic stroke patients in rural emergency departments. J Emerg Med. 2009;36:12–18. doi: 10.1016/j.jemermed.2007.06.041. [DOI] [PubMed] [Google Scholar]
- 18.Kazley AS, Wilkerson RC, Jauch E, et al. Access to expert stroke care with telemedicine: Reach MUSC. Front Neurol. 2012;3:44. doi: 10.3389/fneur.2012.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Choi JY, Porche NA, Albright KC, et al. Using telemedicine to facilitate thrombolytic therapy for patients with acute stroke. Joint Comm J Qual Patient Saf. 2006;32:199–205. doi: 10.1016/s1553-7250(06)32025-9. [DOI] [PubMed] [Google Scholar]
- 20.Meyer BC, Raman R, Hemmen T, et al. Efficacy of site-independent telemedicine in the stroke doc trial: A randomised, blinded, prospective study. Lancet Neurol. 2008;7:787–795. doi: 10.1016/S1474-4422(08)70171-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics 2009 update. A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:480–486. doi: 10.1161/CIRCULATIONAHA.108.191259. [DOI] [PubMed] [Google Scholar]
- 22.White H, Boden-Albala B, Wang C, et al. Ischemic stroke subtype incidence among whites, blacks, and hispanics: The Northern Manhattan study. Circulation. 2005;111:1327–1331. doi: 10.1161/01.CIR.0000157736.19739.D0. [DOI] [PubMed] [Google Scholar]
- 23.Howard VJ, McClure LA, Meschia JF, et al. High prevalence of stroke symptoms among persons without a diagnosis of stroke or transient ischemic attack in a general population: The reasons for geographic and racial differences in stroke (REGARDS) study. Arch Intern Med. 2006;166:1952–1958. doi: 10.1001/archinte.166.18.1952. [DOI] [PubMed] [Google Scholar]
- 24.Kleindorfer DO, Khoury J, Moomaw CJ, et al. Stroke incidence is decreasing in whites but not in blacks: A population-based estimate of temporal trends in stroke incidence from the greater Cincinnati/Northern Kentucky stroke study. Stroke. 2010;41:1326–1331. doi: 10.1161/STROKEAHA.109.575043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stansbury JP, Jia H, Williams LS, et al. Ethnic disparities in stroke: Epidemiology, acute care, and postacute outcomes. Stroke. 2005;36:374–386. doi: 10.1161/01.STR.0000153065.39325.fd. [DOI] [PubMed] [Google Scholar]
- 26.Kimball MM, Neal D, Waters MF, et al. Race and income disparity in ischemic stroke care: Nationwide inpatient sample database, 2002 to 2008. J Stroke Cerebrovasc Dis. 2014;23:17–24. doi: 10.1016/j.jstrokecerebrovasdis.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 27.Cruz-Flores S, Rabinstein A, Biller J, et al. Racial-ethnic disparities in stroke care: The American experience: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42:2091–2116. doi: 10.1161/STR.0b013e3182213e24. [DOI] [PubMed] [Google Scholar]
- 28.Lacy CR, Suh DC, Bueno M, et al. Delay in presentation and evaluation for acute stroke: Stroke time registry for outcomes knowledge and epidemiology (S.T.R.O.K.E.) Stroke. 2001;32:63–69. doi: 10.1161/01.str.32.1.63. [DOI] [PubMed] [Google Scholar]
- 29.Karve SJ, Balkrishnan R, Mohammad YM, et al. Racial/ethnic disparities in emergency department waiting time for stroke patients in the United States. J Stroke Cerebrovasc Dis. 2011;20:30–40. doi: 10.1016/j.jstrokecerebrovasdis.2009.10.006. [DOI] [PubMed] [Google Scholar]
- 30.Brown DL, Lisabeth LD, Garcia NM, et al. Emergency department evaluation of ischemic stroke and TIA: The basic project. Neurology. 2004;63:2250–2254. doi: 10.1212/01.wnl.0000147292.64051.9b. [DOI] [PubMed] [Google Scholar]
- 31.Schwamm LH, Reeves MJ, Pan W, et al. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation. 2010;121:1492–1501. doi: 10.1161/CIRCULATIONAHA.109.881490. [DOI] [PubMed] [Google Scholar]
- 32.U.S. Census Bureau. [accessed 17 May 2011];Census of population and housing, population and housing unit counts PHC-3. 2000 www.census.gov/compendia/statab/2012/tables/12s0029.pdf.
- 33.Branas CC, Nance ML, Elliott MR, et al. Urban–rural shifts in intentional firearm death: Different causes, same results. Am J Public Health. 2004;94:1750–1755. doi: 10.2105/ajph.94.10.1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nance ML, Denysenko L, Durbin DR, et al. The rural-urban continuum: Variability in statewide serious firearm injuries in children and adolescents. Arch Pediatr Adolesc Med. 2002;156:781–785. doi: 10.1001/archpedi.156.8.781. [DOI] [PubMed] [Google Scholar]
- 35.Branas CC, Richmond TS, Schwab CW. Firearm homicide and firearm suicide: Opposite but equal. Public Health Rep. 2004;119:114–124. doi: 10.1177/003335490411900203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Butler M, Beale C. [accessed 9 August 2013];Rural-urban continuum codes for metro and nonmetro counties. 1993 www.ers.usda.gov/data-products/rural-urban-continuumcodes.aspx#.UqEtY8RDsn0.
- 37.Wu TC, Lyerly MJ, Albright KC, et al. Impact of telemedicine on access to acute stroke care in the state of Texas. Ann Clin Transl Neurol. 2014;1:27–33. doi: 10.1002/acn3.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.AHA. [accessed 17 May 2011];American Hospital Association: AHA data and directories. www.aha.org/research/rc/stat-studies/data-and-directories.shtml.
- 39.The Joint Commission. [accessed 9 August 2013];Advanced certification for primary stroke centers. 2013 www.jointcommission.org/certification/primary_stroke_centers.aspx.
- 40.Det Norske Veritas. [accessed 17 May 2011];DNV Stroke Center Certifications. http://dnvaccreditation.com/pr/dnv/primary-stroke-center-certification.aspx.
- 41.Alberts MJ, Hademenos G, Latchaw RE, et al. Recommendations for the establishment of primary stroke centers. Brain attack coalition J Am Med Assoc. 2000;283:3102–3109. doi: 10.1001/jama.283.23.3102. [DOI] [PubMed] [Google Scholar]
- 42.Branas CC, MacKenzie EJ, Williams JC, et al. Access to trauma centers in the United States. J Am Med Assoc. 2005;293:2626–2633. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 43.Carr BG, Caplan JM, Pryor JP, et al. A meta-analysis of prehospital care times for trauma. Prehosp Emerg Care. 2006;10:198–206. doi: 10.1080/10903120500541324. [DOI] [PubMed] [Google Scholar]
- 44.Love RF, Morris JG. Mathematical models of road travel distances. Manag Sci. 1979;25:130–139. [Google Scholar]
- 45.Love RF, Wesolowsky GO. Facilities location: Models and methods. New York: North-Holland Publishers; 1988. [Google Scholar]
- 46.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 47.National Conference of State Legislatures. [accessed 9 August 2013];Certificate of need: State health laws and programs. 2012 www.ncsl.org/research/health/con-certificate-of-need-state-laws.aspx.
- 48.Schwamm LH, Audebert HJ, Amarenco P, et al. Recommendations for the implementation of telemedicine within stroke systems of care: A policy statement from the American Heart Association. Stroke. 2009;40:2635–2660. doi: 10.1161/STROKEAHA.109.192361. [DOI] [PubMed] [Google Scholar]
- 49.Wojner-Alexandrov AW, Alexandrov AV, Rodriguez D, et al. Houston paramedic and emergency stroke treatment and outcomes study (HoPSTO) Stroke. 2005;36:1512–1518. doi: 10.1161/01.STR.0000170700.45340.39. [DOI] [PubMed] [Google Scholar]
- 50.Ramanujam P, Castillo E, Patel E, et al. Prehospital transport time intervals for acute stroke patients. J Emerg Med. 2009;37:40–45. doi: 10.1016/j.jemermed.2007.11.092. [DOI] [PubMed] [Google Scholar]
- 51.Kelly-Hayes M, Wolf PA, Kase CS, et al. Temporal patterns of stroke onset. The Framingham study. Stroke. 1995;26:1343–1347. doi: 10.1161/01.str.26.8.1343. [DOI] [PubMed] [Google Scholar]
- 52.Gropen T, Magdon-Ismail Z, Day D, et al. Regional implementation of the stroke systems of care model: Recommendations of the northeast cerebrovascular consortium. Stroke. 2009;40:1793–1802. doi: 10.1161/STROKEAHA.108.531053. [DOI] [PubMed] [Google Scholar]
- 53.Kleindorfer D, Xu Y, Moomaw CJ, et al. US geographic distribution of rt-PA utilization by hospital for acute ischemic stroke. Stroke. 2009;40:3580–3584. doi: 10.1161/STROKEAHA.109.554626. [DOI] [PubMed] [Google Scholar]
- 54.Qureshi AI, Chaudhry SA, Rodriguez GJ, et al. Outcome of the ‘drip-and-ship’ paradigm among patients with acute ischemic stroke: Results of a statewide study. Cerebrovasc Dis Extra. 2012;2:1–8. doi: 10.1159/000335097. [DOI] [PMC free article] [PubMed] [Google Scholar]