Significance
Commonly prescribed drugs for congestive heart failure (CHF) include β-adrenergic receptor antagonists or β-blockers. These drugs operate by inhibiting deleterious apoptotic signaling and normalizing inotropic signaling from these receptors. As the β-adrenergic receptor (β1AR) (dominant subtype in the heart) is systematically down-regulated during CHF while Gi (a G protein that antagonizes contractile signaling) is up-regulated, the ability to selectively control β2AR signaling becomes an attractive therapeutic approach. It is proposed that biasing receptor interaction with β-arrestins (promoting antiapoptotic signaling and possibly contraction) over G proteins may be therapeutically advantageous for the treatment of CHF. Here, we report a β-arrestin–biased pepducin of the β2AR that is able to induce cardiomyocyte contractility and antiapoptotic signaling to provide a pharmacological template for next-generation cardiovascular pharmaceuticals.
Keywords: GPCR, pepducin, carvedilol, arrestin, heart failure
Abstract
β-adrenergic receptors (βARs) are critical regulators of acute cardiovascular physiology. In response to elevated catecholamine stimulation during development of congestive heart failure (CHF), chronic activation of Gs-dependent β1AR and Gi-dependent β2AR pathways leads to enhanced cardiomyocyte death, reduced β1AR expression, and decreased inotropic reserve. β-blockers act to block excessive catecholamine stimulation of βARs to decrease cellular apoptotic signaling and normalize β1AR expression and inotropy. Whereas these actions reduce cardiac remodeling and mortality outcomes, the effects are not sustained. Converse to G-protein–dependent signaling, β-arrestin–dependent signaling promotes cardiomyocyte survival. Given that β2AR expression is unaltered in CHF, a β-arrestin–biased agonist that operates through the β2AR represents a potentially useful therapeutic approach. Carvedilol, a currently prescribed nonselective β-blocker, has been classified as a β-arrestin–biased agonist that can inhibit basal signaling from βARs and also stimulate cell survival signaling pathways. To understand the relative contribution of β-arrestin bias to the efficacy of select β-blockers, a specific β-arrestin–biased pepducin for the β2AR, intracellular loop (ICL)1–9, was used to decouple β-arrestin–biased signaling from occupation of the orthosteric ligand-binding pocket. With similar efficacy to carvedilol, ICL1–9 was able to promote β2AR phosphorylation, β-arrestin recruitment, β2AR internalization, and β-arrestin–biased signaling. Interestingly, ICL1–9 was also able to induce β2AR- and β-arrestin–dependent and Ca2+-independent contractility in primary adult murine cardiomyocytes, whereas carvedilol had no efficacy. Thus, ICL1–9 is an effective tool to access a pharmacological profile stimulating cardioprotective signaling and inotropic effects through the β2AR and serves as a model for the next generation of cardiovascular drug development.
Beta-antagonists, also known as β-blockers, have been indicated for the treatment of pathological cardiac diseases, including congestive heart failure (CHF) and high blood pressure, for decades (1, 2). A select number of these agents, including the clinically used carvedilol, have been identified as β-arrestin–biased agonists of β-adrenergic receptors based on their ability to promote β-arrestin–dependent signaling over G-protein activation (3, 4). It is believed that the β-arrestin activation may provide additional cardioprotection based on its ability to mediate antiapoptotic signaling. As these are orthosteric ligands, there have been no means to decouple the activation of receptor-dependent β-arrestin signaling from the occupation of the orthosteric ligand-binding pocket to study their independent contribution to its efficacy as these properties appear inherently linked.
Recently, we described the characterization of a library of modulators of the β2-adrenergic receptor (β2AR) known as pepducins (5). Pepducins are lipidated peptides derived from the intracellular loops (ICLs) of a G-protein–coupled receptor (GPCR) that can stimulate or inhibit downstream signaling processes of their cognate receptor (6). From a 2D screen, the β2AR pepducin library displayed a wide range of properties, spanning those that had complete Gs bias to some that were β-arrestin biased (5).
In this report, ICL1–9, a β-arrestin–biased pepducin derived from the β2AR, is used to dissect the relative contribution of β-arrestin bias in the bipartite mechanism of clinically relevant β-blockers. ICL1–9 is able to effectively promote the activities expected of a β-arrestin–biased agonist including GPCR kinase (GRK)-mediated receptor phosphorylation, β-arrestin recruitment, receptor internalization, ERK activation, and EGF receptor transactivation comparable to the efficacy of carvedilol. As these actions are independent of the orthosteric ligand-binding site, ICL1–9 is a unique tool with which the contribution of β-arrestin processes and signaling of a β-arrestin–biased β-blocker can be assessed in isolation.
To this end, we performed a comparative functional study between carvedilol and ICL1–9 to assess their relative efficacy in regulating primary murine cardiomyocyte contractility. Surprisingly, ICL1–9 was able to induce cardiomyocyte contraction, whereas carvedilol did not. Taken together, we characterize a β2AR-dependent β-arrestin–biased pepducin that promotes cardioprotective signaling paired with induction of cardiomyocyte contractility. This pharmacological profile is not only the first to be reported to our knowledge through the β2AR, but may prove to be therapeutically superior to currently prescribed heart failure drugs.
Results
ICL1–9 Is a Potent β-Arrestin–Biased Pepducin.
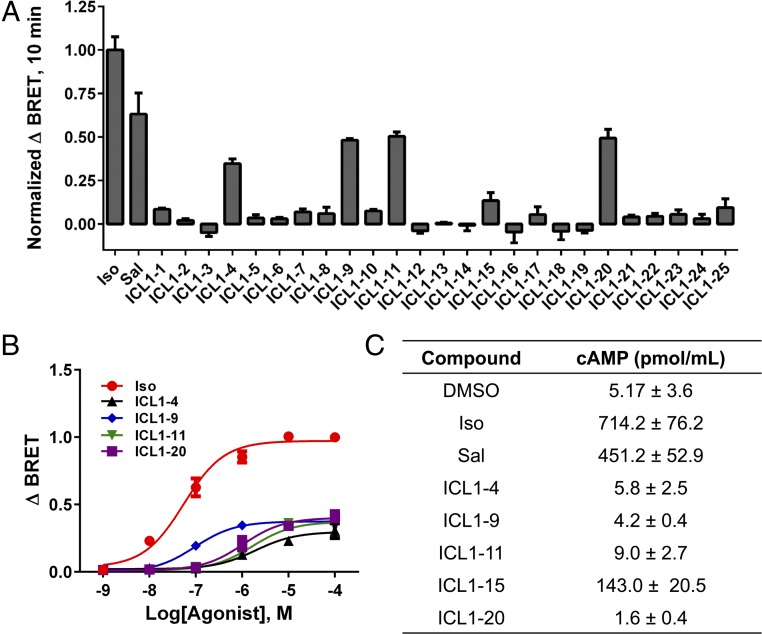
In our initial characterization of the β2AR-derived pepducin library, it appeared that putative “β-arrestin–biased” pepducins were derived from ICL1 (5). To further assess pepducin-promoted β-arrestin recruitment, bioluminescense resonance energy transfer (BRET) was monitored in HEK293 cells cotransfected with a β2AR–Renilla reniformus luciferase II fusion (β2AR–RLucII) and GFP10-tagged β-arrestin2. In secondary screening assays, the pepducins ICL1–4, –9, –11, –15 and –20 were able to promote significant β-arrestin recruitment after 10 min with efficacies ranging between 13% and 50% of the response to isoproterenol (a nonselective β-agonist) (Fig. 1A). As ICL1–15 has been previously demonstrated to promote increases in cAMP production (5), it was not studied further. Putative β-arrestin–biased pepducins were next analyzed by BRET for their relative potency. ICL1–9 exhibited the highest potency with an EC50 of β-arrestin2 recruitment of 96 ± 14 nM, whereas ICL1–4 (1.9 ± 0.5 μM), ICL1–11 (1.7 ± 0.5 μM) and ICL1–20 (1.1 ± 0.3 μM) demonstrated lower potencies (Fig. 1B). The β-arrestin bias of these pepducins was verified by analysis of cAMP production in HEK293 cells. ICL1–4, –9, and –20 did not promote any cAMP production compared with vehicle control, whereas ICL1–11 gave an ∼2-fold increase (Fig. 1C). This compares with isoproterenol and salbutamol, which gave 137-fold and 87-fold increases in cAMP, respectively. Thus, ICL1–9 is a potent β-arrestin–biased activator of the β2AR and was used for additional characterization and mechanistic studies.
Fig. 1.
ICL1–9 is a potent β-arrestin–biased pepducin. (A) β-Arrestin recruitment was assessed by BRET2 in HEK293 cells transiently transfected with β2AR–RLucII and GFP10–β-arrestin2. β-Arrestin2 recruitment is reported at 10 min postagonist stimulation with 1 μM isoproterenol (Iso), 5 μM salbutamol (Sal), or 10 μM pepducin. The sequences of these pepducins and initial BRET analysis for isoproterenol, salbutamol, ICL1–4, ICL1–11, ICL1–15, and ICL1–20 have been previously reported, albeit as time courses (5). Although ICL1–9 exhibited a modest ability to promote β-arrestin recruitment in our previous primary screen (5), subsequent analysis shows that it has comparable efficacy to ICL1–4, ICL1–11, and ICL1–20. The data are represented by the mean ± SD from three independent experiments. (B) ICL1–9 is a high-potency β-arrestin–biased pepducin with an EC50 of 96 ± 14 nM with a sequence of LVITAIAKFERLQTVTNY containing an N-terminal palmitate and C-terminal amide (5). ICL1–4 (1.9 ± 0.5 μM), ICL1–11 (1.7 ± 0.5 μM), and ICL1–20 (1.1 ± 0.3 μM) demonstrated comparable efficacy to ICL1–9 but operated with lower potency. The data are represented by the mean ± SD from three independent experiments. (C) cAMP production in HEK293 cells using Iso, Sal, and the pepducins that promoted β-arrestin recruitment in A. The data represent the mean ± SD from three independent experiments and are primarily derived from our previous report (5).
ICL1–9 Exhibits the Functional Properties of β-Arrestin Bias.
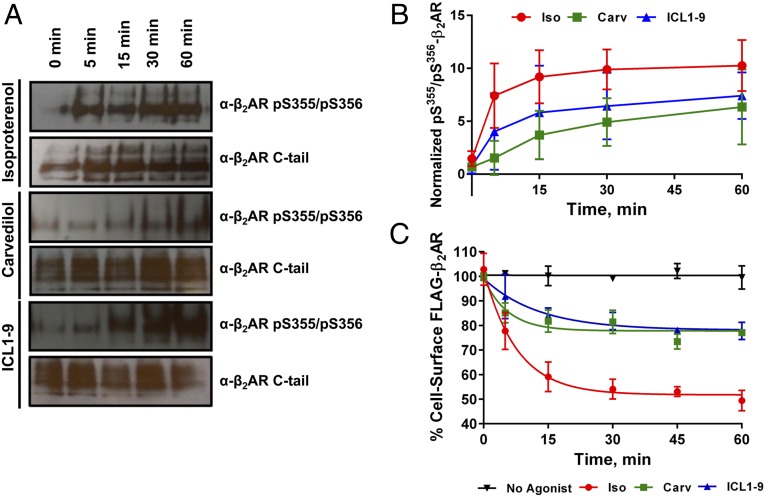
β-Arrestin recruitment is dependent on GRK-mediated phosphorylation of the C-terminal tail of the β2AR (7). Agonist-promoted GRK-mediated β2AR phosphorylation was assessed using a phosphospecific antibody detecting phosphorylation of Ser355/Ser356 in HEK293 cells stably expressing FLAG–β2AR (8–10). Isoproterenol rapidly and robustly promoted phosphorylation at this site, whereas both carvedilol (a nonselective β-arrestin–biased agonist) and ICL1–9 also stimulated receptor phosphorylation, albeit with slower kinetics and extent of phosphorylation (Fig. 2 A and B). It appears that ICL1–9 may stabilize a β2AR conformation that is a favorable substrate for GRKs and subsequent β-arrestin recruitment.
Fig. 2.
ICL1–9 promotes β2AR phosphorylation and internalization. (A) Receptor phosphorylation was monitored over a time course in the presence of 1 μM isoproterenol, 10 μM carvedilol or 10 μM ICL1–9 in HEK293 cells stably overexpressing FLAG–β2AR. In-cell phosphorylation was detected using a phosphospecific antibody for pSer355/pSer356 postreceptor immunoprecipitation. With slower kinetics than isoproterenol, ICL1–9 and carvedilol promoted robust receptor phosphorylation. The data are representative of three independent experiments. (B) Relative pSer355/pSer356 detection as determined by densitometry analysis (ImageJ) of immunoprecipitated β2AR from HEK293 cells stably overexpressing a FLAG–β2AR in the presence of 1 μM isoproterenol, 10 μM carvedilol, or 10 μM ICL1–9. The data are represented by the mean ± SD from three independent experiments. (C) Both carvedilol and ICL1–9 were able to stimulate comparable levels of FLAG–β2AR internalization as monitored by a cell-surface ELISA, albeit less than that induced by isoproterenol. The data are represented by the mean ± SD from three independent experiments.
β-Arrestins are critical regulators of agonist-promoted receptor internalization for many GPCRs, including the β2AR (11). Receptor internalization of the β2AR was studied by cell surface ELISA poststimulation using isoproterenol, carvedilol, and ICL1–9. As expected, isoproterenol, carvedilol, and ICL1–9 were able to promote β2AR internalization, albeit with variable kinetics and efficacy (Fig. 2C).
ICL1–9 Demonstrates Selectivity for the β2AR.
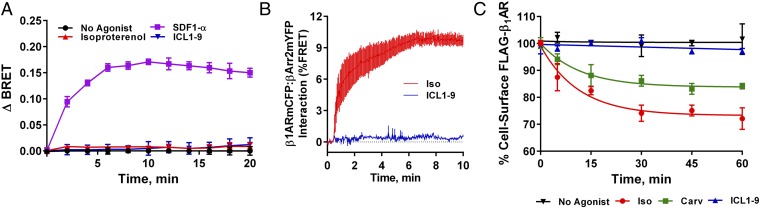
It was believed that pepducins demonstrate receptor specificity for the cognate receptor from which they were derived (6). However, there is growing evidence that some pepducins can operate through multiple GPCRs as some pepducin sequences can be found in multiple receptor subtypes (5, 12–14). It is also plausible that ICL1–9 is operating independently of a particular receptor and directly recruiting β-arrestins to the cell membrane. This mode of operation may crowd the membrane with the BRET acceptor and create a “false-positive” profile for specific BRET interactions that could be concluded at any receptor of interest. To test the receptor specificity and dependency mechanism of action, β-arrestin recruitment to the GPCR CXCR4 was assessed by BRET (15). ICL1–9 demonstrated no efficacy in the recruitment of β-arrestins to CXCR4, unlike its endogenous ligand, SDF1α (Fig. 3A). Importantly, isoproterenol promoted recruitment of β-arrestin to the β2AR, whereas monitoring β-arrestin–CXCR4 BRET (to simulate BRET acceptor membrane crowding) did not promote any change in ΔBRET (Fig. 3A). As these experiments were performed in HEK293 cells stably overexpressing FLAG–β2AR, this demonstrates that mass recruitment of β-arrestins to the membrane does not induce a specific BRET response with CXCR4–RlucII. These results suggest that ICL1–9 promotes a β2AR-dependent interaction with β-arrestins and does not operate via direct recruitment of β-arrestin to the cell membrane.
Fig. 3.
ICL1–9 demonstrates specificity toward the β2AR compared with CXCR4 and the β1AR. (A) β-Arrestin2 recruitment was monitored over a time-course postagonist stimulation with 50 nM SDF-1α, 1 μM isoproterenol, or 10 μM ICL1–9 by BRET2 in HEK293 cells stably overexpressing FLAG–β2AR and transiently transfected with CXCR4–RLucII and GFP10–β-arrestin2. SDF-1α was able to effectively promote β-arrestin2 recruitment to CXCR4, whereas isoproterenol and ICL1–9 had no effect. The data are represented by the mean ± SD from three independent experiments. (B) β-Arrestin2 recruitment was monitored over a time-course postagonist stimulation with 1 μM isoproterenol or 10 μM ICL1–9 by FRET in U2S cells infected with FLAG–β1AR–mCFP and Ad–β-arrestin2–mYFP. Isoproterenol was able to effectively promote β-arrestin2 recruitment to the β1AR, whereas ICL1–9 did not demonstrate similar efficacy. The data are represented by the mean ± SEM from three independent experiments. (C) Agonist-promoted β1AR internalization was monitored by a cell-surface ELISA in HEK293 cells transiently expressing FLAG–β1AR. Both carvedilol (10 μM) and isoproterenol (1 μM) were able to promote FLAG–β1AR internalization, whereas ICL1–9 (10 μM) did not stimulate FLAG–β1AR internalization. The data are represented by the mean ± SD from three independent experiments.
Due to sequence similarity of the β1AR and β2AR (71% identity and 76% similarity in ICL1; 54% identity and 61% similarity overall), it is plausible that ICL1–9 can also signal through the β1AR as ICL3–9 demonstrated in our previous report (5). To assess the specificity of ICL1–9 between the two subtypes, β-arrestin recruitment to the β1AR was monitored by FRET. Agonist-promoted β-arrestin recruitment was observed when cells were treated with isoproterenol, whereas no change in FRET activity was observed in response to ICL1–9 (Fig. 3B). Further corroborating β2AR selectivity, isoproterenol and carvedilol were able to induce FLAG–β1AR internalization, whereas ICL1–9 did not induce significant receptor internalization over a 1-h time course (Fig. 3C). Thus, ICL1–9 appears to be selective for the β2AR and shows no activity toward the β1AR.
ICL1–9 Promotes β-Arrestin Signaling.
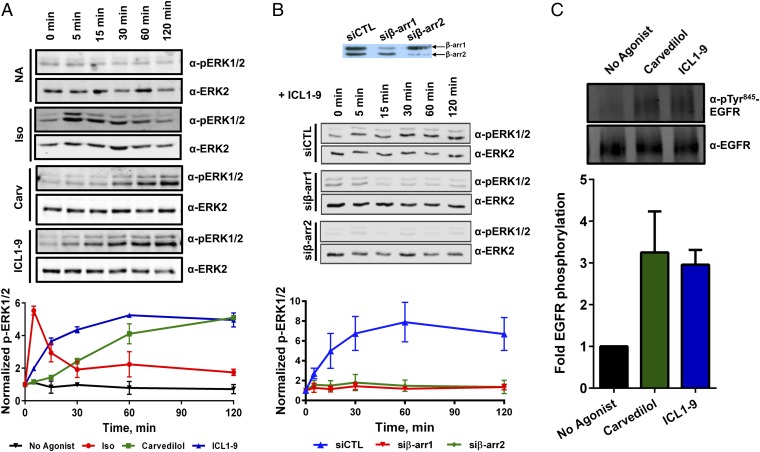
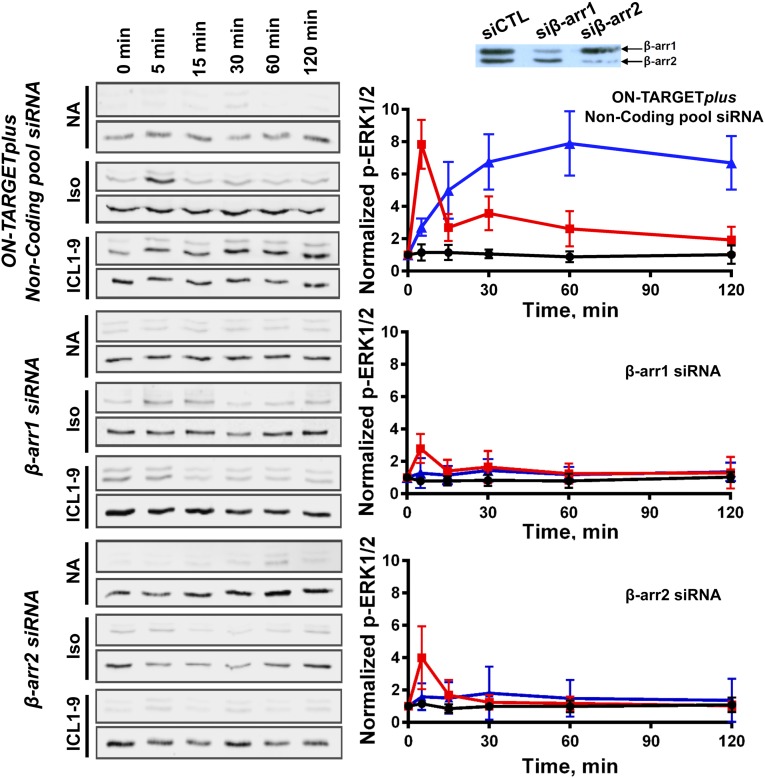
GPCRs are now appreciated to signal through a number of intracellular transducers beyond heterotrimeric G proteins including β-arrestins (7), which can act as a scaffold for multiple protein kinase cascades such as MAP kinases (16, 17). Previous studies have demonstrated that isoproterenol and carvedilol can promote β-arrestin–dependent ERK1/2 phosphorylation (3). Over a 2-h time course, ICL1–9 was able to induce ERK1/2 phosphorylation with a response profile that demonstrated faster kinetics despite similar efficacy compared with carvedilol. Isoproterenol exhibited the fastest kinetics to maximal efficacy but lacked the magnitude of the late-phase signal observed with carvedilol and ICL1–9 stimulation (Fig. 4A). ERK1/2 phosphorylation in response to ICL1–9 was completely dependent on the expression of β-arrestins (Fig. 4B). The stark loss on ICL1–9 promoted ERK1/2 phosphorylation in cells treated with β-arrestin siRNAs further corroborate an essential role for β-arrestins in ICL1–9 activity. It should also be noted that β-arrestin1/2 knockdown also reduced isoproterenol-promoted ERK1/2 phosphorylation (Fig. S1), as previously seen by others (18).
Fig. 4.
ICL1–9 promotes β-arrestin–biased intracellular signaling. (A) As monitored by Western blotting, ICL1–9, carvedilol, and isoproterenol promoted ERK1/2 phosphorylation in HEK293 cells stably overexpressing a FLAG–β2AR with response profiles that varied in kinetics (isoproterenol > ICL1–9 > carvedilol) and efficacy. The blots are representative of three independent experiments and the plot represents the quantitated mean ± SD from three independent experiments. (B) In cells treated with siRNAs targeted to β-arrestin1 (Middle) and β-arrestin2 (Bottom), ICL1–9-promoted ERK1/2 phosphorylation (blue) is dependent on β-arrestin expression. The blots are representative of three independent experiments and the plot represents the quantitated mean ± SD from three independent experiments. (C) Carvedilol and ICL1–9 demonstrated similar efficacy in EGFR transactivation as monitored by Western blotting for EGFR pTyr845 in HEK293 cells stably overexpressing FLAG–β2AR. The blot is representative of three independent experiments and the plot represents the quantitated mean ± SD from three independent experiments.
Fig. S1.
In cells treated with siRNAs targeted to β-arrestin1 (Middle) and β-arrestin2 (Bottom), ICL1–9-promoted ERK1/2 phosphorylation (blue) is dependent on β-arrestin expression. Interestingly, siRNA treatment targeting β-arrestin1 and β-arrestin2 also reduced the burst and sustained phase of isoproterenol-promoted ERK1/2 phosphorylation (red). The blots are representative of three independent experiments and the plot represents the quantitated mean ± SD from three independent experiments. The ICL1–9 results are identical to those shown in Fig. 4B.
One mechanism by which β-arrestin–biased β-blockers promote ERK1/2 phosphorylation involves βAR cross-talk with the EGF receptor (EGFR) (17, 19). For example, carvedilol has been shown to promote βAR-mediated EGFR transactivation in a β-arrestin–dependent manner (20). In HEK293 cells stably overexpressing FLAG–β2AR, ICL1–9 promoted EGFR transactivation, as monitored by receptor phosphorylation at EGFR Tyr845, comparable to what is observed with carvedilol (Fig. 4C). These studies indicate that ICL1–9 and carvedilol mediate similar intracellular signaling responses in HEK293 cells, although with slightly different kinetics and efficacy.
Mechanism of ICL1–9 Action.
ICL1–9 decouples β-arrestin–bias activity from the orthosteric ligand-binding pocket.
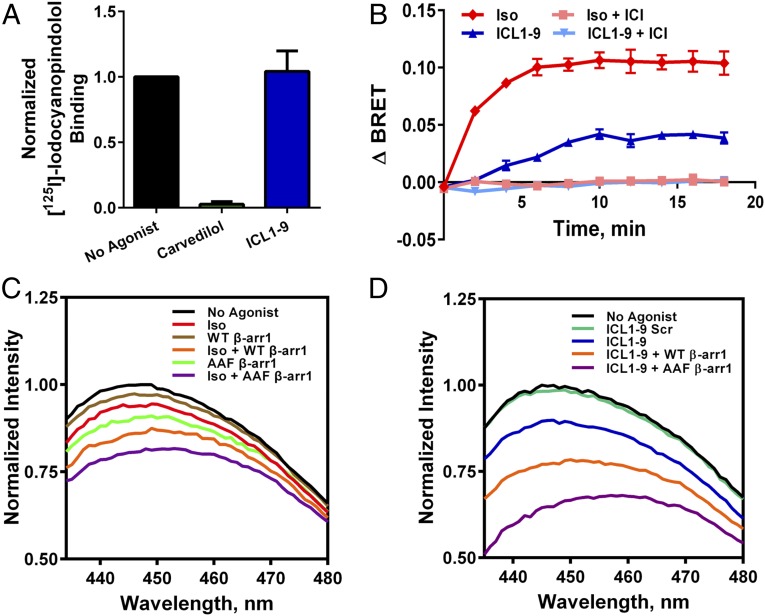
ICL1–9 can selectively promote GRK-mediated β2AR phosphorylation, β-arrestin recruitment, receptor internalization, and β-arrestin–dependent signaling comparable to carvedilol. Currently, there is no method to decouple the ability of β-blockers to occupy the orthosteric ligand-binding site with the ability to promote β-arrestin recruitment. To determine whether ICL1–9 acts to alter orthosteric ligand binding, we performed radioligand-binding studies. As expected, carvedilol effectively inhibited access to the orthosteric-binding site, whereas ICL1–9 did not affect [125I]-iodocyanopindolol binding to β2ARs (Fig. 5A). Because ICL1–9 acts at β2ARs independently of the orthosteric-binding site to induce β-arrestin–dependent signaling with comparable efficacy to carvedilol, it may serve as an ideal tool to understand the relative impact of β-arrestin–dependent β2AR signaling.
Fig. 5.
ICL1–9 operates independently of the orthosteric ligand-binding site to stabilize a β2AR conformation that can interact with β-arrestins. (A) ICL1–9 did not modulate [125I]-iodocyanopindolol binding in HEK293 cells stably overexpressing a FLAG–β2AR, whereas carvedilol completely inhibited radioligand binding. The data are represented by the mean ± SD from three independent experiments. (B) The ability of ICL1–9 to recruit β-arrestins (as monitored by BRET2) can be inhibited by the inverse agonist ICI-118551 despite its ability to operate independently of the ligand-binding site. The data are represented by the mean ± SD from three independent experiments. (C) Lipid bicelles containing 50 nM purified β2AR labeled with monobromobimane at Cys265 detected TM6 movement (loss of peak fluorescence and increase in λmax) in the presence of 100 nM isoproterenol (red), 50 nM WT β-arrestin1 (brown), and 50 nM β-arrestin1–AAF (green) with response profiles that varied in magnitude (β-arrestin1–AAF > isoproterenol > WT β-arrestin1). Coincubation with WT β-arrestin1 (orange) or β-arrestin1–AAF (purple) in the presence of isoproterenol further stabilized TM6 movement. (D) ICL1–9 (10 μM, blue) also stabilized a conformational change in the β2AR that promoted TM6 movement. Coincubation of ICL1–9 with WT β-arrestin1 (orange) or β-arrestin1–AAF (purple) further stabilized TM6 movement.
ICL1–9 is sensitive to the inverse agonist ICI-118551.
The inverse-agonist ICI-118551 is proposed to operate by restricting conformational dynamics of the β2AR and stabilize an inactive receptor conformation (21–23). Thus, if ICL1–9 requires a conformational change in the β2AR for activity, it may demonstrate sensitivity to ICI-118551. Indeed, the ability of ICL1–9 to promote β-arrestin coupling to the β2AR (as monitored by BRET) was significantly inhibited by pretreatment with ICI-118551 (Fig. 5B). A similar relationship was observed when cells were pretreated with ICI-118551 and stimulated with isoproterenol, although this activity can be best explained by orthosteric-binding site competition. As ICL1–9 operates independently from the orthosteric ligand-binding pocket, its sensitivity to ICI-118551 likely stems from a conformational competition between an ICL1–9-promoted β-arrestin–biased conformation and an ICI-118551–promoted inactive conformation of the β2AR.
ICL1–9 promotes a β2AR conformation that couples to β-arrestins.
Upon GRK-mediated phosphorylation, many GPCRs, including the β2AR, bind β-arrestins with high affinity (11). Recently, visualization of the GPCR–arrestin interface was achieved by serial femtosecond X-ray laser crystallography of a rhodopsin/arrestin complex (24). Additional insight was gained through cocrystallization studies of an arrestin finger loop peptide and rhodopsin (25), and by electron microscopy and deuterium exchange analysis of a β-arrestin1 complex with a β2AR–vasopressin 2 receptor C-terminal tail fusion (26). Each study reported a number of common structural features, including the stabilization of an outward movement of the receptor transmembrane 6 (TM6) by the arrestin finger loop (25). This conformational stabilization is similar to that induced by Gs interaction with the β2AR (27). Thus, it may be possible to detect β-arrestin/β2AR interaction by methods similar to those used in assessing G-protein coupling.
TM6 movement associated with receptor activation and G-protein interaction has been previously monitored using purified β2AR modified with monobromobimane at Cys265 (mbb–β2AR) (28, 29). The environmentally sensitive monobromobimane demonstrates a decrease in peak fluorescence and a red shift upon TM6 movement when Cys265 moves from a local hydrophobic environment to a position that is solvent exposed (28). Both isoproterenol and ICL1–9 were able to promote mbb–β2AR conformational changes that stabilized TM6 movement (indicated by loss of peak fluorescence and increase in λmax; Fig. 5 C and D). Additionally, β-arrestin–promoted conformational changes were detected in TM6 as incubation with WT β-arrestin or β-arrestin1–AAF (a partially preactivated mutant that promotes independence from prerequisite receptor phosphorylation) (30)-modulated monobromobimane fluorescence (AAF > WT; Fig. 5C). Pretreatment with isoproterenol further stabilized TM6 movement in the presence of WT or mutant β-arrestin (Fig. 5C). Coincubation with ICL1–9 and β-arrestins (WT and AAF) led to striking changes in mbb–β2AR TM6 movement (Fig. 5D). Whereas ICL1–9-stabilized β2AR/β-arrestin1 complexes exhibited greater relative changes in the Stokes shift and λmax compared with isoproterenol-treated complexes (Fig. 5 C and D), isoproterenol was used at a subsaturating concentration in these studies.
ICL1–9 Promotes β2AR-Dependent Cardiomyocyte Contractility.
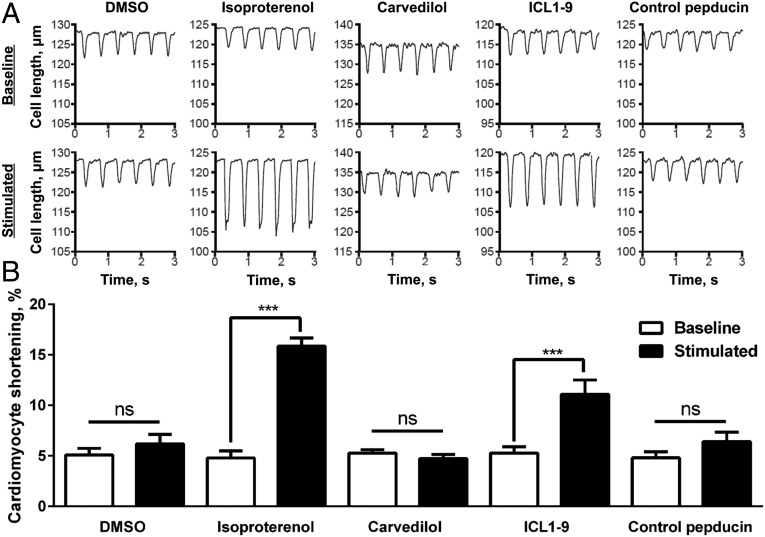
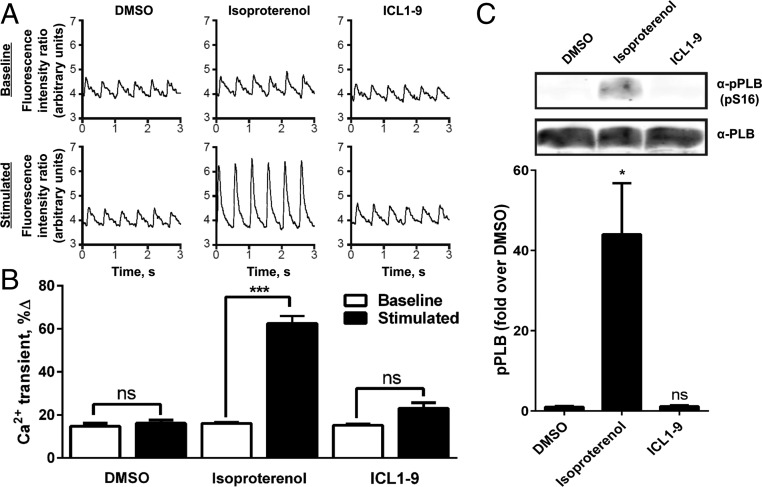
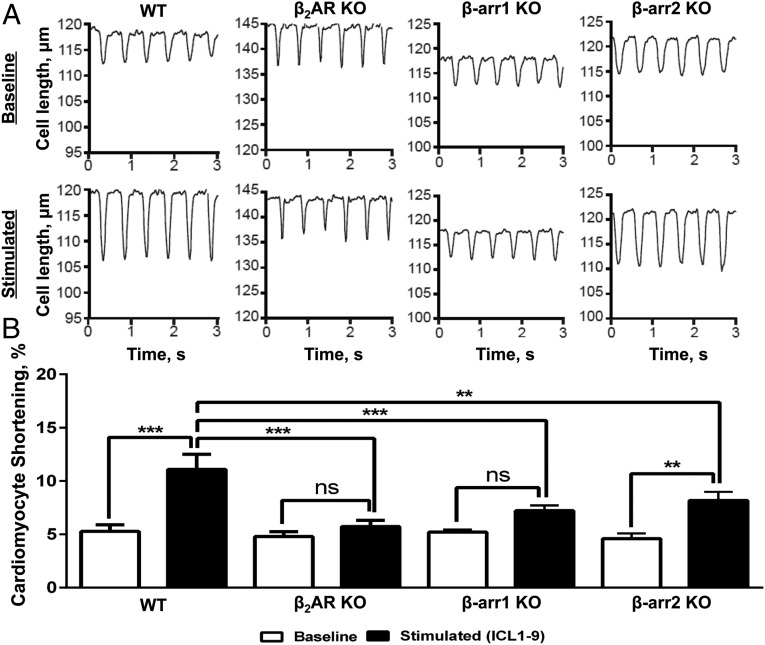
β-Blockers are commonly prescribed pharmaceuticals used in the treatment of CHF (1, 2). It is believed that β-blockers act to inhibit pathogenic βAR signaling pathways, including those mediating cell death (31–33). As G-protein–dependent signaling has been attributed to cardiomyocyte death, the use of a β-arrestin–biased agonist could be an advantageous therapeutic approach (34). Beyond its inability to activate G-protein signaling, evidence has suggested that β-arrestin–biased signaling promotes cardiomyocyte survival signaling along with induction of cardiomyocyte contractility (3, 35–38). Indeed, a β-arrestin–biased agonist for the angiotensin II type 1A receptor (AT1AR), TRV027, has demonstrated the ability to promote β-arrestin–dependent cardiac contraction in vivo and is currently in clinical trials for the treatment of heart failure (37, 38). As a comparable pharmacological profile through the β2AR has yet to be reported, the ability to promote contraction was assessed using primary WT adult murine cardiomyocytes. Surprisingly, ICL1–9 was able to induce robust cardiomyocyte contraction (∼53% of isoproterenol promoted) despite its inability to stimulate Gs-protein activation (Fig. 6 A and B). Interestingly, when WT cardiomyocytes were treated with carvedilol, a partial restriction of basal contraction was observed rather than induction of contraction (Fig. 6 A and B). Conventional cardiomyocyte contraction mechanisms depend on calcium mobilization and subsequent activation of the cardiomyocyte sarcomere. Unlike isoproterenol, ICL1–9 did not promote significant calcium mobilization in primary murine cardiomyocytes (Fig. 7 A and B). The activation of PKA signaling also plays a prominent role in conventional cardiomyocyte inotropic mechanisms. PKA activity is dependent on the upstream generation of cAMP and phosphorylates a number of effectors involved in cardiomyocyte inotrophy and lusitrophy. In response to β-agonists, PKA contributes to cardiomyocyte relaxation mechanisms through the phosphorylation of phospholamban (PLB), which relieves its inhibition of the sarcoplasmic reticulum Ca2+-ATPase (SERCA) pump and leads to rapid calcium reuptake into the sarcoplasmic reticulum. As ICL1–9 is proposed to operate through a β-arrestin–mediated mechanism of cardiomyocyte contraction, ICL1–9 was unable to induce significant PLB phosphorylation, whereas isoproterenol, a conventional β-agonist, stimulated robust PLB phosphorylation (Fig. 7C). Although ICL1–9 does not promote cardiomyocyte contraction through conventional mechanisms, ICL1–9 activity is strikingly dependent on the β2AR and operates through β-arrestin recruitment as cardiomyocytes derived from β2AR, β-arrestin1, or β-arrestin2 knockout mice exhibit significantly impaired responsiveness to ICL1–9 (Fig. 8 A and B). It is worth noting that ICL1–9-induced cardiomyocyte contraction was particularly dependent on β-arrestin1 (Fig. 8), perhaps reflecting the higher level of β-arrestin1 expression in the heart compared with β-arrestin2 (Fig. S2).
Fig. 6.
ICL1–9 promotes β2AR-mediated cardiomyocyte contraction, whereas carvedilol does not demonstrate similar efficacy. (A) WT adult murine cardiomyocytes were isolated and assessed for basal and agonist-promoted contractility using a digital videocamera-coupled microscope in the presence or absence of 0.1% DMSO, 0.5 μM isoproterenol, 10 μM carvedilol, 10 μM ICL1–9, or 10 μM control pepducin. Representative cell length (in micrometers) tracings at 2 Hz in the basal or stimulated state for each test condition are reported. (B) ICL1–9 was able to promote significant contraction in WT adult murine cardiomyocytes, whereas carvedilol did not stimulate a similar effect. The data are represented by the mean ± SEM from n = 4–8 individual cardiomyocytes from at least three independent primary isolations. ns, not significant, ***P < 0.001 using a one-way ANOVA with Newman–Keuls multiple comparison test.
Fig. 7.
ICL1–9 does not induce Ca2+ mobilization or PLB phosphorylation in adult cardiomyocytes. (A) Representative tracings from field stimulation (2 Hz)–induced Ca2+ transients in Fura2-loaded WT adult murine cardiomyocytes in response to 0.1% DMSO, 0.5 μM isoproterenol, or 10 μM ICL1–9. Representative fluorescence intensity ratio tracings in the basal or stimulated state for each test condition are reported. (B) Isoproterenol increased, whereas ICL1–9 did not have a significant impact on Ca2+-transient responses in adult murine cardiomyocytes. The data are represented by the mean ± SEM from 6–12 cardiomyocytes from at least three independent primary isolations. ns, not significant, ***P < 0.001 using a one-way ANOVA with Newman–Keuls multiple comparison test. (C) Immunoblot for total (Bottom) and phosphorylated (Ser16, Top) PLB following stimulation of isolated WT adult murine cardiomyocytes with 0.1% DMSO, 0.1 μM isoproterenol or 10 μM ICL1–9 for 5 min. Summarized data in the histogram show that isoproterenol, but not ICL1–9, significantly increased PLB phosphorylation. The data are represented by the mean ± SEM from three independent primary cardiomyocyte isolations. ns, not significant, *P < 0.05, **P < 0.01 using a one-way ANOVA with Newman–Keuls multiple comparison test.
Fig. 8.
ICL1–9-promoted cardiomyocyte contractility is dependent on the expression of the β2AR and β-arrestin. (A) β2AR-, β-arrestin1-, or β-arrestin2 knockout adult murine cardiomyocytes were isolated and assessed for basal and agonist-promoted contractility using a digital videocamera-coupled microscope in the presence or absence of 0.1% DMSO or 10 μM ICL1–9. Representative cell length (in micrometers) tracings at 2 Hz in the basal or stimulated state for each test condition are reported. (B) ICL1–9 was unable to promote significant contraction in β2AR- and β-arrestin1 knockout adult murine cardiomyocytes, and its ability to do so in β-arrestin2 knockout cardiomyocytes was significantly reduced. The data are represented by the mean ± SEM from six to seven cardiomyocytes from at least three independent primary isolations. ns, not significant, **P < 0.01, ***P < 0.001 using a one-way ANOVA with Newman–Keuls multiple comparison test.
Fig. S2.
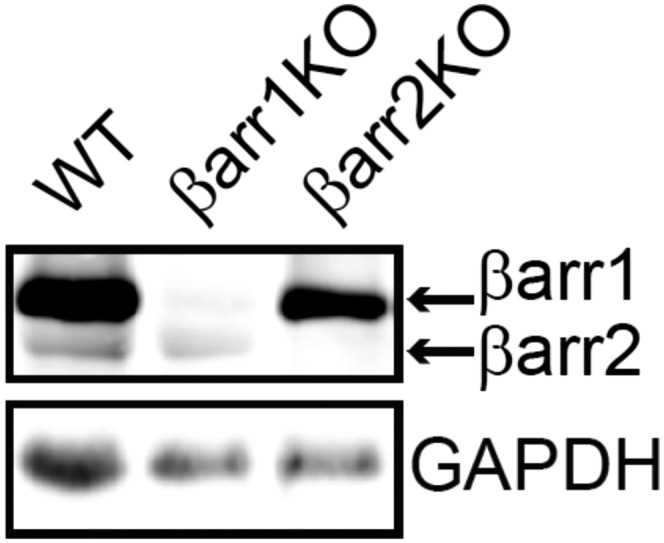
Immunoblotting of β-arrestins from whole heart lysates from WT, β-arrestin1, and β-arrestin2 knockout mice. Cardiac lysates from WT mice have higher expression of β-arrestin1 vs. β-arrestin2, whereas the respective knockout strains have a specific loss of either β-arrestin1 or β-arrestin2.
Discussion
In the initial screens of the β2AR pepducin library, it was clear that β-arrestin–biased pharmacology was evidenced primarily in pepducins derived from ICL1 sequences (5). Further characterization revealed ICL1–9 as a potent (EC50 of 96 nM) β-arrestin–biased pepducin that exhibits complete bias toward β-arrestin recruitment and signaling pathways over G-protein activation. ICL1–9 promoted a pharmacological profile consistent with a β-arrestin–biased agonist, such as carvedilol, including receptor phosphorylation, internalization, and β-arrestin–dependent signaling. Despite its similarity with carvedilol, ICL1–9 features three critical properties that carvedilol lacks. ICL1–9 operates independently of the orthosteric ligand-binding pocket; it demonstrates specificity among β-adrenergic receptor family members; and it can induce cardiomyocyte contraction. Conventional GPCR agonists, antagonists, and inverse agonists operate through binding the receptor orthosteric ligand-binding pocket and modulate the signaling propensity of the cognate receptor by influencing receptor conformational dynamics (agonist or inverse agonist) or simply competing for ligand binding (antagonist) (21). Carvedilol, for example, operates through interaction with the orthosteric ligand-binding pocket (evidenced by [125I]-iodocyanopindolol displacement) and is believed to stabilize a β-arrestin–biased receptor conformation that promotes β-arrestin–dependent processes and intracellular signaling (3). Similar analysis of ICL1–9 suggests that it operates independently of the orthosteric ligand-binding pocket to stimulate a signaling profile similar, yet not identical, to carvedilol. Although ICL1–9 does not influence receptor conformation in a conventional manner, it stabilizes a β2AR conformation that is both a substrate for GRK-mediated phosphorylation and β-arrestin binding. By monitoring β2AR–TM6 movement in vitro, ICL1–9 was observed to promote a significant conformational change in the β2AR as well as interactions between the β2AR and β-arrestin1 (WT and AAF). β-arrestin1–AAF is a mutant that lacks specific hydrophobic residues in the regulatory three-element region that creates a partially “preactivated” form of β-arrestin1 that does not require the typical prerequisite GRK-mediated receptor phosphorylation to couple to the β2AR (30). WT β-arrestin1 interaction, however, is enhanced by receptor phosphorylation and, thus, cannot couple to the β2AR as efficiently in this assay. Finally, β-arrestin recruitment was sensitive to the inverse agonist ICI-118551, which is believed to restrict receptor conformational dynamics. Although the particular conformational changes remain elusive, it is clear that ICL1–9 stabilizes a β-arrestin–biased β2AR conformation independent of the orthosteric ligand-binding site. This property provides the first opportunity to our knowledge to decouple β-arrestin–biased signaling from orthosteric site binding and may be a useful tool in studying the relative contribution of β-arrestin–dependent processes in the treatment of cardiovascular disease.
Pepducins are believed to operate through the cognate receptor in which they were derived, although there is a growing body of evidence that their specificity, especially among closely related family members, must be considered (5, 6, 12–14). ICL1–9 demonstrated complete specificity toward the β2AR compared with the β1AR, as ICL1–9 could not promote β-arrestin recruitment to the β1AR or β1AR internalization. Although both the β1AR and the β2AR are present in cardiomyocytes, in the normal heart, the β1AR is the dominant subtype with an ∼4:1 expression ratio between the two subtypes (39). However, in the failing heart, the β1AR is down-regulated at the protein and mRNA level leading to a loss of ∼50% of the β1AR, whereas β2AR expression remains unaltered (39, 40). Interestingly, each receptor subtype demonstrates distinct intracellular signaling pathways in the cardiomyocyte. Thus, in the failing heart, the changes in receptor subtype ratio can completely alter the intracellular signaling environment and regulatory cross-talk between the two pathways (34). As currently indicated CHF drugs are either β1AR-selective or nonselective agents, the β2AR may be an underappreciated therapeutic target. β1-selective pharmaceuticals, such as metoprolol and bisoprolol, are used in the treatment of CHF to inhibit the activation of cAMP-dependent, calmodulin-dependent kinase II (CaMKII)-mediated apoptosis observed with persistent stimulation of the β1AR (41). Activation of CaMKII, by complexing with β-arrestin1 and Epac, promoted agonist-dependent cardiac hypertrophy in vitro while also stimulating cardiac remodeling mechanisms in vivo (32, 33, 41, 42). This process is believed to be β1AR specific and not mediated through the β2AR (41). However, stimulation of the β2AR during CHF may also contribute to the pathophysiological advancement of the syndrome. Whereas β1AR levels are reduced in the failing heart, Gi, a hetrotrimeric G protein that has been shown to couple to the β2AR in the heart, is up-regulated (43, 44). Gi signaling reduces adenylyl cyclase activity and subsequent downstream inotropic responses critical for cardiac contraction while, in a Gβγ-dependent manner, promoting cell survival signaling such as Akt activation (45). The dichotomous nature of β2AR signaling in the failing heart suggests that conventional receptor activation may not be the best therapeutic approach.
As conventional activation of β-adrenergic receptors is unlikely to be a viable therapeutic approach to treat CHF, a more desirable pharmacological profile would promote inotropic effects while also stimulating cell survival pathways. Indeed, a β-arrestin–biased agonist of the AT1AR, TRV027, has been reported to promote cardiomyocyte contraction along with activation of antiapoptotic signaling (37, 38). To date, a comparable ligand has not been reported for β-adrenergic receptors. As the inotropic effects of TRV027 are proposed to operate through a β-arrestin–mediated pathway, it is possible that a β-arrestin–biased βAR agonist, such as carvedilol, would be able to promote similar effects. Interestingly, carvedilol was unable to promote murine cardiomyocyte contraction, whereas ICL1–9 promoted robust contraction. Carvedilol, biochemically characterized as a β-arrestin–biased agonist, can promote β-arrestin–mediated processes, such as receptor internalization, ERK activation, and EGFR transactivation, but failed at promoting cardiomyocyte contraction. This may stem from an inability of carvedilol to stimulate an unknown β-arrestin–dependent pathway through the β2AR linked to contraction or, alternatively, the ability of carvedilol to interact with both β1AR and β2AR may have contrasting effects on myocyte contraction. In contrast, ICL1–9 was able to stimulate a β2AR/β-arrestin complex that could both promote cell survival signaling pathways along with activation of cardiac inotropic effects. Although ICL1–9 does not promote cardiomyocyte contraction through traditional mechanisms (Fig. 7), it is possible that ICL1–9 couples β-arrestins to the myofilament proteins (as also proposed for TRV027). These mechanisms of calcium sensitization could operate through proteins that regulate the response to calcium, such as myosin-binding protein C or, more directly, troponin. Considering the ability to couple to the contractile machinery and prosurvival signaling pathways, ICL1–9 demonstrates that this potentially advantageous β-arrestin–biased conformation is accessible through the β2AR and should be targeted for the next generation of heart failure therapeutics.
Methods
cAMP Measurement.
HEK293 cells were cultured to confluency in 24-well plates at 37 °C in DMEM (Cellgro) supplemented with 10% (vol/vol) FBS and 50 μg/mL G418 sulfate (Cellgro). Cells were stimulated with 100 pM to 100 μM isoproterenol or ICL1–9 for 10 min at 37 °C in the presence of 0.5 mM 3-isobutyl-1-methylxanthine. Stimulation was ended by the removal of media on ice and cells were lysed by adding 80 μL 0.1 M HCl followed by a 20-min incubation at room temperature on an orbital shaker. Lysates were cleared by centrifugation at 1,000 × g for 15 min. cAMP levels were measured using the Cayman Chemical cAMP EIA kit according to the manufacturer’s instructions.
β-Arrestin2 Recruitment Using BRET.
β-arrestin2 recruitment to the β2AR was measured as previously described (5). In brief, HEK293 cells coexpressing β-arrestin2–GFP10 (energy acceptor) and β2AR–RLucII (energy donor) were stimulated with 100 pM to 100 μM isoproterenol or ICL1–9 in the presence of 2.5 μM coelenterazine 400a. BRET was monitored over the course of 24 min using a Tecan Infinite F500 microplate reader. BRET ratios were calculated as the light intensity emitted by GFP10 at 510 nm divided by the light emitted by the donor RLucII at 400 nm. The background of unstimulated trials was subtracted from the BRET measured from the stimulated trials to report ΔBRET.
β-Arrestin2 recruitment to CXCR4 was measured similarly in HEK293 cells stably overexpressing a FLAG–β2AR and transiently transfected with β-arrestin2–GFP10 and CXCR4–RLucII (15). BRET was monitored poststimulation using 50 nM SDF-1α, 1 μM isoproterenol, or 10 μM ICL1–9.
Detection of β2AR Phosphorylation Using Phosphospecific Antibodies.
HEK293 cells stably overexpressing FLAG–β2AR were grown in 10-cm dishes at 37 °C in DMEM supplemented with 10% (vol/vol) FBS and 50 μg/mL G418 sulfate (Cellgro). Cells were stimulated with 1 μM isoproterenol, 10 μM carvedilol, or 10 μM ICL1–9 for 0–60 min at 37 °C and the cells were washed, lysed, and then analyzed for β2AR phosphorylation at Ser355 and Ser356 as previously described (5). Briefly, cell lysates were immunoprecipitated using mouse monoclonal M2 anti-FLAG (Sigma-Aldrich) and Protein G agarose PLUS beads (Santa Cruz Biotechnologies). The beads were incubated overnight at 4 °C, pelleted, washed, and then suspended in Laemeli buffer. Immunoprecipitated proteins were separated by SDS/PAGE and receptor phosphorylation was analyzed by Western blotting using a phosphospecific antibody (1:500) against β2AR phospho-Ser355/356 (Santa Cruz Biotechnologies). Chemiluminescence was measured using Pico chemiluminescent substrate (Thermo Scientific).
β-Adrenergic Receptor Internalization by Cell Surface ELISA.
Receptor internalization was measured by cell surface ELISA as previously described (46).
β1AR/β-Arrestin2 Interaction Measurements by FRET.
Human osteosarcoma (U2S) cells were seeded on fibronectin (10 µg/mL)-coated glass coverslips in 35-mm dishes in MEM containing 10% (vol/vol) FBS and 1% penicillin/streptomycin/amphotericin B and infected with adenoviral constructs for Flag–β1AR–mCFP [multiplicity of infection (MOI), 60] and Ad–βarrestin2–mYFP (MOI, 200). Twenty-four hours following infection, cells were rinsed and media replaced with imaging buffer (HBSS supplemented with 0.2% BSA and 20 mM Hepes) 10 min before imaging using a Leica DMI4000B inverted microscope with a Leica DFC365 FX 1.4-megapixel monochrome digital camera. CFP (433/475 nm), YFP (514/527 nm), and FRET (433/527 nm) excitation and emission wavelengths were measured every 3.5 s. After 30 s of baseline reads the cells were stimulated with isoproterenol (1 µM) or ICL1–9 (10 µM) and whole field-of-view measurements at 20× magnification were used to assess changes in FRET. Quantification of the changes in FRET (corrected FRET = FRET − (CFP*CFP bleedthrough [36%]) − (YFP*YFP bleedthrough [13%]) were expressed as a percentage of total CFP emission (%FRET = cFRET/[cFRET + CFP]).
Detection of ERK Phosphorylation and EGFR Transactivation.
HEK293 cells stably overexpressing FLAG–β2AR were grown to ∼90% confluence in six-well plates and serum starved for 16 h. Cells were stimulated with 10 μM carvedilol or 10 μM ICL1–9 over a 1-h time course at 37 °C in 0.05% DMSO in nonpepducin trials. On ice, assay media was removed and 100 μL of lysis buffer was added. Cell lysates were scraped and briefly sonicated. A total of 20 μL of 6× Laemmli buffer was added and the lysate was boiled for 10 min. ERK phosphorylation was detected by Western blotting using a polyclonal primary antibody against phospho-ERK1/2 (1:500 in TBST with 5% (wt/vol) BSA; Cell Signaling Technologies) and total ERK2 levels were detected using a monoclonal anti-ERK2 antibody (1:1,000 in TBST with 5% (wt/vol) BSA; Santa Cruz Biotechnologies). ERK phosphorylation levels (normalized to ERK2) were quantitated by detection of anti-mouse IRDye 800 and anti-rabbit IRDye 680 antibodies using a LiCOR Odyssey system.
siRNA Knockdown of β-Arrestin1 and 2.
HEK293 cells stably overexpressing FLAG–β2AR were grown to ∼90% confluence in 10-cm dishes and transfected with siRNA constructs using Lipofectamine 2000 per manufacturer’s protocol with 600 pM siRNA per dish. Cells were lifted and plated into 12-well plates 48 h posttransfection. ERK phosphorylation was detected as described above.
[125I]-Iodocyanopindolol Binding.
HEK293 cells stably expressing a FLAG–β2AR were isolated and washed three times with assay buffer (HBSS with calcium and magnesium, 0.1% BSA, pH 7.4), diluted to 25,000 cells per milliliter, and incubated with 1 nM [125I]-iodocyanopindolol in the presence or absence of pepducin or carvedilol for 2 h at 25 °C. Incubations were terminated by rapid filtration on GF/B filters. Filters were washed four times with 5 mL of cold assay buffer and [125I]-iodocyanopindolol binding was quantitated by γ-emission counting.
β-Arrestin Coupling Assessed by Monobromobimane Fluorescence.
Full-length PN1–β2AR was purified from Sf9 insect cells and labeled with monobromobimane as previously described (47). Monobromobimane-labeled β2AR was reconstituted in 2% (wt/vol) DOPC/CHAPSO (3:1) with 1.13 mM CHS lipid bicelles by incubating for 30 min on ice. Lipid bicelles containing 50 nM mbb–β2AR were incubated for 15 min at 25 °C in 20 mM Hepes, pH 7.5, 100 mM NaCl with 100 nM isoproterenol, or 10 μM ICL1–9. In experiments using β-arrestin1, 50 nM WT β-arrestin1 or β-arrestin1–AAF was incubated for 10 min at 25 °C alone or postagonist addition, depending on experimental set-up. mbb–β2AR fluorescence was measured by excitation at 370 nm and recording emission from 430 to 510 nm at 1 nm increments with 1 nm⋅s−1 integration on a Photon Technology International fluorescence spectrophotometer set at a 2-mm excitation and emission bandwidth pass. Background fluorescence contributed by the assay buffer and ligand was subtracted from the experimental spectra.
Isolation of Adult Murine Cardiac Myocytes, Contractility, and Ca2+ Measurements.
Adult murine cardiac myocytes were isolated from the septum and left ventricular free wall of 8- to 12-wk-old mice as previously described (48). Briefly, mice were heparinized (1,500 units/kg i.p.) and anesthetized (pentobarbital sodium, 50 mg/kg i.p.). Excised hearts were mounted on a steel cannula and retrograde perfused (100 cm H2O, 37 °C) with Ca2+-free bicarbonate buffer followed by enzymatic digestion (collagenases B and D, protease XIV). Isolated myocytes were plated on laminin-coated glass coverslips, and the Ca2+ concentration of the buffer was incrementally increased (0.05, 0.125, 0.25, and 0.5 mM) with 10 min of exposure at each concentration. The final Ca2+ buffer was then aspirated and replaced with MEM (Sigma-Aldrich) containing 1.2 mM Ca2+, 2.5% (vol/vol) FBS, and 1% penicillin/streptomycin. The pH was adjusted to 7.0 in 4% CO2 by the addition of NaHCO3 (0.57 g/L). After 1 h (4% CO2, 37 °C), media were replaced with FBS-free MEM containing 0.1 mg/mL BSA and antibiotics. Myocytes adherent to coverslips were bathed in 0.7 mL of air and temperature equilibrated (37 °C), Hepes-buffered (20 mM, pH 7.4) medium 199 containing 1.8 mM [Ca2+], and used within 2–8 h of isolation. For Ca2+ transient measurements, cardiomyocytes were exposed to 0.67 µM Fura 2-AM for 15 min at 37 °C. Measurements of myocyte contraction and Ca2+ transients at a pacing frequency of 2 Hz were performed in the presence of vehicle (0.1% DMSO), isoproterenol (0.5 µM), ICL1–9 (10 µM), control pepducin (10 µM), or carvedilol (10 µM) as described. All animal procedures were performed in accordance with the Institutional Animal Care and Use Committee at Temple University and in accordance to the NIH Guidelines on the Use of Laboratory Animals.
Detection of β-Arrestin Expression and Phospholamban Phosphorylation.
Isolated cardiomyocytes (prepared as described above) were stimulated with 0.1% DMSO, 0.1 µM isoproterenol, or 10 µM ICL1–9 for 5 min. On ice, assay media were removed and 100 μL of lysis buffer was added, cells were scraped and or nutated at 4 °C for 30 min. A total of 20 μL of 6× Laemeli buffer was added and the lysate was boiled for 10 min. Left ventricular samples were homogenized in lysis buffer containing 20 mM Tris⋅HCl, pH 7.4, 137 mM NaCl, 10% (vol/vol) glycerol, 1 mM EDTA, 1% Nonidet P-40, 10 mM NaF (Fisher Scientific), 1× HALT protease inhibitor mixture (Thermo Scientific), and phosphatase inhibitor mixture set IV (Calbiochem). Lysates were run on 8% SDS/PAGE gels and transferred to Immobilon-PSQ polyvinylidene fluoride 0.2-mm pore size membranes (Millipore). PLB phosphorylation (cardiomyocyte lysates) was detected using anti-Phospho-Ser16 PLB rabbit pAb (1:5,000; Badrilla) and normalized to total PLB as detected with anti-PLB mouse mAb (1:1,000; Badrilla). β-Arrestin1 and 2 expression levels (left ventricular lysates) were detected using anti–β-arrestin1/2 rabbit mAb (1:1,000, Cell Signaling Technology) and normalized to GAPDH levels as detected with anti-GAPDH rabbit mAb (1:1,000; Cell Signaling Technology). Membranes were subsequently incubated with appropriate anti-rabbit or anti-mouse IRDye (680 or 800)-labeled antibodies and detected using the LiCOR Biosciences Odyssey system.
Acknowledgments
The authors thank Drs. Charles Scott, Raymond Penn, and Brian Kobilka for valuable discussions; Dr. Michel Bouvier for the BRET constructs; and Dr. Mark von Zastrow for the HEK293 cells stably overexpressing FLAG–β2AR. This research was supported by NIH Awards R37-GM047417, R01-GM068857, and P01-HL114471 (to J.L.B.); R01-HL105414 (to D.G.T.); R01-HL074854 (to J.Y.C.); P01-HL075443 and P01-HL091799 (to W.J.K.); and T32-GM100836 (to R.L.C.).
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1606267113/-/DCSupplemental.
References
- 1.Javed U, Deedwania PC. Beta-adrenergic blockers for chronic heart failure. Cardiol Rev. 2009;17(6):287–292. doi: 10.1097/CRD.0b013e3181bdf63e. [DOI] [PubMed] [Google Scholar]
- 2.Ramani GV, Uber PA, Mehra MR. Chronic heart failure: Contemporary diagnosis and management. Mayo Clin Proc. 2010;85(2):180–195. doi: 10.4065/mcp.2009.0494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wisler JW, et al. A unique mechanism of beta-blocker action: Carvedilol stimulates beta-arrestin signaling. Proc Natl Acad Sci USA. 2007;104(42):16657–16662. doi: 10.1073/pnas.0707936104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Erickson CE, et al. The β-blocker nebivolol is a GRK/β-arrestin biased agonist. PLoS One. 2013;8(8):e71980. doi: 10.1371/journal.pone.0071980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carr R, 3rd, et al. Development and characterization of pepducins as Gs-biased allosteric agonists. J Biol Chem. 2014;289(52):35668–35684. doi: 10.1074/jbc.M114.618819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Callaghan K, Kuliopulos A, Covic L. Turning receptors on and off with intracellular pepducins: New insights into G-protein-coupled receptor drug development. J Biol Chem. 2012;287(16):12787–12796. doi: 10.1074/jbc.R112.355461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lefkowitz RJ. Seven transmembrane receptors: Something old, something new. Acta Physiol (Oxf) 2007;190(1):9–19. doi: 10.1111/j.1365-201X.2007.01693.x. [DOI] [PubMed] [Google Scholar]
- 8.Tran TM, et al. Characterization of agonist stimulation of cAMP-dependent protein kinase and G protein-coupled receptor kinase phosphorylation of the beta2-adrenergic receptor using phosphoserine-specific antibodies. Mol Pharmacol. 2004;65(1):196–206. doi: 10.1124/mol.65.1.196. [DOI] [PubMed] [Google Scholar]
- 9.Vaughan DJ, et al. Role of the G protein-coupled receptor kinase site serine cluster in beta2-adrenergic receptor internalization, desensitization, and beta-arrestin translocation. J Biol Chem. 2006;281(11):7684–7692. doi: 10.1074/jbc.M500328200. [DOI] [PubMed] [Google Scholar]
- 10.Nobles KN, et al. Distinct phosphorylation sites on the β(2)-adrenergic receptor establish a barcode that encodes differential functions of β-arrestin. Sci Signal. 2011;4(185):ra51. doi: 10.1126/scisignal.2001707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kang DS, Tian X, Benovic JL. Role of β-arrestins and arrestin domain-containing proteins in G protein-coupled receptor trafficking. Curr Opin Cell Biol. 2014;27:63–71. doi: 10.1016/j.ceb.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Covic L, Misra M, Badar J, Singh C, Kuliopulos A. Pepducin-based intervention of thrombin-receptor signaling and systemic platelet activation. Nat Med. 2002;8(10):1161–1165. doi: 10.1038/nm760. [DOI] [PubMed] [Google Scholar]
- 13.Stampfuss JJ, Schrör K, Weber AA. Inhibition of platelet thromboxane receptor function by a thrombin receptor-targeted pepducin. Nat Med. 2003;9(12):1447, author reply 1447–1448. doi: 10.1038/nm1203-1447a. [DOI] [PubMed] [Google Scholar]
- 14.Winther M, Gabl M, Welin A, Dahlgren C, Forsman H. A neutrophil inhibitory pepducin derived from FPR1 expected to target FPR1 signaling hijacks the closely related FPR2 instead. FEBS Lett. 2015;589(15):1832–1839. doi: 10.1016/j.febslet.2015.05.050. [DOI] [PubMed] [Google Scholar]
- 15.Quoyer J, et al. Pepducin targeting the C-X-C chemokine receptor type 4 acts as a biased agonist favoring activation of the inhibitory G protein. Proc Natl Acad Sci USA. 2013;110(52):E5088–E5097. doi: 10.1073/pnas.1312515110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeWire SM, Ahn S, Lefkowitz RJ, Shenoy SK. Beta-arrestins and cell signaling. Annu Rev Physiol. 2007;69:483–510. doi: 10.1146/annurev.physiol.69.022405.154749. [DOI] [PubMed] [Google Scholar]
- 17.Patel PA, Tilley DG, Rockman HA. Beta-arrestin-mediated signaling in the heart. Circ J. 2008;72(11):1725–1729. doi: 10.1253/circj.cj-08-0734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shenoy SK, et al. β-arrestin-dependent, G protein-independent ERK1/2 activation by the β2 adrenergic receptor. J Biol Chem. 2006;281(2):1261–1273. doi: 10.1074/jbc.M506576200. [DOI] [PubMed] [Google Scholar]
- 19.Noma T, et al. Beta-arrestin-mediated beta1-adrenergic receptor transactivation of the EGFR confers cardioprotection. J Clin Invest. 2007;117(9):2445–2458. doi: 10.1172/JCI31901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim IM, et al. Beta-blockers alprenolol and carvedilol stimulate beta-arrestin-mediated EGFR transactivation. Proc Natl Acad Sci USA. 2008;105(38):14555–14560. doi: 10.1073/pnas.0804745105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luttrell LM. Minireview: More than just a hammer: Ligand “bias” and pharmaceutical discovery. Mol Endocrinol. 2014;28(3):281–294. doi: 10.1210/me.2013-1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chidiac P, Hebert TE, Valiquette M, Dennis M, Bouvier M. Inverse agonist activity of beta-adrenergic antagonists. Mol Pharmacol. 1994;45(3):490–499. [PubMed] [Google Scholar]
- 23.Samama P, Pei G, Costa T, Cotecchia S, Lefkowitz RJ. Negative antagonists promote an inactive conformation of the beta 2-adrenergic receptor. Mol Pharmacol. 1994;45(3):390–394. [PubMed] [Google Scholar]
- 24.Kang Y, et al. Crystal structure of rhodopsin bound to arrestin by femtosecond X-ray laser. Nature. 2015;523(7562):561–567. doi: 10.1038/nature14656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Szczepek M, et al. Crystal structure of a common GPCR-binding interface for G protein and arrestin. Nat Commun. 2014;5:4801. doi: 10.1038/ncomms5801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shukla AK, et al. Visualization of arrestin recruitment by a G-protein-coupled receptor. Nature. 2014;512(7513):218–222. doi: 10.1038/nature13430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rasmussen SG, et al. Crystal structure of the β2 adrenergic receptor-Gs protein complex. Nature. 2011;477(7366):549–555. doi: 10.1038/nature10361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yao X, et al. Coupling ligand structure to specific conformational switches in the beta2-adrenoceptor. Nat Chem Biol. 2006;2(8):417–422. doi: 10.1038/nchembio801. [DOI] [PubMed] [Google Scholar]
- 29.Yao XJ, et al. The effect of ligand efficacy on the formation and stability of a GPCR-G protein complex. Proc Natl Acad Sci USA. 2009;106(23):9501–9506. doi: 10.1073/pnas.0811437106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Burtey A, et al. The conserved isoleucine-valine-phenylalanine motif couples activation state and endocytic functions of beta-arrestins. Traffic. 2007;8(7):914–931. doi: 10.1111/j.1600-0854.2007.00578.x. [DOI] [PubMed] [Google Scholar]
- 31.Zhu WZ, et al. Linkage of beta1-adrenergic stimulation to apoptotic heart cell death through protein kinase A-independent activation of Ca2+/calmodulin kinase II. J Clin Invest. 2003;111(5):617–625. doi: 10.1172/JCI16326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bisognano JD, et al. Myocardial-directed overexpression of the human beta(1)-adrenergic receptor in transgenic mice. J Mol Cell Cardiol. 2000;32(5):817–830. doi: 10.1006/jmcc.2000.1123. [DOI] [PubMed] [Google Scholar]
- 33.Engelhardt S, Hein L, Wiesmann F, Lohse MJ. Progressive hypertrophy and heart failure in beta1-adrenergic receptor transgenic mice. Proc Natl Acad Sci USA. 1999;96(12):7059–7064. doi: 10.1073/pnas.96.12.7059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Woo AY, Xiao RP. β-Adrenergic receptor subtype signaling in heart: From bench to bedside. Acta Pharmacol Sin. 2012;33(3):335–341. doi: 10.1038/aps.2011.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wei H, et al. Independent beta-arrestin 2 and G protein-mediated pathways for angiotensin II activation of extracellular signal-regulated kinases 1 and 2. Proc Natl Acad Sci USA. 2003;100(19):10782–10787. doi: 10.1073/pnas.1834556100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rajagopal K, et al. Beta-arrestin2-mediated inotropic effects of the angiotensin II type 1A receptor in isolated cardiac myocytes. Proc Natl Acad Sci USA. 2006;103(44):16284–16289. doi: 10.1073/pnas.0607583103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Violin JD, et al. Selectively engaging β-arrestins at the angiotensin II type 1 receptor reduces blood pressure and increases cardiac performance. J Pharmacol Exp Ther. 2010;335(3):572–579. doi: 10.1124/jpet.110.173005. [DOI] [PubMed] [Google Scholar]
- 38.Boerrigter G, et al. Cardiorenal actions of TRV120027, a novel ß-arrestin-biased ligand at the angiotensin II type I receptor, in healthy and heart failure canines: A novel therapeutic strategy for acute heart failure. Circ Heart Fail. 2011;4(6):770–778. doi: 10.1161/CIRCHEARTFAILURE.111.962571. [DOI] [PubMed] [Google Scholar]
- 39.Bristow MR, et al. Beta 1- and beta 2-adrenergic-receptor subpopulations in nonfailing and failing human ventricular myocardium: Coupling of both receptor subtypes to muscle contraction and selective beta 1-receptor down-regulation in heart failure. Circ Res. 1986;59(3):297–309. doi: 10.1161/01.res.59.3.297. [DOI] [PubMed] [Google Scholar]
- 40.Bristow MR, et al. Reduced beta 1 receptor messenger RNA abundance in the failing human heart. J Clin Invest. 1993;92(6):2737–2745. doi: 10.1172/JCI116891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mangmool S, Shukla AK, Rockman HA. beta-Arrestin-dependent activation of Ca(2+)/calmodulin kinase II after beta(1)-adrenergic receptor stimulation. J Cell Biol. 2010;189(3):573–587. doi: 10.1083/jcb.200911047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sucharov CC, et al. A beta1-adrenergic receptor CaM kinase II-dependent pathway mediates cardiac myocyte fetal gene induction. Am J Physiol Heart Circ Physiol. 2006;291(3):H1299–H1308. doi: 10.1152/ajpheart.00017.2006. [DOI] [PubMed] [Google Scholar]
- 43.Böhm M, et al. Radioimmunochemical quantification of Gi alpha in right and left ventricles from patients with ischaemic and dilated cardiomyopathy and predominant left ventricular failure. J Mol Cell Cardiol. 1994;26(2):133–149. doi: 10.1006/jmcc.1994.1017. [DOI] [PubMed] [Google Scholar]
- 44.Feldman AM, et al. Increase of the 40,000-mol wt pertussis toxin substrate (G protein) in the failing human heart. J Clin Invest. 1988;82(1):189–197. doi: 10.1172/JCI113569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhu WZ, et al. Dual modulation of cell survival and cell death by beta(2)-adrenergic signaling in adult mouse cardiac myocytes. Proc Natl Acad Sci USA. 2001;98(4):1607–1612. doi: 10.1073/pnas.98.4.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Daunt DA, et al. Subtype-specific intracellular trafficking of alpha2-adrenergic receptors. Mol Pharmacol. 1997;51(5):711–720. doi: 10.1124/mol.51.5.711. [DOI] [PubMed] [Google Scholar]
- 47.Rosenbaum DM, et al. GPCR engineering yields high-resolution structural insights into beta2-adrenergic receptor function. Science. 2007;318(5854):1266–1273. doi: 10.1126/science.1150609. [DOI] [PubMed] [Google Scholar]
- 48.Wang J, et al. Regulation of in vivo cardiac contractility by phospholemman: Role of Na+/Ca2+ exchange. Am J Physiol Heart Circ Physiol. 2011;300(3):H859–H868. doi: 10.1152/ajpheart.00894.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]