Abstract
Introduction
Self-medication is an increasingly growing health problem, which has many adverse effects on human and the cost used in the production of medications.
Aim
The current study was conducted to estimate the prevalence of self-medication among student of Kermanshah University of Medical Sciences in 2014.
Materials and Methods
In a descriptive-cross-sectional study, 364 students of Kermanshah University of Medical Sciences were recruited through stratified random sampling method. Data collection was done by researcher-made questionnaire, entered to SPSS22 software and analysed by descriptive and inferential statistics.
Results
Of the 364 students, prevalence of self-medication was 123 (33.7%) the mean age was 21.63±1.92, among them 64.2% took the medication from the pharmacy and 34.95% have faced complications of self-medication. The main cause of self-medication among students were the history of a disease of taking medication (44.71%), deemed no importance of the disease (34.95%), and easy accessibility of the medication (20.32%).
Conclusion
With regard to the high prevalence of self-medication among the students, it is suggested to provide educational programs on the adverse effects of self-medication, and appropriate measures to control and prevent easy access to the medications.
Keywords: Complications, Drug resistance, Prescription drug overuse
Introduction
Despite various initiatives and policies, now-a-days, aberrant use of medication, particularly intractable consumption, has been considered as a national health dilemma with negative effects on a community in term of socio-economic development and health promotion [1]. Self-Medication (SM) is a medical behaviour of individuals, which is often common for subsiding the primary symptoms of diseases as the first choice [2]. It is defined as the use of medications by self, out of the consultation or prescription of a physician. In this way, the diagnosing, prescription and caring were done by own individual [3]. Now-a-days, SM and uncontrolled use of medication are remarked as the main problem in all nations. It is reported that there is a mismatch between consumption and prescription of medication in Iran, this is the reason for takeing this topic [4]. SM increases the likelihood of outlawing use of medications and drug abuse. Moreover, it causes the symptoms of the diseases to be concealed, so this increases the probability of the severity of disease and drug resistance as well as the delay in diagnosing measures [3]. Unfortunately, the social vision to medications is just on the healing aspects, while it is supposed to be a double-edged blade in the medical literature, one edge to treatment and another invades the human because of unawareness to the right use of them [5]. The researchers believe that there are no drugs without complications, while the discriminate use of them duplicates the side effects so that the SM endangers a drug resistance, consequently the treatments of the associated unwanted complications and poisoning will be ignored [6]. The medications effects various systems of the body causing osteoporosis, poisoning, gastrointestinal ulcers, and renal and liver failures. Accordingly the inquiries attributed, 30% of liver and renal defects and 3% of hospitalizations in USA due to misuse of medication [7]. It was estimated that SM was seen in 40.5% students of medicine dentistry 20.3%, pharmacy 31.1%, health education 25%, hygiene 41.2%, nursing 32.1%, midwifery 29.4%, and economic and management 50% [8]. SM is affected by some factors such as symptomatic treatment of the disease, considering the disease as non-important, and the high cost of the doctor visit. Moreover, some other socioeconomic reasons such as education level, profession, and location may facilitate the SM [1]. Overall, the causes of the SM could be included to the disease history, factors like easy access of drug, providing the medications from a pharmacy without prescription, considering the disease is non-important, having no enough time to refer to a physician and take an appropriate result from that, these factors restrain the referring to the doctor as well [8–10]. Antibiotics (68%), cold tablets (64%), Iron tablets (57%) and the tranquilizers (54%) are the most common drugs used as the SM [6]. The students mostly use antibiotics, common cold drugs, sedatives, and antiemetic as SM [8,9]. In this regards, overall the antibiotics, sedative and herbal medicine are commonly used drugs in the community [11].
Due to the false beliefs and attitude related to the medical components [12] and regarding the growing of the SM phenomenon, its negative consequences, direct role of the individuals in choosing and consuming the drugs and the cost for medications production, SM is an important issue in community, therefore, for reducing the adverse effects of this problem, it must be scrutinized widely. Whilst, due to the social level, and being a proper role model to other people in the society, medical students should be investigated to SM. In addition, to establish the appropriate measures for decreasing the prevalence of SM, the risk factors, and its prevalence should be elucidated. With respect to a lack of information in this issue in Iranian students, the current study was conducted to determine the prevalence of SM and associated factors from students of Kermanshah University of Medical Sciences (KUMS) in 2014.
Materials and Methods
This study was done as descriptive-cross-sectional in 2014; the population was all the students of KUMS. The sample was 364 individuals were recruited through stratified random sampling method. Sample size estimated based on the prevalence (0.4) of SM of Ghafouri et al., study and following statistic formula [13].
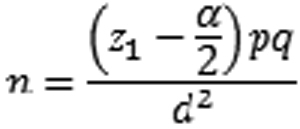 |
The questionnaire designed was based on the literature and validated by Pour Reza et al., study [8]. In our study validity was determined as content validity by consulting to the faculties in medical, instrumentation, and nursing. For determining the reliability, Cronbach’s alpha was measured as 0.83. The tool consisted of the 16 questions, including demographic characteristics, economic status, the class of drugs, the contributing factors of SM, the rate of information to the drugs, the ways of achieving the information and the cost expended to the SM.
This study was approved by ethical committee of research deputy of KUMS with number 94393. The purpose of the study was explained to the subjects and were assured about the anonymity and confidentiality of their personal information. The questionnaire was offered to the students after obtaining the informed consent form.
Statistical Analysis
Data was entered to SPSS 22 and analysed by descriptive and inferential statistics (chi-squares) statistics. The significant level for the tests was 0.05.
Results
Of the 364 students participated in the study, 66.5% were female, the mean and Standard Deviation (SD) of age was 21.63± 1.92 years. The students studied in pharmacology (42 people, 11.5%), nutrition (33, 9.1%), medical (41, 11.3%), hygiene (52, 14.3%), nursing (42, 11.5%), midwifery (50, 13.7%), laboratory (33, 9.1%), anaesthesiology (30, 8.2%), operating room (25, 6.9%), and emergency (16, 4.4%). The education levels were un-continued bachelor (BSC) (4.7%), continued BSC (72.5%), and professional doctorate (PhD) (22.8%). Most of the students (194 people, 53.3%) inhabited in the Kermanshah city, more of the education level of the father of the subjects (123, 36.3%) were university and to the mother (114, 31.3%) diploma. The health assurance of the participants was 25.5% health service, 34.9% social protection, 15.4% military forces, 6% rural, 6.6% other, and 11.5% had no assurances. More than 90% of the students were married and about 10% single.
From the 364 students, 185 (50.8%) did not confront to any physical or psychological illness within a month. Of the remained 179 persons, 56 had referred to a physician, 112 individuals have experienced the SM and 11 acted both, the referring to physician and SM. In general, SM rate and referring to the physician were 33.7% (123 individuals) and 18.4% (67 individuals) respectively. From referred to the physician (67 individuals), just 47 (12.9%) people fully consumed the medications.
The class of drugs commonly used for SM were related to common cold medications (52.84%) and the analgesics (49.59%) e.g. diclofenac, acetaminophen, and Ibuprofen, while the heart and the opioids (eg-codeine and tramadol) drugs were less prevalent (5.7% each one) [Table/Fig-1]. The history of the disease (44.71%) and deemed no importance of the disease (34.95%) were the common contributing factors for SM [Table/Fig-2]. Females (36.3%) were more at risk to SM than male (28.7%) significantly by chi-squares test (p<0.05). The students declared the fever and headache (43.8%), and common cold were the main Health problems which lead to SM, but the skin disorders was reported frequently (4.87%) [Table/Fig-3]. The main source of SM was the pharmacy [Table/Fig-4] and about 60% of the students expensed a cost between 10000-50000 Rials a month to it.
[Table/Fig-1]:
Classes of Drugs Commonly used for self-medication.
| Used drugs | Frequency (%) |
|---|---|
| Common cold tablet and syrups | 65 (52.84) |
| Analgesics | 61 (49.59) |
| Antibiotics | 51 (41.46) |
| Vitamins and nutritional complements | 40 (32.52) |
| Gastrointestinal drugs | 34 (27.64) |
| Anti-allergic | 26 (21.13) |
| Herbal components | 25 (20.32) |
| Psychoactive | 24 (19.51) |
| Skin | 19 (15.44) |
| Anti-parasite | 10 (8.13) |
| Opioids | 7 (5.7) |
| Cardiovascular | 7 (5.7) |
[Table/Fig-2]:
Factors contributing for self-medication.
| Factors contributing for SM | Incidence (%) |
|---|---|
| History of the disease | 55 (44.71) |
| deemed no importance of the disease | 43 (34.95) |
| easy accessibility of the medication | 25 (20.32) |
| High cost of the physicians visits | 19 (15.44) |
| Unbeloved to the physicians | 13 (10.56) |
| affected by the friends and relatives | 10 (8.13) |
| Having no assurance | 0 (0.0) |
| Other | 1 (0.81) |
[Table/Fig-3]:
Health problems which lead to self-medications.
| Health problems | Incidence (%) |
|---|---|
| Fever and headache | 53 (43.08) |
| Cold | 52 (42.27) |
| Gastrointestinal disorders | 27 (21.95) |
| Respiratory problems | 21 (17.07) |
| Allergy | 19 (15.44) |
| Psychological problems | 13 (10.56) |
| Skin diseases | 6 (4.87) |
| Other | 2 (1.62) |
[Table/Fig-4]:
Sources of medication for self-medication.
| Sources of medication | Frequency (%) |
|---|---|
| Pharmacy | 79 (64.2) |
| Previous prescription | 33 (26.8) |
| Friends | 18 (14.6) |
From the self-medicated students, 43 people (34.95%) were faced complication consequently, the side effects mostly were associated to Antibiotic medications, whereas psychoactive, narcotic drugs had the lowest complications. The students received the drug information from their colleges (50%), the internet (39.3%), the therapeutic centers such as the hospitals (29.4%), friends (22%), scientific journals (20.6%), non-scientific journals (1.4%) and drug brochures (0.5%).
The SM rate amongst the students in term of the educational field was the pharmacology equal to 40.5%, nutrition 36.3%, medical 26.8%, hygiene 34.6%, nursing 31%, midwifery 32%, laboratory science 48.5%, anaesthesiology 30%, operating room 32% and medicine emergency 18.8%.
Discussion
In this study, the SM incidence amongst the students of the KUMS was estimated as 33.7%. This rate varied in different target groups, and was demonstrated between16%-83% in Iran [1]; accordingly, a systematic review study (2015) estimated, the SM prevalence of 67% to Iranian students [4]. In Badiger et al., study, 92% of medical students reported SM during one year [14] and Sarahroordi et al., concluded more than 76% of Iranian students have carried out SM during three months [15]. In other assessment conducted by Patel et al., 88% of the students took action to SM [3], moreover 83% of the Ardabil university students had experienced the SM too [16]. These results are higher than our study. But comply with the current study, in an assessment in Tehran, the SM rate was seen to 35.7% [8]. The low rate of the SM in this study could be reasoned to having a knowledge base of the students to some drug components such as pain relievers, antibiotics, and common cold tablets and syrups, moreover lower knowledge to other drugs such as psychoactive, narcotics, and cardiovascular medications.
The results showed the drugs commonly used for SM were the common cold, cough suppressants, analgesics and antibiotics, but the lowest rate was linked to the narcotics (e.g. codeine and tramadol), and cardiac drugs. This could be related to the needs to the drugs in this age range, the possible availability of the drugs and selling without description by the pharmacies. In the study conducted by Jalilian et al., analgesics, cough suppressants, antibiotics, and common cold drugs had high consumption to SM [17]. While, the antipyretics and analgesic were more common in Indian medical students [14]. According to the study by Banerjee et al., west of Bengal, antibiotics, pain relievers, and antipyretics were commonly used for SM [18]. Castle et al., carried out an investigation to SM on six countries in Latin America in 1996, and concluded that analgesics, antibiotics, steroid components, cardiovascular and Central Nerve System (CNS) agents more prevalent to SM [19].
According to the results, the female students had more at risk to SM and its incidence was estimated about 36%, this rate was 28% in men. Akici et al., also reportded that SM was more in female than male substantially [20]. Because the influence of some unhealthy behaviours, the likelihood of SM was greater in female in Spain [21]. Other investigation in Slovenia by Smogavec et al., concluded sex and age were the disposing factors and so that the female have more prevalence of SM [22]. Because of being sensitive to diseases and having special femininity problems [23], it appears the high prevalence of SM in woman students is justifiable.
In this study, the factors contributing to SM were “History of the disease”, “deemed no importance of the disease”, “accessibility of the medicines” and “the high cost of the physicians visit” respectively. Coincide with our results, Azami-Aghdash et al., concluded the reasons to SM in Iran are mostly mild symptoms of a disease, self-diagnosis of disease symptoms, previous use of medication, and ease of access to non-prescribed medication [4]. Accordingly, in the study by Pour Reza et al., the factors such as “former experience to the disease”, “accessibility of the drugs” and “assuming to no importance of disease” have been presented [8]. Gutema et al., also declared the SM is related to two reasons including an experience of the disease and having mild symptoms [24]. The most commonly factors to SM expressed by Yousef et al., included “having minor signs and no need to a physician”, “long waiting time at the doctor’s office”, and “avoiding pay the doctor’s visit” [25].
In our study, the common health problems which lead to SM by the students were fever and headache (43.8%), common cold (42.27%), and gastrointestinal disorders (21.95%). Comply with us, in the study conducted by Kumar et al., and Badiger et al., studies, fever, common cold and headache were mentioned as the main diseases of students to SM [14,26], in the study in 2014, SM was used for the health problems such as coughing, cold, diarrhea, fever, headache, heartburn and gastric ulcer [18]. And other investigation by Gutema et al., revealed that a headache and cold are two main purpose of SM [24]. It appears some diseases such as common cold, which created mild symptoms are the main option to SM, however, with emerging the new types of cold and flues, the SM is strictly prohibited [27].
We concluded that the main sources of medication for SM of students were the pharmacy without prescription, taking from the friends and previously purchased drugs, moreover they got the drug information from the college, the internet, and health centers. In a study by Patel et al., people also received the needed drugs to SM from the pharmacies, other the sources of the SM components were the family members, friends, and previously bought drugs. They got the information about the medications either by pharmacist, friends, and relatives [3]. Yousef et al., announced the individuals earn their information to drugs through asking the pharmacy staffs, friends and neighbors, and via a formal consultation to a nurse or expert, or based on the previous experiences and similar diseases [25]. In the study by Awad et al., the main source of drugs was the pharmacies [28]. Unfortunately, in Iran, the open markets and pharmacies freely take action to sell medications, this could increase the SM incidences.
Limitation
In the present study, prevalance of SM was studied for one month only, but it can be different at other time period as well as in various seasons. Therefore, further studies should be performed in various seasons and time periods.
Conclusion
According to the results, about 33% of the students of the KUMS had experienced SM during a month, which is a considerable rate. Most of these students took the drugs from the pharmacy without a prescription and the common cold and analgesics were the main drugs to SM. Some of the SM students were affected by the drugs and were facing side effect. It was seen that history of the disease and considering no importance of the signs of disease are the main causes of the SM.
Regarding the above-mentioned issues, SM, which imposes many undesirable outcomes to the health system of a community, should be reduced by establishing the educational programs to the students in the universities and other people via mass media, as well as, it is suggested that the basic steps such as restricting the pharmacies for selling the non-description drugs and warning the people to the SM complications should be done. Moreover, to design the best policy, extra investigations on other community groups are necessary.
Acknowledgments
This study was approved by the vice-chancellor centers of Kermanshah University of Medical Sciences, so we are grateful to all the officials and the students who co-operated in the study.
Financial or Other Competing Interests
None.
References
- [1].Jalilian F, Hazavehei SMM, Vahidinia AA, Jalilian M, Moghimbeigi A. Prevalence and related factors for choosing self-medication among pharmacies visitors based on Health Belief Model in Hamadan Province, West of Iran. Journal of Research in Health Sciences. 2013;13(1):81–85. [PubMed] [Google Scholar]
- [2].Klemenc-Ketis Z, Hladnik Z, Kersnik J. A cross-sectional study of sex differences in self-medication practices among university students in Slovenia. Collegium Antropologicum. 2011;35(2):329–34. [PubMed] [Google Scholar]
- [3].Patel MM, Singh U, Sapre C, Salvi K, Shah A, Vasoya B. Self-medication practices among college Students: A cross sectional study in Gujarat. National Journal of Medical Research. 2013;3(3):257–60. [Google Scholar]
- [4].Azami-Aghdash S, Mohseni M, Etemadi M, Royani S, Moosavi A, Nakhaee M. Prevalence and Cause of Self-Medication in Iran: A Systematic Review and Meta-Analysis Article. Iranian Journal of Public Health. 2015;44(12):1580. [PMC free article] [PubMed] [Google Scholar]
- [5].Ziayee T, Azgoli G, Yagmaei F, A AZ. Knowledge, attitude and practice of self-medication in pregnant women in prenatal health centers affiliated to Shahid Beheshti University of Medical Sciences. Journal of Nursing & Midwifery, Shahid Beheshti University of Medical Sciences and Health Services. 2008;18(62):9–35. [Google Scholar]
- [6].Shamsi M, Tajik R, Mohammad Beigi A. Effect of education based on Health Belief Model on self-medication in mothers referring to health centers of Arak. Arak Medical University Journal (AMUJ) 2009;12(3):57–66. [Google Scholar]
- [7].Baghianimoghadam MH, Ehrampoush MH. Evaluation of attitude and practice of students of Yazd University of Medical Sciences to self-medication. Tabib-e-Shargh. 2006;8(2):111–19. [Google Scholar]
- [8].Purreza A, Khalafi A, Ghiasi A, Farrokh Mojahed F, Nurmohammadi M. To Identify Self-Medication Practice Among Medical Students of Tehran University of Medical Science. Iranian Journal of Epidemiology. 2013;8(4):40–46. [Google Scholar]
- [9].Eslami AA, Moazemi Goudarzi A, Najimi A, Sharifirad G. Knowledge, Attitude and Practice of Students in Universities of Isfahan, Iran toward Self Medication. Journal of Research in Health Systems. 2012;5(7):541–49. [Google Scholar]
- [10].Shamsi M, Biranvand Z. Knowledge, attitude and practice of medical and non- medical students of Lorestan in the context of self-medication in 2011. Journal of Naishabour University of Medical Sciences. 2013;1(1):49–55. [Google Scholar]
- [11].Shamsi M, Byati A. The Effect of Education on Knowledge, Attitudeand Practice of Pregnant Woman Referring to Health Centers AboutSelf-Medication in Arak City. The Horizon of Medical Sciences. 2009;15(3):27–35. [Google Scholar]
- [12].Okumura J, Wakai S, Umenai T. Drug utilisation and self-medication in rural communities in Vietnam. Social Science & Medicine. 2002;54(12):1875–86. doi: 10.1016/s0277-9536(01)00155-1. [DOI] [PubMed] [Google Scholar]
- [13].Ghafouri M, Yaghubi M, Lashkardoost H, Sharifi SH Seyed. The prevalence of self medication among students of Bojnurd universities and its related factors in 2013. Journal of North Khorasan University of Medical Sciences. 2014;5(5) [Google Scholar]
- [14].Badiger S, Kundapur R, Jain A, Kumar A, Pattanshetty S, Thakolkaran N, et al. Self-medication patterns among medical students in South India. The Australasian medical journal. 2012;5(4):217. doi: 10.4066/AMJ.2012.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Sarahroodi S, Maleki-Jamshid A, Sawalha AF, Mikaili P, Safaeian L. Pattern of self-medication with analgesics among Iranian University students in central Iran. Journal of family & community medicine. 2012;19(2):125. doi: 10.4103/2230-8229.98302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Firouz A, et al. Study of arbitrary drug use among students in universities of Ardabil city in 2010. Journal of Ardabil University of Medical Sciences. 2011;11(3):201–07. [Google Scholar]
- [17].Jalilian F, Hazavehei S, Vahidinia A, Moghimbeigi A, Motlagh FZ, Alavijeh MM. Study of Causes of Self-Medication among Hamadan Province Pharmacies Visitors. Sci J Hamadan Univ Med Sci. 2013;20(2):160–66. [Google Scholar]
- [18].Banerjee I, Bhadury T. Self-medication practice among undergraduate medical students in a tertiary care medical college, West Bengal. Journal of postgraduate medicine. 2012;58(2):127–31. doi: 10.4103/0022-3859.97175. [DOI] [PubMed] [Google Scholar]
- [19].Castel JM, Laporte J-R, Reggi V, Aguirre J, de Buschiazzo PM, Coelho HL, et al. Multicenter study on self-medication and self-prescription in six Latin American countries*. Clinical Pharmacology & Therapeutics. 1997;61(4):488–93. doi: 10.1016/S0009-9236(97)90199-5. [DOI] [PubMed] [Google Scholar]
- [20].Akici A, Basaran NF. University Students’ Attitudes Concerning OTC Drug Use; Survey from Istanbul. ARPN Journal of Science and Technology. 2013;3(3):309–15. [Google Scholar]
- [21].Carrasco-Garrido P, Hernández-Barrera V, López de Andrés A, Jiménez-Trujillo I, Jiménez-García R. Sex—Differences on self-medication in Spain. pharmacoepidemiology and drug safety. 2010;19(12):1293–99. doi: 10.1002/pds.2034. [DOI] [PubMed] [Google Scholar]
- [22].Smogavec M, Softic N, Kersnik J, Klemenc-Ketiš Z. An overview of self-treatment and self-medication practices among Slovenian citizens. Zdravniški Vestnik. 2010;79(11):757–63. [Google Scholar]
- [23].Shamsi M, Bayati A, Mohammadbeyghi A, Tajik R. The effect of educational program based on Health Belief Model (HBM) on preventive behaviour of self-medication in woman with pregnancy in Arak, Iran. Pejouhandeh. 2010;14(6):324–31. [Google Scholar]
- [24].Gutema GB, Gadisa DA, Kidanemariam ZA, Berhe DF, Berhe AH, Hadera MG, et al. Self-Medication Practices among Health Sciences Students: The Case of Mekelle University. Journal of Applied Pharmaceutical Science. 2011;1(10):183–89. [Google Scholar]
- [25].Yousef A-MM, Al-Bakri AG, Bustanji Y, Wazaify M. Self-medication patterns in Amman, Jordan. Pharmacy World & Science. 2008;30(1):24–30. doi: 10.1007/s11096-007-9135-x. [DOI] [PubMed] [Google Scholar]
- [26].Kumar N, Kanchan T, Unnikrishnan B, Rekha T, Mithra P, Kulkarni V, et al. Perceptions and Practices of Self-Medication among Medical Students in Coastal South India. PloS one. 2013;8(8):e72247. doi: 10.1371/journal.pone.0072247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Saxena SK, Mishra N, Saxena R, Saxena S. Swine flu: influenza A/H1N1 2009: the unseen and unsaid. Future Microbiology. 2009;4(8):945. doi: 10.2217/fmb.09.71. [DOI] [PubMed] [Google Scholar]
- [28].Awad A, Eltayeb I, Matowe L, Thalib L. Self-medication with antibiotics and antimalarials in the community of Khartoum State, Sudan. J Pharm Pharm Sci. 2005;8(2):326–31. [PubMed] [Google Scholar]


