Abstract
Introduction
From a series of radiolabelled cholecystokinin (CCK) and gastrin analogues, 111In-CP04 (111In-DOTA-(DGlu)6-Ala-Tyr-Gly-Trp-Met-Asp-Phe-NH2) was selected for further translation as a diagnostic radiopharmaceutical towards a first-in-man study in patients with medullary thyroid carcinoma (MTC). A freeze-dried kit formulation for multicentre application has been developed. We herein report on biosafety, in vivo stability, biodistribution and dosimetry aspects of 111In-CP04 in animal models, essential for the regulatory approval of the clinical trial.
Materials and methods
Acute and extended single dose toxicity of CP04 was tested in rodents, while the in vivo stability of 111In-CP04 was assessed by HPLC analysis of mouse blood samples. The biodistribution of 111In-CP04 prepared from a freeze-dried kit was studied in SCID mice bearing double A431-CCK2R(±) xenografts at 1, 4 and 24 h pi. Further 4-h animal groups were either additionally treated with the plasma expander gelofusine or injected with 111In-CP04 prepared by wet-labelling. Pharmacokinetics in healthy mice included the 30 min, 1, 4, 24, 48 and 72 h time points pi. Dosimetric calculations were based on extrapolation of mice data to humans adopting two scaling models.
Results
CP04 was well-tolerated by both mice and rats, with an LD50 > 178.5 μg/kg body weight for mice and a NOAEL (no-observed-adverse-effect-level) of 89 μg/kg body weight for rats. After labelling, 111In-CP04 remained >70% intact in peripheral mouse blood at 5 min pi. The uptake of 111In-CP04 prepared from the freeze-dried kit and by wet-labelling were comparable in the A431-CCK2R(+)-xenografts (9.24 ± 1.35%ID/g and 8.49 ± 0.39%ID/g, respectively; P > 0.05). Gelofusine-treated mice exhibited significantly reduced kidneys values (1.69 ± 0.15%ID/g vs. 5.55 ± 0.94%ID/g in controls, P < 0.001). Dosimetry data revealed very comparable effective tumour doses for the two scaling models applied, of 0.045 and 0.044 mSv/MBq.
Conclusion
The present study has provided convincing toxicology, biodistribution and dosimetry data for prompt implementation of the freeze-dried kit formulation without or with gelofusine administration in a multicentre clinical trial in MTC patients.
Keywords: Radiopharmaceutical development, Medullary thyroid cancer, CCK2R-targeting of tumours, Gastrin-radioligand, Radionuclide therapy, Clinical translation
1. Introduction
Medullary thyroid cancer (MTC) is a neuroendocrine tumour of the parafollicular or C cells of the thyroid, not accumulating iodine. It accounts for 3% to 5% of thyroid carcinomas (Pacini et al., 2010; Wells et al., 2015). In many cases disease has already metastasized at the time of diagnosis with limited therapeutic options. Long-term responses by radiotherapy or systemic therapy are uncommon (Pacini et al., 2010) and new targeted chemotherapy approaches (like tyrosine kinase inhibitors, TKI) show significant toxicity and do not change overall survival is (Nikiforova and Nikiforov, 2008; Zhang et al., 2009). MTC therefore still remains a highly challenging cancer for both the patient and the physician.
Molecular nuclear medicine can play an important role in diagnosis (SPECT/CT, PET/CT) and therapy of advanced MTC (Reubi and Maecke, 2008). Molecular imaging and peptide receptor radionuclide therapy (PRRT) approaches can exploit the overexpression of cholecystokinin subtype 2 receptors (CCK2R) at an incidence of over 90% in MTC (Reubi et al., 1997; Reubi and Waser, 1996). This finding has motivated a number of research groups to develop site-specific radiolabeled analogues of cholecystokinin-8 (CCK-8; Asp-Tyr-Met-Gly-Trp-Met-Asp-Phe-NH2) or minigastrin (MG, Leu-(Glu)5-Ala-Tyr-Gly-Trp-Met-Asp-Phe-NH2). (Behr and Behe, 2002; Froberg et al., 2009; Nock et al., 2005; Sosabowski et al., 2007; von Guggenberg et al., 2004; von Guggenberg et al., 2007).
The very high kidney retention of these tracers, which limits their application for radionuclide therapy (Behe and Behr, 2002), has stimulated further research which revealed the importance of the multi-negative charges of the penta-Glu chain but also of the secondary peptide structure on the in vivo profile of resulting minigastrin radioligands (Breeman et al., 2008; Good et al., 2008; Kolenc-Peitl et al., 2011; Kolenc Peitl et al., 2015; Mather et al., 2007; von Guggenberg et al., 2009, 2012).
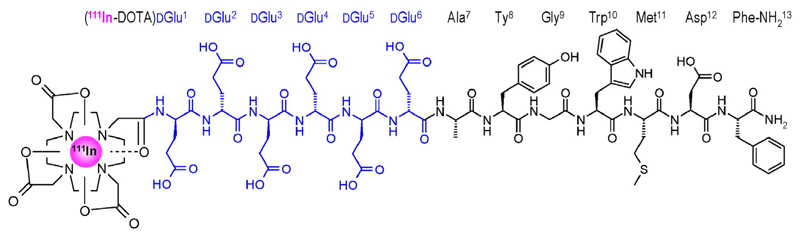
From a series of such analogues the linear peptide radioligand 111In-DOTA-(DGlu)6-Ala-Tyr-Gly-Trp-Met-Asp-Phe-NH2 (111In-CP04, also named PPF11; Fig. 1) was selected as the best candidate for a subsequent phase I clinical study in the diagnosis and therapy of human MTC, owing to its high tumour uptake and retention as well as the favorable tumour-to-kidney ratios attained (Aloj et al., 2011; Laverman et al., 2011; Ocak et al., 2011).
Fig. 1.
Chemical structure of 111In-CP04 with the DGlu1–6-chain highlighted in blue. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
For conducting a multicenter clinical trial in Europe, an Investigational Medicinal Product Dossier (IMPD) has to be submitted and approved by the Authorities. Such IMPD is based on the common technical dossier (CTD) which for radiopharmaceuticals should additionally include information related to radioactivity and radiolabelling procedures (Todde et al., 2014). Data on the chemical and pharmaceutical development and characterization of a freeze-dried kit formulation for radiolabelling of the radiopharmaceutical precursor CP04 with 111In (chapter 2.1 of the CTD) has been recently presented (Pawlak et al., 2016). We herein further describe the additional data generated for translating this promising radiopharmaceutical into a first in human clinical trial. This includes the non-clinical pharmacology, pharmacokinetics and toxicity data. Initial preclinical data already have been reported (Aloj et al., 2011; Laverman et al., 2011; Ocak et al., 2011; Kolenc Peitl et al., 2015). In the present work we additionally report on the specific requirements for a radioactive medicinal product, including specific toxicity studies (Koziorowski et al., 2016), animal tumour models and estimation of the expected human radiation dose extrapolated from animal data, essential for the regulatory approval of the clinical trial.
2. Materials and methods
2.1. Chemicals and peptides
If not otherwise stated, chemicals, materials and solvents were of pharmaceutical grade for kit preparation and reagent grade for other experiments and were used without further purification. l-methionine was provided by SAFC chemicals (Cleveland OH), ascorbic acid and gentisic acid (Ultrapure quality) were provided by Sigma Aldrich (St. Louis, MO). The CP04-precursor in GMP grade was provided by PiChem (Graz, Austria) and CP04 freeze-dried kits for the preparation of 111In-CP04 were prepared as previously described (Pawlak et al., 2016).
2.2. Animals
For acute intravenous toxicity studies Crl:NMRI (SPF) female mice provided by Charles River Laboratories (Germany) of 7–9 weeks of age and a body weight of 26–33 g were used. For extended acute single dose toxicity study in rats, 45 female and 45 male Wistar Hannover RccHan™ rats were used purchased from Harlan Laboratories, B.V. (The Netherlands). Animals were 7–7 weeks of age and the body weights were 195–235 g for males and 164–199 g for females. For in vivo stability tests and biodistribution/dosimetry studies healthy male Swiss albino mice from NCSR “Demokritos” Animal House were used, of 8–10 weeks of age and a body weight of 20–25 g. For the CCK2R-expressing tumour model, male SCID mice from NCSR “Demokritos” Animal House were used, of 6 weeks of age on arrival day and a body weight of 20 ± 2 g.
2.3. Toxicity studies
2.3.1. Acute toxicity of CP04 in mice
The CP04 precursor was dissolved in phosphate buffered saline (PBS pH 7.4) and was administered at a dose of 178.5 μg/kg body weight and a dose volume of 5 mL/kg body weight into the caudal vein of two groups of three mice (Acute Intravenous Toxicity Study in Mice, Harlan Laboratories Study #D04314). The test procedures were based on OECD Guideline 423 “Acute Oral Toxicity – Acute Toxic Class Method”, adopted on 17th December 2001. In brief, the animals were examined daily during the acclimatisation period. Mortality, viability and clinical signs were recorded. All animals were examined for clinical signs within the first 30 min and approximately 1, 2, 3 and 5 h after treatment on test day 1 and once daily during test days 2–15. Mortality/viability was recorded within the first 30 min and approximately 1, 2, 3 and 5 h after administration on test day 1 (with the clinical signs) and twice daily during days 2–15. Body weights were recorded on test day 1 (prior to administration) and on test days 8 and 15. All animals were necropsied and examined macroscopically.
2.3.2. Extended acute single dose toxicity study in rats
The study was designed according to the microdosing concept as described in ICH guideline M3 (R2) (“Note for guidance on non-clinical safety studies for the conduct of human clinical trials and marketing authorization for pharmaceuticals” (CPMP/ICH/286/95)). In brief, 90 rats were distributed into three dose groups, each containing fifteen animals per sex (Table 1). The animals from Group 1 received only PBS, serving as controls, while groups II and III received the CP04 solution by single intravenous (bolus) injection at a low (89 μg/kg body weight: Group 2) and a high dose (890 μg/kg body weight: Group 3). A 24-h observation period followed (Allocation A), except for five animals per sex from each group for which treatment was followed by an additional 14-day treatment-free recovery period (Allocation B).
Table 1. Number of wistar rats per group according to dose, sex and monitoring.
| Groups | 1* (control) | 2 | 3 |
| Treatment | Vehicle | CP04 | CP04 |
| Dose levels | 0 μg/kg | 89 μg/kg | 890 μg/kg |
| Male A | 10 | 10 | 10 |
| Male B | 5 | 5 | 5 |
| Female A | 10 | 10 | 10 |
| Female B | 5 | 5 | 5 |
A: animals for main study (Allocation A); B: animals for recovery (Allocation B); 1*: group 1 received vehicle only.
At day 2 blood samples were withdrawn from Allocation-A animals for haematology, clinical biochemistry and samples for urinary analyses were collected. These animals were necropsied on the same day and histological examinations were performed on an extended set of organs (adrenal glands, kidneys, liver, pancreas, sternum (including bone marrow), small intestine, stomach, thyroid/parathyroid glands and gross lesions). The animals from Allocation-B remained untreated for the following 14 days, but on day 15 underwent the same procedure described above (Extended Acute Intravenous (Bolus) Toxicity Study in Rats, Harlan Study #S47364).
2.4. Radiolabeling and quality control
For labelling, a sterile, non-pyrogenic solution of non-carrier-added 111InCl3 in 0.05 M HCl was supplied from Mallinckrodt Medical (Petten, NL). The solution contained 185 MBq (5 mCi) of 111InCl3 per 0.5 mL at time of calibration (specific activity of > 1.85 GBq/μg indium at time of calibration). CP04 (10 μg POLATOM kit, 4.88 nmol) was dissolved in 400 μL water for injection (Pharm.Eur., Fresenius Kabi, Halden, Norway), 111InCl3 was added (~120 μL, 94.35 MBq) and the mixture was incubated for 12 min at 85 °C. The “wet-labelling” of CP04 with 111In was completed in an Eppendorf vial. Freshly prepared sodium ascorbate buffer (10 mM) was added in the vial, followed by 111InCl3 solution (37–74 MBq), Met (1000 nmol) and CP04 (10 nmol). The mixture was left to react at 80 °C for 20 min. Before quality control tests, EDTA in 0.1 M acetate buffer (pH 4.6) was added to a final concentration of 1 mM to the labelling reaction mixture as a “free” 111In3+ scavenger. Quality control was conducted by HPLC analysis on (system 1) a RP-18 XTerra column (5 μm, 3.9 mm × 20 mm) eluted at a flow rate of 1 mL/min with the linear gradient: 100% A/0% B to 40% A/60% B within 60 min (A = 0.1% aqueous TFA and B = MeCN).
2.5. In vivo stability of 111In-CP04 in mice
A bolus of 111In-CP04 (100 μL, 11 MBq, ≈3 nmol peptide) was injected in the tail vein of healthy mice. Blood withdrawn 5 min post injection (pi) was directly placed in pre-chilled polypropylene tubes containing EDTA and Met on ice. Samples were centrifuged (10 min, 2000 ×g/4 °C, in a Hettich, Universal 320R, centrifuge, Tüttlingen, Germany), plasma was collected, mixed with chilled MeCN in a 1/1 v/v ratio and centrifuged again (10 min, 15,000 ×g/4 °C). Supernatants were concentrated to a small volume under a gentle N2-flux at 40 °C, diluted with physiological saline (≈400 μL) and filtered through a Millex GV filter (0.22 μm). Aliquots thereof were analysed by HPLC under the following conditions (system 2): A RP-18 Symmetry Shield column (5 μm, 3.9 mm × 20 mm) was eluted at a flow rate of 1 mL/min with the linear gradient: 100% A/0% B to 40% A/60% B within 60 min (A = 0.1% aqueous TFA and B = MeCN); the tR of intact 111In-CP04 was determined by co-injection of a parent radioligand sample.
2.6. Pharmacokinetics of 111In-CP04 in healthy mice
A bolus of 111In-CP04 (100 μL, 111 kBq, 10 pmol peptide) was injected via the tail vein in healthy mice and animals were euthanized in groups of four at 30 min, 1 h, 4 h, 24 h, 48 h and 72 h pi. Samples of blood and tissues of interest were excised, weighted and counted for radioactivity in the gamma counter (automated well-type multi-sample gamma counter; NaI(Tl) 3″ crystal, Canberra Packard Auto-Gamma 5000 series instrument). Data was calculated as percent injected dose per gramtissue (%ID/g) with the aid of suitable standards of the injected dose.
2.7. Biodistribution of 111In-CP04 in mice bearing double A431-CCK2R(±) xenografts
The human epidermoid A431 cell line transfected to stably express the CCK2R (A431-CCK2R(+)) or devoid of CCK2R expression (A431-CCK2R(−)) used for tumour induction in this work was a gift from Prof. O. Boerman (Department of Nuclear Medicine, Radboud University Nijmegen Medical Centre, Nijmegen, The Netherlands) and Prof. L. Aloj (Istituto di Biostrutture e Bioimmagini, Consiglio Nazionale delle Ricerche, Naples, Italy) and cells were cultured as previously reported (Aloj et al., 2004). Suspensions of freshly harvested A431-CCK2R(±) cells (~150 μL, 1.6 × 107/1.4 × 107) in normal saline were subcutaneously injected in the flanks of mice. A week later well palpable tumours (260 ± 80 mg) developed at the inoculation sites and biodistribution was conducted.
At the day of the experiment, a bolus of 111In-CP04 (100 μL, 111 kBq, 10 pmol peptide) was injected in the tail vein of mice. Animals were euthanized in groups of four at 1 h, 4 h and 24 h pi; in a separate 4-h group animals received gelofusine (100 μL) together with the radioligand. A further 4-h group of mice was injected with 111In-CP04 prepared by “wet labelling” (100 μL, 111 kBq, 10 pmol peptide). Mice were dissected and samples of blood and tissues of interest as well as tumours were excised, weighted and counted for radioactivity in the gamma counter. Data was calculated as percent injected dose per gram tissue (%ID/g) with the aid of suitable standards of the injected dose and represent mean ± SD. In all above experiments, analysis of the solution used in the biodistribution experiment was conducted prior to and after completion of all animal injections.
Statistical analysis using the unpaired two-tailed Student’s t-test was performed to compare values between A431-CCK2R(+) and A431-CCK2R(−) tumours, as well as kidney, stomach and A431-CCK2R(+) tumour values between 4 h control and gelofusine-treated animal groups; values P < 0.05 were considered statistically significant (Table 2). The pharmacokinetic profile was determined by fitting an exponential curve through the organ time-activity data according to the least-squares method. The number of exponentials in the fitted curve was analysed according to the Aikake Information Criterion (AICc). All fitting was performed with Graphpad Prism version 5.
Table 2. Biodistribution of 111In-CP04 in healthy Swiss albino mice.
| %ID/g tissue ± SD (n = 4) |
||||||
|---|---|---|---|---|---|---|
|
111In-CP04 |
||||||
| Organs | 30 min | 1h | 4h | 24 h | 48 h | 72 h |
| Blood | 1.74 ± 0.22 | 0.51 ± 0.14 | 0.02 ± 0.01 | 0.00 ± 0.00 | 0.01 ± 0.01 | 0.01 ± 0.01 |
| Liver | 0.77 ± 0.11 | 0.32 ± 0.15 | 0.12 ± 0.02 | 0.06 ± 0.01 | 0.06 ± 0.00 | 0.05 ± 0.01 |
| Heart | 0.70 ± 0.10 | 0.21 ± 0.04 | 0.03 ± 0.01 | 0.02 ± 0.01 | 0.02 ± 0.01 | 0.03 ± 0.02 |
| Kidneys | 9.80 ± 2.07 | 8.84 ± 2.05 | 7.90 ± 1.98 | 3.61 ± 0.31 | 2.81 ± 0.63 | 2.62 ± 0.24 |
| Stomach | 4.88 ± 0.85 | 2.99 ± 0.55 | 2.61 ± 0.82 | 1.48 ± 0.55 | 1.26 ± 0.26 | 0.92 ± 0.04 |
| Intestines | 0.82 ± 0.14 | 0.39 ± 0.12 | 1.05 ± 0.35 | 0.18 ± 0.14 | 0.08 ± 0.02 | 0.09 ± 0.04 |
| Spleen | 0.36 ± 0.04 | 0.14 ± 0.04 | 0.05 ± 0.01 | 0.04 ± 0.01 | 0.03 ± 0.01 | 0.04 ± 0.01 |
| Muscle | 0.59 ± 0.10 | 0.18 ± 0.04 | 0.04 ± 0.02 | 0.02 ± 0.01 | 0.03 ± 0.02 | 0.03 ± 0.02 |
| Lung | 1.05 ± 0.10 | 0.40 ± 0.10 | 0.06 ± 0.01 | 0.03 ± 0.01 | 0.02 ± 0.01 | 0.03 ± 0.01 |
| Femur | 4.62 ± 1.24 | 2.62 ± 0.42 | 0.96 ± 0.18 | 0.53 ± 0.04 | 0.55 ± 0.11 | 0.49 ± 0.06 |
| Pancreas | 0.67 ± 0.08 | 0.26 ± 0.08 | 0.10 ± 0.01 | 0.05 ± 0.01 | 0.04 ± 0.01 | 0.06 ± 0.03 |
All animal experiments were approved by national authorities and were carried out in compliance with national and European guidelines.
2.8. Dosimetric calculations
Dosimetric calculations were based on biodistribution of 111In-CP04 in healthy mice from 30 min to 72 h pi (Table 2). Clearance kinetics in each organ was determined by exponential curve fitting. The time-integrated activity concentration (TIAC) was obtained by integration of this exponential curve folded with the decay curve of 111In and 177Lu.Mouse dosimetry was calculated for both 177Lu and 111In using the TIAC and the 25 g RADAR mouse absorbed dose rates per unit activity S for each source and target organ combination (Keenan et al., 2010; Konijnenberg et al., 2014).
Extrapolation of biodistribution uptake data in mice to humans was based on two options for interspecies scaling (Stabin, 2008).
| 1. |
with m the organ mass and M the total body weight of mouse or human and with the percentage of the injected activity concentration and per organ, respectively. The mouse organ TIACs are multiplied with the ratio of mouse and human body weights to obtain the extrapolated human TIAC, and this multiplied with the organ mass (from the MIRD standard man phantom) yields the residence time in each source organ.
| 2. |
in this method the uptake per organ is extrapolated one-to-one from mouse to man. The extrapolated human residence time is obtained by multiplying the mouse TIAC or each source organ with its mouse organ mass.
The extrapolated human source organ residence times were used as input in the Olinda/EXM dosimetry software to calculate the absorbed doses per administered activity in humans (Stabin et al., 2005).
3. Results
3.1. Toxicology
3.1.1. Acute toxicity of CP04 in mice
All animals survived until the end of the study with no systemic signs of toxicity evident throughout the entire observation period. The animal body weight was within the range commonly recorded for this strain and age. No macroscopic findings were recorded at necropsy. The median lethal dose (LD50) of CP04 after single intravenous administration to female mice observed over a period of 14 days was found to be ≥ 178.5 μg/kg body weight.
3.1.2. Extended acute single dose toxicity of CP04 in rats
All animals survived the 24-h study period with no clinical signs being recorded. Under the experimental conditions, single bolus injection of CP04 in rats at a dose of 890 μg/kg body weight caused a moderate decrease in mean food consumption and body weight -gain and a marked decrease in the reticulocyte count in the male rats 14 days after administration. Based on pathological examination, the no-observed-adverse-effect-level (NOAEL) was initially established at 890 μg/kg body weight. However, the reversibility of the effect recorded in the reticulocyte count remained unknown and it was not possible to assess whether it represents a true adverse effect. Accordingly, the lower dose of 89 μg/kg body weight was eventually set as NOAEL, supported also by the absence of toxicological adverse alterations in morphology, functional capacity, growth, development or life-span of treated animals.
3.2. Metabolic stability of111In-CP04 in mice
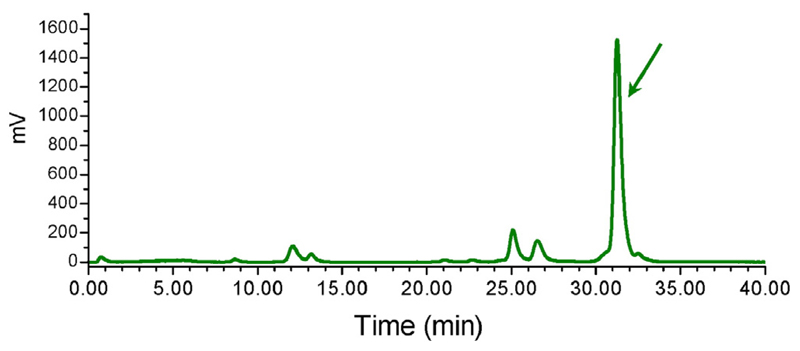
According to the HPLC analysis of mouse blood samples collected 5 min pi > 70% of 111In-CP04 remained intact in peripheral mouse blood. A radiochromatogram of a representative mouse blood sample is included in Fig. 2.
Fig. 2.
Typical HPLC (system 2) radiochromatogram of blood sample collected 5 min after intravenous injection of 111In-CP04 in Swiss albino mice with 70% intact radiotracer still detected; the tR of intact 111In-CP04 is indicated by the arrow.
3.3. Biodistribution of111In-CP04 in healthy mice
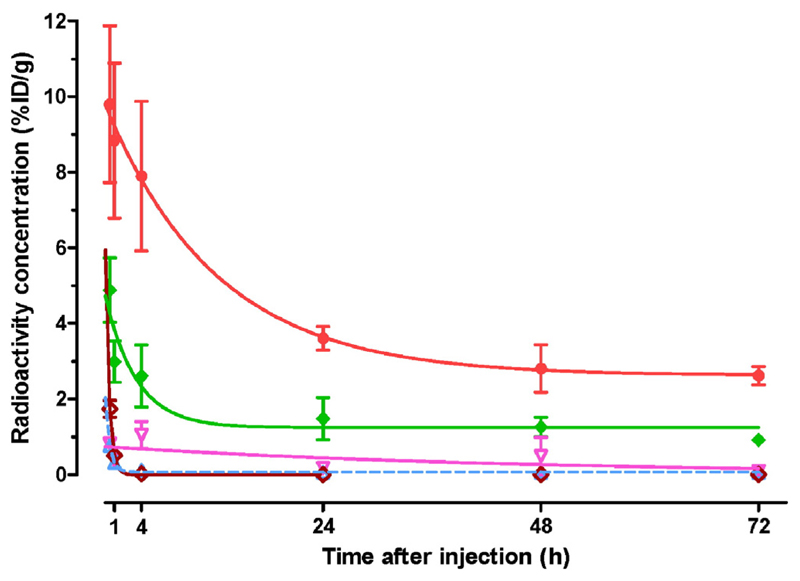
Biodistribution data of 111In-CP04 in healthy mice at 30 min, 1, 4, 24, 48 and 72 h pi is summarized in Table 2 as %ID/g (mean ± SD, n = 4), whereas time-dependent clearance curves selectively for kidneys, stomach, liver, intestines and blood are included in Fig. 3. The radiotracer cleared very rapidly from the blood and the body of mice predominantly via the kidneys and the urinary tract. Radioactivity was retained mainly in the stomach (a CCK2R-positive organ) and in the kidneys.
Fig. 3.
Time-dependent radioactivity clearance after injection of 111In-CP04 in Swiss albino mice shown for selected tissues;  kidneys,
kidneys,  stomach,
stomach,  intestines,
intestines,  liver,
liver,  blood; values represent mean %ID/g ± SD, n = 4. Single-exponential fits through the data are shown by the curves with corresponding color. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
blood; values represent mean %ID/g ± SD, n = 4. Single-exponential fits through the data are shown by the curves with corresponding color. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
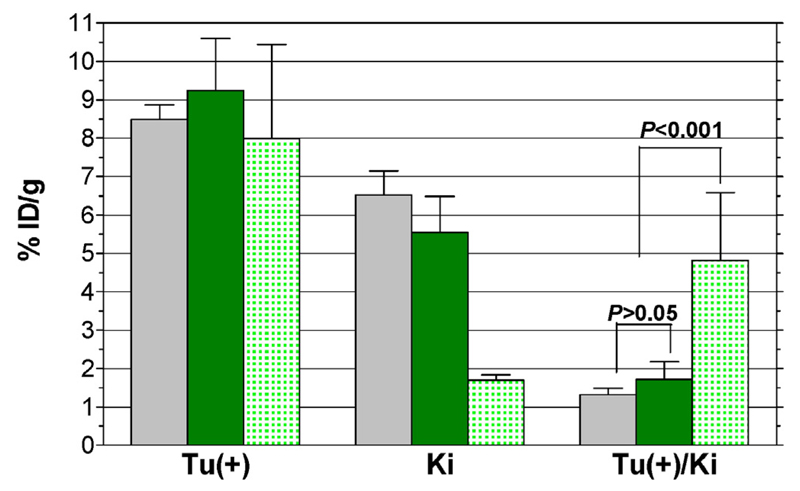
3.4. Biodistribution in A431-CCK2R(±) tumour-bearing mice
Biodistribution data of 111In-CP04 in mice bearing double A431-CCK2R(±) xenografts at 1, 4, and 24 h pi is presented in Table 3 as %ID/g (mean ± SD, n = 4). Additional animal groups at 4 h pi are also included in the Table 3, corresponding to mice coinjected with gelofusine or receiving 111In-CP04, prepared by wet-labelling. Selective data for A431-CCK2R(+) tumours, kidneys and kidney-to-blood ratios for 4-h animal groups is included in Fig. 4 for comparison. In agreement to findings of the healthy mice study, the radiotracer cleared very rapidly from the blood and the background via the kidneys and the urinary system, showing some retention in the CCK2R-possitive stomach and in the kidneys. It is interesting to note that gelofusine coinjection induced a significant (P < 0.001) reduction of renal uptake from 5.55 ± 0.94%ID/g to 1.69 ± 0.15%ID/g at 4 h pi, with the radioactivity excreted rapidly into urine. A CCK2R-independent process seems to be involved in the prolonged retention of the radiotracer in mouse kidney, since the CCK2R-positive stomach and tumour were not affected by gelofusine injection.
Table 3. Biodistribution of 111In-CP04 in SCID mice bearing double A431-CCK2R(±) xenografts.
| %ID/g tissue, mean ± sd (n = 4) |
|||||
|---|---|---|---|---|---|
| [111In]CP04 |
|||||
| Organs | 1 h | 4 h | 4 h + gelo | 4 h ref. | 24 h |
| Blood | 0.55 ± 0.17 | 0.02 ± 0.01 | 0.02 ± 0.01 | 0.04 ± 0.02 | 0.00 ± 0.00 |
| Liver | 0.38 ± 0.12 | 0.11 ± 0.01 | 0.17 ± 0.14 | 0.12 ± 0.02 | 0.01 ± 0.01 |
| Heart | 0.24 ± 0.08 | 0.02 ± 0.01 | 0.03 ± 0.01 | 0.03 ± 0.01 | 0.02 ± 0.00 |
| Kidneys | 5.53 ± 0.78 | 5.55 ± 0.94 | 1.69 ± 0.15*** | 6.52 ± 0.63ns | 3.29 ± 0.56 |
| Stomach | 2.60 ± 0.48 | 2.09 ± 0.32 | 2.15 ± 0.24ns | 1.63 ± 0.20 | 1.58 ± 0.15 |
| Intestines | 0.36 ± 0.13 | 0.22 ± 0.08 | 0.39 ± 0.13 | 0.29 ± 0.18 | 0.10 ± 0.04 |
| Spleen | 0.18 ± 0.04 | 0.04 ± 0.02 | 0.07 ± 0.01 | 0.06 ± 0.02 | 0.05 ± 0.01 |
| Muscle | 0.14 ± 0.05 | 0.03 ± 0.02 | 0.03 ± 0.01 | 0.02 ± 0.01 | 0.01 ± 0.01 |
| Lung | 0.47 ± 0.13 | 0.04 ± 0.01 | 0.05 ± 0.03 | 0.04 ± 0.01 | 0.03 ± 0.01 |
| Femur | 0.96 ± 0.46 | 0.30 ± 0.22 | 0.27 ± 0.02 | 0.39 ± 0.08 | 0.24 ± 0.09 |
| Pancreas | 0.23 ± 0.08 | 0.06 ± 0.01 | 0.07 ± 0.01 | 0.07 ± 0.01 | 0.05 ± 0.01 |
| Tumour(+) | 12.60 ± 1.73 | 9.24 ± 1.35 | 7.99 ± 2.45ns | 8.49 ± 0.39ns | 4.98 ± 0.56 |
| Tumour(–) | 1.07 ± 0.29+++ | 0.19 ± 0.05+++ | 0.22 ± 0.03+++ | 0.14 ± 0.02+++ | 0.10 ± 0.02+++ |
Statistical analysis was performed using the Student’s t-test with P values indicating very significant (***/+++P < 0.001) and not significant (ns, P > 0.05) difference (+) between Tumour(+) (A431-CCK2R(+)) and Tumour(–) (A431-CCK2R(–)) and (*) between the 4 h and 4 h + gelofusine-treated mice. The values in column 4 h-ref. correspond to a separate group of mice injected with 111In-CP04 obtained by “wet-labelling”; no significant differences were observed between this group and the 4-h group injected with 111In-CP04 prepared by kit reconstitution.
Fig. 4.
Biodistribution of 111In-CP04 ( ) prepared by wet-labelling, (
) prepared by wet-labelling, ( ) after kit-reconstitution and (
) after kit-reconstitution and ( ) during gelofusine coinjection in A431-CCK2R(+) tumour bearing SCID mice at 4 h pi. Results expressed as mean %ID/g ± SD are selectively shown for comparison for Tu(+): tumour, Ki: kidneys and Tu(+)/Ki: tumour-to-kidney ratios. Statistical analyses were performed using the unpaired two-tailed Student’s t-test.
) during gelofusine coinjection in A431-CCK2R(+) tumour bearing SCID mice at 4 h pi. Results expressed as mean %ID/g ± SD are selectively shown for comparison for Tu(+): tumour, Ki: kidneys and Tu(+)/Ki: tumour-to-kidney ratios. Statistical analyses were performed using the unpaired two-tailed Student’s t-test.
Another significant finding is the indistinguishable biodistribution profile between the 111In-CP04 prepared from the freeze-dried kit and from wet-labelling. No significant difference in the radioactivity levels in the A431-CCK2R(+) tumours was observed between kit and wet-labelling animal groups (9.24 ± 1.35%ID/g and 8.49 ± 0.39%ID/g, respectively; P > 0.05), or between untreated and gelofusine-treated mice (9.24 ± 1.35%ID/g and 7.99 ± 2.45%ID/g, respectively; P > 0.05). The high uptake of the radiotracer in the human xenografts expressing the CCK2R, but not in the tumours devoid of CCK2R-expression suggests in vivo CCK2R-specificity.
3.5. Dosimetric calculations
Total body clearance was calculated to be 90% with T1/2 = 17 min and 10% with T1/2 = 38 h, whereas a gastrointestinal tract clearance of 2.5% was observed. Mouse dosimetry was calculated for both 111In and 177Lu and is presented in Table 4. Based on mouse data and adopting two interspecies scaling models for extrapolating animal to human data the expected absorbed doses per injected activity in humans were calculated, leading to very comparable effective doses for both options of 0.045 and 0.044 mSv/MBq (Table 5). Assuming a radioactivity dose of 220 MBq 111In is injected in a patient, a whole body radiation dose of 9.9 mSv should be expected. This estimation needs to be eventually verified during the clinical study.
Table 4. Dosimetry of 111In-CP04 and 177Lu-CP04 in mice.
| Absorbed dose per injected activity (mGy/MBq) |
||
|---|---|---|
| Organs | 111In-CP04 | 177Lu-CP04 |
| Kidneys | 56 | 400 |
| Stomach wall | 15 | 86 |
| Bone | 9 | 51 |
| Large intestine | 7 | 36 |
| Small intestine | 7 | 36 |
| Total body | 4 | 19 |
| Pancreas | 5 | 16 |
| Lungs | 3 | 12 |
| Spleen | 3 | 9 |
| Liver | 3 | 7 |
Table 5. Expected absorbed doses of 111In-CP04 in humans based on two scaling models for translating mouse to human data.
| Absorbed dose per injected activity (mGy/MBq) |
||
|---|---|---|
| Organs | Option 1 | Option 2 |
| LLI wall | 0.078 | 0.075 |
| Small intestine | 0.026 | 0.024 |
| Stomach wall | 0.012 | 0.011 |
| ULI wall | 0.037 | 0.035 |
| Heart wall | 0.005 | 0.003 |
| Kidneys | 0.039 | 0.124 |
| Liver | 0.005 | 0.009 |
| Lungs | 0.004 | 0.003 |
| Muscle | 0.010 | 0.009 |
| Pancreas | 0.008 | 0.017 |
| Red marrow | 0.010 | 0.012 |
| Osteogenic cells | 0.015 | 0.034 |
| Spleen | 0.007 | 0.011 |
| Urinary bladder wall | 0.459 | 0.456 |
| Total body | 0.011 | 0.010 |
| Effective dose (mSv/MBq) | 0.045 | 0.044 |
4. Discussion
The therapeutic options for metastatic MTC are quite limited. Whereas classical cytotoxic chemotherapies are often linked to life-threatening toxicity, many novel targeted therapies (such as TKIs), although less toxic, still show considerable side effects. As a result, these systemic treatments are justified only for patients at significant risk of morbidity or mortality due to progressive spread disease. The rational design of new effective and less toxic site-directed drugs exploits the overexpression of molecular targets in MTC to specifically deliver cytotoxic loads to tumour cells. For example, minigastrin-based radionuclide carriers may deliver cytotoxic radiation to MTC lesions via CCK2R-targets on tumour cells while at the same time sparing surrounding healthy tissue. To improve the efficacy and limit the side-effects of this approach, radiolabeled minigastrin analogues should show high CCK2R-affinity, good in vivo stability for sufficient delivery to tumour-associated targets, rapid blood and physiological organ clearance preferably through the kidneys into urine. All above parameters are considered essential to optimize tumour to background ratios and thereby the therapeutic index of radiolabeled minigastrin analogues.
According to reported results, CP04 and 111/natIn-CP04 showed high CCK2R-affinity with the respective IC50s found in the lower nM range (Aloj et al., 2011; Kolenc Peitl et al., 2015). The 111In-CP04 radiotracer previously shown to be very stable in serum (Kolenc Peitl et al., 2015) and in animal tissue homogenates (Ocak et al., 2011), turned out to be fairly stable in peripheral mouse blood in the present work as well (Fig. 2). During a previous comparative biodistribution study within the COST BM0607, 111In-CP04 exhibited high uptake and retention in A431-CCK2R(+) tumours in mice combined with low kidney retention (Laverman et al., 2011) and cleared very rapidly from blood and the background. In the present work identical overall pharmacokinetic profile of 111In-CP04 prepared from the freeze-dried kit (Pawlak et al., 2016) and by wet-labelling was obtained. This finding is a strong demonstration of the efficacy and suitability of the freeze-dried kit formulation for further use in the clinical trial. The kidney retention of 111In-CP04 prepared from kit reconstitution was found low in agreement with previous data. Nevertheless, we aimed to further decrease the kidney retention by co-injecting the plasma expander gelofusine reported to reduce renal uptake of minigastrin radioligands in rodents (Gotthardt et al., 2007; Kolenc Peitl et al., 2015). Evidently, this approach was successful in inducing a significant (P < 0.001) reduction of the renal uptake of 111In-CP04 in our animal model without negatively affecting the radiotracer uptake in the A431-CCK2R(+) xenografts, and led to significant improvement of the tumour-to-kidney ratios (Table 3, Fig. 4).
Previous experience from small-scale studies performed in MTC patients using radiolabelled minigastrin analogues at a peptide dose of 5–10 μg (Froberg et al., 2009) and from the routine pentagastrin test, undesirable effects were recorded due to ligand-induced CCK2R-activation. Adverse reactions included increase of serum calcitonin levels, increase of heart rate, flushes, mild nausea, paraesthesia in the hands and dizziness. These effects were mild and disappeared spontaneously shortly after CCK2R-ligand administration. Biosafety risks related to the pharmacological effects seem to be acceptable for the intended application under certain conditions, such as the administration of the IMP under strict surveillance of the responsible physician and close mesh monitoring plan.
Nevertheless, the toxicity of the CP04 precursor was extensively tested in two animal species, revealing the very low toxicity of CP04. The higher dose of 890 μg/kg tested during the extended acute intravenous toxicity study in rats (Harlan Study #S47364) caused a marked decrease in the reticulocyte count, but the reversibility of this effect remains unknown. Therefore, the lower tested dose 89 μg/kg was set as the NOAEL. It should be noted that the human equivalent dose (HED) calculated for this lower NOAEL value was 14.4 μg/kg (HED (μg/kg) = NOAEL × rat km/human km = 89 μg/kg × 6/37 = 14.4 μg/kg). By taking into account a safety factor of 10, the maximum recommended starting dose (MRSD) for a first-in-human clinical trial would be 1.4 μg/kg.
According to the clinical trial protocol (Eudra-CT No 2015–000,805-38) only adults with confirmed metastatic MTC will be included in the study. Subjects will be intravenously injected with either a lower peptide dose of 10 μg/patient or a higher peptide dose of 50 μg/patient. It should be noted that both doses are below the MRSD. The rationale for selecting the above two doses in the clinical protocol are related to restrictions of CP04 radiolabeling with 200–250 MBq 111In, biosafety considerations due to peptide-induced side-effects and future theranostic use of 177Lu-CP04 for PRRT. Specifically, first applications of 111In-CP04 in man will be performed with the lower peptide dose. Once the biosafety of this approach is clinically established, the higher peptide dose useful for translation to 177In-CP04 for PRRT will be applied.
On the other hand, radiation-associated risk assessment is based on dosimetric calculations derived from animal data. Based on biodistribution data of 111In-CP04 in healthy mice for a 30 min-72 h period pi dosimetric calculations revealed the highest absorbed doses for kidneys (Table 5). By employing two different dosimetric scaling options to translate mouse data to the human situation almost identical values were obtained. The effective activity dose predicted for 111In-CP04 in the clinical trial was below 10 mSv (9.9 mSv/220 MBq). Thus, the effective dose of 111In-CP04 for two hypothetical successive applications would in fact be lower than that of the licensed product OctreoScan® for just one similar application in receptor imaging with SPECT (effective dose of 26 mSv/220 MBq according to SPC). Considering the severity of metastatic MTC this is a justifiable risk for the patient. The comparison of calculated absorbed dose for kidneys would be 27.5 mGy/220 MBq for 111In-CP04, while the respective value for Octreoscan® is being estimated at 108.3 mGy/220 MBq.
5. Conclusion
Toxicity studies have indicated the biosafety of CP04 for single intravenous injection in human planned in the clinical trial. Radiation-associated risk assessment based on dosimetry calculations from animal data has revealed a justifiable risk for the patients. Furthermore, biodistribution experiments in tumour-bearing mice have not only confirmed indistinguishable in vivo behaviour for 111In-CP04 prepared by the freeze-dried kit or by wet-labelling, but also the high and CCK2R-specific tumour-targeting efficacy of 111In-CP04 as well as the role of gelofusine in significantly reducing renal retention. This data is in favour of prompt implementation of the freeze-dried kit formulation without or with gelofusine coinjection in a first multicentre clinical trial in MTC patients.
Acknowledgements
This work and the planned clinical trial is supported by the multinational European project on personalized medicine ERA-NET, Project GRANT-T-MTC. GRAN-T-MTC is part of the ERA-NET on Translational Cancer Research (TRANSCAN) First Joint Transnational Call for Proposals 2011 (JTC 2011) on: “Validation of biomarkers for personalised cancer medicine” funded by the European Commission under the Seventh Framework Programme (FP7) with the following national co-found institutions: Ministry of Health (MoH), Italy, National Centre for Research and Development (NCBiR), Poland, Federal Ministry of Education and Research (BMBF), Germany, Austrian Science Fund (FWF, Project No I1224-B19), Austria, Ministry of Higher Education, Science and Technology (MHEST), Slovenia, General Secretariat for Research and Technology, Ministry of Education, Life Long Learning and Religious Affairs (GSRT), Greece.
References
- Aloj L, Aurilio M, Rinaldi V, D'Ambrosio L, Tesauro D, Peitl PK, Maina T, Mansi R, von Guggenberg E, Joosten L, Sosabowski JK, et al. Comparison of the binding and internalization properties of 12 DOTA-coupled and (1)(1)(1)In-labelled CCK2/gastrin receptor binding peptides: a collaborative project under COST action BM0607. Eur J Nucl Med Mol Imaging. 2011;38:1417–1425. doi: 10.1007/s00259-011-1816-y. [DOI] [PubMed] [Google Scholar]
- Aloj L, Caraco C, Panico M, Zannetti A, Del Vecchio S, Tesauro D, De Luca S, Arra C, Pedone C, Morelli G, Salvatore M. In vitro and in vivo evaluation of 111In-DTPAGlu-G-CCK8 for cholecystokinin-B receptor imaging. J Nucl Med. 2004;45:485–494. [PubMed] [Google Scholar]
- Behe M, Behr TM. Cholecystokinin-B (CCK-B)/gastrin receptor targeting peptides for staging and therapy of medullary thyroid cancer and other CCK-B receptor expressing malignancies. Biopolymers. 2002;66:399–418. doi: 10.1002/bip.10356. [DOI] [PubMed] [Google Scholar]
- Behr TM, Behe MP. Cholecystokinin-B/gastrin receptor-targeting peptides for staging and therapy of medullary thyroid cancer and other cholecystokinin-B receptor-expressing malignancies. Semin Nucl Med. 2002;32:97–109. doi: 10.1053/snuc.2002.31028. [DOI] [PubMed] [Google Scholar]
- Breeman WA, Froberg AC, de Blois E, van Gameren A, Melis M, de Jong M, Maina T, Nock BA, Erion JL, Macke HR, Krenning EP. Optimised labeling, preclinical and initial clinical aspects of CCK-2 receptor-targeting with 3 radiolabeled peptides. Nucl Med Biol. 2008;35:839–849. doi: 10.1016/j.nucmedbio.2008.09.006. [DOI] [PubMed] [Google Scholar]
- Froberg AC, de Jong M, Nock BA, Breeman WA, Erion JL, Maina T, Verdijsseldonck M, de Herder WW, van der Lugt A, Kooij PP, Krenning EP. Comparison of three radiolabelled peptide analogues for CCK-2 receptor scintigraphy in medullary thyroid carcinoma. Eur J Nucl Med Mol Imaging. 2009;36:1265–1272. doi: 10.1007/s00259-009-1098-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Good S, Walter MA, Waser B, Wang X, Muller-Brand J, Behe MP, Reubi JC, Maecke HR. Macrocyclic chelator-coupled gastrin-based radiopharmaceuticals for targeting of gastrin receptor-expressing tumours. Eur J Nucl Med Mol Imaging. 2008;35:1868–1877. doi: 10.1007/s00259-008-0803-4. [DOI] [PubMed] [Google Scholar]
- Gotthardt M, van Eerd-Vismale J, Oyen WJ, de Jong M, Zhang H, Rolleman E, Maecke HR, Behe M, Boerman O. Indication for different mechanisms of kidney uptake of radiolabeled peptides. J Nucl Med. 2007;48:596–601. doi: 10.2967/jnumed.106.036020. [DOI] [PubMed] [Google Scholar]
- von Guggenberg E, Behe M, Behr TM, Saurer M, Seppi T, Decristoforo C. 99mTc-labeling and in vitro and in vivo evaluation of HYNIC- and (Nalpha-His)acetic acid-modified [D-Glu1]-minigastrin. Bioconjug Chem. 2004;15:864–871. doi: 10.1021/bc0300807. [DOI] [PubMed] [Google Scholar]
- von Guggenberg E, Dietrich H, Skvortsova I, Gabriel M, Virgolini IJ, Decristoforo C. 99mTc-labelled HYNIC-minigastrin with reduced kidney uptake for targeting of CCK-2 receptor-positive tumours. Eur J Nucl Med Mol Imaging. 2007;34:1209–1218. doi: 10.1007/s00259-006-0348-3. [DOI] [PubMed] [Google Scholar]
- von Guggenberg E, Rangger C, Sosabowski J, Laverman P, Reubi J-C, Virgolini IJ, Decristoforo C. Preclinical evaluation of radiolabeled DOTA-derivatized cyclic minigastrin analogs for targeting cholecystokinin receptor expressing malignancies. Mol Imaging Biol. 2012;14:366–375. doi: 10.1007/s11307-011-0506-2. [DOI] [PubMed] [Google Scholar]
- von Guggenberg E, Sallegger W, Helbok A, Ocak M, King R, Mather SJ, Decristoforo C. Cyclic minigastrin analogues for gastrin receptor scintigraphy with technetium-99 m: preclinical evaluation. J Med Chem. 2009;52:4786–4793. doi: 10.1021/jm900400w. [DOI] [PubMed] [Google Scholar]
- Keenan MA, Stabin MG, Segars WP, Fernald MJ. RADAR realistic animal model series for dose assessment. J Nucl Med. 2010;51:471–476. doi: 10.2967/jnumed.109.070532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolenc Peitl P, Tamma M, Kroselj M, Braun F, Waser B, Reubi JC, Sollner Dolenc M, Maecke HR, Mansi R. Stereochemistry of amino acid spacers determines the pharmacokinetics of (111)In-DOTA-minigastrin analogues for targeting the CCK2/gastrin receptor. Bioconjug Chem. 2015;26:1113–1119. doi: 10.1021/acs.bioconjchem.5b00187. [DOI] [PubMed] [Google Scholar]
- Kolenc-Peitl P, Mansi R, Tamma M, Gmeiner-Stopar T, Sollner-Dolenc M, Waser B, Baum RP, Reubi JC, Maecke HR. Highly improved metabolic stability and pharmacokinetics of indium-111-DOTA-gastrin conjugates for targeting of the gastrin receptor. J Med Chem. 2011;54:2602–2609. doi: 10.1021/jm101279a. [DOI] [PubMed] [Google Scholar]
- Konijnenberg MW, Breeman WA, de Blois E, Chan HS, Boerman OC, Laverman P, Kolenc-Peitl P, Melis M, de Jong M. Therapeutic application of CCK2R-targeting PP-F11: influence of particle range, activity and peptide amount. EJNMMI Res. 2014;4:47. doi: 10.1186/s13550-014-0047-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koziorowski J, Behe M, Decristoforo C, Ballinger J, Elsinga P, Ferrari V, Kolenc Peitl P, Todde S, Mindt TL. Position paper on requirements for toxicological studies in the specific case of radiopharmaceuticals. EJNMMI Radiopharm Chem. 2016;1:1–6. doi: 10.1186/s41181-016-0004-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laverman P, Joosten L, Eek A, Roosenburg S, Peitl PK, Maina T, Macke H, Aloj L, von Guggenberg E, Sosabowski JK, de Jong M, et al. Comparative biodistribution of 12 (1)(1)(1)In-labelled gastrin/CCK2 receptor-targeting peptides. Eur J Nucl Med Mol Imaging. 2011;38:1410–1416. doi: 10.1007/s00259-011-1806-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mather SJ, McKenzie AJ, Sosabowski JK, Morris TM, Ellison D, Watson SA. Selection of radiolabeled gastrin analogs for peptide receptor-targeted radionuclide therapy. J Nucl Med. 2007;48:615–622. doi: 10.2967/jnumed.106.037085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikiforova MN, Nikiforov YE. Molecular genetics of thyroid cancer: implications for diagnosis, treatment and prognosis. Expert Rev Mol Diagn. 2008;8:83–95. doi: 10.1586/14737159.8.1.83. [DOI] [PubMed] [Google Scholar]
- Nock BA, Maina T, Behe M, Nikolopoulou A, Gotthardt M, Schmitt JS, Behr TM, Macke HR. CCK-2/gastrin receptor-targeted tumor imaging with (99 m)Tc-labeled minigastrin analogs. J Nucl Med. 2005;46:1727–1736. [PubMed] [Google Scholar]
- Ocak M, Helbok A, Rangger C, Peitl PK, Nock BA, Morelli G, Eek A, Sosabowski JK, Breeman WA, Reubi JC, Decristoforo C. Comparison of biological stability and metabolism of CCK2 receptor targeting peptides, a collaborative project under COST BM0607. Eur J Nucl Med Mol Imaging. 2011;38:1426–1435. doi: 10.1007/s00259-011-1818-9. [DOI] [PubMed] [Google Scholar]
- Pacini F, Castagna MG, Cipri C, Schlumberger M. Medullary thyroid carcinoma. Clin Oncol (R Coll Radiol) 2010;22:475–485. doi: 10.1016/j.clon.2010.05.002. [DOI] [PubMed] [Google Scholar]
- Pawlak D, Rangger C, Kolenc-Peitl P, Garnuszek P, Maurin M, Ihli L, Kroselj M, Maina T, Maecke H, Erba P, Kremser L, et al. From preclinical development to clinical application: kit formulation for radiolabelling the minigastrin analogue CP04 with In-111 for a first-inhuman clinical trial. Eur J Pharm Sci. 2016 doi: 10.1016/j.ejps.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reubi JC, Maecke HR. Peptide-based probes for cancer imaging. J Nucl Med. 2008;49:1735–1738. doi: 10.2967/jnumed.108.053041. [DOI] [PubMed] [Google Scholar]
- Reubi JC, Waser B. Unexpected high incidence of cholecystokinin-B/gastrin receptors in human medullary thyroid carcinomas. Int J Cancer. 1996;67:644–647. doi: 10.1002/(SICI)1097-0215(19960904)67:5<644::AID-IJC9>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- Reubi JC, Schaer JC, Waser B. Cholecystokinin(CCK)-A and CCK-B/gastrin receptors in human tumors. Cancer Res. 1997;57:1377–1386. [PubMed] [Google Scholar]
- Sosabowski JK, Lee M, Dekker BA, Simmons BP, Singh S, Beresford H, Hagan SA, McKenzie AJ, Mather SJ, Watson SA. Formulation development and manufacturing of a gastrin/CCK-2 receptor targeting peptide as an intermediate drug product for a clinical imaging study. Eur J Pharm Sci. 2007;31:102–111. doi: 10.1016/j.ejps.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Stabin MG. Fundamentals of Nuclear Medicine Dosimetry. 1 ed. Springer-Verlag; New York: 2008. [Google Scholar]
- Stabin MG, Sparks RB, Crowe E. OLINDA/EXM: the second-generation personal computer software for internal dose assessment in nuclear medicine. J Nucl Med. 2005;46:1023–1027. [PubMed] [Google Scholar]
- Todde S, Windhorst AD, Behe M, Bormans G, Decristoforo C, Faivre-Chauvet A, Ferrari V, Gee AD, Gulyas B, Halldin C, Peitl PK, et al. EANM guideline for the preparation of an Investigational Medicinal Product Dossier (IMPD) Eur J Nucl Med Mol Imaging. 2014 doi: 10.1007/s00259-014-2866-8. [DOI] [PubMed] [Google Scholar]
- Wells SA, Jr, Asa SL, Dralle H, Elisei R, Evans DB, Gagel RF, Lee N, Machens A, Moley JF, Pacini F, Raue F, et al. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. 2015;25:567–610. doi: 10.1089/thy.2014.0335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Yang PL, Gray NS. Targeting cancer with small molecule kinase inhibitors. Nat Rev Cancer. 2009;9:28–39. doi: 10.1038/nrc2559. [DOI] [PMC free article] [PubMed] [Google Scholar]