Abstract
Few studies comprehensively evaluate which types of life stress are most strongly associated with depressive episode onsets, over and above other forms of stress, and comparisons between acute and chronic stress are particularly lacking. Past research implicates major (moderate to severe) stressful life events (SLEs), and to a lesser extent, interpersonal forms of stress; research conflicts on whether dependent or independent SLEs are more potent, but theory favors dependent SLEs. The present study used five years of annual diagnostic and life stress interviews of chronic stress and SLEs from two separate samples (Sample 1 N = 432; Sample 2 N = 146) transitioning into emerging adulthood; one sample also collected early adversity interviews. Multivariate analyses simultaneously examined multiple forms of life stress to test hypotheses that all major SLEs, then particularly interpersonal forms of stress, and then dependent SLEs would contribute unique variance to major depressive episode (MDE) onsets. Person-month survival analysis consistently implicated chronic interpersonal stress and major interpersonal SLEs as statistically unique predictors of risk for MDE onset. In addition, follow-up analyses demonstrated temporal precedence for chronic stress; tested differences by gender; showed that recent chronic stress mediates the relationship between adolescent adversity and later MDE onsets; and revealed interactions of several forms of stress with socioeconomic status (SES). Specifically, as SES declined, there was an increasing role for non-interpersonal chronic stress and non-interpersonal major SLEs, coupled with a decreasing role for interpersonal chronic stress. Implications for future etiological research were discussed.
Keywords: depression, interpersonal, chronic stress, stressful life events, socioeconomic status
One of the most consistent and well-accepted findings in the psychopathology literature is that life stress significantly predicts the onset of major depression. Indeed, meta-analytic findings indicate that unshared environmental factors, such as stress, contribute approximately 63% of variance in risk (Sullivan, Neale, & Kendler, 2000). This work underscores the importance of the environment in precipitating depression, but does not indicate which specific aspects may be most depressogenic. Similarly, substantial research has examined different forms of stressors in predicting depression. However, different forms of stress tend to correlate with one another, making it difficult to discern which stressors, if any, are most depressogenic: Variance shared between more potent and less potent stressors may result in less potent stressors appearing to significantly predict depression. Thus, multivariate models that account for an array of forms of stress may reveal which contribute unique variance over and above the others. The present study uses this approach to identify which stressors are the most depressogenic during emerging adulthood.
Forms of Adversity Associated with Depression
Prior research has examined three primary forms of stress in the context of depression: recent stressful life events, recent chronic stress, and early adversity occurring in childhood or adolescence. Here we focus on studies that used interview-based measures of life stress given their enhanced validity as compared to questionnaires (for a review, see Monroe, 2008). First, recent stressful life events, or SLEs, characterized by their acute onset and relatively brief duration, are widely implicated in depression risk, particularly SLEs with moderate to severe levels of negative impact (“major” SLEs), as opposed to those with less than moderate impact (“minor” SLEs), (e.g., Brown & Harris, 1978; Kendler et al., 1995; Monroe, 2008). Studies also show a relationship between depression and recent chronic stress, which in contrast to SLEs is characterized by endurance over time (e.g., Hammen, 2005). Finally, depression is also associated with so-called “early” adversity occurring during childhood and adolescence in contrast to recent stressors occurring in the past months to year (e.g, Gilman, Kawachi, Fitzmaurice, & Buka, 2003; Kessler, Davis, & Kendler, 1997). However, early adversity may indirectly confer risk for adult onset depression via more recent chronic stress, rather than acting directly (e.g., Hazel, Hammen, Brennan, & Najman, 2008).
Additional Distinctions in Forms of Stress: Interpersonal Content and Independence
Beyond these, two additional distinctions exist in forms of stress. First, several interpersonal theories of depression underscore the importance of interpersonal stress (e.g., rejection, poor social support) to depression (Coyne & Downey, 1991; Hammen, 2003, 2005; Joiner & Metalsky, 1995). Consistent with this, meta-analyses support a link between depression and interpersonal adversity, such as marital discord (Whisman, 2001), bereavement (Cole & Dendukuri, 2003), parental rejection (McLeod, Weisz, & Wood, 2007) and dysfunctional parent-child attachment (Groh, Roisman, van IJzendoorn, Bakermans-Kranenburg, & Fearon, 2012). In addition, research that compares multiple types of stress suggests (but does not explicitly test) that interpersonal forms may contribute significant unique variance to depression. For example, studies show that major SLEs involving loss, humiliation, or targeted rejection are more depressogenic than major SLEs without these characteristics (Brown & Harris, 1978, p. 104; Kendler, Hettema, Butera, Gardner, & Prescott, 2003; Slavich, Thornton, Torres, Monroe, & Gotlib, 2009; Stroud, Davila, Hammen, & Vrshek-Schallhorn, 2011). Finally, interpersonal, but not non-interpersonal, chronic stress predicted recurrence of MDEs in young adults (Sheets & Craighead, 2014). Thus, theory and evidence suggest that interpersonal forms of stress will predict MDE onsets over and above non-interpersonal forms, but additional evidence from studies that include multiple forms of stress is needed.
Second, SLEs have been distinguished based on their independence—the degree to which their occurrence depends upon the behavior of the individual. Independent (or fateful) SLEs occur independently of the person's behavior (e.g., death of a relative) whereas dependent SLEs occur as least partially due to the person's behavior (e.g., failing an exam). Despite considerable research, it remains unclear whether either is more depressogenic. Some research suggests that independent SLEs are more depressogenic (Monroe et al., 2006; Shrout et al., 1989; Stroud et al., 2011), whereas other work suggests that dependent events, particularly interpersonal ones, are more depressogenic (e.g., Hammen, Mayol, DeMayo, & Marks, 1986; Kendler, Karkowski, & Prescott, 1999; Lenze, Cyranowski, Thompson, Anderson, & Frank, 2008). In addition to this mixed evidence, only one study has explicitly tested whether the effects of independent or dependent SLEs on MDE onsets significantly differed (Kendler et al., 1999). In that study, dependent SLEs had significantly larger effects, yet this may have been driven by the interpersonal nature of these SLEs, as dependent SLEs are often interpersonal. Consistent with this, stress generation theory suggests that dependent events, especially interpersonal ones, may be particularly relevant for depression (e.g., Hammen, 2006). Thus, despite mixed evidence, there is greater basis to predict that dependent SLEs may be more depressogenic; however, this has not explicitly been tested while accounting for the interpersonal nature of SLEs.
Testing Unique Contributions of Different Forms of Stress
Despite the substantial body of research on interpersonal stress, several criteria are necessary to provide robust tests of whether certain forms of stress uniquely contribute to depression. To-date, no study meets all criteria. First, clinical interviews for depression should cover limited periods of time to help prevent recall failures (Moffitt et al., 2010). Second, objective, contextual interview-based assessments of stress are vital because existing questionnaires lack validity (Monroe, 2008); interviews should assess both chronic and episodic stress because these correlate and could be confounded if only one were assessed. Third, measures should account for key hypothesized distinctions of SLEs, especially distinctions that might confound each other's effects (e.g., interpersonal SLEs and dependent SLEs). Fourth, samples that include both individuals with and without depression permit estimation of generalizable effect sizes for stress. Finally, ideally, interviews should collect dates for SLEs and onsets to establish the temporal precedence of SLEs to MDEs. We believe this is the first study to fulfill these criteria.
Present Study
To provide a robust test of whether certain forms of stress contribute significant unique variance to depression, the present study examined two samples of older adolescents transitioning into young adulthood, focusing on which forms of stress contribute unique variance on average. We accounted for several variables that may affect the stress-depression association, including gender (e.g., Hammen, 2003), socioeconomic status (SES; e.g., Lorant et al., 2003) and depression history (e.g., Stroud, Davila, & Moyer, 2008). Both samples comprised five years of life stress interviews and clinical diagnostic interviews for major depressive episodes (MDEs); one sample provided childhood and adolescent adversity indices. In addition to interpersonal and non-interpersonal chronic stress, both samples permitted examination of three distinctions of SLEs (yielding eight different types): major versus minor SLEs, interpersonal versus non-interpersonal SLEs, and independent versus dependent SLEs. Thus, each sample provided 10-12 forms of stress for study. We hypothesized that major interpersonal SLEs as well as interpersonal chronic stress would contribute significant unique variance. Despite conflicting empirical evidence, we hypothesized that dependent major interpersonal SLEs would contribute significant unique variance over independent major interpersonal SLEs. In Sample 1, we did not anticipate that early adversity would make unique contributions to MDEs because one study indicated that early adversity acts indirectly (Hazel et al., 2008).
Method
Participants and Procedures
Sample 1
This study was part of a larger investigation of biopsychosocial risk factors for the emotional disorders, the Youth Emotion Project (YEP). Prior to invitation to the YEP, high school juniors were screened for neuroticism level using the Revised Eysenck Personality Questionnaire (Eysenck, Eysenck, & Barrett, 1985). Those who scored in the top third were oversampled (approximately 60% of participants) to increase the number of new onsets of disorders (for more information, see Zinbarg et al., 2010). Participants (N = 627) provided informed consent and completed in-person baseline diagnostic and life stress interviews. Follow-up interviews were repeated annually via telephone; five years of data were used in the present study. Interviewers were post-baccalaureate research assistants, graduate students, and postdoctoral psychologists, who completed extensive training and produced interview ratings that matched gold standard ratings developed by the principal investigators. Interviewers were blind to previous assessments and presented all cases to a doctoral level supervisor. Beginning in the sixth year, participants were invited to complete the Childhood Trauma Interview (CTI; Fink, Bernstein, Handelsman, Foote, & Lovejoy, 1995). Individuals who did (n = 456) and did not (n = 171) complete the CTI did not differ significantly on minority race/ethnicity, gender, SES, or screening neuroticism score (all ps > .05, see Vrshek-Schallhorn, Wolitzky-Taylor, et al., 2014).
Individuals were excluded from analyses for one or more of the following criteria: lacking the baseline SES measurement (n = 31), diagnosis of bipolar disorder I or II (n = 13), psychotic symptoms (n = 5), or depression lasting all months assessed (n = 1). The 432 individuals (296 females, 68.5%) in the final sample began the study with a mean age of 16.91 years (SD = 0.38 years), contributed an average of 53.35 person-months to analyses (SD = 11.04, range 13-70), and completed an average of 4.38 of 5 interviews (SD = .87). They came from varied SES backgrounds, but were on average upper-middle class (Hollingshead SES; range 13-66, M = 48.59, SD = 12.56). Self-reported ethnicity was: African American, 13.2%; Asian, 4.2%; Caucasian, 49.1%; Hispanic, 14.6%; Pacific Islander, 0.7%; multiple races/ethnicities, 13%; and other, 5.3%. Gender, minority status, SES, and the number of prior MDEs at baseline did not predict total months of assessments available (all ps < .05).
Sample 2
This study was part of a larger project examining psychosocial predictors of depression in the transition to adulthood. Participants were recruited from the senior classes at three public high schools that were demographically representative of Los Angeles County. After consenting, all female 12th grade students (N = 902) received a questionnaire packet and 513 (57%) were returned and completed; 341 participants agreed to be contacted. Three months following graduation, 155 were scheduled for initial face-to-face interviews. The reduced number scheduled was due to study time commitments, difficulties contacting participants (due to traveling or moves), lack of transportation, or scheduling (due to work). To evaluate the representativeness of the reduced sample, Hammen and colleagues (e.g., see Hammen, Henry, & Daley, 2000) conducted two sets of comparisons of demographic variables and psychological adjustment; analyses revealed no significant differences.
Individuals were excluded from analyses for any of one of the following: lacking the baseline SES measurement (n = 3), a diagnosis of bipolar disorder (n = 1), or participating in the study for less than 6 months (n = 5). The 146 female participants began the study with a mean age of 18.27 years (SD = 0.46, range 16.72-19.43) and came from diverse socioeconomic backgrounds, but were on average middle-class (Hollingshead score; range 9 to 66; M = 45.86, SD = 12.99; Hollingshead, 1975). Minority status, and the number of prior MDEs at baseline did not predict total months of assessments available (ps < .05), but lower SES predicted fewer months of assessment available (β = .20; t = 2.23; p <.05).
Self-reported ethnicity was African American, 1.3%; Asian American, 9.4%; Caucasian, 45.6%; Chicana or Latina, 21.5%; other, 21.5%; and unreported, 0.7%. Of the 155 participants who completed the initial interview, 118-140 (76% - 90%) completed each follow-up (contributing on average 50.18 months to analyses, SD = 14.37; range 4-62), which occurred 6 months after the initial interview and then annually for five years. Licensed clinical psychologists or clinical psychology graduate students conducted all interviews.
Measures
SES
SES scores used Hollingshead's (1975) index of parental education and occupation, which provides a continuous scale ranging from 8-66.
Assessment of Depression
The Structured Clinical Interview for DSM-IV and DSM-III-R respectively, non-patient editions (SCID-NP; herein called the SCID; Sample 1: First, Spitzer, Gibbon, & Williams, 2001; Sample 2: Spitzer, Williams, Gibbon, & First et al., 1990) were used to assess major depression. The initial interview covered lifetime and current disorders, and follow-ups probed the period between interviews. Inter-rater reliability for depression diagnoses was similar in the two samples (assessed by independent ratings from audiotapes; Sample 1 (approximately 10% of cases per year): kappa values adjusted due to departure from equiprobable distributions: .82 - .94 (M = .89, SD = .05); Sample 2: weighted kappas = .89 (n = 46) for initial interview and .93 (n = 20) for follow-ups). In Sample 1, most participants (n = 364; 84%) entered the study with no prior episodes; 52 (12%) had one, and 16 (4%) had two or more. In Sample 2, 102 (68%) participants entered the study with no prior episodes and 49 (32%) participants entered the study with at least one prior episode (1 prior MDE : n = 46; 2 prior MDEs: n = 3).
Recent Life Stress Assessment
Chronic and episodic stress were assessed with the UCLA Life Stress Interview (LSI; Hammen et al., 1987; Hammen, Marks, Mayol, & DeMayo, 1985). The baseline interview assessed the past year; follow-up interviews assessed the period since the last interview.
Chronic Stress
The LSI examined the enduring aspect of ongoing objective stress over the interview period in an array of domains (best friend relationship, peer social circle, romantic relationships, family relationships, academics, work, finances, neighborhood conditions, physical health, and family's health, although Sample 2 lacked neighborhood conditions). Interviewers rated each chronic stress domain independently of related SLEs that occurred, to the extent possible. In addition, interviewers were trained to rate separate chronic stress domains distinct from one another, avoiding a “halo effect.” When chronic conditions changed partway through an interview period (sometimes due to an SLE, rated separately), interviewers rated each epoch separately and prorated the final summary score accounting for both epochs. In both samples, the interviewer assessed and rated each domain on a scale from 1 (excellent/ optimal circumstances) to 5 (very bad circumstances) in half-point increments using behavioral descriptions for each scale point. Inter-rater reliability (inter-class correlations; ICCs) ranged from 0.72 to 0.83 within site and 0.62 to 0.80 cross-site using approximately 10% of interviews in Sample 1, and from .82 to .91 (n = 57) in Sample 2. We created two chronic stress composites for each interview period. The mean of the best friend relationship, peer social circle, romantic relationships, and family relationships domains comprised an interpersonal chronic stress composite, and the mean of the academics, work, financial, and neighborhood condition domains (the latter for Sample 1 only), comprised a non-interpersonal chronic stress composite.
Stressful life events
The episodic LSI (e.g., Hammen et al., 1985) was adapted from Brown's contextual threat assessment method (Brown & Harris, 1978). For each SLE, interviewers assessed the date, nature, and surrounding context. Subsequently, interviewers presented narrative accounts of each SLE including details of what happened, duration, consequences, and context (such as circumstances and resources to cope with it, expectedness, and prior experience with similar events), to a team of two or more raters who were blind to participants’ diagnoses and subjective responses. The rating team assigned context-based ratings of severity and a code to describe each event (e.g., death) from a modified Paykel and Mangen (1980) event list. When experiences occurred in close succession (compound events, e.g., discovery of romantic infidelity followed by break-up), the general approach of the LSI was to consider sequelae as part of the context, impact, and threat, but the independent rating team decided whether these constituted a single, unfolding event or multiple, separate events (e.g., romantic infidelity and a much later break-up) on a case-by-case basis. Further, when “events” were highly recurrent and consistent in severity and content (e.g., repeated arguments in a poor quality romantic relationship), these were captured only by the chronic stress rating, except for those that were atypical in severity or content (e.g., physical altercation leading to police intervention), which were scored as SLEs.
Severity ratings ranged from 1 (non-event, or no significant threat or negative impact) to 5 (a very severe event, maximal negative impact or threat) in half-point increments, indicating the expected amount of impact for a typical individual given a similar context. In Sample 1, based on an a priori, contextually-based decision applied to all previous published LSI analyses for this sample, events with a severity rating ≥ 2.5 were designated as major SLEs (e.g., Uliaszek et al., 2012; Vrshek-Schallhorn, Mineka, et al., 2014). In Sample 2, events rated ≥ 3.0 were designated as major SLEs, consistent with prior analyses in this sample (e.g., Hammen et al., 2000; Stroud et al., 2011). In both samples, SLEs with a severity rating below each cutoff and above 1.0 were classified as minor. Due to slight intra-study differences in assignment of ratings, and following visual inspection of brief event descriptions, we believe these are roughly equivalent (and the closest matching possible) cut points for major SLEs. Table 2 presents descriptive information about the number of events experienced, and the frequency of major and minor events was similar between samples. Further, both studies classified similar percentages of SLEs as major (Sample 1, 20.8%; Sample 2, 16.7%).
Table 2.
Pearson zero-order correlations of demographic variables, stress variables, and MDE onsets
| a. Sample 1 | Variable Number | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Sample 1 M(SD) | Sample 2 M(SD) | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
| 1. Gender (male=1, female=0) | 0.31 (0.46) | .09 | −.10* | −.03 | .06 | −.20** | .09 | −.16** | .14** | −.14** | −.18** | −.01 | .14** | −.09 | −.15** | .01 | .19** | .02 | .09 | −.11* | |
| 2. SocioeconomicStatus | 48.59 (12.56) | 45.86(12.99) | -- | −.06 | −.27** | −.46** | −.21** | −.20** | .10* | .05 | −.11* | −.22** | −.21** | −.11* | .07 | .08 | .06 | .03 | −.20** | −.10* | −.02 |
| 3. Number of previous MDEs | 0.34 (0.58) | .65 (.71) | .04 | -- | .33** | .22** | .22** | .16** | .03 | .13** | .09 | .25** | .16** | .08 | .01 | .05 | .19* | .10* | .17** | .23** | .63** |
| 4. Chronic Interpersonal Stress (1-5) | 2.31 (0.37) | 2.69 (.48) | −.27** | .25** | -- | .63** | .37** | .32** | .04 | .04 | .16** | .44** | .20** | .30** | .03 | .06 | .02 | .08 | .40** | .38** | .34** |
| 5. Chronic Non-interpersonal Stress(1-5) | 2.20 (0.37) | 2.51 (.39) | −.19** | .20** | .63** | -- | .40** | .48** | −.02 | .17** | .30** | .35** | .33** | .41** | .00 | −.01 | .09 | .19** | .47** | .43** | .20** |
| 6. Major Interpersonal SLE | 1.62 (1.81) | 2.31 (2.20) | −.06 | .25** | .40** | .41** | -- | .32** | .20** | .21** | .78** | .81** | .28** | .22** | .19** | .18** | .21** | .16** | .22** | .25** | .23** |
| 7. Major Non-Interpersonal SLE | 1.05 (1.34) | .95 (1.11) | −.04 | .17* | .37** | .33** | .56** | -- | .20** | .31** | .24** | .31** | .80** | .74** | .16** | .19** | .21** | .29** | .27** | .28** | .12** |
| 8. Minor Interpersonal SLE | 5.85 (3.1) | 8.38 (4.68) | .17* | .13 | .30** | .24** | .33** | .27** | -- | .33** | .15** | .18** | .13** | .19** | .75** | .84** | .33** | .24** | .06 | .11* | .05 |
| 9. Minor Non-Interpersonal SLE | 4.33 (2.56) | 7.88 (3.74) | .19* | .15 | .11 | .03 | .22** | .23** | .52** | -- | .20** | .13** | .20** | .27** | .35** | .26** | .78** | .77** | .08 | .13** | .05 |
| 10. Major Independent Interpersonal SLE | 0.89 (1.13) | .97 (1.08) | .10 | .23** | .16 | .19* | .69** | .33** | .16 | .20* | -- | .29** | .19** | .21** | .20** | .09 | .22** | .14** | .16** | .18** | .11* |
| 11. Major Dependent Interpersonal SLE | 0.80 (1.24) | 1.42 (1.72) | −.15 | .20* | .44** | .43** | .89** | .54** | .32** | .17* | .30** | -- | .28** | .22** | .11* | .20** | .11* | .11* | .20** | .24** | .26** |
| 12. Major Independent Non-Interpersonal SLE | 0.63 (0.92) | .55 (.84) | .06 | .15 | .17* | .16 | .29** | .68** | .13 | .18* | .32** | .18* | -- | .21** | .10* | .13** | .16** | .16** | .19** | .22** | .10* |
| 13. Major Dependent Non-Interpersonal SLE | 0.46 (0.88) | .42 (.83) | −.14 | .09 | .34** | .31** | .47** | .69** | .24** | .13 | .13 | .55** | −.04 | -- | .15** | .17** | .14** | .29** | .24** | .24** | .10* |
| 14. Minor Independent Interpersonal SLE | 2.74 (1.94) | 1.81 (1.54) | .14 | .15 | .04 | −.01 | .15 | .08 | .47** | .31** | .18* | .08 | .00 | .07 | -- | .31** | .41** | .21** | .02 | .07 | −.02 |
| 15. Minor Dependent Interpersonal SLE | 3.61 (2.32) | 6.89 (4.27) | .15 | .09 | .31** | .27** | .32** | .28** | .95** | .49** | .14 | .32** | .14 | .25** | .20* | -- | .20** | .27** | .10* | .14** | .11* |
| 16. Minor Independent Non-Interpersonal SLE | 2.58 (1.87) | 2.55 (1.90) | .16* | .16 | −.02 | −.11 | .13 | .07 | .39** | .70** | .17* | .05 | .09 | −.01 | .29** | .35** | -- | .25** | .03 | .04 | .08 |
| 17. Minor Dependent Non-Interpersonal SLE | 2.16 (1.79) | 5.73 (2.98) | .17** | .09 | .16 | .12 | .24** | .26** | .45** | .90** | .16* | .21* | .16 | .21* | .23** | .44** | .35** | -- | .11* | .20** | −.01 |
| 18. Childhood Adversity Summary Index (Sample 1) | 9.2 (9.53) | -- | .66** | .17** | |||||||||||||||||
| 19. Adolescent Adversity Summary Index (Sample 1) | 18.81 (14.48) | -- | .22** | ||||||||||||||||||
| 20. Number of MDE Onsets in Study Period | 0.38 (0.75) | .81 (1.01) | .10 | .73** | .22* | .21* | .30** | .21* | .14 | .10 | .20* | .28** | .16 | .12 | .19* | .09 | .09 | .10 | .21* | .30** | -- |
Note: Sample 1 results are above the diagonal in white, and Sample 2 results are below the diagonal in light gray. Sample 2 is exclusively female, therefore no correlations with gender are presented. M = Mean. SD = Standard Deviation. MDE = Major Depressive Episode. SLE = Stressful life event. Number of previous MDEs represents the average of the time-varying variable across person-months used in analyses. SLE frequencies represent the number of months with at least one new occurrence of each type of event reported over the entire five-year study period. Chronic stress here refers to average levels of these time-varying variables across all person-months used in analyses, in contrast to survival analyses in which one chronic stress rating per domain is assigned per interview period (e.g., 12 months).
p < .05 (2-tailed).
p < .01 (2-tailed).
The team rated the independence of the events from 1 (fully independent of the person's behavior, abilities, and characteristics; e.g., death) to 5 (fully dependent; occurred strictly as a result of the person's own actions; e.g., failed exam). Events coded as 3 or higher were considered to be at least partly the result of the participant's actions and were coded as dependent, following previous studies (e.g., Davila, Hammen, Burge, Paley, & Daley, 1995; Stroud et al., 2011). A second team re-rated a set of events on severity and independence blind to the original ratings. Inter-rater reliability was good (Sample 1 using 10% of interviews annually: severity: ICCs = .69 - .76 (M = .72, SD = .03); independence: ICCs = .77 - .86 (M = 0.83, SD = .04); Sample 2: severity: ICC = .92 (n =74); independence: ICC = .97 (n =53)).
In Sample 1, the events were coded a priori from the Paykel list by content (primarily interpersonal or not), and in Sample 2, the scoring team rated events as interpersonal or not based on the contextual information for each event. In both cases, interpersonal content referred to situations primarily involving or affecting relationships with the participant.
To ensure the temporal precedence of events to MDE onsets in Sample 1, when an MDE and an SLE were dated to the same person-month, staff examined interview records to determine the order of occurrence. In Sample 2, timelines precisely dating MDEs and SLEs assured that events preceded episodes. In both samples, when it was not clear whether events preceded episodes, the event (but not the MDE or participant) was excluded from analysis.
Childhood and Adolescent Adversity Assessment in Sample 1
As previously described (Vrshek-Schallhorn, Wolitzky-Taylor, et al., 2014), the semi-structured CTI (Fink et al., 1995) assessed adversity from birth through the age of 16, including separation from or loss of a caregiver, neglect by a caregiver, emotional abuse, physical abuse, witnessing violence, and sexual abuse or assault. Interviewers rated the severity of each adversity from 1 (minimal or mild) to 6 (very extreme, sadistic) based on behavioral descriptions provided by participants and using over 260 examples in a scoring manual. Scores were summed to create an index of total adversity. Adversities for ages 0 to 9 years old (“early and middle childhood”) and 9 to 16 years old (“preadolescence and adolescence”) were considered separately in light of evidence of prepubertal physiological changes by nine years of age (Romeo, 2010) and because this age was approximately midway through the time period assessed and corresponded roughly to the mean age of reported adversities in this sample. There was no comparable measure in Sample 2.
Statistical Approach
Survival analyses were conducted using person-month datasets. MDE onset and offset dates were assigned to the nearest month. The use of months is consistent with recommendations to use the smallest accurate unit of time (Singer & Willett, 2003). In Sample 1, the date one year prior to the baseline interview marked the beginning of time in analyses. In Sample 2, the date of the baseline interview marked the beginning of time in analyses. Individuals diagnosed with an ongoing MDE at the study's beginning were excluded from analyses until that MDE ended. Likewise, in the month immediately following a new MDE onset, individuals were excluded from analyses until the MDE ended, when they were re-included. A period of eight weeks without meeting criteria was used to define an offset, consistent with DSM-IV-TR (American Psychiatric Association, 2000); successive MDEs separated by fewer than eight weeks of recovery were combined into a single episode. The MDE onset variable was coded as present (1) or absent (0) for each person-month.
Consistent with prior work (e.g., Kendler, Karkowski, & Prescott, 1998; Kendler et al., 1995), analyses of SLEs focused on dichotomous occurrences, which were coded as absent (0) or present (1) for each type of SLE for each person-month. Events were dated to the month of occurrence and lagged to a second month in order to permit each event to be included in statistical prediction of MDEs for two person-months, consistent with approaches of similar studies that use person-month datasets (Stroud et al., 2011; Vrshek-Schallhorn, Mineka, et al., 2014). For example, if an individual experienced a major interpersonal SLE and a minor non-interpersonal SLE in the 25th month of the study, a major interpersonal SLE and a minor non-interpersonal SLE were each coded as present for both the 25th and 26th months. This two-month period was selected given evidence that most event-triggered MDE onsets occur within a month of the SLE (Kendler et al., 1995) but also evidence indicating that SLEs can increase risk beyond the first month (Kendler et al., 1998; Surtees & Wainwright, 1999). Chronic stress scores were assigned uniformly across all person-months covered by a given interview period (i.e., these ratings did not vary by month and instead covered approximately 12 months, except for the first follow-up of Sample 2 which covered 6 months) and were standardized to center variables and allow interpretation in terms of standard deviations.
Primary Analyses
We conducted three sets of primary analyses. First, all types of stress were examined in isolation (but with covariates included) to test whether stressors significantly predicted MDE onsets when examined alone. Second, bivariate correlations examined the extent to which stress variables and the covariates were intercorrelated. Third, multivariate stress models simultaneously examined all stress variables that produced individual associations of p ≤ .10 in Step 1 to investigate which stressors may contribute unique variance to MDE onsets. All models included SES, history of depression, and gender (Sample 1 only; male = 1, female = 0) as covariates. History of depression varied over time: Each time a participant recovered from an MDE and re-entered the model, the number of their previous MDEs was increased by one, up to two. (Only a small percentage of participants had greater than 2 prior lifetime episodes.) Hazard ratios (HRs) reported indicate the difference in likelihood of MDE onset associated with any one unit increase in the predictor (Singer & Willett, 2003).
Secondary Analyses
Following the primary analyses, we conducted several secondary analyses. Pre-planned analyses include examination of: a) the potential role of gender; b) tests enforcing strict temporal precedence of chronic stress prior to MDEs; and c) deviance tests to assess whether unique variance significantly differed between forms of stress. Post-hoc models examined one discrepancy between results for the two samples, and investigated the role of childhood and adolescent adversity.
Results
Sample 1
Analyses of Types of Stress in Isolation and Zero Order Correlations
In 22,988 person-months, 163 MDEs were recorded. One-hundred-ten participants had MDEs (70 had one MDE, 30 had two MDEs, seven had three MDEs, and three had four MDEs). Examination of different forms of stress in isolation from each other (with gender, SES, and depression history covaried) indicated that almost all hypothesized forms of stress were significantly and positively associated with MDE onset (Table 1a) except for major non-interpersonal dependent SLEs, which only approached significance, HR = 1.995, p = .059. Although minor SLEs tended not to be significantly associated with MDE onset, minor interpersonal SLEs approached significance, HR = 1.389, p = .060, which appeared to be driven by events that were dependent, HR = 1.461, p = .055, rather than independent, HR = 1.115, p = .641. Further, almost all of the different forms of stress were significantly intercorrelated (Table 2), with several exceptions (e.g., chronic stress was not significantly associated with several minor SLEs).
Table 1.
Univariate Associations of Different Forms of Stress in Predicting MDE Onsets
| a. Sample 1 | ||||||
|---|---|---|---|---|---|---|
| Stress Variable | β | SE(β) | HR | 95% Lower CI | 95% Upper CI | p-value |
| Chronic Interpersonal Stress | .729 | .089 | 2.073 | 1.740 | 2.469 | .000 |
| Chronic Non-interpersonal Stress | .536 | .100 | 1.710 | 1.406 | 2.080 | .000 |
| Major Interpersonal SLE | 1.033 | .205 | 2.810 | 1.880 | 4.201 | .000 |
| Major Non-Interpersonal SLE | .735 | .266 | 2.086 | 1.237 | 3.515 | .006 |
| Minor Interpersonal SLE | .328 | .174 | 1.389 | .987 | 1.955 | .060 |
| Minor Non-Interpersonal SLE | −.456 | .245 | .634 | .392 | 1.023 | .062 |
| Major Independent Interpersonal SLE | .881 | .280 | 2.412 | 1.392 | 4.180 | .002 |
| Major Dependent Interpersonal SLE | 1.127 | .243 | 3.086 | 1.917 | 4.969 | .000 |
| Major Independent Non-Interpersonal SLE | .811 | .329 | 2.249 | 1.181 | 4.285 | .014 |
| Major Dependent Non-Interpersonal SLE | .691 | .366 | 1.995 | .974 | 4.086 | .059 |
| Minor Independent Interpersonal SLE | .109 | .234 | 1.115 | .705 | 1.765 | .641 |
| Minor Dependent Interpersonal SLE | .379 | .198 | 1.461 | .992 | 2.153 | .055 |
| Minor Independent Non-Interpersonal SLE | −.500 | .313 | .606 | .328 | 1.119 | .110 |
| Minor Dependent Non-Interpersonal SLE | −.430 | .313 | .650 | .352 | 1.200 | .169 |
| Childhood Adversity Summary Index | .252 | .069 | 1.286 | 1.124 | 1.472 | .000 |
| Adolescent Adversity Summary Index | .279 | .064 | 1.322 | 1.167 | 1.498 | .000 |
| b. Sample 2 | ||||||
|---|---|---|---|---|---|---|
| Stress Variable | β | SE(β) | HR | 95% Lower CI | 95% Upper CI | p-value |
| Chronic Interpersonal Stress | .693 | .127 | 2.000 | 1.560 | 2.563 | .000 |
| Chronic Non-interpersonal Stress | .590 | .126 | 1.804 | 1.410 | 2.308 | .000 |
| Major Interpersonal SLE | 1.493 | .223 | 4.452 | 2.873 | 6.899 | .000 |
| Major Non-Interpersonal SLE | 1.499 | .307 | 4.475 | 2.452 | 8.167 | .000 |
| Minor Interpersonal SLE | .431 | .188 | 1.538 | 1.063 | 2.225 | .022 |
| Minor Non-Interpersonal SLE | .272 | .196 | 1.919 | .893 | 1.928 | .166 |
| Major Independent Interpersonal SLE | 1.628 | .274 | 5.095 | 2.978 | 8.717 | .000 |
| Major Dependent Interpersonal SLE | 1.196 | .298 | 3.306 | 1.842 | 5.931 | .000 |
| Major Independent Non-Interpersonal SLE | 1.529 | .392 | 4.613 | 2.140 | 9.942 | .000 |
| Major Dependent Non-Interpersonal SLE | 1.320 | .459 | 3.745 | 1.523 | 9.207 | .004 |
| Minor Independent Interpersonal SLE | .592 | .285 | 1.807 | 1.033 | 3.160 | .038 |
| Minor Dependent Interpersonal SLE | .307 | .199 | 1.359 | .921 | 2.006 | .122 |
| Minor Independent Non-Interpersonal SLE | .693 | .242 | 1.999 | 1.244 | 3.210 | .004 |
| Minor Dependent Non-Interpersonal SLE | −.002 | .226 | .998 | .641 | 1.556 | .994 |
Note. Each form of stress was entered without other stress variables in a Cox regression model predicting MDE onsets. Gender (sample 1 only), number of previous MDEs (0, 1, or 2 or more), and socioeconomic status are covaried. SLE = Stressful Life Event. MDE = Major Depressive Episode.
Multivariate Models (Table 3)
Table 3.
Multivariate Associations of Different Forms of Stress with MDE Onsets
| Model 1. Stratify SLEs by severity & interpersonal status only | ||||||
|---|---|---|---|---|---|---|
| Stress Variable | β | SE(β) | HR | 95% Lower CI | 95% Upper CI | p-value |
| a. Sample 1 | ||||||
| Gender | -.320 | .198 | .726 | .493 | 1.070 | .106 |
| Socioeconomic Status | .171 | .087 | 1.186 | 1.001 | 1.406 | .049 |
| Number of previous MDEs (0, 1, 2) | .346 | .101 | 1.414 | 1.161 | 1.723 | .001 |
| Chronic Interpersonal Stress | .581 | .110 | 1.787 | 1.441 | 2.218 | .000 |
| Chronic Non-interpersonal Stress | .092 | .122 | 1.096 | .863 | 1.392 | .453 |
| Major Interpersonal SLE | .801 | .208 | 2.228 | 1.482 | 3.350 | .000 |
| Major Non-Interpersonal SLE | .445 | .271 | 1.561 | .918 | 2.654 | .100 |
| Minor Interpersonal SLE | .218 | .175 | 1.243 | .882 | 1.753 | .214 |
| Childhood Adversity Summary Index | .016 | .092 | 1.016 | .849 | 1.217 | .860 |
| Adolescent Adversity Summary Index | .096 | .087 | 1.101 | .929 | 1.305 | .266 |
| b. Sample 2 | ||||||
| Socioeconomic Status | .129 | .094 | 1.138 | .947 | 1.368 | .167 |
| Number of previous MDEs (0, 1, 2) | .122 | .105 | 1.130 | .920 | 1.387 | .224 |
| Chronic Interpersonal Stress | .441 | .142 | 1.554 | 1.176 | 2.055 | .002 |
| Chronic Non-interpersonal Stress | .257 | .141 | 1.293 | .982 | 1.703 | .068 |
| Major Interpersonal SLE | 1.116 | .236 | 3.054 | 1.924 | 4.846 | .000 |
| Major Non-Interpersonal SLE | .939 | .321 | 2.558 | .1.363 | 4.801 | .003 |
| Minor Interpersonal SLE | .294 | .190 | 1.341 | .924 | 1.948 | .123 |
| Model 2. Stratify SLEs by severity, interpersonal status, and independence | ||||||
|---|---|---|---|---|---|---|
| Stress Variable | β | SE(β) | HR | 95% Lower CI | 95% Upper CI | p-value |
| a. Sample 1 | ||||||
| Gender | -.322 | .197 | .725 | .493 | 1.067 | .103 |
| Socioeconomic Status | .179 | .087 | 1.196 | 1.008 | 1.418 | .040 |
| Number of previous MDEs (0, 1, 2) | .342 | .101 | 1.408 | 1.156 | 1.716 | .001 |
| Chronic Interpersonal Stress | .597 | .111 | 1.817 | 1.462 | 2.257 | .000 |
| Chronic Non-interpersonal Stress | .110 | .122 | 1.116 | .878 | 1.418 | .370 |
| Major Independent Interpersonal SLE | .640 | .305 | 1.896 | 1.043 | 3.448 | .036 |
| Major Dependent Interpersonal SLE | .679 | .258 | 1.973 | 1.189 | 3.272 | .008 |
| Major Independent Non-Interpersonal SLE | .445 | .362 | 1.560 | .767 | 3.173 | .219 |
| Major Dependent Non-Interpersonal SLE | -.062 | .408 | .940 | .422 | 2.092 | .879 |
| Minor Dependent Interpersonal SLE | .286 | .199 | 1.331 | .901 | 1.964 | .150 |
| Childhood Adversity Summary Index | .014 | .092 | 1.014 | .847 | 1.215 | .879 |
| Adolescent Adversity Summary Index | .095 | .087 | 1.099 | .928 | 1.302 | .274 |
| b. Sample 2 | ||||||
| Socioeconomic Status | .106 | .094 | 1.112 | .926 | 1.337 | .256 |
| Number of previous MDEs (0, 1, 2) | .076 | .104 | 1.079 | .880 | 1.324 | .464 |
| Chronic Interpersonal Stress | .472 | .139 | 1.603 | 1.220 | 2.108 | .001 |
| Chronic Non-interpersonal Stress | .284 | .140 | 1.329 | 1.011 | 1.748 | .042 |
| Major Independent Interpersonal SLE | 1.340 | .283 | 3.817 | 2.191 | 6.650 | .000 |
| Major Dependent Interpersonal SLE | .572 | .315 | .772 | .956 | 3.285 | .069 |
| Major Independent Non-Interpersonal SLE | 1.014 | .404 | 2.756 | 1.248 | 6.088 | .012 |
| Major Dependent Non-Interpersonal SLE | .745 | .475 | 2.107 | .830 | 5.351 | .117 |
| Minor Independent Interpersonal SLE | .553 | .287 | 1.738 | .991 | 3.047 | .054 |
| Minor Independent Non-Interpersonal SLE | .575 | .246 | 1.777 | 1.098 | 2.877 | .019 |
Note. SLE = Stressful Life Event. MDE = Major Depressive Episode. P-values ≤ .05 are bolded.
When events were stratified only by severity and interpersonal status (Model 1), the significant unique predictors were interpersonal chronic stress (HR = 1.787, p < .001) and major interpersonal SLEs (HR = 2.228, p < .001). Indicators of childhood (HR = 1.016, p = .860) and adolescent adversity (HR = 1.101, p = .266) were not significant unique predictors.1 When events were further stratified by independence (Model 2), the significant unique predictors were chronic interpersonal stress (HR = 1.817, p < .001), major interpersonal independent SLEs (HR = 1.896, p = .036), major interpersonal dependent SLEs (HR = 1.973, p = .008). Neither major non-interpersonal independent nor dependent events were significant, nor were childhood and adolescent adversity (Table 3).2
Sample 2
Analyses of Types of Stress in Isolation and Zero Order Correlations
In 7,167 person-months, 118 MDEs were recorded. Seventy participants had at least 1 MDE (37 had one MDE, 18 had two MDEs, 15 had three MDEs). As in Sample 1, when examined in isolation (with SES and depression history covaried), almost all hypothesized forms of stress were significantly and positively associated with depression onset (Table 1b). In addition, minor interpersonal SLEs were associated with MDE onset, which in contrast to Sample 1, appeared to be driven by events that were independent, HR = 1.807, p = .038, rather than dependent, HR = .921, p = .122. Moreover, minor independent non-interpersonal SLEs were associated with increased risk, HR = 1.244, p = .004, but minor dependent non-interpersonal SLEs and overall minor non-interpersonal SLEs were not.
Further, almost all of the different forms of major stress were significantly intercorrelated (Table 2). Exceptions included that the chronic stress variables tended not to be significantly associated with minor non-interpersonal SLEs, in contrast to significant association with minor interpersonal SLEs.
Multivariate Models (Table 3)
When events were stratified only by severity and interpersonal status (Model 1), the significant unique predictors were chronic interpersonal stress (HR = 1.554, p < .01) and major interpersonal (HR = 3.054, p < .001) and non-interpersonal (HR = 2.558, p < .01) SLEs. When events were further stratified by independence, the significant unique predictors were: chronic interpersonal (HR = 1.603, p < .01) and non-interpersonal stress (HR = 1.329, p < .05); major independent interpersonal SLEs (HR = 3.817, p < .001); major independent non-interpersonal SLEs (HR = 2.756, p < .05); and minor independent non-interpersonal SLEs (HR = 1.777, p < .05). Finally, major dependent non-interpersonal SLEs did not contribute significant unique variance to risk of MDE onset (HR = 2.107, p = .12; Table 3).
Secondary Analyses
Influence of Gender
Using Sample 1, we examined Model 1 separately for males and females. The pattern of significant unique stressors did not differ from the full results, except that for males, major interpersonal SLEs did not reach significance, HR = 2.017, 95% CI [0.678, 6.000], p = .207, despite an effect size estimate similar to that for females, HR = 2.350, 95% CI [1.512, 3.654], p < .001. To examine whether the effect of major interpersonal SLEs significantly differed between males and females, we added a Gender × Major Interpersonal SLE interaction to Model 1. This was not significant, HR = 0.834, 95% CI [0.267, 2.599], p = .754, suggesting that the primary results were consistent across gender. Model 2 produced a similar pattern of results (available upon request).
SES and Non-Interpersonal Forms of Stress
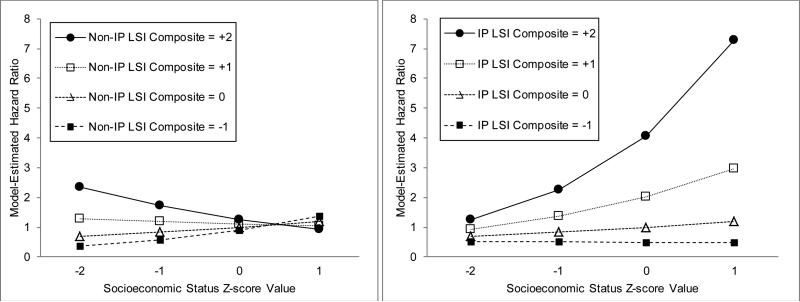
One discrepancy in the results was that non-interpersonal major SLEs and non-interpersonal chronic stress were significant unique predictors in Sample 2, but not Sample 1. We hypothesized that SES might help explain this difference. Indeed, Sample 1 (M = 48.59, SD = 12.56) had slightly but significantly higher SES than Sample 2 (M = 45.86, SD = 13.00; F(1,576) = 5.05, p =.025). We examined whether SES interacts with both interpersonal and non-interpersonal chronic and episodic stress in Sample 1, a test which provided greater power. First, we tested interactions of both interpersonal and non-interpersonal chronic stress with SES in a single model. Non-interpersonal stress became a more potent predictor of MDE onsets as SES declined, HR = 0.78, 95% CI [0.611, 0.995], p = .045, and interpersonal chronic stress became a more potent predictor as SES increased, HR = 1.22, 95% CI [1.002, 1.487], p = .047 (Figure 1).
Figure 1.
Model-estimated hazard ratios for MDE onset from Sample 1 depicting dual two-way interactions between socioeconomic status (SES) and interpersonal chronic stress, and between SES and non-interpersonal chronic stress. IP LSI Z = Interpersonal chronic stress composite z-score; Non-IP LSI Z = Non-interpersonal chronic stress composite z-score. Variable ranges reflect those available in the data.
In a second model, we tested interactions of both interpersonal and non-interpersonal major SLEs with SES. To reduce the number of interaction terms and enhance power, we used the full spectrum of SLE severity (the maximum severity score for each month for each respective type of event, lagged an additional month, and standardized to center variables) rather than dichotomous SLE variables. Non-interpersonal SLEs significantly interacted with SES, becoming a more potent predictor of MDE onsets as SES declined, HR = 0.81, 95% CI [0.716, 0.908], p = .000. However, the potency of interpersonal SLEs appeared to remain consistent across SES, HR = 1.012, 95% CI [.902, 1.136], p = .839.
Deviance Tests of Interpersonal versus Non-Interpersonal Unique Effects
In Sample 1, we examined whether interpersonal forms of stress contributed significantly greater unique variance than non-interpersonal forms of stress using deviance tests. Each compared a model where the unique variance of these forms of stress was constrained to be equal to models where their unique variance was permitted to differ. In a deviance test for chronic stress, the unique variance contributed by interpersonal chronic stress was significantly greater than that contributed by non-interpersonal chronic stress (when constrained to equality −2LL = 2785.67, when unconstrained −2LL = 2779.65, χ2(1) = 6.02, p = 0.014). In a deviance test for SLEs that used dimensional SLE severity to reduce the number of terms, enhance power, and pit interpersonal and non-interpersonal SLEs against each other at identical severity ratings, the unique variance contributed by interpersonal SLEs was significantly greater than that contributed by non-interpersonal SLEs (when constrained to equality −2LL = 2782.27, unconstrained −2LL = 2771.71, χ2(1) = 10.56, p = 0.001).
Temporal Precedence of Chronic Stress
With SLEs, both studies used strategies to ensure temporal precedence of events to episodes. By contrast, chronic stress scores represent an entire interview period. As a result, it is impossible to tease apart the level of chronic stress that occurred just prior to versus after an MDE onset. To ensure the temporal precedence of chronic stress to MDE onsets, we repeated the multivariate analyses of Model 1 with modifications: We utilized the first available chronic stress ratings in each sample (Sample 1: the 12 months prior to the first interview; Sample 2: the first 6 months of the study) and excluded from analyses all person-months covered by these interviews. We also excluded individuals who had an MDE onset prior to the first follow-up period to rule out the possibility that the first available chronic stress ratings were influenced by prior depression.
In Sample 1, 15,294 person-months and 85 depressive episodes were available after exclusions. Interpersonal chronic stress remained a significant unique predictor (HR = 1.669, p = .003), and non-interpersonal chronic stress remained a non-significant unique predictor (HR = 0.811, p = .317). In Sample 2, 4,095 person-months and 52 depressive episodes were available after exclusions. Interpersonal chronic stress (HR = 1.562, p < .05) remained a significant unique predictor, but non-interpersonal chronic stress was no longer significant (HR = 1.364, p = .143), despite a similar effect size estimate in the primary analyses (HR = 1.293).
Effects of Individual Chronic Stress Domains
Although the chronic stress composites simplified interpretation, they may have obscured a unique effect of some non-interpersonal domain in Sample 1 and they did not permit exploration of which domains of chronic stress were most potent. Thus, we re-conducted Model 1 with the domain scores instead of composites. In Sample 1, the non-interpersonal chronic stress domains did not uniquely predict MDEs (HRs 0.88-1.15, ps > .05); among the interpersonal domains, the romantic and family domains contributed significant unique variance (HRs 1.41-1.45, ps < .001), but the best friend and social circle domains did not (HRs 0.98-1.06, ps > .05). In Sample 2, among the non-interpersonal chronic stress domains, the academic domain (HR 1.42, p < .001), but not the work and finances domains (HRs .945–1.01, ps > .05), contributed significant unique variance; among interpersonal chronic stress domains, only the romantic domain contributed significant unique variance (HR 1.28, p < .05; best friend, family and social circle: HRs 1.03 – 1.11, ps > .05.3
Mediation of Adolescent Adversity by Recent Interpersonal Stress in Sample 1
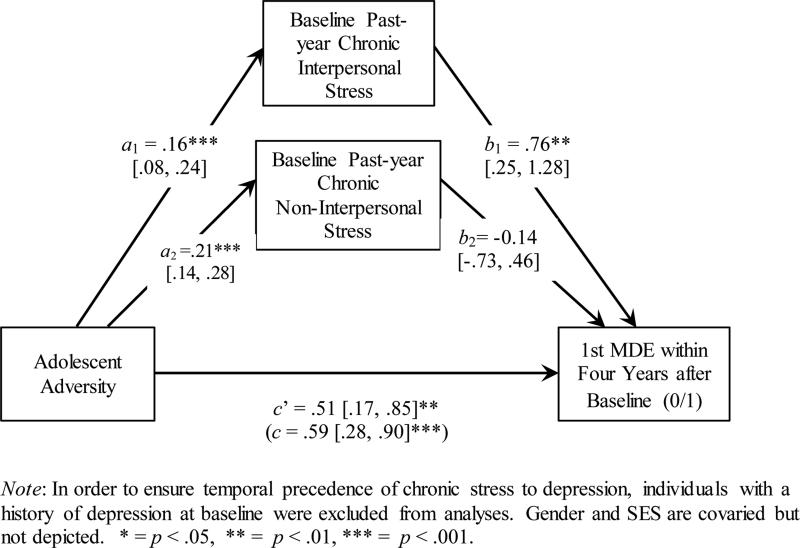
To examine why childhood and adolescent adversity were not significant unique predictors, we tested whether baseline chronic stress mediated the relationship between adolescent adversity and first onsets of MDEs over four annual interviews following baseline. Analyses used the SPSS macro PROCESS, Model 4 to test mediation in logistic regression (Hayes, 2012).4 We focused on adolescent adversity because, in the process of validating the CTI scoring method, we previously showed that adolescent adversity predicts depression over childhood adversity (Vrshek-Schallhorn, Wolitzky-Taylor, et al., 2014). First onset MDEs were predicted to ensure temporal precedence of baseline stress to MDEs. We did not examine SLEs in this model because others have shown they significantly predict depression for up to a few months, not years (e.g., Kendler et al., 1995). Analyses covaried gender and SES. Consistent with recommendations, significance was evaluated using bootstrapped (n = 5000) asymmetric confidence intervals (Hayes, 2012). Significant effects are those not including zero in the 95% confidence interval.
Results indicated that baseline interpersonal (a1b1 = 0.12, SE = 0.06, 95% CI [.03, .26]), but not non-interpersonal (a2b2 = −0.03, SE = 0.06, 95% CI [−.16, .10]) chronic stress mediated the effect of adolescent adversity on first onsets of MDEs (Figure 2). Both the total effect, c = 0.59, SE = 0.16, 95% CI [0.28, 0.90], p = .0002, and the direct effect of adolescent adversity on MDE onsets were significant, c’ = 0.51, SE = 0.17, 95% CI [0.17, 0.85], p = .003, suggesting that there are additional mediators of adolescent adversity on young adult depression.
Figure 2.
Mediation of Adolescent Adversity on First Major Depressive Episodes Onsets by Chronic Stress in Sample 1
Discussion
This study provides novel evidence from two samples that two interpersonal forms of recent stress—major interpersonal SLEs and interpersonal chronic stress—are both significant unique predictors of MDE onsets during emerging adulthood, with partial replication of other results. These findings occurred when simultaneously examining multiple forms of recent chronic stress, episodic month-specific major and minor SLEs, and, in one sample, also early adversity. In addition, follow-up analyses added five findings: a) unique predictors of MDEs did not significantly vary by gender in Sample 1, b) the effects of several forms of stress varied across SES levels, c) interpersonal chronic stress continued to predict MDEs when temporal precedence was strictly enforced, d) in exploratory analyses of chronic stress domains, romantic chronic stress uniquely predicted MDEs across both samples, and e) the effect of adolescent adversity on first onset MDEs was mediated by baseline interpersonal chronic stress in Sample 1. Together, findings reveal which forms of stress contribute significant unique variance to MDEs, and under what circumstances.
Features of Stressors Contributing Unique Variance to Depression
Two features distinguished stressors that contributed significant unique variance to depression risk from those that did not: major severity (of SLEs) and interpersonal nature. First, SLEs that were of major severity—and generally not those of minor severity—contributed significant unique variance to MDE onsets. This further supports the historical focus of the stress-depression research community on major SLEs (e.g., Monroe, 2008). However, based on stress sensitization theory (Monroe & Harkness, 2005; Post, 1992) and evidence (e.g., Stroud et al., 2011), which suggests that less severe events become more potent with increasing recurrences of depression, we cannot rule out that minor events might contribute unique variance among individuals with recurrent depression. Second, consistent with prior theoretical and empirical work (e.g., Hammen, 2005), both episodic and chronic interpersonal stress contributed significant unique variance to MDE onsets. Furthermore, in Sample 1, interpersonal SLEs and chronic stress contributed significantly greater unique variance than their non-interpersonal counterparts. These findings point to the importance of considering interpersonal and non-interpersonal forms of stress separately in future research, and of characterizing vulnerabilities particularly to interpersonal forms of stress.
In contrast, there was no evidence that the potency of major interpersonal SLEs varied as a function of independence, as both major independent and dependent interpersonal SLEs were significant unique predictors of MDE onsets (although the latter effect was only marginal in Sample 2).5 Furthermore, independence did not differentiate whether major non-interpersonal SLEs contributed significant unique variance. Together with mixed evidence for the relative importance of independent versus dependent SLEs (e.g., Kendler et al., 1999; Stroud et al., 2011), this suggests that neither is more important than the other after accounting for the interpersonal status of SLEs. However, it is plausible that they lead to depression via different psychological mechanisms and in concert with different moderators, such as age (e.g., Harkness, Bruce, & Lumley, 2006) or depression history (e.g., Stroud et al., 2011).
Chronic and Episodic Recent Stress
Whether stress was chronic or episodic also did not distinguish whether stressors were significant unique predictors of MDE onsets. Interpersonal chronic stress was a significant unique predictor across both samples, and it contributed significantly greater variance than non-interpersonal chronic stress in follow-up analyses in Sample 1. Moreover, it remained a unique predictor even after establishing the temporal precedence of interpersonal chronic stress to MDE onsets. Further, exploratory analyses indicated that, in both samples, romantic chronic stress was a significant unique predictor of MDE onsets, even though it was not consistently more severe than other domains. This is consistent with research documenting the salience of romantic dysfunction for depression (e.g., Joyner & Udry, 2000; Kendler et al., 1995) and extends it by suggesting that romantic chronic stress (e.g., a poor quality relationship or difficulty initiating any relationship) uniquely predicts depression above and beyond even chronic stress in some other relationships. In comparison to episodic stress, the effects of chronic stress on depression are relatively understudied (e.g., Hammen, 2005), suggesting a renewed focus on interpersonal chronic stress. Further, our analyses assumed that chronic stress contributes to risk in a linear and dimensional fashion, rather than via a quadratic or exponential effect, or a step-function; future research could examine these alternatives.
Mechanisms of Interpersonal Stress on Depression
Findings that interpersonal forms of stress contribute unique variance raise the question of how they act on depression. At a psychological level of analysis, others have argued that interpersonal relationships are integral to the human experience and well-being (e.g., Baumeister & Leary, 1995; Hames, Hagan, & Joiner, 2013). In this view, both acute and chronic factors that threaten an individual's minimum acceptable levels of quality or number of relationships frustrate human needs for belonging and acceptance and have the potential to lead to depression. In some instances, a key emotional mediator appears to be shame (Orth, Berking, & Burkhardt, 2006), consistent with evidence that targeted rejections produce more rapid depression onsets than similarly severe events (Slavich et al., 2009), and with other evidence documenting the importance of humiliation (Brown, Harris, & Hepworth, 1995; Kendler et al., 2003).
At a biological level of analysis, several systems may be differentially sensitive to social threats and isolation, including inflammatory immune responses (e.g., Slavich, O'Donovan, Epel, & Kemeny, 2010), the hypothalamic-pituitary-adrenal axis and its hormone cortisol (e.g., Dickerson & Kemeny, 2004; Doane & Adam, 2010), and the oxytocin and vasopressin systems (Tabak et al., in press). Interestingly, there are bidirectional associations between each of these three systems and the serotonin system (e.g., Dantzer, O'Connor, Lawson, & Kelley, 2011; Insel & Winslow, 1998; Miller, Wankerl, Stalder, Kirschbaum, & Alexander, 2013), and there is also evidence that serotonergic vulnerability moderates interpersonal but not non-interpersonal major SLEs (Vrshek-Schallhorn, Mineka, et al., 2014). Thus, future research should examine how these systems act independently and collectively to confer vulnerability to interpersonal stress.
Effects of Stress Type Vary by SES
In addition to these potential psychobiological mechanisms of stress on depression, interaction results also suggest that mechanisms of stress partly differ as a function of SES—with one pathway characterized by a greater role for interpersonal chronic stress in higher SES conditions, and one by a relatively greater role for non-interpersonal chronic stress and major SLEs in lower SES conditions. This pattern is consistent with at least one model of risk under poor SES conditions, in which hopelessness emerges from a vicious cycle of learning to expect negative outcomes, elevated chronic stress, and reduced ability to cope with novel stressors (Kristenson, Eriksen, Sluiter, Starke, & Ursin, 2004). This model and the interaction of SES with non-interpersonal SLEs suggest that lower SES might be associated with having fewer resources to address the sequelae of non-interpersonal stressors (e.g., to pay medical bills following an injury or illness), and that this likely generates additional chronic stress. Also, SES and chronic non-interpersonal stress were negatively correlated (Table 2), indicating that more severe levels are increasingly common as SES declines. In contrast to these interactions, major interpersonal SLEs did not significantly interact with SES, indicating they remain threatening irrespective of SES.
Indirect Action of Early Adversity via Chronic Interpersonal Stress
Neither childhood nor adolescent adversity conferred significant unique risk for MDE onsets. Prior work showed that early adversity predicts later chronic and episodic stress (Hammen, Hazel, Brennan, & Najman, 2012), and that recent stress mediates the effects of early adversity on later depression (Hazel et al., 2008). We replicated and extended this latter finding in showing that interpersonal, but not non-interpersonal, chronic stress significantly mediated the association between earlier adversity and later first onsets of depression. After accounting for this, the direct path of adolescent depression remained significant, suggesting other mediators. For example, although it was not feasible to test whether SLEs also mediated this relationship in the present study as tests of mediation for survival models need to be further developed, it is likely that this is the case (e.g., Hammen et al., 2012). Future work should examine predictors of interpersonal stress continuation and develop interventions that interrupt it; one possible target may be adult attachment style, which has also been shown to mediate the relationship between early adversity and later depression (Bifulco et al., 2006).
Role of Gender and Developmental Context
Results may have been influenced by either the gender (Sample 1, 68.5% females; Sample 2, all females) or the emerging adult developmental stage of participants. First, however, in separate analyses for males and females in Sample 1, the overall pattern of significant unique predictors suggested no marked differences across gender. Prior work conflicts on this question, with some showing greater vulnerability to certain stressors for adolescent girls versus boys (e.g., Rudolph & Hammen, 1999) but others showing no difference in stress vulnerability by gender (e.g., Kendler et al., 2003). These results are preliminary, given that Sample 1 included only a small percentage of males with a low number of MDEs. Future work should examine unique environmental predictors of MDEs in males.
Second, prior research has shown that emerging adults have more stressful life events than other developmental periods, which may influence the relative importance of SLEs versus chronic stress. In one example that also demonstrated gender effects, Harkness and colleagues (2010) showed that as compared to emerging adult (age 18-29) males, their female counterparts reported greater numbers of several kinds of SLEs prior to depression—an effect that was attenuated or absent in other age groups. This suggests that events may be more important for depression among emerging adults (e.g., age 18-29), particularly females, than for those in other developmental periods. Thus, multivariate studies in a younger or older sample might demonstrate less unique variance from major SLEs than observed in the present sample. However, consistent with interpersonal theories of depression (e.g., Coyne & Downey, 1991; Hammen, 2005), we suggest that interpersonal factors are integral regardless of developmental stage. Indeed, we predict that interpersonal stress will have more robust effects than non-interpersonal stress throughout the lifespan.
Strengths and Limitations
The present study has several strengths including two independent datasets with heavily overlapping measures and designs, the use of longitudinal designs and repeated interview measures of both stress and depression, the use of month-specific survival models, and addressing temporal precedence of both SLEs and chronic stress. However, there are also limitations. First, neither sample was representative of the general population. Sample 1 was oversampled for high neuroticism in an effort to increase the number of observed prospective onsets of emotional disorders. However, a simulation study showed that oversampling does not bias regression estimates (Hauner, Zinbarg, & Revelle, 2014), and covarying neuroticism did not alter the overall pattern of results. Likewise, Sample 2 comprised only females; however, secondary analyses conducted separately by gender in Sample 1 support that the uniquely contributing forms of stress do not substantially vary between males and females. Despite this, replication in a representative sample—especially one with wide-ranging SES—would be beneficial.
Second, there were four additional potentially influential methods discrepancies between the samples. 1) The a priori severity cutoff for major SLEs differed by 0.5 points (10% of the scale); however, similar proportions of SLEs classified as major in each sample—and similar results across the samples—suggest this did not lead to marked differences in results. 2) The interpersonal status of SLEs was assigned differently, but this seems more likely to have led to discrepant results rather than spurious similarities; similar rates of interpersonal SLEs between studies suggest this had little impact. 3) Only Sample 1 included neighborhood chronic stress in the non-interpersonal composite variable. Omitting neighborhood from the Sample 1 non-interpersonal stress composite did not change the pattern of results or the significance of the unique variance of non-interpersonal chronic stress (Model 1: HR = 1.004, p = .973). 4) Analyses included a measure of early adversity for Sample 1 only, but given the lack of significant unique contributions by early adversity in Sample 1, this is unlikely to have strongly influenced Sample 2 results. Thus, the downside of using two samples not originally designed for this purpose is slight differences in methodological details. The benefit, however, is showing in two samples that major interpersonal SLEs and chronic interpersonal stress contribute significant unique variance, plus the tempering evidence that other forms of stress will at times also be significant unique predictors, as occurred in Sample 2.
Third, our approach examines the individual main effects of stressors, rather than either synergistic effects of stress or vulnerability by stressor interactions. Indeed, prior research demonstrates stress sensitization processes (synergistic effects) via interactions between early adversity and later SLEs (Hammen et al., 2000; Harkness et al., 2006; Slavich, Monroe, & Gotlib, 2011), and between chronic stress and burden of SLEs (Hammen, Kim, Eberhart, & Brennan, 2009). However, in studies of how biological vulnerabilities (e.g., genotypes) moderate the effects of stress, it is common to examine interactions between a biological variable and a single form of stress, necessitating guidance about which form to examine. Further, challenges for examining vulnerability-stress interactions in multivariate models—with the potential of introducing up to 9 interaction terms, yielding up to 18 total stress-related predictors—include difficulties with interpretation and a strong need for theory-driven a priori hypotheses. However, future work might examine whether unique contributions of stress differ in first onsets versus recurrences of MDEs, or for individuals with prior anxiety disorders, or for individuals at elevated genetic risk (e.g., based on family history). The current approach also does not examine the cumulative effects of stressors because there is no accepted approach to aggregate multiple forms and time courses of stress. Nonetheless, examining individual main effects reveals which contribute significant unique variance on average, which is likely to be useful to future research.
A final limitation is that the results can tell us little about the means by which certain stressors emerge as unique predictors over and above other stressors. Individuals may be more sensitive to certain stressors, or certain stressors may simply tend to occur at more severe levels than other stressors—or both may contribute. Given that these are not mutually exclusive possibilities (i.e., tests of one possibility do not also rule out the other), and that tests of differences in stressor severity are not valid in many cases (e.g., comparing SLEs and chronic stress), this is an intriguing issue for future research.
Conclusion
Together, these results provide robust evidence that very negative, impactful interpersonal events and levels of interpersonal chronic stress predict MDE onsets over and above other forms of stress, including several non-interpersonal forms of stress. By contrast, whether stressful events were caused by the person or were instead independent of the person's behavior was not a key factor. Results suggest that a focus on individual differences in vulnerability to interpersonal stress and the mechanistic pathways of interpersonal stress will be fruitful for etiological research.
Acknowledgments
This research was supported by a two-site grant from the National Institute of Mental Health to SM and REZ (R01-MH065652) and to MGC (R01-MH065651); a Postdoctoral NRSA from the National Institute of Mental Health (F32-MH091955) and later institutional funds from UNCG to SVS; and a grant from the William T. Grant Foundation to CH. CBS was supported by institutional funds from Williams College.
Footnotes
A portion of these data were presented by the first author at the 2013 annual meeting of the Society for Research in Psychopathology, and a different portion by the second author at the 2014 annual meeting of the Association for Behavioral and Cognitive Therapies. The content is the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health.
The authors declare no conflicts of interest.
Lay Summary required for JAP Revisions: Interpersonal forms of stress consistently predict depressive episode onsets over and above other correlated forms of stress, and interpersonal chronic stress mediates the effect of childhood adversity on later depression.
In Samples 1 and 2, when an indicator of minority race or ethnicity was added to Models 1 and 2, the overall pattern of significant results did not change, nor was this covariate a significant predictor of MDE onsets. In Sample 1, when neuroticism was covaried in Models 1 and 2, the pattern of significant unique stressors did not change, and neuroticism was a robust predictor of MDE onses (HR = 1.83-1.85, ps <.001). Neuroticism was not measured in Sample 2.
In Sample 1, when SLEs were split on severity and independence but not interpersonal status, both major dependent (HR = 1.878, p =.005) and major independent SLEs (HR =2.270, p =.000) contributed significant unique variance, in addition to chronic interpersonal stress. In Sample 2, both major dependent (HR = 1.843, p = .034) and major independent SLEs (HR = 3.893, p =.000) and minor independent SLEs (HR =1.896, p = .002) contributed significant unique variance in addition to interpersonal and non-interpersonal chronic stress as before. These results, which are consistent across samples other than the finding for minor independent SLEs in Sample 2, provides further support that independence does not differentiate unique predictors from non-significant ones.
To examine whether uniquely predicting interpersonal chronic stress domains were more severe than the remaining domains, we aggregated raw interpersonal chronic stress across the five years and conducted repeated measures ANOVAs. In Sample 1, an omnibus test of all four domains revealed that severity differed by domain, F(1,431) = 216.26, p < .001. Follow up tests showed that in each case, family and romantic domains had higher scores than did the best friend and social circle domains, all Fs(1,431) ≥ 84.39, ps < .001, except for the romantic and social domain comparison, F(1,431) = 2.43, p = .120. In Sample 2, an omnibus test of all four domains revealed that severity differed by domain, F(1,146) = 16.475, p < .001. Follow up tests showed that the romantic domain had higher scores than the best friend and social circle domains, all Fs(1,146) ≥ 18.181, ps < .001, but not the family domain, F(1,146) = .330, p = .566. Together, these results are only partially consistent with the explanation that the domains that emerged as unique predictors were more severe than other domains.
Mediation methods have not yet been extended to Cox regression with repeated events and continuous, time-varying mediators.
Although some events were less common, particularly when SLEs were split on three distinctions, significant associations of less common SLEs with MDE onsets prior to accounting for other forms of stress support that power was more than adequate.
Contributor Information
Suzanne Vrshek-Schallhorn, Northwestern University and University of North Carolina at Greensboro.
Catherine B. Stroud, Williams College
Susan Mineka, Northwestern University.
Constance Hammen, University of California – Los Angeles.
Richard Zinbarg, Northwestern University and the Family Institute at Northwestern University.
Kate Wolitzky-Taylor, University of California – Los Angeles.
Michelle G. Craske, University of California – Los Angeles
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. Fourth Edition, Text Revision American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Baumeister RF, Leary MR. The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin. 1995;117(3):497–529. [PubMed] [Google Scholar]
- Bifulco A, Kwon J, Jacobs C, Moran PM, Bunn A, Beer N. Adult attachment style as mediator between childhood neglect/abuse and adult depression and anxiety. Social psychiatry and psychiatric epidemiology. 2006;41(10):796–805. doi: 10.1007/s00127-006-0101-z. [DOI] [PubMed] [Google Scholar]
- Brown G, Harris T. Social origins of depression: A study of psychiatric disorder in women. Tavistock Publications Limited; Oxfordshire: 1978. [Google Scholar]
- Brown G, Harris TO, Hepworth C. Loss, humiliation and entrapment among women developing depression: A patient and non-patient comparison. Psychological Medicine. 1995;25(1):7–21. doi: 10.1017/s003329170002804x. [DOI] [PubMed] [Google Scholar]
- Cole MG, Dendukuri N. Risk factors for depression among elderly community subjects: A systematic review and meta-analysis. American Journal of Psychiatry. 2003;160(6):1147–1156. doi: 10.1176/appi.ajp.160.6.1147. [DOI] [PubMed] [Google Scholar]
- Coyne JC, Downey G. Social factors and psychopathology: Stress, social support, and coping processes. Annual Review of Psychology. 1991;42(1):401–425. doi: 10.1146/annurev.ps.42.020191.002153. [DOI] [PubMed] [Google Scholar]
- Dantzer R, O'Connor JC, Lawson MA, Kelley KW. Inflammation-associated depression: from serotonin to kynurenine. Psychoneuroendocrinology. 2011;36(3):426–436. doi: 10.1016/j.psyneuen.2010.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davila J, Hammen C, Burge D, Paley B, Daley SE. Poor interpersonal problem solving as a mechanism of stress generation in depression among adolescent women. Journal of Abnormal Psychology. 1995;104(4):592–600. doi: 10.1037//0021-843x.104.4.592. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychological Bulletin. 2004;130(3):355–391. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- Doane LD, Adam EK. Loneliness and cortisol: Momentary, day-to-day, and trait associations. Psychoneuroendocrinology. 2010;35(3):430–441. doi: 10.1016/j.psyneuen.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eysenck SBG, Eysenck HJ, Barrett P. A revised version of the psychoticism scale. Personality and Individual Differences. 1985;6:21–29. [Google Scholar]
- Fink L, Bernstein D, Handelsman L, Foote J, Lovejoy M. Initial reliability and validity of the Childhood Trauma Interview: A new multidimensional measure of childhood interpersonal trauma. American Journal of Psychiatry. 1995;152(9):1329–1335. doi: 10.1176/ajp.152.9.1329. [DOI] [PubMed] [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSMIV-TR Axis I Disorders--Non-patient Edition. New York State Psychiatric Institute, Biometrics Research Department; New York: 2001. [Google Scholar]
- Gilman SE, Kawachi I, Fitzmaurice G, Buka S. Socio-economic status, family disruption and residential stability in childhood: Relation to onset, recurrence and remission of major depression. Psychological Medicine. 2003;33(8):1341–1355. doi: 10.1017/s0033291703008377. [DOI] [PubMed] [Google Scholar]
- Groh AM, Roisman GI, van IJzendoorn MH, Bakermans-Kranenburg MJ, Fearon R. The Significance of insecure and disorganized attachment for children's internalizing symptoms: A meta-analytic study. Child Development. 2012;83(2):591–610. doi: 10.1111/j.1467-8624.2011.01711.x. [DOI] [PubMed] [Google Scholar]
- Hames JL, Hagan CR, Joiner TE. Interpersonal processes in depression. Annual Review of Clinical Psychology. 2013;9:355–377. doi: 10.1146/annurev-clinpsy-050212-185553. [DOI] [PubMed] [Google Scholar]
- Hammen C. Interpersonal stress and depression in women. Journal of Affective Disorders. 2003;74(1):49–57. doi: 10.1016/s0165-0327(02)00430-5. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annual Review of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress generation in depression: Reflections on origins, research, and future directions. Journal of clinical psychology. 2006;62(9):1065–1082. doi: 10.1002/jclp.20293. [DOI] [PubMed] [Google Scholar]
- Hammen C, Adrian C, Gordon D, Burge D, Jaenicke C, Hiroto D. Children of depressed mothers: Maternal strain and symptom predictors of dysfunction. Journal of Abnormal Psychology. 1987;96(3):190–198. doi: 10.1037//0021-843x.96.3.190. [DOI] [PubMed] [Google Scholar]
- Hammen C, Hazel N, Brennan P, Najman J. Intergenerational transmission and continuity of stress and depression: Depressed women and their offspring in 20 years of follow-up. Psychological Medicine. 2012;42(05):931–942. doi: 10.1017/S0033291711001978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C, Henry R, Daley S. Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology. 2000;68(5):782–787. [PubMed] [Google Scholar]
- Hammen C, Kim E, Eberhart N, Brennan P. Chronic and acute stress and the prediction of major depression in women. Depression and Anxiety. 2009;26(8):718–723. doi: 10.1002/da.20571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C, Marks T, Mayol A, DeMayo R. Depressive self-schemas, life stress, and vulnerability to depression. Journal of Abnormal Psychology. 1985;94(3):308–319. doi: 10.1037//0021-843x.94.3.308. [DOI] [PubMed] [Google Scholar]
- Hammen C, Mayol A, DeMayo R, Marks T. Initial symptom levels and the life-event–depression relationship. Journal of Abnormal Psychology. 1986;95(2):114–122. doi: 10.1037//0021-843x.95.2.114. [DOI] [PubMed] [Google Scholar]
- Harkness K, Alavi N, Monroe S, Slavich G, Gotlib I, Bagby RM. Gender differences in life events prior to onset of major depressive disorder: The moderating effect of age. Journal of Abnormal Psychology. 2010;119(4):791–803. doi: 10.1037/a0020629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkness K, Bruce A, Lumley M. The role of childhood abuse and neglect in the sensitization to stressful life events in adolescent depression. Journal of Abnormal Psychology. 2006;115(4):730–741. doi: 10.1037/0021-843X.115.4.730. [DOI] [PubMed] [Google Scholar]
- Hauner K, Zinbarg R, Revelle W. A latent variable model approach to estimating systematic bias in the oversampling method. Behavior Research Methods. 2014;46:786–797. doi: 10.3758/s13428-013-0402-6. [DOI] [PubMed] [Google Scholar]
- Hayes AF. [November 3, 2014];PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White Paper] 2012 from http://www.afhayes.com/public/process2012.pdf.
- Hazel N, Hammen C, Brennan P, Najman J. Early childhood adversity and adolescent depression: The mediating role of continued stress. Psychological Medicine. 2008;38(4):581–589. doi: 10.1017/S0033291708002857. [DOI] [PubMed] [Google Scholar]
- Hollingshead A. Four factor index of social status. Unpublished manuscript. Yale University; New Haven, CT.: 1975. [Google Scholar]
- Insel TR, Winslow JT. Serotonin and neuropeptides in affiliative behaviors. Biological psychiatry. 1998;44(3):207–219. doi: 10.1016/s0006-3223(98)00094-8. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Metalsky GI. A prospective test of an integrative interpersonal theory of depression: A naturalistic study of college roommates. Journal of Personality and Social Psychology. 1995;69(4):778–788. doi: 10.1037//0022-3514.69.4.778. [DOI] [PubMed] [Google Scholar]
- Joyner K, Udry JR. You don't bring me anything but down: Adolescent romance and depression. Journal of Health and Social Behavior. 2000;41(4):369–391. [PubMed] [Google Scholar]
- Kendler K, Hettema JM, Butera F, Gardner CO, Prescott CA. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Archives of General Psychiatry. 2003;60(8):789–796. doi: 10.1001/archpsyc.60.8.789. [DOI] [PubMed] [Google Scholar]
- Kendler K, Karkowski L, Prescott C. Stressful life events and major depression: Risk period, long-term contextual threat, and diagnostic specificity. Journal of Nervous and Mental Disease. 1998;186(11):661–669. doi: 10.1097/00005053-199811000-00001. [DOI] [PubMed] [Google Scholar]
- Kendler K, Karkowski L, Prescott C. Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry. 1999;156(6):837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- Kendler K, Kessler R, Walters E, MacLean C, Neale M, Heath A, Eaves L. Stressful life events, genetic liability, and onset of an episode of major depression in women. American Journal of Psychiatry. 1995;152(6):833–842. doi: 10.1176/ajp.152.6.833. [DOI] [PubMed] [Google Scholar]
- Kessler R, Davis CG, Kendler K. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychological Medicine. 1997;27(05):1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Kristenson M, Eriksen HR, Sluiter JK, Starke D, Ursin H. Psychobiological mechanisms of socioeconomic differences in health. Social Science & Medicine. 2004;58(8):1511–1522. doi: 10.1016/S0277-9536(03)00353-8. [DOI] [PubMed] [Google Scholar]
- Lenze S, Cyranowski JM, Thompson WK, Anderson B, Frank E. The cumulative impact of nonsevere life events predicts depression recurrence during maintenance treatment with interpersonal psychotherapy. Journal of Consulting and Clinical Psychology. 2008;76(6):979–987. doi: 10.1037/a0012862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorant V, Deliège D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: A meta-analysis. American Journal of Epidemiology. 2003;157(2):98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Weisz JR, Wood JJ. Examining the association between parenting and childhood depression: A meta-analysis. Clinical Psychology Review. 2007;27(8):986–1003. doi: 10.1016/j.cpr.2007.03.001. [DOI] [PubMed] [Google Scholar]
- Miller R, Wankerl M, Stalder T, Kirschbaum C, Alexander N. The serotonin transporter gene-linked polymorphic region (5-HTTLPR) and cortisol stress reactivity: A meta-analysis. Molecular Psychiatry. 2013;18:1018–1024. doi: 10.1038/mp.2012.124. doi: 10.1038/mp.2012.124. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Taylor A, Kokaua J, Milne B, Polanczyk G, Poulton R. How common are common mental disorders? Evidence that lifetime prevalence rates are doubled by prospective versus retrospective ascertainment. Psychological Medicine. 2010;40(06):899–909. doi: 10.1017/S0033291709991036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe S. Modern approaches to conceptualizing and measuring human life stress. Annual Review of Clinical Psychology. 2008;4:33–52. doi: 10.1146/annurev.clinpsy.4.022007.141207. [DOI] [PubMed] [Google Scholar]
- Monroe S, Harkness K. Life stress, the “kindling” hypothesis, and the recurrence of depression: Considerations from a life stress perspective. Psychological review. 2005;112(2):417–444. doi: 10.1037/0033-295X.112.2.417. [DOI] [PubMed] [Google Scholar]
- Monroe S, Torres L, Guillaumot J, Harkness K, Roberts J, Frank E, Kupfer D. Life stress and the long-term treatment course of recurrent depression: III. Nonsevere life events predict recurrence for medicated patients over 3 years. Journal of Consulting and Clinical Psychology. 2006;74(1):112–120. doi: 10.1037/0022-006X.74.1.112. [DOI] [PubMed] [Google Scholar]
- Orth U, Berking M, Burkhardt S. Self-conscious emotions and depression: Rumination explains why shame but not guilt is maladaptive. Personality and Social Psychology Bulletin. 2006;32(12):1608–1619. doi: 10.1177/0146167206292958. [DOI] [PubMed] [Google Scholar]
- Paykel E, Mangen S. Interview for recent life events. St. George's Hospital Medical School; London: 1980. [Google Scholar]
- Post R. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. American Journal of Psychiatry. 1992;149(8):999. doi: 10.1176/ajp.149.8.999. [DOI] [PubMed] [Google Scholar]
- Romeo RD. Adolescence: A central event in shaping stress reactivity. Developmental Psychobiology. 2010;52(3):244–253. doi: 10.1002/dev.20437. [DOI] [PubMed] [Google Scholar]
- Rudolph KD, Hammen C. Age and gender as determinants of stress exposure, generation, and reactions in youngsters: A transactional perspective. Child Development. 1999;70(3):660–677. doi: 10.1111/1467-8624.00048. [DOI] [PubMed] [Google Scholar]
- Sheets E, Craighead W. Comparing chronic interpersonal and noninterpersonal stress domains as predictors of depression recurrence in emerging adults. Behaviour Research and Therapy. 2014;63:36–42. doi: 10.1016/j.brat.2014.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Link BG, Dohrenwend BP, Skodol AE, Stueve A, Mirotznik J. Characterizing life events as risk factors for depression: The role of fateful loss events. Journal of Abnormal Psychology. 1989;98(4):460–467. doi: 10.1037//0021-843x.98.4.460. [DOI] [PubMed] [Google Scholar]
- Singer J, Willett J. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press; USA: 2003. [Google Scholar]
- Slavich G, Monroe S, Gotlib I. Early parental loss and depression history: Associations with recent life stress in major depressive disorder. Journal of Psychiatric Research. 2011;45(9):1146–1152. doi: 10.1016/j.jpsychires.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich G, O'Donovan A, Epel ES, Kemeny ME. Black sheep get the blues: A psychobiological model of social rejection and depression. Neuroscience & Biobehavioral Reviews. 2010;35(1):39–45. doi: 10.1016/j.neubiorev.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavich G, Thornton T, Torres LD, Monroe S, Gotlib I. Targeted rejection predicts hastened onset of major depression. Journal of Social and Clinical Psychology. 2009;28(2):223–243. doi: 10.1521/jscp.2009.28.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First M. Structured Clinical Interview for DSM-III-R—Non-Patient Edition (SCID-NP, Version 1.0) American Psychiatric Press; Washington, DC: 1990. [Google Scholar]
- Stroud CB, Davila J, Hammen C, Vrshek-Schallhorn S. Severe and nonsevere events in first onsets versus recurrences of depression: Evidence for stress sensitization. Journal of Abnormal Psychology. 2011;120(1):142–154. doi: 10.1037/a0021659. [DOI] [PubMed] [Google Scholar]
- Stroud CB, Davila J, Moyer A. The relationship between stress and depression in first onsets versus recurrences: A meta-analytic review. Journal of Abnormal Psychology. 2008;117(1):206–213. doi: 10.1037/0021-843X.117.1.206. [DOI] [PubMed] [Google Scholar]
- Sullivan P, Neale M, Kendler K. Genetic epidemiology of major depression: Review and meta-analysis. American Journal of Psychiatry. 2000;157(10):1552–1562. doi: 10.1176/appi.ajp.157.10.1552. [DOI] [PubMed] [Google Scholar]
- Surtees P, Wainwright N. Surviving adversity: Event decay, vulnerability and the onset of anxiety and depressive disorder. European Archives of Psychiatry and Clinical Neuroscience. 1999;249(2):86–95. doi: 10.1007/s004060050071. [DOI] [PubMed] [Google Scholar]
- Tabak B, Vrshek-Schallhorn S, Zinbarg R, Prenoveau J, Mineka S, Redei E, Craske M. Interaction of CD38 variant and chronic interpersonal stress is associated with social anxiety and depression symptoms over six years. Clinical Psychological Science. doi: 10.1177/2167702615577470. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uliaszek AA, Zinbarg RE, Mineka S, Craske MG, Griffith JW, Sutton JM, Hammen C. A longitudinal examination of stress generation in depressive and anxiety disorders. Journal of Abnormal Psychology. 2012;121(1):4–15. doi: 10.1037/a0025835. [DOI] [PubMed] [Google Scholar]
- Vrshek-Schallhorn S, Mineka S, Zinbarg R, Craske M, Griffith J, Sutton J, Adam EK. Refining the candidate environment: Interpersonal stress, the serotonin transporter polymorphism, and gene-environment interactions in major depression. Clinical Psychological Science. 2014;2(3):235–248. doi: 10.1177/2167702613499329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vrshek-Schallhorn S, Wolitzky-Taylor K, Doane L, Epstein A, Sumner J, Mineka S, Adam E. Validating new summary indices for the Childhood Trauma Interview: Associations with first onsets of major depressive disorder and anxiety disorders. Psychological Assessment. 2014;26(3):730–740. doi: 10.1037/a0036842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whisman MA. The association between marital dissatisfaction and depression. In: Beach S, editor. Marital and family processes in depression: A scientific foundation for clinical practice. American Psychological Association; Washington, DC: 2001. pp. 3–24. [Google Scholar]
- Zinbarg R, Mineka S, Craske M, Griffith J, Sutton J, Rose R, Waters A. The Northwestern-UCLA Youth Emotion Project: Associations of cognitive vulnerabilities, neuroticism and gender with past diagnoses of emotional disorders in adolescents. Behaviour Research and Therapy. 2010;48(5):347–358. doi: 10.1016/j.brat.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]