Abstract
Background
The Institute of Medicine (2006) recommended that cancer survivors completing primary treatment receive a survivorship care plan (SCP) based on face validity. The state of scientific knowledge regarding SCP is unclear. We conducted an integrative review of existing evidence regarding SCP.
Methods
We searched MEDLINE /PubMed, EMBASE, and CINAHL for relevant studies published between 2006 – 2013 using a combination of keywords: ‘survivors,’ ‘survivorship,’ ‘care plans,’ ‘care planning,’ ‘treatment summaries’ and ‘cancer.’ Articles were included if they (1) reported results of an empirical study; (2) included cancer survivors diagnosed at age 18 or older; (3) related to SCP; and (4) were published in English. A total of 781 records were retrieved; 77 were duplicates, 665 were abstracts or presentations, did not relate to SCP for adults or were not empirical – leaving 42 for inclusion in this review.
Results
Studies regarding SCP fell into three categories: (a) content (n=14); (b) dissemination and implementation (n=14); and (c) survivor and provider outcomes (n=14). SCP were endorsed and associated with improved knowledge, but SCP use remains sporadic. Only 4 studies were randomized controlled trials (RCT) that avoided many biases associated with observational studies. Other limitations included cross-sectional or pre-post designs, limited generalizability due to lacking sample diversity, and lack of systematic testing of data collection tools.
Conclusions
The quantity and quality of SCP research is limited. SCP were endorsed, but evidence of improved outcomes associated with SCP is limited. Future research that addresses extant studies’ methodological concerns is needed regarding SCP use, content, and outcomes.
Keywords: survivorship, cancer, dissemination, implementation, content, outcomes
There are now almost 14 million cancer survivors in the US, and this number is projected to increase in the next 10 years as the population ages.1 As improvements in cancer treatments increase the number of long-term survivors, survivorship health issues have emerged as an important public health concern.2 Multiple recent studies have demonstrated that cancer survivors are less likely to receive general preventive care and care associated with non-cancer-related medical conditions than individuals without cancer.3
As a result, there is increasing attention on research and interventions to improve the health care – and health – of cancer survivors. The 2005 Institute of Medicine (IOM) report, “Cancer Patient to Cancer Survivor: Lost in Transition,”(1) highlighted concerns about care for cancer survivors and recommended survivorship care plans (SCP), documents which include “a personalized treatment summary, information on possible late and long-term effects, information on signs of recurrence, guidelines for follow-up care,” as a “common sense” approach to addressing these concerns.(1) The IOM report recognized that this recommendation was not supported by empiric evidence at that time but had face validity in improving communication among health care providers (e.g., between the oncologist and primary care providers [PCP]) and survivors and, consequently, improving quality of care and outcomes following cancer treatment. More recently, the American College of Surgeon’s Commission on Cancer, which accredits US cancer programs, announced that SCP implementation will be required for accreditation starting in 2015.4
In light of these high-profile endorsements of SCP as a means of improving care and outcomes for cancer survivors, a body of research on the use, content, and outcomes of SCP has developed. The results of this research and conclusions that may be drawn from it have not previously been summarized. A summary of SCP research could inform efforts to refine content, improve associated outcomes, and promote use. As such, our objective was to summarize the state of scientific knowledge currently available regarding SCP for adult cancer survivors. In addition to achieving this objective, we identify gaps in knowledge regarding SCP to be addressed in future research.
Methods
To summarize empirical literature regarding SCP use in adult cancer survivors, we conducted an integrative review.67
An integrative review differs from other types of reviews such as meta-analyses, which use statistical analyses to synthesize studies with similar study designs and hypotheses, and systematic reviews, which combine evidence from several studies using a statistical or quasi-statistical approach to answer a particular clinical question. Integrative reviews summarize evidence from studies with diverse methodologies (e.g., experimental and non-experimental studies) to provide information regarding the state of the science for a particular phenomenon.7
We used the PRISMA guidelines in preparing our strategy and this report.68
Search Strategy
We searched the following databases: (1) PubMed; (2) the Excerpta Medica Database (EMBASE®); and (3) the Cumulative Index to Nursing and Allied Health Literature (CINAHL). An experienced research librarian with expertise in cancer used a list of terms and medical subject headings (MeSH®) developed by the first and second authors. Table 1 lists search terms and limits for each database. We searched for articles published between 2006 and 2013 because the 2005 IOM report “Cancer Patient to Cancer Survivor: Lost in Transition”2 recommended SCP while recognizing that empirical evidence was needed. Our objective was to summarize research that responded to the IOM report. A total of 781 articles were identified with this approach.
TABLE 1.
| PubMed | ||
|---|---|---|
| Search # | Query | Items Found |
| 1 | Search Survivors[MesH] OR survivorship OR survivors OR survivor | 815,323 |
| 2 | Search Survivors[MesH] OR survivorship OR survivors OR survivor Filters: English | 748,414 |
| 3 | Search Survivors[MesH] OR survivorship OR survivors OR survivor Filters: Publication date from 2006/01/01 to 2014/12/31; English | 349,794 |
| 4 | Search Neoplasms[MeSH] OR cancer[all fields] Filters: Publication date from 2006/01/01 to 2014/12/31; English | 823,568 |
| 5 | Search Patient care planning[MeSH] OR “care plan”[all fields] OR “care plans”[all fields] OR “care planning”[all fields] OR “treatment summary”[all fields] OR “treatment summaries”[all fields] Filters: Publication date from 2006/01/01 to 2014/12/31; English | 13,917 |
| 6 | #3 AND #4 AND #5 Filters: Publication date from 2006/01/01 to 2014/12/31; English |
345 |
| EMBASE®d | ||
| Search # | Query | Items Found |
| 1 | ’cancer survivor’/exp OR ’survivor’/exp OR survivors OR survivorship | 78,605 |
| 2 | ’neoplasm’/exp OR ’cancer’ | 3,853,791 |
| 3 | ’patient care planning’/exp OR ’nursing care plan’/exp OR ’care plan’ OR ’care plans’ OR ’care planning’ OR ’treatment summary’ OR ’treatment summaries’ | 110,106 |
| 4 | #1 AND #2 AND #3 | 537 |
| 5 | #1 AND #2 AND #3 AND [english]/lim AND [embase]/lim AND [2006–2014]/py | 397 |
| CINAHLe | ||
| Search # | Query | Items Found |
| 1 | (MH “Neoplasms+”) OR “cancer” | 204,338 |
| 2 | (MH “Survivors+”) OR “survivors” OR (MH “Cancer Survivors”) | 16,886 |
| 3 | “survivor” OR “survivorship” | 3,071 |
| 4 | S2 OR S3 | 18,119 |
| 5 | (MH “Patient Care Plans+”) OR (MH “Nursing Care Plans+”) OR “care plans” | 6,369 |
| 6 | “care plan” OR “care planning” OR “patient care planning” OR “treatment summary” OR “treatment summaries” | 4,202 |
| 7 | S5 OR S6 | 9,590 |
| 8 | S1 AND S4 AND S7 | 121 |
| 9 | S1 AND S4 AND S7 Limiters – Published Date: 20060101–20141231; English Language |
115 |
| 10 | S1 AND S4 AND S7 Limiters – Published Date: 20060101–20141231; English Language; Exclude MEDLINE records |
39 |
All searches conducted on December 6, 2013 and included publication dates through 2014 to account for e-pub ahead of print.
Final search listed for each database represents number of articles reviewed
Duplicate records were found across databases. Records found in Medline only were excluded, but items indexed by both EMBASE® and Medline were included, and some of these might have also appeared in CINAHL.
Excerpta Medica Database
Cumulative Index to Nursing and Allied Health Literature
Review Process
To be included in the full-text review, articles had to meet the following inclusion criteria: (1) Report results of an empirical study; (2) relate to survivors diagnosed at age 18 or older; (3) relate to cancer; and (4) report findings associated with SCP. Three authors reviewed abstracts from the first 50 articles, reaching agreement on whether or not 37 (75%) articles should be included in the full-text review. Discrepancies were then reviewed and discussed until consensus was reached. In most cases, the reason for disagreement was obvious (e.g., misapplication of inclusion/exclusion criteria). The same three authors then each independently reviewed a third of the remaining abstracts. Articles meeting inclusion criteria based on the review of abstracts underwent full-text review. Further exclusions were made when the articles did not meet the inclusion criteria at this level of review (e.g. were abstracts or presentations; focused on adult survivors of childhood cancers; or did not include empiric data).
Data abstraction
Data from articles meeting inclusion criteria based on the full-text review were abstracted. Each author abstracted information regarding study characteristics and the PICOTS (Population, Intervention, Comparator, Outcomes, Timing, and Setting) for a third of included articles. Articles were graded based on levels of evidence identified by the National Cancer Institute.9, 10
Level I: prospective, randomized, controlled trials and meta-analyses of prospective, randomized, controlled trials;
Level II: prospective, nonrandomized, controlled trials; prospective cohort studies; prospective case series; and cross-sectional studies;
Level III: retrospective studies including case-control and case studies or reports; and
Level IV: opinions of respected authorities based on clinical experience, consensus statements from expert committees, or authoritative reviews.
The first author reviewed all abstractions for completeness and accuracy. Articles were also classified based on their methods (e.g., observational, randomized controlled trial, etc.), outcomes assessed (e.g., survivor preferences, health care service utilization), and other relevant characteristics (e.g., study population).
Results
Figure 1 describes the number of articles that we identified as evidence associated with SCP. From an initial yield of 781 articles, 42 articles were empirical studies of cancer SCP for survivors age 18 or older published in English between 2006-and 2013 and thus met the criteria for inclusion in the integrative review. Based on the review of the final selection of articles, articles were grouped into one of three areas: 1) SCP content and delivery, including formative work on what should be included in SCP (n=14); 2) Dissemination and Implementation studies to evaluate SCP use (n=14); and 3) Survivor- and provider-level outcomes associated with SCP use (n=14). Most of these studies were published since 2011; 19% were published between 2006 and 2011, 26.2% in 2011, 16.7% in 2012 and 38.1% in 2013.
FIGURE 1.
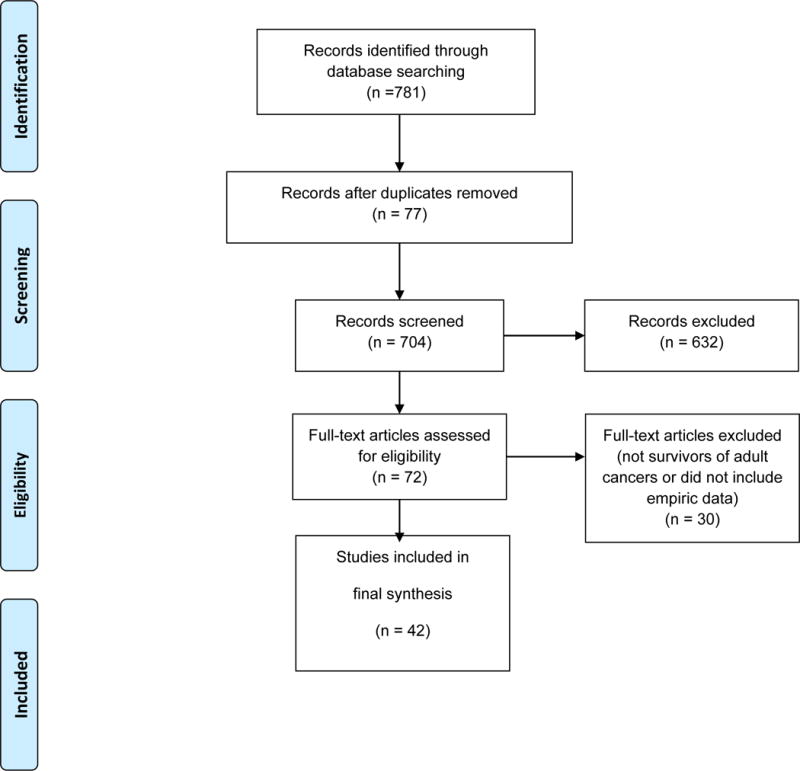
PRISMA Flow Diagrama
aFrom: Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(6): e1000097. doi:10.1371/journal.pmed1000097
I. SCP Content
There were 14 studies that focused on SCP content and delivery preferences using a number of methods.11–21, 21–23 Each of these studies is summarized in Table 2. Focus groups were used in 8 of the studies, including 7 with cancer survivors; 5 were conducted with breast cancer survivors; and 3 were conducted specifically with African American women with breast cancer. Interviews (n= 6) were conducted more often with providers (oncologists, PCP, nurses and navigators or cancer program administrators) than with survivors. In the 5 studies that used surveys, both survivors and providers were surveyed.12, 24–27 Only one survey study had a pre-post SCP design28; 3 had a post-SCP delivery design.24, 29, 30
TABLE 2.
Survivorship Care Plan Content-focused Studies (n= 14)
| Evidence level | Primary author, year | Data collection/methods | Sample and setting | Intervention | Results (data) | Conclusions |
|---|---|---|---|---|---|---|
| 4 | Ashing-Giwa, 2013 | Focus groups | 25 African-American BCS and 3 advocates: ages 32–79, 60% ≥ 5 years post diagnosis | ASCO SCP Template | African-American BCS believed that increased mortality may be due to comorbidities and inadequate surveillance and follow-up care. Participants recommended that the SCP document all comorbidities and medications; allow PCP to participate; and make referrals to providers familiar with treating African-American BCS, who note the importance of spirituality and disproportionately high levels of socioecological stress. | Current SCP lacked cultural responsiveness and patient-centeredness. |
| 4 | Baravelli, 2009 | Survey and interviews | 20 survivors, ages 31–81, completed the survey regarding survivorship experiences; 14 PCP participated in interviews; 12 survivors reviewed a sample SCP; 95 health care professionals completed the survey regarding SCP elements. | SCP with ASCO colorectal cancer flow sheet | Participants expressed strong support for SCP use but had differing opinions on content and when to deliver SCP. | SCP concept endorsed but survivors and nurses wanted more supportive care and psychosocial elements included in SCP than PCP. |
| 4 | Burg, et al. 2009 | Focus groups | Purposive sampling 32 BCS from Sister’s Network: 29 African-American, 1 Hispanic, 2 white | ASCO SCP template | Survivors were dissatisfied with the amount of information they received on cancer-related side-effects, including race-specific information. | SCP were viewed as important but ASCO template too technical and limited in information on side-effects and self-care approaches. |
| 4 | Haq, 2013 | Focus groups and interviews | Purposive sampling of 61 BCS (mean age 55.5), family physicians and oncologists | SCP | In the first study phase, BCS indicated that both web- and paper-based SCP with human resources components were desirable and described their evolving needs throughout their cancer journey; family physicians indicated that they needed key information in a user-friendly format. | BCS and family physicians felt Participants thought that the SCP developed in the study’s second phase was an improvement over the standard of care. |
| 4 | Hewitt, 2007 | Focus groups and interviews | 3 focus groups of survivors; 3 focus groups with 34 oncology nurses; 2 focus groups of PCP; 20 interviews with oncologists | SCP | Survivors expressed support for SCP. PCP indicated that SCP would help with follow-up care. Nurses suggested that they could play a key role in developing and delivering SCP, whereas physicians recognized the value of SCP but were unwilling to assist in their use due to time constraints. | Endorsed SCP concept but identified barriers that might interfere with implementation. |
| 4 | Hill-Kayser, 2009 | Survey | 3343 survivors: median age at cancer diagnosis: 48 years (range: 18–100+); median current age: 51 years (range: 18–100+); 71% women; 86% white; 78% college-educated; 2% reported more than one cancer diagnosis. 1880 users completed OncoLife surveys; of these, 64% were survivors (64.2%, n = 1198); 25% were health care providers; and 12% were friends/family members of survivors. 150 users completed satisfaction surveys; of these, 57% were survivors or family members/friends of survivors; 43% were health care providers. | OncoLife, an Internet-based SCP tool | Ninety-eight percent of health care providers rated their experience using OncoLife as “good” to “excellent”; 95% survivors/friends/family members rated their experience “good” to “excellent.” | Participants were satisfied with an online self-developed SCP. |
| 4 | Hill-Kayser, 2012 | Survey | Between May 2007 and October 2009, 8717 SCP were created. Forty-eight percent were for BCS, mean age at diagnosis: 48.5 (range: 18–85); mean current age: 51.6 years (range: 19–89); mean time since diagnosis: 3 years (range <1–39); 89% white; 83% attended at least some college. | OncoLife, an Internet-based SCP tool | Fifty-eight percent of users reported finding the amount of information presented in SCP to be “just right”; 6% found it to be too much; 24% found it to be too little. | Participants satisfied with content in self-developed online SCP. |
| 2 | Jefford, 2011 | Survey and interviews | Ten CCS survivors within a year of completing treatment | SurvivorCare intervention included booklet; DV; question prompt list; SCP; end-of-treatment nurse visit; and 3 follow-up phone calls | CCS felt intervention package was useful, relevant and convenient. SCP took 1–1.5 hours to complete. | SCP as a component of SurvivorCare was well received. |
| 4 | Kantsiper, 2009 | Focus groups | Twenty-one survivors in 5 groups, 15 PCP in 2 groups, and 16 oncology specialists in 2 groups. One survivor group consisted of four African-Americans. | SCP | Survivors form intense relationships with specialists and rely on them for reassurance and expertise. Many believed PCP lacked necessary oncology expertise. Survivors reported psychosocial and communication issues. African-Americans cited concerns about access to care and clinical trials, as well as taboos to discussing cancer. Specialists reported that they struggle with discharging survivors due to protective relationships. PCP were concerned about time and training to provide survivorship care and communication problems with oncologists. Written SCP were regarded by all groups as possibly helpful but insufficient to ease the transition. | BCS may experience difficulties transitioning to survivorship, including ongoing psychosocial issues. African-American survivors may face additional and unique barriers to successful survivorship. Oncology specialists may have concerns about discharging cherished survivors. |
| 4 | Marbach & Griffie, 2011 | Focus groups | Forty survivors in 4 groups | SCP | Want written treatment plan and SCP. Wanted SCP in writing and delivered in person. Would trust nursing staff to provide SCP. | Endorsed SCP concept, especially need for written surveillance for late effects. |
| 4 | Mayer, 2012 | Focus groups and interviews | 4 focus groups of 29 survivors; 5 PCP interviews | 5 SCP templates | No survivor had received SCP but endorsed content and preferred JourneyForward template; providers wanted an abbreviated version. | SCP are necessary but not sufficient to address needs during transition in care. |
| 4 | Smith, 2011a | Focus groups | 26 BCS in 5 groups, ages 45–80. | SCP | BCS indicated preferences for the inclusion of a TS, information on nutrition/exercise, expected side effects, signs and symptoms of recurrence, recommended follow-up schedule, information sent to PCP, and updates on changes in SCP. BCS preferred individualized content based on physical and psychosocial effects. Rural BCS preferred electronic formats. | SCP core elements would be helpful but also need ability to individualize content. |
| 4 | Smith, 2011b | Survey | 577 PCP | SCP | PCP wanted diagnosis, TS and recommended surveillance in discharge letter from oncologists. | PCP satisfied with discharge letter that included treatment summary and surveillance plan. |
| 4 | Shalom, 2011 | Interviews | 15 PCP who had received at least 1 SCP | SCP | PCP felt more confident and better prepared after reading SCP in delivering care and 8/15 changed care as a result. | SCP valued by PCP who felt more confident in care delivery. |
Abbreviations: ASCO, American Society of Clinical Oncology; BCS, breast cancer survivor; CCS, colorectal cancer survivor; IOM, Institute of Medicine; NCI, National Cancer Institute; PCP, primary care provider; RCT, randomized controlled trial; SCP, survivorship care plan; TS, treatment summary
SCP content preferences
Many of the studies used SCP templates to elicit feedback; the most common were templates from the American Society of Clinical Oncology or JourneyForward™. Most participants endorsed the concept of a SCP while some identified it as ‘necessary but not sufficient’ when transitioning a survivor to survivorship care. There were differing opinions about what content should be included: Survivors wanted more content on health promotion, psychosocial support, and financial and other resources and emphasized a need for flexibility and tailoring, whereas providers preferred a streamlined version that clearly identified what components of care they were responsible for administering.
SCP delivery preferences
Both paper and electronic SCP were identified as useful by survivors but some preferred to receive both. Mayer20 and Haq14 found that respondents preferred for SCP to be delivered either directly preceding or directly following treatment. Survivors wanted a treatment plan to be delivered at the time of diagnosis. Most of these studies did not address preferences for timing nor who should deliver the SCP.
Limitations
The strength of evidence for content studies was low, with all studies using observational designs. Studies employing focus groups have included primarily white breast cancer survivors. Data collection tools (e.g., surveys; interview guides) were not systematically tested, limiting reliability and validity.
II. Dissemination and Implementation
Outcomes of interest included: SCP use in cancer programs and among cancer care providers (6/14); survivor and PCP receipt of SCP (5/14); retention of SCP (1/14); and determinants of SCP use (7/14).31–42 Each of these studies is summarized in Table 3. To measure these outcomes, most SCP dissemination and implementation studies used surveys (11/14); 2 used interviews; and 1 used both interviews and focus groups. In most of these studies, the unit of analysis was the individual provider or survivor (9/14); for the remaining 5 studies, the unit of analysis was the cancer program. The stakeholder of interest for most studies was survivors (7/14); PCP, cancer care providers, and cancer programs were each represented in 3 studies.
TABLE 3.
Survivorship Care Plan Dissemination and Implementation-focused Studies (n= 14)
| Evidence level | Primary author, year | Data collection/methods | Sample and setting | Intervention | Results (data) | Conclusions |
|---|---|---|---|---|---|---|
| 3 | Hahn, 2011 | Interviews | Clinicians such as oncology nurse specialists, social workers, and nurse practitioners; administrative personnel such as program coordinators and quality improvement staff at an academic medical center, a community hospital, a primary care medical group, and a county hospital | SCP | Each survivorship program developed and implemented unique types of SCP documents. | The SCP document is a flexible tool that can be successfully adapted for use in extremely varied settings, from primary care to hospitals, to inform and educate survivors and providers. |
| 4 | Birken, 2013 | Survey | 23 cancer programs in the Southeast Atlantic United States | SCP | Eighty-six percent of cancer programs reported some SCP use; less than a quarter of cancer programs’ providers had ever used SCP; 61% began using SCP because of professional societies’ recommendations. Key barriers to SCP use were insufficient organizational resources (75%) and systems for SCP use. Patterns were found in SCP use across location, program type and professional society membership. | Most cancer programs have adopted SCP, but use remains inconsistent. Efforts to promote SCP use should address barriers, particularly in cancer programs that are susceptible to barriers to SCP use. |
| 4 | Birken, 2014 | Survey | Eighty-one cancer programs throughout the United States with a wide range of annual incident cancers, program types, and cancer care quality improvement organization memberships | SCP | Fifteen percent of cancer programs developed SCPs for ≥75% survivors; 25% delivered ≥75% SCPs to survivors; 23% delivered ≥75% SCPs to PCP; 4% met all three of these criteria. SCP use consistency was associated with geographic region (p = .05), initiating SCP use in response to survivors’ requests (p = .03), and membership in the National Cancer Institute’s National Community Cancer Centers Program (p = .01). | SCP use is highly inconsistent. Survivors might improve SCP use consistency by initiating SCP use; cancer care quality improvement organizations might improve it by specifying how SCP use compliance will be assessed. |
| 4 | Campbell, 2012 | Survey | A convenience sample of 20 head and neck cancer survivors; 21 physicians and dentists in an ambulatory, tertiary care medical center | SCP | Only 2/20 survivors and 11/21 physicians or dentists could locate or remember receiving the SCP 3 years later. Eighteen of 20 survivors were unsure of the value of SCP. | Neither head and neck cancer survivors nor their PCP were aware of SCP 3–4 years after receiving them. |
| 4 | Chubak, 2012 | Interviews | 40 clinical leaders, administrators, and providers in oncology, primary care, nursing administration, and specialty care in 10 Cancer Research Network sites | SCP | Twenty-five percent of respondents were not familiar with SCP; 12.5% used SCP. Electronic health records were used as a communication tool. Respondents’ survivorship services were mostly educational. | Interview participants were aware of survivorship care planning, but approaches vary. |
| 4 | Dulko, 2013 | Survey | Thirty-nine PCP completed surveys and 58 BCS/CCS participated in a telephone survey in an urban academic medical center and a rural community academic cancer center in Vermont. | SCP | Mean SCP preparation time was 53.9 minutes; the perceived optimal time to deliver SCP was 3–6 months after treatment ended. Sixty-four percent of PCP cited limited access to survivors as a barrier to providing follow-up care; 58% reported insufficient knowledge of survivorship issues. Eighty-three percent of survivors found the SCP visit very useful. | Time to develop SCP may be a barrier to widespread implementation. Survivors find SCP useful, but PCP feel insufficient knowledge of survivorship issues is a barrier to providing best follow-up care. |
| 4 | Forsythe, 2013 | Survey | Nationally representative sample of 1130 medical oncologists and 1020 PCP | Oncologist provision and PCP receipt of SCP | Nearly half of oncologists reported always/almost always providing TS, whereas 20% reported always/almost always providing SCP (TS + follow-up plan). A third of PCP indicated always/almost always receiving TS; 13.4% reported always/almost always receiving SCP. Oncologists who reported training in late- and long-term effects of cancer and use of electronic medical records were more likely to report providing SCP (P< .05). PCP receipt of SCP was associated with better PCP-reported care coordination, physician–physician communication, and confidence in survivorship care knowledge compared to receipt of neither TS nor SCP (P< .05). | Confidence regarding survivorship care knowledge may differ from actual knowledge. Providing SCP to PCP may enhance survivorship care coordination, physician–physician communication, and PCP confidence. However, considerable progress will be necessary to achieve implementation of sharing SCP among oncologists and PCP. |
| 4 | Friedman, 2010 | Survey | 67 non-Hodgkin lymphoma survivors, ages 29–86, and 22 physicians | SCP | > 50% concordance on 11 of 19 content areas; 8 areas were low in concordance with mostly psychosocial and financial issues. | Survivors prefer SCP centered on medical issues and coordination between oncologists and PCP. Tailoring SCP to tumor groups is important. |
| 4 | Hewitt, 2007 | Interviews and focus groups | 34 nurses included advanced practice nurses and ambulatory office-based nurses. 20 oncologists (urologists and radiation, medical, and gynecologic oncologists). PCP were family practitioners and internists. Survivors were ages 25–70, men and women, with different types of cancer. | SCP | Survivors reported satisfaction with post-treatment medical care, but felt that their psychosocial needs were not met. Survivors expressed enthusiastic support for receipt of SCP. PCP viewed themselves as playing an important role during the post-treatment period and indicated that a written SCP for follow-up would help them improve their survivorship practices. Nurses recognized the need to improve survivorship care and suggested that they could play an active role in creating and implementing SCP. Physicians providing oncology care acknowledged the value of SCP, but were not inclined to complete them because such plans would not reduce other reporting and communication requirements and would be burdensome to develop. | Survivorship care planning (including SCP) is viewed favorably by consumers, nurses, and physicians; however, there are many barriers to SCP use. |
| 4 | Hill-Kayser, 2009 | Survey | From May 2007 to November 2008, 3343 individuals (Survivors, providers, and friends/family of survivors) utilized OncoLife. | Use and satisfaction with OncoLife, an internet-based program for creating SCP | 25% of respondents were health care providers; 12% friends/family of survivors; 63% survivors, median age at diagnosis: 48 (range 18–100+); median current age: 51 (range 19–100+); 87% white, 71% female; 82% college-educated. Cancer types included 46% breast; 12% hematologic; 11% gastrointestinal; 9% gynecologic; 8% genitourinary. Eighty-four percent had undergone surgery; 80% chemotherapy; 60% radiotherapy. Fifty-three percent reported receiving follow-up care from an oncologist only; 13% from a PCP only, 32% from both an oncologist and PCP. Twelve percent reported having received survivorship information previously. Over 90% survivors and health care providers reported satisfaction levels of “good” to “excellent” using OncoLife. | Survivors and health care providers appear both willing to use this type of tool and satisfied with the information provided. Most users have never before received survivorship information. |
| 4 | Merport, 2012 | Survey | Massachusetts practice cancer specialists (75% male; 60% medical oncologists; 40% radiation oncologists; 32% hematologists; 55% worked in a hospital setting); PCP (51% male) | SCP and TS | Fifty-six percent of cancer specialist physicians reported that they, or their staff, prepared TS for their survivors; however, only 14% reported preparing SCP. Fifty-four percent of PCP reported ever receiving a TS, but only 16% ever received a SCP. Cancer specialists cited lack of training, reimbursement, and templates as barriers to preparing SCP. | Interventions, such as specific training, reimbursement, and templates that capture automated data, are needed to make TS and SCP a part of standard care. |
| 4 | Salz, 2012 | Survey | 53 NCI-designated cancer programs | SCP | Forty-three percent used SCP for BCS and/or CCS; 50% indicated that they planned to use SCP. None of the programs that used SCP included all IOM-recommended elements. | Adoption and implementation of SCP is poor, possibly due to barriers such as lack of time and staff. |
| 4 | Schootman, 2013 | Survey | 9530 survivors who completed the Missouri Behavioral Risk Factor Surveillance System | SCP and TS | Twenty-four percent of respondents received TS. There were no significant differences between those who received TS and those who did not with respect to a variety of sociodemographic factors. Rural survivors were less likely to receive SCP than urban survivors. | Rural survivors face many health challenges. Interventions should be adapted to meet their needs. |
| 4 | Stricker, 2011 | Survey | SCP for 65 survivors in 13 LiveSTRONG Centers of Excellence | SCP | 61.5% used institutionally created templates. Concordance of content with IOM recommendations for TS and SCP varied from 0.01–98. SCP chart abstraction took from 31->60 minutes in 12/13 sites. | Accordance with IOM recommendations is limited in most cancer programs. Time may be a barrier to completeness. Research is needed to identify essential SCP elements. |
Abbreviations: ASCO, American Society of Clinical Oncology; BCS, breast cancer survivor; CCS, colorectal cancer survivor; IOM, Institute of Medicine; NCI, National Cancer Institute; PCP, primary care provider; RCT, randomized controlled trial; SCP, survivorship care plan; TS, treatment summary
Determinants of SCP use
Only 3 studies conducted statistical tests of relationships between SCP use and hypothesized determinants. Birken, Mayer and Weiner (2013)32 found in their study of 23 cancer programs in the South Atlantic division of the American Cancer society that cancer programs reporting no SCP use were located in a single state, and cancer programs reporting no SCP use were all teaching hospitals, none of which was a member of the American Hospital Association. A study of 81 cancer programs throughout the US with a wide range of annual incident cancers, program types, and cancer care quality improvement organization memberships33 found that consistent SCP use (i.e., development and delivery of SCP to all survivors and their PCP) was associated with geographic region, initiating SCP use in response to survivors’ requests, and membership in the National Cancer Institute’s National Community Cancer Centers Program. Forsythe et al. (2013)37 found in a study using a nationally representative sample of oncologists that oncologists with training in late- and long-term effects of cancer and those who used electronic medical records were more likely to report SCP use. Several descriptive studies reported that barriers to SCP use included insufficient resources such as time, staff, training, templates and funding.15, 43–45,15, 32, 40 Nurses indicated that their involvement could facilitate SCP use.46
SCP use in cancer programs and among cancer care providers
The 11 studies that assessed SCP use were consistent in reporting that SCP use was limited. Most US cancer programs reported some SCP use, but less than a quarter of cancer programs’ providers had ever used a SCP.43,32 Just 1 of 36 US cancer programs surveyed developed and delivered SCP to at least 75% of all survivors and their PCP.33 Only 12.5% of 10 Cancer Research Network cancer program representatives reported SCP use.47 Forsythe et al. (2013) found in their nationally representative sample that 20.2% of cancer care providers reported always/almost always providing SCP.37 Merport et al. (2012)48 found in their study of Massachusetts cancer programs that 14% of cancer care providers reported preparing SCP.
SCP receipt
In their study of Massachusetts practices, Merport et al. (2012) found that 16% of PCP had ever received a SCP.40 Campbell, Massey and Myers (2012) assessed 20 head and neck cancer survivors and 21 of their physicians and dentists in an ambulatory, tertiary care medical center.34 They found that only 2 survivors (10%) and 11 providers (52%) were able to locate or remember having received the SCP 3 years later. Schootman et al. (2013) conducted the only statistical tests of determinants of SCP receipt in their study of Missouri cancer survivors, 24% of survivors received SCP; rural survivors were less likely than urban survivors to receive a SCP.41 Some of the studies identified the nurse as the person who delivered the SCP.15, 21, 31, 31 However most inferred that the oncologist was responsible for delivering the SCP.
Limitations
The strength of evidence from dissemination and implementation studies was generally low because they were all observational. Each dissemination and implementation study employed methods that relied on respondents’ self-reported outcomes of interest (i.e., surveys, focus groups, interviews). Consequently, each study was subject to social desirability bias (i.e., tendency to respond to questions in ways that will be viewed as favorable49. All of these studies were cross-sectional, limiting the ability to infer causality. No study described efforts to systematically test the validity and reliability of survey items or focus group or interview questions. Several characteristics of dissemination and implementation studies limited their generalizability: Ten of the 14 studies had small samples; 8 were limited by selection bias, often associated with convenience samples; and among the 7 studies that assessed survivor-level outcomes, 6 lacked variation in survivor characteristics including demographics and cancer type.
III. SCP Outcomes
Fourteen studies focused on the potential influence of SCP on survivor- (13/14), provider- (1/14), and -level outcomes (2/14). Each of the studies is summarized in Table 4.30, 50–64 Three of these were randomized controlled trials (RCT) and 11 were observational studies, including eight survivor surveys54, 58, 61, 62, 65–68, 69 and two interview studies of survivors30, 63, 63 and oncology providers.63 Two observational studies analyzed administrative data.58, 70, 60 Five observational studies included a comparison group that either reflected survivor outcomes prior to an SCP intervention60, 61 or a concurrent group of survivors that did not receive an SCP.54, 59, 71
TABLE 4.
Survivorship Care Plan Outcome-focused Studies (n=14)
| Evidence level | Primary author, year | Data collection/methods | Sample and setting | Intervention | Results (data) | Conclusions |
|---|---|---|---|---|---|---|
| 1 | Grunfeld, 2011 | RCT | 408 women with early-stage breast cancer who completed primary treatment at least 3 months previously; mean age: 61.7; median time since diagnosis: 35.3 months. | Intervention group: Discharge visit plus SCP, reviewed during a 30-minute educational session with a nurse and delivered to PCP. Control group: Discharge visit only. | There were no differences between groups on cancer-related distress, satisfaction, or QOL. More survivors in the intervention than control group correctly identified their PCP as primarily responsible for follow-up (98.7% vs. 89.1%; difference, 9.6%; 95% CI, 3.9 to 15.9; p = .005) | The results do not support the hypothesis that SCPs are beneficial for improving patient-reported outcomes. |
| 1 | Hershman, 2013 | RCT | 126 BCS within 6 weeks of completing adjuvant therapy; mean age: 54; 48% Hispanic. | Intervention group: SCP delivered in 1-hour visit with a nurse practitioner and a nutritionist in English or Spanish. Control group received the NCI’s “Facing Forward” publication. | No significant differences were seen at 3 or 60 months between the two groups on the Impact of Cancer or treatment and survivor satisfaction scale. Health worry was lower in the intervention group (p = 0.02). | While the intervention did not lead to significant improvements in most patient-reported outcomes, it was associated with decreased health worry. Future interventions should determine the most efficient and effective method for delivering survivorship care plans. |
| 1 | Brothers, 2013 | RCT | 121 survivors of gynecological cancer across 3 providers, mean age: 60 (range: 24–89); 91% white; 6% African-American; 1% Asian; 2% other; 57% rural | Intervention group: Individualized SCP. Control group: no SCP/usual care. | The intervention group was more likely to report receiving educational materials (p=0.019); no differences were noted in satisfaction. | Gynecologic oncology patients providing ratings of health services and satisfaction with care provided equivalent evaluations, regardless if they had/had not received a SCP from the physician. Thus, the need remains for further evaluations of SCPs if they are to be vehicles for improving health service outcomes. |
| 2 | Sprague, 2013 | Interview | 48 BCS ages 35–75 and 10 CCS ages 41–70. | JourneyForward SCP | Most survivors felt SCP was useful, easy to understand and helpful in understanding diagnosis, treatment, follow-up care. | SCP helpful but still needing clarification about PCP and oncologists role in surveillance. |
| 4 | Casillas, 2011 | Survey | 376 survivors, mean age: 28 (range 18–39); 74% white; 54% female. | SCP | Being a minority and not receiving SCP were significantly associated with low confidence in managing survivorship care (p<0.05). | Findings suggest that provision of survivorship care plans for young adult cancer survivors can be used to improve confidence in managing survivorship care, particularly for ethnic minorities. |
| 2 | Jefford, 2011 | Survey and interviews | Ten CCS survivors within a year of completing treatment | SurvivorCare intervention included booklet; DV; question prompt list; SCP; end-of-treatment nurse visit; and 3 follow-up phone calls | CCS felt that the intervention package was useful, relevant and convenient. SCP took 1–1.5 hours to complete. | SCP as a component of SurvivorCare was well received. |
| 4 | Rechis, 2013 | Survey | 2759 post-treatment survivors, mean age: 49 (TS group), 50 (no TS); female: 61% (TS group), 67% (no TS); white: 92% (TS group), 89% (no TS); mean time since diagnosis: 5.8 years (TS group), 6.9 (no TS). In both groups, the majority of participants were BCS. | TS | 34% received TS. Those who didn’t receive TS experienced more emotional concerns (p<0.05). Those who received TS were more likely to be receiving care from an oncologist (p<0.01), report that their providers were meeting their needs during and after treatment (p<0.01); that they received information about possible late effects; and that the information met their needs (p<0.01). | Receipt of a TS was associated with a variety of positive outcomes; however, only approximately one third of survivors received one |
| 4 | Rosales, 2013 | Survey | 118 BCS in the St. Luke’s Mountain States Tumor Institute | SCP prepared in the electronic health record, reviewed during an appointment with a nurse practitioner and social worker, and mailed to the PCP. | Eighty-eight percent of survivors strongly agreed or agreed that they understood their SCP; 86% strongly agreed or agreed to feeling the survivorship visit met their survivorship needs. At 1 month, 80% of participants were still working on wellness goals. Survivor accounts analysis showed revenue covered costs. | Survivorship care at MSTI meets new standards, allows for patient engagement and satisfaction, and improves care coordination. Costs are covered by reimbursement. |
| 4 | Sabatino, 2013 | National Health Interview Survey | 1345 survivors, current age: 20–85+; 40% age <50 at diagnosis; 59% female, 83% white, 61% privately insured, 59% college educated, 20% BCS; 40% diagnosed ≤5 or >10 years prior; 63% had one treatment modality; 89% had no recent treatments; 91% did not participate in clinical trials; 75% were in good health or better. | TS and written instructions | 32% reported receiving TS. Written instructions were associated with reporting recent provider recommendations for breast (p=0.03) and cervical cancer (p=0.007) surveillance. Written instructions were associated with recent mammography use (p=0.05). | Many recently diagnosed cancer survivors did not report receiving treatment summaries and written follow-up instructions. Opportunities exist to examine associations between use of these documents and recommended care and outcomes, and to facilitate their adoption. |
| 4 | Makari-Judson, 2013 | Pre-post practice data audit | Wait times and surgical patient volume in a single medical center | Surgeons, medical oncologists and nurse practitioners in a breast cancer clinic agreed upon guidelines for follow up of BCS, developed a survivorship care program to follow active treatment, and gave survivors SCP following diagnosis beginning in 2009. | Wait times decreased from 43.5 before SCP use to 9 days after SCP use began; surgical patient volume increased from 573 to 650. | SCPs were useful in re-engineering follow-up habits of clinicians, adding value to each visit and gaining acceptance from established patients regarding recommended surveillance. SCPs contributed to reduced wait times and increase in volume of new patients seen by breast surgeons. |
| 2 | Nissen, 2013 | Survey | 203 BCS and 141 CCS, median time since diagnosis: 7.9 years (range, 3.2 – 13.1 years). BCS were younger and had been diagnosed less recently than CCS. Stage of disease and type of treatment differed for BCS and CCS. | TS | After receiving TS, Both BCS and CCS showed significant improvement in accuracy on stage of disease; BCS showed significant improvement in accuracy on morphology, estrogen receptor status, progesterone receptor status, receipt of hormone therapy, and receipt of doxorubicin (p<0.001). | Accuracy improved significantly, but survivor knowledge remained incomplete following TS receipt. |
| 4 | Blinder, 2013 | Survey | 174 BC patients in 20 diverse oncology practices, median age: 58; 84% white; most had stage I cancer (range 0-III). | Patients received treatment plans and summaries (TPSs) as part of the American Society of Clinical Oncology Breast Cancer Registry pilot program of 20 community oncology practices. | Of 157 patients who recalled receiving a TPS, 94% believed that the documents improved survivor-physician communication; 82% believed that they improved communication between physicians; 72% said the documents increased their peace of mind; 1% had less peace of mind. Ninety-seven percent still had their documents; of these, 97% said they were useful and 62% had given or planned to give the documents to another physician. All survivors recommended TPSs to continue to be provided. | Participants in this study expressed high satisfaction with TPSs. Additional research is needed to study the broad-scale implementation of the BCR and to evaluate the impact of routine use of TPSs on the quality of care delivered. Cancer 2013. © 2012 American Cancer Society. |
| 4 | Faul, 2012 | Interviews | 7 oncology providers; 7 CCS, all white, age range: 54–84 | SCP | Survivors perceived reduced duplication of services and reduced worry associated with SCP. Providers noted billing/reimbursement issues and time to develop SCP as potential barriers. | Further investigation of SCPs is warranted regarding utility prior to widespread adoption in follow-up care. |
| 4 | Hill-Kayser, 2013 | Survey | 8690 cancer survivors used the SCP tool. Of these, 298 responded to a 1- month follow-up survey. Respondents 75% female, with a median age of 55. 93% were white, and 45% had breast cancer. | Internet-based SCP. | The majority of respondents (63%) thought that the SCP changed their health care participation, and 80% shared/planned to share it with their health care team. Of those survivors who had done so, 80% reported that it improved communication with their health care providers. Greater than one-half of survey users (54%) reported that they had made or planned to make a lifestyle change in response to the SCP, most commonly dietary modification and increased exercise. | Survivorship care plans are useful vehicles with which to promote lifestyle and behavioral changes, and to assist survivors with communication with health care providers. These findings support recommendations from the Institute of Medicine and the American College of Surgeons Commission on Cancer. |
Survivor-level outcomes
There were three randomized controlled trials (RCT) of SCP influence on survivor outcomes. Grunfeld and colleagues conducted an RCT to determine whether SCP for breast cancer survivors and their PCP improved survivor-reported outcomes up to 12 months after the transition from oncology care to PCP-led follow up care.51 The authors found no benefit from the SCP on any outcomes (e.g., distress, QOL, satisfaction), either proximal to time of transfer to PCP or at 12 months. They posited that the lack of an intervention effect may have been due in part to their sample, as the survivors in their study may have been better adjusted as a result of time of diagnosis (median time from diagnosis was 35 months). Further, breast cancer survivors may be better informed and have better access to supportive care resources than survivors of other cancers. Lack of differences between the intervention and control groups suggest that a standard discharge visit with an oncologist – the control condition – may accomplish many of the goals of SCP.
The RCT conducted by Hershman and colleagues tested an in-person survivorship intervention (including treatment summary and follow-up care plan) following adjuvant breast cancer therapy.72,52 They observed no effect of the intervention on cancer worry, treatment satisfaction, cancer survivor concerns, depression, or the impact of cancer. The authors suggested that null results might be due to survivor-reported outcomes, which do not capture other health benefits or potential long-term improvements in outcomes or quality and coordination of care.
Finally, the RCT conducted by Brothers and colleagues compared outcomes of gynecologic cancer survivors who received standard of care plus an SCP or standard of care only.47 The authors found no significant differences between the intervention and control groups with regard to their satisfaction with care. Brothers and colleagues suggested that results may have been null because survivors who do not receive an SCP do not know that anything is missing from their care; that is, survivors without an SCP do not know what they do not know.
In contrast to the RCT, which found few relationships between SCP and outcomes, nine observational studies in this category described positive outcomes for survivors, including satisfaction with the SCP itself67, 75–77 and satisfaction with care71, 71. SCP use was also associated with survivors’ reporting improved communication with62, 77 and between providers62. Further, SCP were linked to improvements in self-reported63 and objectively measured61, 78 knowledge about cancer, treatment, and follow-up care, and to enhanced peace of mind79, 79 and confidence54 through providing a plan to manage follow-up care. Finally, SCP were also linked to changes in survivors’ health behaviors. Hill-Kayser et al.68, 69 found that more than half of SCP users in their study reported that they had made or planned to make a lifestyle change in response to the SCP (e.g., dietary modification, increased exercise). Another study by Sabatino et al.59 found that written provider instructions about follow-up care associated with use of cancer screening.
Provider-level outcomes
Only one study assessed the influence of SCP on providers.63 Oncology providers saw SCP as augmenting continuity and quality of cancer care, but they also noted concerns about billing and reimbursement for SCP creation and delivery.
Cancer program outcomes
Two studies evaluated outcomes at the cancer program level. Makari-Judson et al.70 developed and implemented a survivorship care program, which included the use of SCP, in their breast cancer clinic. A pre-post evaluation found that patient wait times decreased and patient volume increased after program implementation. The authors attributed the changes to a shift in appointment types. With nurse practitioners leading the survivorship care program and managing the care of survivors who were five years or more post-treatment, medical oncologists were available to manage the follow-up care of survivors who were less than five years post-treatment. Consequently, the need for follow-up care by surgeons was eliminated, increasing the clinic’s capacity for new patients. In another study, by comparing the average cost per SCP visit to the average amount of reimbursement, Rosales et al.58, 80, 81 found that the return on investment of SCP visits was approximately 6%.
Limitations
The strength of evidence for studies in this category was generally low, with the majority of studies using observational designs. Although the observational studies in this category of evidence linked SCP to improved survivor- and cancer program-level outcomes, several methodological considerations limit their interpretation. First, all studies were cross-sectional, limiting their ability to establish causality. Second, most studies relied on survivors’ self-report, so data may be subject to social desirability and/or recall bias. Third, the studies’ reliance on convenience samples may have introduced selection bias. Fourth, generalizability was limited in most cases due to evaluation in non-representative survivor populations. An important strength of the studies was their sample size: most studies in this category had more than 100 participants.
Discussion
This integrative review identified 42 studies of SCP in survivors of adult cancers. Similar to the review conducted by Salz and colleagues (2011), we found that SCP are endorsed, but evidence of improved outcomes associated with SCP is limited, and implementation is not yet widespread. An equal number of studies identified in our review addressed SCP content, dissemination and implementation, and outcomes. Significant gaps in knowledge remain within each of these categories, suggesting several areas for future research. Areas for future research and methodological concerns that it should address are summarized in table 5 and discussed by study category below.
TABLE 5.
RECOMMENDED AREAS FOR FUTURE SCP RESEARCH AND METHODOLOGICAL CONCERNS TO BE ADDRESSED
| Content |
|
|
| 1. When do survivors and providers prefer for SCP to be delivered? |
| 2. How frequently do survivors and providers prefer for SCP to be delivered? |
| 3. Which type of provider most effectively develops SCP? |
| 4. Which type of provider most effectively delivers SCP? |
|
|
| Dissemination and implementation |
|
|
| 1. What determines whether survivors and primary care providers receive and retain SCP? |
| 2. Does a limited-content SCP template minimize resources required for SCP use? |
| 3. Does a limited-content SCP template increase SCP use? |
|
|
| Outcomes |
|
|
| 1. What are the “active ingredients” of effective transitions from treatment to follow-up care? |
| 2. Are survivors who receive SCP more likely than survivors without SCP to get guideline-concordant care? |
| 3. Are survivors who receive SCP less likely than survivors without SCP to receive duplicative services? |
| 4. How confident are providers in managing survivors’ follow-up care? |
| 5. What costs are associated with SCP use. |
| 6. Which patient-, provider-, and cancer program-level variables are most relevant SCP-related outcomes? |
|
|
| Methodological concerns to be addressed |
|
|
| 1. Biases associated with observational studies may be addressed by using RCT. |
| 2. Inability to infer causality may be addressed with longitudinal studies. |
| 3. Limited generalizability may be addressed with more diverse samples of cancer programs, providers, and survivors that reflect the diversity found in practice. |
| 4. Concerns about validity and reliability may be addressed through systematic testing of data collection tools. |
Abbreviations for all tables: ASCO, American Society of Clinical Oncology; BCS, breast cancer survivor; CCS, colorectal cancer survivor; IOM, Institute of Medicine; NCI, National Cancer Institute; PCP, primary care provider; RCT, randomized controlled trial; SCP, survivorship care plan; TS, treatment summary
Content
Many of the studies focusing on the content and delivery process of SCP were derived from focus groups, interviews and surveys. There is little variation across these studies in the preferred content among survivors and PCPs. Less clear are preferences for the timing of delivery, which these studies defined as close to the end of initial cancer treatment. Nurses are frequently identified as ieal for delivering SCP, but whether they are more effective at doing so than other providers has not been empirically tested.
Dissemination and implementation
Dissemination and implementation science will be important in promoting SCP implementation in anticipation of the 2015 Commission on Cancer Standards83. In particular, research is lacking regarding determinants of SCP use at the cancer program level. Cancer care quality improvement organizations plan to evaluate compliance with SCP use requirements at the cancer program level (e.g., whether or not a process for providing SCP has been developed and implemented in the cancer program). As such, understanding determinants of SCP use at the cancer program level may facilitate compliance with SCP use requirements.79, 84 Only one study assessed SCP retention following SCP receipt, and it did not use inferential statistics to identify determinants.16 Understanding SCP receipt and retention and their determinants is particularly important because, if survivors and their PCPs do not receive and retain SCP, then the intent underlying the IOM’s recommendation to use SCP as a tool to foster communication will not be met.80
Several studies reported that barriers to SCP use included insufficient resources such as time, staff, training, templates, and funding15, 44, 48. The American Society of Clinical Oncology Survivorship Care Plan Working Group recently attempted to limit SCP content to critical elements with the goal of minimizing resources required for SCP use (D. Mayer, personal communication). Future research should evaluate whether the revised ASCO template achieves this goal.
Outcomes
The three RCT evaluating the influence of SCP on survivor outcomes found no effect of SCP on distress, satisfaction, or quality of life. Nevertheless, the RCT offer insight into the challenges of conducting SCP research and suggest specific areas for future research. First, control conditions such as a standard discharge visit with an oncologist may accomplish many of the goals of SCP. This suggests that future studies should endeavor to identify the “active ingredients” of effective transitions from treatment to follow-up care.
Second, survivor-reported outcomes are limited in capturing some health benefits or potential long-term improvements in outcomes or quality and coordination of care. Third, survivors in the control condition (i.e., without an SCP) may not recognize that they lack information that may improve their outcomes. Taken together the second and third insights derived from extant RCT suggest that future studies should employ both survivor-reported outcomes and objective measures of outcomes associated with SCP. Potential measures might include whether survivors who receive SCP are more likely than survivors without SCP to get care in accordance with guidelines and less likely to receive duplicative services; PCPs’ confidence in managing follow-up care of cancer survivors; and the cost of SCP use.
Fourth, results from RCT may be null because the influence of timing and frequency of SCP delivery have not yet been fully explored. This is analogous to dose-finding chemotherapy trials – perhaps one “dose” of SCP upon treatment completion does not result in long-lasting beneficial survivor effects, or if delivered too late may not be as beneficial, but repeated doses or earlier timing may be more effective. Empiric work on the optimal timing and frequency of SCP is needed before declaring this to be an ineffective tool for survivorship care.
In contrast to RCT results, several observational studies did find relationships between SCP use and positive survivor outcomes. However, most of these studies evaluated process-based outcomes including survivor knowledge and satisfaction. Significantly more work – perhaps involving key stakeholder interviews – is needed to identify the most relevant outcomes to be measured in studies examining the efficacy of delivering an SCP to a survivor and/or their PCP. As Parry (2013) noted, there is a need to look beyond SCP delivery and examine both proximal (care coordination and communication) and distal (adherence, management, utilization, quality of life) outcomes. In addition to the several topics not addressed in extant research, we found many methodological concerns associated with SCP studies that should be addressed in future research. First, few studies used RCT, which avoid many of the biases associated with observational studies, which were far more common in the SCP literature. Second, all studies were either cross-sectional or pre-post. Longitudinal studies are needed to infer causality. Third, larger, more diverse samples of cancer programs, providers and survivors with characteristics that reflect the diversity found in practice are needed to afford sufficient power for inferential statistics and improve generalizability. Fourth, systematic testing is needed in future studies to promote the reliability and validity of tools to collect data regarding SCP use, content, and outcomes, which are currently lacking.81, 85
The National Cancer Institute issued a program announcement “Examination of Survivorship Care Planning Efficacy and Impact (PA PA-12-274 [R21] and PA-12-275 [R01])” and a number of grants have been awarded. We look forward to the results of those studies. We can then focus on other issues related to transitions in care for cancer survivors82.
Acknowledgments
This program is supported by Health-e-NC, an initiative of the University Cancer Research Fund at the University of North Carolina at Chapel Hill. Dr. Birken’s effort was funded by grant number 5 R25 CA57726 from the National Cancer Institute. We would like to thank Jennifer Walker, Research Librarian, for her assistance in the literature search.
Footnotes
Conflict of Interest Disclosure Statement: The authors have no financial disclosures.
References
- 1.Siegel R, DeSantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62:220–241. doi: 10.3322/caac.21149. [DOI] [PubMed] [Google Scholar]
- 2.Hewitt M, Greenfield S, Stovall E, editors. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, D. C.: THE NATIONAL ACADEMIES PRESS; 2005. [Google Scholar]
- 3.Snyder CF, Frick KD, Kantsiper ME, et al. Prevention, screening, and surveillance care for breast cancer survivors compared with controls: changes from 1998 to 2002. J Clin Oncol. 2009;27:1054–1061. doi: 10.1200/JCO.2008.18.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Snyder CF, Frick KD, Peairs KS, et al. Comparing care for breast cancer survivors to non-cancer controls: a five-year longitudinal study. J Gen Intern Med. 2009;24:469–474. doi: 10.1007/s11606-009-0903-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Voelker R. Cancer care accreditation standards: improve quality and help patients cope. JAMA. 2011;306:1314. doi: 10.1001/jama.2011.1373. [DOI] [PubMed] [Google Scholar]
- 6.Snyder CF, Earle CC, Herbert RJ, Neville BA, Blackford AL, Frick KD. Preventive care for colorectal cancer survivors: a 5-year longitudinal study. J Clin Oncol. 2008;26:1073–1079. doi: 10.1200/JCO.2007.11.9859. [DOI] [PubMed] [Google Scholar]
- 7.Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52:546–553. doi: 10.1111/j.1365-2648.2005.03621.x. [DOI] [PubMed] [Google Scholar]
- 8.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Snyder CF, Frick KD, Herbert RJ, et al. Preventive care in prostate cancer patients: following diagnosis and for five-year survivors. J Cancer Surviv. 2011;5:283–291. doi: 10.1007/s11764-011-0181-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Cancer Institute. Levels of Evidence for Supportive and Palliative Care Studies (PDQ) Available at: http://www.cancer.gov/cancertopics/pdq/levels-evidence-supportive-care/HealthProfessinal/page2. [PubMed]
- 11.Ashing-Giwa K, Tapp C, Brown S, et al. Are survivorship care plans responsive to African-American breast cancer survivors?: voices of survivors and advocates. J Cancer Surviv. 2013 doi: 10.1007/s11764-013-0270-1. [DOI] [PubMed] [Google Scholar]
- 12.Baravelli C, Krishnasamy M, Pezaro C, et al. The views of bowel cancer survivors and health care professionals regarding survivorship care plans and post treatment follow up. J Cancer Surviv. 2009;3:99–108. doi: 10.1007/s11764-009-0086-1. [DOI] [PubMed] [Google Scholar]
- 13.Burg MA, Lopez ED, Dailey A, Keller ME, Prendergast B. The potential of survivorship care plans in primary care follow-up of minority breast cancer patients. J Gen Intern Med. 2009;24(Suppl 2):S467–71. doi: 10.1007/s11606-009-1012-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haq R, Heus L, Baker NA, et al. Designing a multifaceted survivorship care plan to meet the information and communication needs of breast cancer patients and their family physicians: results of a qualitative pilot study. BMC Med Inform Decis Mak. 2013;13 doi: 10.1186/1472-6947-13-76. 76-6947-13-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hewitt ME, Bamundo A, Day R, Harvey C. Perspectives on post-treatment cancer care: qualitative research with survivors, nurses, and physicians. J Clin Oncol. 2007;25:2270–2273. doi: 10.1200/JCO.2006.10.0826. [DOI] [PubMed] [Google Scholar]
- 16.Hill-Kayser CE, Vachani C, Hampshire MK, Jacobs LA, Metz JM. An internet tool for creation of cancer survivorship care plans for survivors and health care providers: design, implementation, use and user satisfaction. J Med Internet Res. 2009;11:e39. doi: 10.2196/jmir.1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jefford M, Lotfi-Jam K, Baravelli C, et al. Development and pilot testing of a nurse-led posttreatment support package for bowel cancer survivors. Cancer Nurs. 2011;34:E1–E10. doi: 10.1097/NCC.0b013e3181f22f02. [DOI] [PubMed] [Google Scholar]
- 18.Kantsiper M, McDonald EL, Geller G, Shockney L, Snyder C, Wolff AC. Transitioning to breast cancer survivorship: perspectives of patients, cancer specialists, and primary care providers. J Gen Intern Med. 2009;24(Suppl 2):S459–66. doi: 10.1007/s11606-009-1000-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Marbach TJ, Griffie J. Patient preferences concerning treatment plans, survivorship care plans, education, and support services. Oncol Nurs Forum. 2011;38:335–342. doi: 10.1188/11.ONF.335-342. [DOI] [PubMed] [Google Scholar]
- 20.Mayer D, Gerstel A, Leak A, Smith S. Patient and Provider Preferences for Survivorship Care Plans. 2012 doi: 10.1200/JOP.2011.000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith SL, Singh-Carlson S, Downie L, Payeur N, Wai ES. Survivors of breast cancer: patient perspectives on survivorship care planning. J Cancer Surviv. 2011;5:337–344. doi: 10.1007/s11764-011-0185-7. [DOI] [PubMed] [Google Scholar]
- 22.Smith SL, Wai ES, Alexander C, Singh-Carlson S. Caring for survivors of breast cancer: Perspective of the primary care physician. Curr Oncol. 2011;18:e218–e226. doi: 10.3747/co.v18i5.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shalom MM, Hahn EE, Casillas J, Ganz PA. Do survivorship care plans make a difference? A primary care provider perspective. J Oncol Pract. 2011;7:314–318. doi: 10.1200/JOP.2010.000208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Blinder VS, Norris VW, Peacock NW, et al. Patient perspectives on breast cancer treatment plan and summary documents in community oncology care : A pilot program. Cancer. 2012 doi: 10.1002/cncr.27856. [DOI] [PubMed] [Google Scholar]
- 25.Smith SL, Wai ES, Alexander C, Singh-Carlson S. Caring for survivors of breast cancer: perspective of the primary care physician. Curr Oncol. 2011;18:e218–26. doi: 10.3747/co.v18i5.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Friedman DR, Dupont AH, Coan AD, Herndon JE, Rowe KL, Abernethy AP. Survivorship care planning needs in diffuse large B-cell lymphoma (DLBCL) J Clin Oncol. 2009;27:e20703. [Google Scholar]
- 27.Stricker CT, Jacobs LA, Panzer SL, Palmer SC. Breast cancer survivorship visits: Presenting concerns and resulting recommendations. J Clin Oncol. 2013;31 [Google Scholar]
- 28.Jefford M, Lotfi-Jam K, Baravelli C, et al. Development and pilot testing of a nurse-led posttreatment support package for bowel cancer survivors. Cancer Nurs. 2011;34:E1–10. doi: 10.1097/NCC.0b013e3181f22f02. [DOI] [PubMed] [Google Scholar]
- 29.Hill-Kayser CE, Vachani C, Hampshire MK, Jacobs LA, Metz JM. An internet tool for creation of cancer survivorship care plans for survivors and health care providers: design, implementation, use and user satisfaction. J Med Internet Res. 2009;11:e39. doi: 10.2196/jmir.1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sprague BL, Dittus KL, Pace CM, et al. Patient satisfaction with breast and colorectal cancer survivorship care plans. Clin J Oncol Nurs. 2013;17:266–272. doi: 10.1188/13.CJON.17-03AP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hahn EE, Ganz PA. Survivorship programs and care plans in practice: variations on a theme. J Oncol Pract. 2011;7:70–75. doi: 10.1200/JOP.2010.000115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Birken SA, Mayer DK, Weiner BJ. Survivorship Care Plans: Prevalence and Barriers to Use. J Cancer Educ. 2013 doi: 10.1007/s13187-013-0469-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Birken S, Deal A, Mayer DK, Weiner B. Prevalence and barriers to survivorship care plan use in United States cancer programs. J Cancer Education. 2014 doi: 10.1007/s13187-014-0628-8. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Campbell BH, Massey BL, Myers KB. Survivorship care plans for patients with head and neck cancer. Arch Otolaryngol Head Neck Surg. 2012;138:1116–1119. doi: 10.1001/jamaoto.2013.683. [DOI] [PubMed] [Google Scholar]
- 35.Chubak J, Pocobelli G, Weiss NS. Tradeoffs between accuracy measures for electronic health care data algorithms. J Clin Epidemiol. 2012;65:343–349.e2. doi: 10.1016/j.jclinepi.2011.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dulko D, Pace CM, Dittus KL, et al. Barriers and facilitators to implementing cancer survivorship care plans. Oncol Nurs Forum. 2013;40:575–580. doi: 10.1188/13.ONF.575-580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Forsythe LP, Parry C, Alfano CM, et al. Gaps in survivorship care plan delivery and potential benefits to survivorship care. J Clin Oncol. 2013;31 [Google Scholar]
- 38.Friedman DR, Coan AD, Smith SK, Herndon JE, II, Abernethy AP. Informational needs assessment of non-Hodgkin lymphoma survivors and their physicians. Am J Hematol. 2010;85:528–532. doi: 10.1002/ajh.21725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Friedman DR, Dupont AH, Coan AD, Herndon JE, Rowe KL, Abernethy AP. Survivorship care planning needs in diffuse large B-cell lymphoma (DLBCL) J Clin Oncol. 2009;27:e20703. [Google Scholar]
- 40.Merport A, Lemon SC, Nyambose J, Prout MN. The use of cancer treatment summaries and care plans among Massachusetts physicians. Support Care Cancer. 2012;20:1579–1583. doi: 10.1007/s00520-012-1458-z. [DOI] [PubMed] [Google Scholar]
- 41.Schootman M, Homan S, Weaver KE, Jeffe DB, Yun S. The health and welfare of rural and urban cancer survivors in missouri. Prev Chronic Dis. 2013;10:E152. doi: 10.5888/pcd10.130052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stricker CT, Jacobs LA, Risendal B, et al. Survivorship care planning after the institute of medicine recommendations: how are we faring? J Cancer Surviv. 2011;5:358–370. doi: 10.1007/s11764-011-0196-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Birken SA, Mayer DK, Weiner BJ. Survivorship Care Plans: Prevalence and Barriers to Use. J Cancer Educ. 2013 doi: 10.1007/s13187-013-0469-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Birken SA, Mayer DK, Weiner BJ. Survivorship care plans: prevalence and barriers to use. J Cancer Educ. 2013;28:290–296. doi: 10.1007/s13187-013-0469-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Merport A, Lemon SC, Nyambose J, Prout MN. The use of cancer treatment summaries and care plans among Massachusetts physicians. Supportive Care Cancer. 2012;20:1579–1583. doi: 10.1007/s00520-012-1458-z. [DOI] [PubMed] [Google Scholar]
- 46.Hewitt ME, Bamundo A, Day R, Harvey C. Perspectives on post-treatment cancer care: Qualitative research with survivors, nurses, and physicians. J Clin Oncol. 2007;25:2270–2273. doi: 10.1200/JCO.2006.10.0826. [DOI] [PubMed] [Google Scholar]
- 47.Chubak J, Tuzzio L, Hsu C, et al. Providing care for cancer survivors in integrated health care delivery systems: practices, challenges, and research opportunities. J Oncol Pract. 2012;8:184–189. doi: 10.1200/JOP.2011.000312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Merport A, Lemon SC, Nyambose J, Prout MN. The use of cancer treatment summaries and care plans among Massachusetts physicians. Support Care Cancer. 2012;20:1579–1583. doi: 10.1007/s00520-012-1458-z. [DOI] [PubMed] [Google Scholar]
- 49.Trochim W, Donnelly JP. The Research Methods Knowledge Base. Mason, OH: Thomson Publishing; 2007. rd ed. [Google Scholar]
- 50.Grunfeld E, Julian JA, Maunsell E, Pond G, Coyle D, Levine MN. Reply to M. Jefford et al and C.T. Stricker et al. J Clin Oncol. 2012;30:1393–1394. [Google Scholar]
- 51.Grunfeld E, Julian JA, Pond G, et al. Evaluating survivorship care plans: results of a randomized, clinical trial of patients with breast cancer. J Clin Oncol. 2011;29:4755–4762. doi: 10.1200/JCO.2011.36.8373. [DOI] [PubMed] [Google Scholar]
- 52.Hershman DL, Greenlee H, Awad D, et al. Randomized controlled trial of a clinic-based survivorship intervention following adjuvant therapy in breast cancer survivors. Breast Cancer Res Treat. 2013;138:795–806. doi: 10.1007/s10549-013-2486-1. [DOI] [PubMed] [Google Scholar]
- 53.Brothers BM, Easley A, Salani R, Andersen BL. Do survivorship care plans impact patients’ evaluations of care? A randomized evaluation with gynecologic oncology patients. Gynecol Oncol. 2013;129:554–558. doi: 10.1016/j.ygyno.2013.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Casillas J, Syrjala KL, Ganz PA, et al. How confident are young adult cancer survivors in managing their survivorship care? A report from the LIVESTRONG Survivorship Center of Excellence Network. J Cancer Surviv. 2011;5:371–381. doi: 10.1007/s11764-011-0199-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jefford M, Aranda S, Gough K, et al. Evaluating a nurse-led survivorship care package (SurvivorCare) for bowel cancer survivors: study protocol for a randomized controlled trial. Trials. 2013;14 doi: 10.1186/1745-6215-14-260. 260-6215-14-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rechis R, Bann C, Nutt S, Squiers L, Rao N. Who is receiving survivorship care plans? Findings from the 2012 Livestrong survey. J Clin Oncol. 2013;31 [Google Scholar]
- 57.Rechis R, Beckjord EB, Nutt S. Potential Benefits of Treatment Summaries for Survivors’ Health and Information Needs: Results From a LIVESTRONG Survey. J Oncol Pract. 2013 doi: 10.1200/JOP.2013.000973. [DOI] [PubMed] [Google Scholar]
- 58.Rosales A, Clifford K, Brown M, et al. Comprehensive survivorship care: A sustainable model with return on investment. Psycho-Oncology. 2013;22:1–2. [Google Scholar]
- 59.Sabatino SA, Thompson TD, Smith JL, et al. Receipt of cancer treatment summaries and follow-up instructions among adult cancer survivors: results from a national survey. J Cancer Surviv. 2013;7:32–43. doi: 10.1007/s11764-012-0242-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Makari-Judson G, Hubbard S, Wrenn T. Use of survivorship care plans to re-engineer breast cancer follow-up. Open Breast Cancer J. 2013;5:23–26. [Google Scholar]
- 61.Nissen MJ, Tsai ML, Blaes AH, Swenson KK, Koering S. Effectiveness of treatment summaries in increasing breast and colorectal cancer survivors’ knowledge about their diagnosis and treatment. J Cancer Surviv. 2013;7:211–218. doi: 10.1007/s11764-012-0261-7. [DOI] [PubMed] [Google Scholar]
- 62.Blinder VS, Norris VW, Peacock NW, et al. Patient perspectives on breast cancer treatment plan and summary documents in community oncology care: A pilot program. Cancer. 2013;119:164–172. doi: 10.1002/cncr.27856. [DOI] [PubMed] [Google Scholar]
- 63.Faul LA, Rivers B, Shibata D, et al. Survivorship care planning in colorectal cancer: feedback from survivors & providers. J Psychosoc Oncol. 2012;30:198–216. doi: 10.1080/07347332.2011.651260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hill-Kayser CE, Vachani CC, Hampshire MK, Di Lullo G, Jacobs LA, Metz JM. Impact of internet-based cancer survivorship care plans on health care and lifestyle behaviors. Cancer. 2013 doi: 10.1002/cncr.28286. [DOI] [PubMed] [Google Scholar]
- 65.Rechis R, Bann C, Nutt S, Squiers L, Rao N. Who is receiving survivorship care plans? Findings from the 2012 Livestrong survey. J Clin Oncol. 2013;31 [Google Scholar]
- 66.Sabatino SA, Thompson TD, Smith JL, et al. Receipt of cancer treatment summaries and follow-up instructions among adult cancer survivors: results from a national survey. J Cancer Surviv. 2013;7:32–43. doi: 10.1007/s11764-012-0242-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jefford M, Aranda S, Gough K, et al. Evaluating a nurse-led survivorship care package (SurvivorCare) for bowel cancer survivors: study protocol for a randomized controlled trial. Trials. 2013;14 doi: 10.1186/1745-6215-14-260. 260-6215-14-260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hill-Kayser C, Vachani C, Hampshire M, Di Lullo GA, Metz JM. Positive impact of internet-based survivorship care plans on healthcare and lifestyle behaviors. Int J Radiat Oncol Biol Phys. 2012;84:S211–S212. [Google Scholar]
- 69.Hill-Kayser C, Vachani C, Hampshire M, Di Lullo GA, Metz JM. Positive impact of internet-based survivorship care plans on healthcare and lifestyle behaviors. Int J Radiat Oncol Biol Phys. 2012;84:S211–S212. [Google Scholar]
- 70.Makari-Judson G, Hubbard S, Wrenn T. Use of survivorship care plans to re-engineer breast cancer follow-up. Open Breast Cancer J. 2013;5:23–26. [Google Scholar]
- 71.Rechis R, Beckjord EB, Nutt S, Reynolds K, Hayes-Lattin BM. Associations between receipt of a treatment summary, emotional concerns, and patterns of care among post-treatment cancer survivors. J Clin Oncol. 2012;30 [Google Scholar]
- 72.Stricker CT, Jacobs LA, Risendal B, et al. Survivorship care planning after the institute of medicine recommendations: how are we faring? J Cancer Surviv. 2011;5:358–370. doi: 10.1007/s11764-011-0196-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Grunfeld E, Julian JA, Pond G, et al. Evaluating survivorship care plans: results of a randomized, clinical trial of patients with breast cancer. J Clin Oncol. 2011;29:4755–4762. doi: 10.1200/JCO.2011.36.8373. [DOI] [PubMed] [Google Scholar]
- 74.Fernandez C, Fraser GAM, Freeman C, et al. Principles and recommendations for the provision of healthcare in canada to adolescent and young adult-aged cancer patients and survivors. J Adolesc Young Adult Oncol. 2011;1:53–59. doi: 10.1089/jayao.2010.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sprague BL, Dittus KL, Pace CM, et al. Patient satisfaction with breast and colorectal cancer survivorship care plans. Clin J Oncol Nurs. 2013;17:266–272. doi: 10.1188/13.CJON.17-03AP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Blinder VS, Norris VW, Peacock NW, et al. Patient perspectives on breast cancer treatment plan and summary documents in community oncology care: A pilot program. Cancer. 2013;119:164–172. doi: 10.1002/cncr.27856. [DOI] [PubMed] [Google Scholar]
- 77.Hill-Kayser CE, Vachani C, Hampshire MK, Metz JM. High level use and satisfaction with internet-based breast cancer survivorship care plans. Breast J. 2012;18:97–99. doi: 10.1111/j.1524-4741.2011.01195.x. [DOI] [PubMed] [Google Scholar]
- 78.Nissen MJ, Tsai ML, Blaes AH, Swenson KK. Breast and colorectal cancer survivors’ knowledge about their diagnosis and treatment. J Cancer Surviv. 2012;6:20–32. doi: 10.1007/s11764-011-0189-3. [DOI] [PubMed] [Google Scholar]
- 79.Faul LA, Shibata D, Townsend I, Jacobsen PB. Improving survivorship care for patients with colorectal cancer. Cancer Control. 2010;17:35–43. doi: 10.1177/107327481001700105. [DOI] [PubMed] [Google Scholar]
- 80.Rosales AR, Byrne D, Burnham C, et al. Comprehensive Survivorship Care With Cost and Revenue Analysis. J Oncol Pract. 2013 doi: 10.1200/JOP.2013.000945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rosales AR, Byrne D, Burnham C, et al. Comprehensive Survivorship Care With Cost and Revenue Analysis. J Oncol Pract. 2013 doi: 10.1200/JOP.2013.000945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Parry C, Kent EE, Forsythe LP, Alfano CM, Rowland JH. Can’t see the forest for the care plan: a call to revisit the context of care planning. J Clin Oncol. 2013;31:2651–2653. doi: 10.1200/JCO.2012.48.4618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Commission on Cancer. Cancer Program STandards 2012: Ensuring Patient-Centered Care. Vol. 1.2. American College of Surgeons; 2012. http://www.facs.org/cancer/coc/programstandards2012.pdf. [Google Scholar]
- 84.Birken SA, Deal AM, Mayer DK, Weiner BJ. Determinants of survivorship care plan use in United States cancer programs. Journal of cancer education : the official journal of the American Association for Cancer Education. 2014 doi: 10.1007/s13187-014-0645-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Birken SA, Deal AM, Mayer DK, Weiner BJ. Following through: The consistency of survivorship care plan use in United States cancer programs. Journal of Cancer Education. 2014 doi: 10.1007/s13187-014-0628-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cancer Co. Cancer Program Standards 2012, Version 1.2.1: Ensuring Patient-Centered Care. American College of Surgeons; 2012. http://www.facs.org/cancer/coc/programstandards2012.pdf. [Google Scholar]


