Abstract
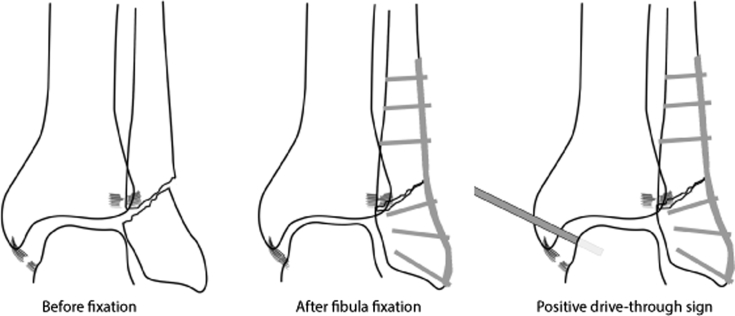
Standalone open reduction–internal fixation (ORIF) of unstable ankle fractures is the current standard of care. Intraoperative stress radiographs are useful for assessing the extent of ligamentous disruption, but arthroscopic visualization has been shown to be more accurate. Concomitant arthroscopy at the time of ankle fracture ORIF is useful for accurately diagnosing and managing syndesmotic and deltoid ligament injuries. The arthroscopic ankle drive-through sign is characterized by the ability to pass a 2.9-mm shaver (Smith & Nephew, Andover, MA) easily through the medial ankle gutter during arthroscopy, which is not usually possible with both an intact deltoid ligament and syndesmosis. This arthroscopic maneuver indicates instability after ankle reduction and fixation and is predictive of the need for further stabilization. Furthermore, when this sign remains positive after fracture fixation, it may guide the surgeon to further evaluate the adequacy of fixation for the possible need for further fixation of the syndesmosis or deltoid. We present the case of an ankle fracture managed with arthroscopy-assisted ORIF and describe the clinical utility of the arthroscopic ankle drive-through sign.
Open reduction–internal fixation (ORIF) has been the standard of care in the treatment of unstable fractures about the ankle. Rotational patterns of ankle fractures (especially supination–external rotation type IV) are often associated with ligamentous injuries that, without adequate stabilization, may lead to continued ankle pain, disability, and eventual progression to arthritis.1 Fixation of the fibula restores the length and alignment of the ankle, but fibula fixation alone may be insufficient to ensure stability of the ankle mortise. After fixation of the fibula, intraoperative stress radiographs are commonly used to assess for syndesmotic stability.2 Disruption of the syndesmosis or deltoid may compromise the ultimate clinical outcome, particularly if the talus is allowed to subluxate with respect to the tibia. Ramsey and Hamilton3 showed that a 1-mm shift led to a 42% increase in contact stress. Thus the anatomic reduction is critical to the long-term health of the ankle.
Intraoperative ligamentous evaluation of ankle fractures is typically performed with stress radiographs, although it has been shown that direct visualization through arthroscopy is more sensitive to detect pathology because of the ability to perform a more thorough and direct examination.4, 5 Moreover, it can be very difficult to assess 1 to 2 mm of malreduction of the ankle with mini-fluoroscopy or C-arm fluoroscopy. In addition, the best assessment of the syndesmotic reduction is performed with axial imaging of the ankle, best provided by computed tomography, because traditional radiographs often underestimate this malreduction.6, 7 Arthroscopic evaluation after ankle fracture shows a high prevalence of intra-articular pathology, although correlation with outcomes has been mixed.8, 9, 10 There has yet to be an arthroscopic sign to characterize ankle instability intraoperatively. For the shoulder, the arthroscopic shoulder drive-through sign, originally reported by Pagnani and Warren,11 is positive when the camera is easily passed between the glenoid and the humeral head into the anteroinferior joint space, which indicates laxity of the anterior capsule, usually after shoulder dislocation. After adequate repair and tightening of the labral-inferior glenohumeral ligament complex, the drive-through sign is eliminated.12
With the increased use of ankle arthroscopy, the role of arthroscopy in the treatment of acute ankle fractures is becoming more appreciated.13 Thus there is a potential benefit to identifying ways to arthroscopically evaluate ankle instability. We have identified a diagnostic maneuver for use during ankle arthroscopy—the arthroscopic ankle drive-through sign.
The arthroscopic ankle drive-through sign is an intraoperative finding characterized by the ability to easily pass an arthroscopic shaver through the medial ankle gutter between the medial malleolus and the talus without scuffing the articular cartilage on either side. In our experience, it is not possible to perform this maneuver in well-reduced and stable ankles. The senior author (M.C.D.) has performed over 500 ankle arthroscopies and has been unable to perform this maneuver in an ankle without a significant syndesmotic injury or in fibula fractures with a medial-sided injury (deltoid rupture or medial malleolus fracture). The presence of the arthroscopic drive-through sign indicates instability due to syndesmotic or deltoid injury and can be a useful adjunct intraoperatively to evaluate ankle stability before and after fixation of the fibula.
The purpose of this technical note is to provide an overview of the technique for performing ankle arthroscopy concomitantly with ORIF for ankle fractures. We describe the utility of the arthroscopic ankle drive-through sign in the intraoperative diagnosis of ankle ligamentous injury (Table 1, Table 2, Table 3).
Table 1.
Benefits of Arthroscopic Drive-through Sign
| The arthroscopic drive-through sign is an easy and reproducible maneuver to identify instability of the syndesmosis. |
| After fixation of the syndesmosis, the sign becomes negative, a dynamic change indicating successful reduction and fixation of the syndesmosis. |
| Ankle arthroscopy in the setting of ankle fracture provides the opportunity to directly visualize and treat potential cartilage injuries, as well as to remove tissue and loose bodies that may hinder adequate reduction of the ankle. |
Table 2.
Technical Pearls
| The patient is positioned supine with the ipsilateral hip elevated using a bump to provide easier access to the lateral fibula. |
| A tourniquet is placed around the thigh. |
| Manual distraction is applied to the ankle, which is usually already quite lax in the setting of an unstable fracture. |
| A 30° arthroscope is inserted into the anterolateral portal. During arthroscopy, the surgeon should evaluate for cartilage injuries and loose bodies that may prevent adequate reduction. |
| The drive-through test is performed by attempting to pass the 2.9-mm shaver from the anteromedial portal between the medial malleolus and the medial talar dome. The test is usually positive at this point because of the fibula fracture, but performing the test now establishes a base case to compare with after the fibula is repaired. |
| Open reduction–internal fixation is performed. |
| The surgeon returns to arthroscopy and performs the drive-through sign again. If the shaver passes easily, the drive-through sign is positive, and further fixation of the syndesmosis is then performed. |
| After syndesmosis fixation, the arthroscope and shaver are again reinserted and the drive-through test is performed. A negative test indicates that the syndesmosis has been adequately reduced and fixed, whereas a test that continues to be positive should raise suspicion for inadequate reduction and/or fixation of the fibula and syndesmosis. |
Table 3.
Pitfalls
| Establishing arthroscopic portals requires care to avoid damage to the neurovascular structures—the tibialis anterior and saphenous nerve/vein are at risk with the anteromedial portal, whereas the intermediate dorsal cutaneous branch of the superficial peroneal nerve is at risk with the anterolateral portal. |
| The surgeon should remove the arthroscope during fixation of the ankle and the syndesmosis to ensure there are no blocks to reduction. |
| It is important to monitor total arthroscopic time to minimize fluid extravasation in the surrounding soft tissues. |
| The drive-through sign should be performed carefully, with minimal force, to avoid cartilage injury while attempting to drive the camera between the medial malleolus and the medial talar dome. Performing a standard external rotation test in addition to the drive-through sign will help establish a feeling of laxity to expect during positive and negative tests. |
Surgical Technique
After appropriate regional or general anesthesia (or both) has been administered, the patient is placed in a supine position with an ipsilateral bump to position the patella and foot pointing directly vertically. The down surfaces are carefully padded with the down leg secured, and the operative field is sterilely prepared and draped. For non-trauma ankle arthroscopies, the ankle joint is typically insufflated or distraction is applied (or both); however, for ankle arthroscopy associated with acute ankle fractures, the ankle joint is easily accessible without using distraction. Before the skin incision, a non-sterile tourniquet is raised to 250 mm Hg and the entire case is performed with the tourniquet inflated as time allows. After this, the proper portals and incision for the fibula fixation are marked (Fig 1).
Fig 1.
Unstable ankle. After fixation of the fibula fracture, the arthroscopic drive-through sign should be performed. If the syndesmosis is incompetent, the talus is unstable within the mortise. The arthroscopic shaver will be easily inserted between the medial malleolus and the talar dome, indicating a positive drive-through sign.
Step 1
The anteromedial portal is established just medial to the tibialis anterior tendon and lateral to the lateral aspect of the medial malleolus, with care taken to avoid the saphenous vein and nerve.
Step 2
The anterolateral portal is established in the soft spot between the lateral malleolus and the peroneus tertius tendon. When the surgeon is establishing this portal, the intermediate dorsal cutaneous branch of the superficial peroneal nerve is at risk; with fine palpation, this superficial structure may sometimes be identified, with care then taken to avoid injury. With both the anteromedial and anterolateral portals established, the anteromedial portal is initially used as the viewing portal whereas the anterolateral portal is used as the working portal. Very often there is a hematoma that is easily evacuated by this technique. Fibula fractures at the level of the mortise can typically be visualized from the anteromedial portal, and a shaver placed through the anterolateral portal is used to debride fibula fracture fragments to aid in later reduction (Fig 2).
Fig 2.
Syndesmosis fixation. After fixation of the syndesmosis, the talus is stable within the mortise. The arthroscopic shaver cannot be easily inserted between the medial malleolus and the talar dome, indicating a negative drive-through sign.
Step 3
Attention is then turned to medial structures, and the working and viewing portals are reversed, with the anterolateral portal now used for visualization and debridement of medial structures performed from the anteromedial portal. Particular attention is paid to assessing the integrity of the deltoid and the posterior tibialis tendon structures. Ligamentous tissue, loose bodies, and small osteochondral injuries or fractures can be identified and addressed. In addition, these areas are debrided to remove any medial-sided mechanical block to reduction. As shown in Video 1, while the surgeon is addressing the medial side, the arthroscopic drive-through sign is positive if a shaver from the medial portal can be directed posteriorly between the talar dome and the medial malleolus with ease; this is pathognomonic for either an isolated syndesmotic injury or a deltoid ligament and fibula injury, or a combination thereof (Fig 3). This shows instability of the talus with respect to the tibia, indicating an unstable ankle.
Fig 3.
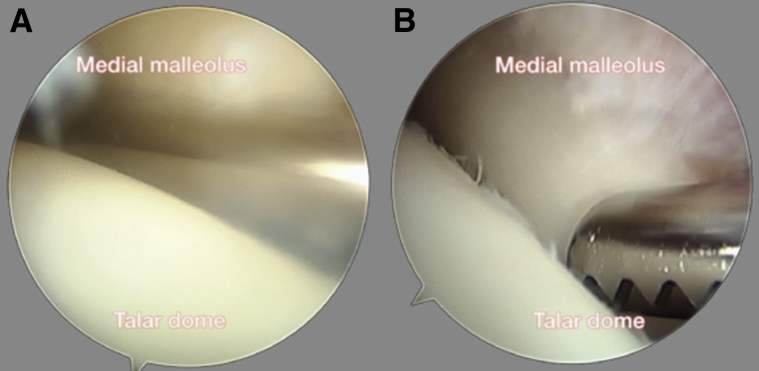
Arthroscopic views of drive-through sign. Ankle arthroscopy is performed with the camera in the lateral viewing portal and the 2.9-mm shaver in the medial portal. The drive-through sign is (A) positive when the shaver is easily inserted between the talar dome and the medial malleolus but (B) negative when the shaver cannot easily pass between these 2 structures. After fibula fixation, a positive test indicates that the mortise is unstable and further fixation of the syndesmosis should be performed.
Step 4
After debridement of medial-sided ankle structures, attention is turned to evaluating the syndesmosis, specifically the anterior-inferior tibiofibular ligament. Often it is possible to visualize several centimeters above the joint line, especially when the syndesmosis is torn. One can perform an external stress test with the arthroscope (Smith & Nephew, Andover, MA) in place to assess instability. Obvious and subtle injuries to the syndesmosis can be diagnosed at this point, and the reduction of the fibula to the tibia can be noted for comparison after fixation.
Step 5
Once this initial diagnostic arthroscopy and debridement have been performed, attention is turned to ORIF. If there is a fibula fracture and deltoid injury, typically a direct lateral approach to the fibula is used. In cases in which there is a significant posterior malleolus fracture that requires stabilization, a posterolateral approach is used to address both the fibula and the posterior malleolus. In this report we describe the direct lateral approach to the fibula, presented in Video 1.
In step 5A, a longitudinal incision is made along the posterior aspect of the fibula extending distally to the tip of the fibula base and proximally 3 fingerbreadths above the fracture site. In step 5B, superficial and deep dissection is carried down to the level of the fibula periosteum, with care taken not to injure the short saphenous vein and the superficial peroneal nerve. In step 5C, once the fracture site is exposed, fracture fragments are further debrided and reduction is performed, being held using reduction clamps. In step 5D, interfragmentary fixation of the fibula fracture is obtained by lag screw techniques. Additional lag screws can be used based on the complexity of the fracture fragment. In step 5E, a locking compression plate is applied to the fibula as a neutralization plate to protect the interfragmentary screws. Distal and proximal screw holes are used, and the screw holes at the level of the syndesmosis are temporarily preserved to allow for syndesmotic fixation as needed.
Step 6
After fibula fixation, an intraoperative stress radiograph is obtained to assess reduction by the medial clear space widening and restoration of the tibial-fibular overlap. However, regardless of the radiographic stress test result, diagnostic arthroscopy is performed again to evaluate the stability of the syndesmosis.
Step 7
At this point, if there is a fibula injury plus a deltoid injury, the ankle is often reduced as long as the syndesmosis is intact. However, in the case of a syndesmotic injury in addition to the aforementioned pathology, simply addressing the fibula may not anatomically reduce the ankle, which allows supraphysiological range of motion of the fibula and talus with respect to the tibia. Therefore, if the arthroscopic drive-through sign is not completely eliminated after fibula fixation, further attention is warranted to stabilize the ankle.
Step 8
For ankles with a positive stress radiograph finding (i.e., medial clear space >3 to 5 mm), further arthroscopic debridement of the syndesmosis and medial-sided structures is performed at this stage.
Step 9
As is done before fibula fixation, the drive-through maneuver is performed by placing the shaver from the medial portal between the talar dome and the medial malleolus. In the stable ankle, this will not be possible. However, in ankles with syndesmotic and deltoid instability, the shaver can pass posteriorly. If this is the case, syndesmosis stabilization is obtained using one or two 4.0- or 4.5-mm cannulated cortical screws drilled across 3 or 4 cortices.
Step 10
If syndesmosis stabilization is performed, the ankle is again re-instrumented arthroscopically for direct visualization of syndesmosis reduction and assessment for the presence of a drive-through sign. For cases of either obvious or subtle syndesmosis injury, placement of syndesmotic screws with good purchase is sufficient to remove the drive-through sign. Absence of the drive-through sign indicates that the deltoid ligament does not need repair to achieve a stable ankle. Often, fixing the fibula indirectly reduces the deltoid, and it remains controversial whether the deltoid should be fixed in this instance. It should also be noted that historically, a case with a persistent wide medial clear space after adequate trans-syndesmotic fixation was commonly due to interposition of the deltoid in the medial gutter. Arthroscopic assessment can diagnose this variant early in the case, and the medial side of the ankle can be opened or addressed arthroscopically for direct repair and tightening of medial-sided structures.
Postoperative Protocol
Postoperatively, patients follow standard ankle fracture protocols at our institution and are kept non–weight bearing in a well-padded splint for 2 weeks. Sutures are removed and the splint is converted to a fracture boot at 2 weeks postoperatively. At 6 weeks, the patient is progressed regarding weight-bearing status and range-of-motion exercises begin during physical therapy.
Discussion
In this technical note we present the arthroscopic ankle drive-through sign, which is shown in Video 1. This is a useful modality for assessing stability of the syndesmosis during arthroscopy. The sign is positive when pathology exists and becomes negative when the syndesmosis has been appropriately stabilized. Ankle arthroscopy during ORIF of ankle fractures is a sensitive tool for detecting subtle ankle instability and ligamentous injury, particularly in cases in which syndesmotic injury occurs without radiographic evidence of syndesmotic diastasis. Arthroscopic evaluation of instability using the tactile feedback of a drive-through sign has been described in both the knee14, 15, 16 and the shoulder.
Intraoperative assessment of syndesmotic stability during ankle fracture ORIF is both challenging and controversial.17 Syndesmotic malreduction and continued subtle ankle instability after ORIF can lead to persistent disability and long-term decreased patient outcomes.1 In our experience, concomitant ankle arthroscopy at the time of ankle ORIF provides the highest diagnostic yield in ankle fracture management and reduction assessment. Although ankle arthroscopy can be technically challenging, the operative techniques presented in this article are simple to perform and allow for smooth incorporation of ankle arthroscopy into the fracture management algorithm without disrupting surgical flow and/or significantly increasing operative time. In experienced hands, concomitant arthroscopy may only increase operative time by 15 to 20 minutes.10 The techniques presented in this report are applicable to the sports, trauma, and foot/ankle surgeon.
For surgeons who already incorporate ankle arthroscopy for operatively treated ankle fractures, the addition of the drive-through test offers little downside. It requires no additional equipment and can be used as an adjunct or alternative to the external rotation stress test. The main risk of the drive-through sign is possible injury to the cartilage of the tibia and/or talus in the medial gutter when one is attempting to insert the shaver, although we have not observed this in our experience. It is important to note that the test is positive when the arthroscope can be inserted easily. The shaver should not be forcefully pushed into the medial gutter because resistance signifies restraint of the talus and a negative test and additional force may result in shear injury to the cartilage.
However, for surgeons who do not routinely incorporate ankle arthroscopy in their treatment of ankle fractures, there are more considerations. The benefits of arthroscopy include the ability to directly visualize and potentially treat cartilage injuries as well as to evaluate stability with the drive-through test. However, this must be weighed against the increased operative time required to perform arthroscopy, increased swelling due to arthroscopic fluid accumulation, and the neurovascular risk associated with creating arthroscopic portals. Thus this is a decision the surgeon must make depending on his or her comfort level with arthroscopy.
The described operative techniques present significant opportunities for hypothesis generation and future clinical studies. Future studies may seek to compare the sensitivity and specificity of the ankle drive-through sign with those of traditional modalities such as perioperative stress radiographs and magnetic resonance imaging for diagnosing syndesmotic injury. Ultimately, it may give the surgeon a sensitive tool capable of improving the assessment of syndesmotic injuries and their reduction.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article.
Supplementary Data
The arthroscopic drive-through sign evaluates stability of the ankle syndesmosis. The patient is positioned supine with a bump under the hip. The arthroscope is inserted in the anterolateral portal, whereas the 2.9-mm shaver (Smith & Nephew) is inserted in the anteromedial portal. After the fibula is fixed, the drive-through sign is performed by attempting to insert the shaver between the medial malleolus and the talar dome. If this is done easily, the mortise is unstable and further fixation of the syndesmosis is indicated. If the surgeon feels resistance while trying to insert the shaver, then the mortise is stable and further fixation is likely not required.
References
- 1.Sagi H.C., Shah A.R., Sanders R.W. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma. 2012;26:439–443. doi: 10.1097/BOT.0b013e31822a526a. [DOI] [PubMed] [Google Scholar]
- 2.Jenkinson R.J., Sanders D.W., Macleod M.D., Domonkos A., Lydestadt J. Intraoperative diagnosis of syndesmosis injuries in external rotation ankle fractures. J Orthop Trauma. 2005;19:604–609. doi: 10.1097/01.bot.0000177114.13263.12. [DOI] [PubMed] [Google Scholar]
- 3.Ramsey P.L., Hamilton W. Changes in tibiotalar area of contact caused by lateral talar shift. J Bone Joint Surg Am. 1976;58:356–357. [PubMed] [Google Scholar]
- 4.Takao M., Ochi M., Naito K. Arthroscopic diagnosis of tibiofibular syndesmosis disruption. Arthroscopy. 2001;17:836–843. doi: 10.1016/s0749-8063(01)90007-6. [DOI] [PubMed] [Google Scholar]
- 5.Takao M., Ochi M., Oae K., Naito K., Uchio Y. Diagnosis of a tear of the tibiofibular syndesmosis. The role of arthroscopy of the ankle. J Bone Joint Surg Br. 2003;85:324–329. doi: 10.1302/0301-620x.85b3.13174. [DOI] [PubMed] [Google Scholar]
- 6.Koenig S.J., Tornetta P., III, Merlin G. Can we tell if the syndesmosis is reduced using fluoroscopy? J Orthop Trauma. 2015;29:e326–e330. doi: 10.1097/BOT.0000000000000296. [DOI] [PubMed] [Google Scholar]
- 7.Garner M.R., Fabricant P.D., Schottel P.C. Standard perioperative imaging modalities are unreliable in assessing articular congruity of ankle fractures. J Orthop Trauma. 2015;29:e161–e165. doi: 10.1097/BOT.0000000000000219. [DOI] [PubMed] [Google Scholar]
- 8.Cha S.D., Kwak J.Y., Gwak H.C. Arthroscopic assessment of intra-articular lesion after surgery for rotational ankle fracture. Clin Orthop Surg. 2015;7:490–496. doi: 10.4055/cios.2015.7.4.490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen X.Z., Chen Y., Liu C.G., Yang H., Xu X.D., Lin P. Arthroscopy-assisted surgery for acute ankle fractures: A systematic review. Arthroscopy. 2015;31:2224–2231. doi: 10.1016/j.arthro.2015.03.043. [DOI] [PubMed] [Google Scholar]
- 10.Fuchs D.J., Ho B.S., LaBelle M.W., Kelikian A.S. Effect of arthroscopic evaluation of acute ankle fractures on PROMIS intermediate-term functional outcomes. Foot Ankle Int. 2016;37:51–57. doi: 10.1177/1071100715597657. [DOI] [PubMed] [Google Scholar]
- 11.Pagnani M.J., Warren R.F. Arthroscopic shoulder stabilization. Oper Tech Sports Med. 1993;1:276–284. [Google Scholar]
- 12.McFarland E.G., Neira C.A., Gutierrez M.I., Cosgarea A.J., Magee M. Clinical significance of the arthroscopic drive-through sign in shoulder surgery. Arthroscopy. 2001;17:38–43. doi: 10.1053/jars.2001.19967. [DOI] [PubMed] [Google Scholar]
- 13.Bonasia D.E., Rossi R., Saltzman C.L., Amendola A. The role of arthroscopy in the management of fractures about the ankle. J Am Acad Orthop Surg. 2011;19:226–235. doi: 10.5435/00124635-201104000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Feng H., Song G.Y., Shen J.W., Zhang H., Wang M.Y. The “lateral gutter drive-through” sign revisited: A cadaveric study exploring its real mechanism based on the individual posterolateral structure of knee joints. Arch Orthop Trauma Surg. 2014;134:1745–1751. doi: 10.1007/s00402-014-2100-y. [DOI] [PubMed] [Google Scholar]
- 15.Feng H., Zhang H., Hong L., Wang X.S., Zhang J. The “lateral gutter drive-through” sign: An arthroscopic indicator of acute femoral avulsion of the popliteus tendon in knee joints. Arthroscopy. 2009;25:1496–1499. doi: 10.1016/j.arthro.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 16.Nha K.W., Bae J.H., Kwon J.H., Kim J.G., Jo D.Y., Lim H.C. Arthroscopic posteromedial drive-through test in posterior cruciate ligament insufficiency: A new diagnostic test. Knee Surg Sports Traumatol Arthrosc. 2015;23:1113–1118. doi: 10.1007/s00167-014-2902-z. [DOI] [PubMed] [Google Scholar]
- 17.Stoffel K., Wysocki D., Baddour E., Nicholls R., Yates P. Comparison of two intraoperative assessment methods for injuries to the ankle syndesmosis. A cadaveric study. J Bone Joint Surg Am. 2009;91:2646–2652. doi: 10.2106/JBJS.G.01537. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The arthroscopic drive-through sign evaluates stability of the ankle syndesmosis. The patient is positioned supine with a bump under the hip. The arthroscope is inserted in the anterolateral portal, whereas the 2.9-mm shaver (Smith & Nephew) is inserted in the anteromedial portal. After the fibula is fixed, the drive-through sign is performed by attempting to insert the shaver between the medial malleolus and the talar dome. If this is done easily, the mortise is unstable and further fixation of the syndesmosis is indicated. If the surgeon feels resistance while trying to insert the shaver, then the mortise is stable and further fixation is likely not required.