Abstract
Objective
We studied whether care management is a pragmatic solution for improving population blood pressure (BP) control and addressing BP disparities between Blacks and Whites in routine clinical environments.
Design
Quasi-experimental, observational study.
Setting and Participants
3,964 uncontrolled hypertensive patients receiving primary care within the last year from one of six Baltimore clinics were identified as eligible.
Intervention
Three in-person sessions over three months with registered dietitians and pharmacists who addressed medication titration, patient adherence to healthy behaviors and medication, and disparities-related barriers.
Main Measures
We assessed the population impact of care management using the RE-AIM framework. To evaluate effectiveness in improving BP, we used unadjusted, adjusted, and propensity-score matched differences-in-differences models to compare those who completed all sessions with partial completers and non-participants.
Results
Of all eligible patients, 5% participated in care management. Of 629 patients who entered care management, 245 (39%) completed all three sessions. Those completing all sessions on average reached BP control (mean BP 137/78) and experienced 9 mm Hg systolic blood pressure (P<.001) and 4 mm Hg DBP (P=.004) greater improvement than non-participants; findings did not vary in adjusted or propensity-score matched models. Disparities in systolic and diastolic BP between Blacks and Whites were not detectable at completion.
Conclusions
It may be possible to achieve BP control among both Black and White patients who participate in a few sessions of care management. However, the very limited reach and patient challenges with program completion should raise significant caution with relying on care management alone to improve population BP control and eliminate related disparities.
Keywords: Care Management, Population Health, Hypertension, Primary Care, Quality Improvement, Disparities
Introduction
Despite the availability of efficacious therapy, only half of hypertensive patients in the United States are adequately controlled.1 Nearly 20% of hypertensive patients are unaware of their diagnosis; a third are not on medication; and nearly a third of those on medications have not achieved control.1,2 Primary care providers (PCPs), who are most likely to treat hypertension, recognize these gaps but lack resources to support patients in chronic illness management, which includes outreach, education, coaching, and frequent follow-up.3
Payers are now holding PCPs accountable for population hypertension control through pay-for-performance programs, such as the Physician Quality Reporting System and Accountable Care Organization metrics.4 Blood pressure (BP) control may be an indicator of population health management because hypertension is prevalent but treatable and a risk factor for many diseases; and vulnerable populations are disproportionately affected. Blacks suffer not only from a higher prevalence of hypertension but also poorer control, compared with Whites.5,6 Disadvantaged groups face particular challenges with self-management, behavior change, medication adherence, and health literacy.6
Care management (CM) is a widespread approach for addressing gaps in population management of chronic illnesses, and a model recently reimbursed by the Center for Medicare & Medicaid Services.7 Care managers work with patients between provider visits to improve clinical care, enhance coordination, and encourage appropriate health care utilization.3 CM is associated with improvement in patient-centered outcomes, quality of care, and resource utilization in outpatients with complex needs and several chronic diseases.8,9
However, it is unclear whether CM is a pragmatic strategy for improving population BP control. Further, there are limited data on whether CM can effectively engage patients in chronic disease treatment within routine clinical settings, where providers must care for disadvantaged populations. Many health systems, such as those in Baltimore, where there is a significant Black population and cardiovascular disease contributes to excess Black mortality, urgently require strategies to overcome the gaps in population BP care.10
We conducted a quasi-experimental, observational study to evaluate whether CM could improve population BP control among uncontrolled hypertensive patients, with particular attention to Blacks, in routine clinical settings.
Methods
Setting
Six primary care practices in the Baltimore metropolitan region, staffed by 45 PCPs, implemented the Reducing Disparities and Controlling Hypertension in Primary Care (ReDCHiP) CM program between 2012 and 2015.10,11 These clinics belong to a network of more than 35 clinics across Maryland, sharing an electronic medical record (EMR). Four of the six study sites are located in medically underserved areas.
Participants
Using the EMR, any patient with a diagnosis of hypertension whose most recent BP was uncontrolled (≥140/90 mm Hg) and who had a visit with their PCP within the last year was eligible for participation; no additional exclusion criteria were applied.
Intervention
Described previously,3,11,12 the ReDCHiP CM program selected professionals with content expertise in nutritional and pharmacological therapy and lifestyle counseling (ie, three fulltime equivalent registered dietitians [RDs], and one-half fulltime equivalent pharmacist) to intensify hypertension care provided by PCPs. RDs focused on medication adherence and health behavior change around the DASH diet, weight loss, exercise, and self-management behaviors. Pharmacists accelerated medication titration and reinforced adherence. Content expertise was enhanced with standardized training in cultural competency, led by authors LAC and CAAM, and training in motivational interviewing, led by author AD. Care managers used motivational interviewing techniques to assess and/or address: patients’ knowledge of and adherence to health behaviors for reducing blood pressure; use of self-management practices; and disparities-related barriers to self-management and adherence.
Care managers performed telephone outreach to eligible patients identified through the EMR; or providers referred eligible patients, identified during routine clinic visits, to CM. There was no cost to patients for participation. The CM program included three sessions, four weeks apart, totaling 120 minutes of face-to-face contact time. Care managers saw patients onsite at primary care clinics.
Study Design
The ReDCHiP CM program was evaluated under routine, clinical circumstances, so that study conditions were representative of real-life clinical settings and findings externally valid.13 Clinic staff were responsible for the delivery of the program, and providers continued their routine management of hypertensive patients with the exception of collaborating with CM at their discretion.
As part of this pragmatic approach, we also used a non-randomized strategy to evaluate CM efficacy, specifically by comparing those who completed all three CM sessions (“completers”) to two groups: 1) those who participated in at least one session but did not complete all sessions (“partial completers”); and 2) a 10% random sample of patients who were eligible but did not participate in CM (“non-participants”). To identify non-participants who resembled participants in health care-seeking behavior, we restricted our random sampling to hypertensive non-participants who had at least one clinical encounter (and thus a recorded BP) during the post-intervention time frame.
Outcome Measures
We used the RE-AIM evaluation framework to assess the population health impact of CM.14
Reach. We define the target population as those patients identified by the electronic registry meeting eligibility criteria. We calculated reach as participation rate in at least one CM session among the target population, as well as representativeness of participants’ pre-intervention BP and race compared with the target population.
Efficacy. We investigated BP change between the pre-intervention period (the time of outreach by CM or provider referral) and the post-intervention period (completion of CM) at each clinic. We used the most recent BP recorded in the EMR at the time of CM outreach or at the time of provider referral as the pre-intervention BP. For the random sample of non-participants and partial completers, we performed chart review to identify BPs that coincided within 30 days of the post-intervention period for CM at their respective clinic location. We preferentially used primary care, nephrology, or cardiology clinic visits, and did not use urgent care, inpatient, emergency room, or procedural visit BPs. We were able to identify relevant post-intervention BPs for 90% (346 patients) of partial completers; the other 10% were excluded from the primary analysis.
Adoption refers to the proportion and representativeness of settings that adopt a program. We have previously reported on strategies used to improve adoption.3,11
Implementation. We measured the number of participants who completed all three sessions, as well as mean face-to-face contact time with care managers and duration of program (from first to last session). We analyzed care manager visit documentation to determine adherence to the ReDCHiP core areas of CM.
Due to the recent completion of the ReDCHiP CM program, we did not evaluate maintenance, or sustainability.
Covariates
Covariates included pre-intervention age and BMI, self-reported race and ethnicity (non-Hispanic White, non-Hispanic Black, or others, which included Hispanic participants), sex, clinic location, method of program entry (CM outreach or provider referral), and PCP. Fifteen patients were missing race/ethnicity data and 13 patients were missing pre-intervention BMI; given the low proportion of missing data, these patients were excluded.
Analysis
We built linear regression models for panel data with differences-in-differences (DID) terms to estimate the difference in systolic and diastolic BP change between the intervention group and each comparison group. Specifically, we compared the change between pre-intervention and post-intervention BPs among those who completed all sessions with the change in BP experienced by partial completers and a random sample of non-participants. We analyzed the effectiveness of CM across all hypertensive patients and whether the effectiveness of CM on BP change varied between Whites and Blacks. For the latter, we included an interaction in each of our models between the DID term and race to determine if there was statistical evidence for variation in the effect of CM by race. All models incorporated clustered standard errors for the repeated observations within each patient.
We performed several sensitivity analyses. First, we compared completers with those who only completed one or two sessions, separately. Second, we compared BP change among all participants (regardless of completion) to non-participants. Third, although we report unadjusted DID analyses to improve interpretability, we also estimated BP changes adjusting for pre-intervention BP and previously listed covariates. Fourth, to better control for PCP involvement in care, we performed an adjusted subset analysis comparing completers only to the partial completers referred by their PCP and whose post-intervention follow-up was with the PCP. Fifth, we checked for variability in intervention effectiveness by clinic site, method of patient entry into CM, and PCP, using statistical interaction tests. Sixth, we repeated the DID analysis, on a propensity score-matched sample, using the same covariates from the adjusted model, employing 1:1 nearest neighbor matching without replacement, caliper size 0.1.
This study was approved by the Johns Hopkins University Institutional Review Board.
Results
Care managers identified 3,964 uncontrolled hypertensive patients using the EMR registry (Table 1). They were able to contact 2037 (51%) by phone; 184 (9% of those contacted, 5% of all patients) attended at least one CM session. PCPs referred another 445 patients who entered the program. Of the 629 patients who started the program, 245 (39%) completed all three sessions. Mean pre-intervention BP (147/85) and percentage of Blacks (63%) in the target population were similar to those who participated in CM and completed all sessions.
Table 1. Reach and implementation of ReDChiP Care Management Program.
| Patients identified through registry reporta | Patients contactedb through outreach (% of registry populationc) | Patients in first session due to outreach (% of registry populationc) | Patients in first session due to PCP referral | Total patients attending first session | Patients completing three sessions (% of first session participants) | |
| Clinic A | 721 | 695 (96) | 51 (7) | 124 | 175 | 66 (38) |
| Clinic B | 448 | 187 (42) | 28 (6) | 13 | 41 | 13 (32) |
| Clinic C | 385 | 364 (95) | 34 (9) | 47 | 81 | 35 (43) |
| Clinic D | 505 | 275 (54) | 24 (5) | 84 | 108 | 48 (44) |
| Clinic E | 286 | 173 (60) | 4 (1) | 95 | 99 | 36 (36) |
| Clinic F | 1619 | 343 (21) | 43 (3) | 82 | 125 | 47 (38) |
| Total | 3964 | 2037 (51) | 184 (5) | 445 | 629 | 245 (39) |
| Pre-intervention BPd mean (SD), mm Hg | 147/85 (14/10) | N/A | N/A | N/A | 148/86 (15/12) | 149/86 (14/12) |
| Black (%) | 2497 (63) | N/A | N/A | N/A | 377 (60) | 149 (61) |
BP, blood pressure; SD, standard deviation; N/A, not applicable.
a. Excludes patients whose blood pressures were found to be controlled during chart verification by care managers.
b. Patients were reached to discuss the care management program.
c. Registry refers to those patient identified through the registry report.
d. Mean pre-intervention blood pressure: blood pressure at the time of registry report and/or referral.
In our analytic sample, which excludes patients with missing data and includes a 10% random sample of non-participants, there were no statistically significant differences in pre-intervention BP or BMI or in racial composition between non-participants, partial completers, and completers (Table 2). Sixty percent, or 337 patients, who began the program, completed two sessions, and 40% completed three sessions (Appendix Table summarizing implementation is available from corresponding author). Ninety-five percent of patients received behavior change counseling at every session; over two-thirds received counseling on two or more health topics. Nearly half of patients reported disparities-related barriers to hypertension control, for which patients received counseling. Table 3 describes differences between participants by race. Pre-intervention systolic and diastolic BP varied by race (P<.001 and P=.02, respectively); Blacks had higher BPs compared with Whites. BMI was also higher among Blacks (35.7 kg/m2) compared with other groups (P=.005).
Table 2. Characteristics of analytic sample by participation in care management.
| Non-participantsa, n=330 | Partial-completers, n=332 | Completers, n=229 | Pb | |
| Pre-intervention blood pressure,a mean (SD), mm Hg | ||||
| Systolic | 147 (13.4) | 148 (14.3) | 149 (11.8) | .27 |
| Diastolic | 86 (10.9) | 87 (11.3) | 86 (10.2) | .48 |
| Race, n (%) | .80 | |||
| Non-Hispanic White | 102 (31) | 108 (33) | 70 (31) | |
| Black | 198 (60) | 201 (60) | 137 (59) | |
| Otherc | 30 (9) | 23 (7) | 22 (10) | |
| Age, mean (SD), years | 55 (12.9) | 55 (14.2) | 58 (12.6) | .01 |
| Female, n (%) | 185 (56) | 193 (58) | 140 (61) | .52 |
| BMI, mean (SD), kg/m2 | 34.4 (9.2) | 35.0 (7.8) | 34.8 (9.5) | .67 |
| Clinic location, n (%) | .51 | |||
| A | 67 (20) | 95 (29) | 63 (28) | |
| B | 30 (9) | 24 (7) | 13 (6) | |
| C | 40 (12) | 39 (12) | 35 (15) | |
| D | 46 (14) | 50 (15) | 44 (19) | |
| E | 26 (8) | 63 (19) | 36 (16) | |
| F | 121 (37) | 61 (18) | 38 (17) | |
| Program entry, n (%) | .003 | |||
| Enrolled through outreach | N/A | 60 (18) | 64 (28) | |
| Referred by provider | N/A | 272 (82) | 165 (72) |
BMI, body mass index; SD, standard deviation.
a. Non-participants refers to the 10% random sample of non-participants.
b. P from chi-square test for difference in proportions and F-test (ANOVA) for difference in means where appropriate.
c. 29 Hispanics, 19 Asians, 2 American Indians, 1 Pacific Islander, and 24 mixed race persons.
Table 3. Characteristics of analytic sample by race.
| Non-Hispanic White, n=280 | Black, n=536 | Othera, n=75 | Pb | |
| Pre-intervention blood pressure, mean (SD), mm Hg | ||||
| Systolic | 147 (14.4) | 150 (15.3) | 145 (12.8) | <.001 |
| Diastolic | 86 (11.9) | 88 (12.3) | 85 (11.2) | .02 |
| Care management participation, n (%) | .80 | |||
| Non-participantsc | 102 (36) | 198 (37) | 30 (40) | |
| Partial completers | 108 (39) | 201 (38) | 23 (31) | |
| Completers | 70 (25) | 137 (26) | 22 (29) | |
| Age, mean (SD), years | 57 (13.5) | 58 (13.6) | 54 (13.8) | .06 |
| Female, n (%) | 157 (56) | 322 (60) | 39 (52) | .30 |
| BMI, mean (SD) | 34.2 (8.9) | 35.7 (8.4) | 31.9 (6.7) | .005 |
| Clinic location, n (%) | <.001 | |||
| A | 5 (2) | 210 (39) | 10 (13) | |
| B | 18 (6) | 31 (6) | 18 (24) | |
| C | 73 (26) | 33 (6) | 8 (11) | |
| D | 25 (9) | 111 (21) | 4 (5) | |
| E | 78 (28) | 43 (8) | 4 (5) | |
| F | 81 (29) | 108 (20) | 31 (41) | |
| Program entry, n (%) | .93 | |||
| Enrolled through outreach | 41 (23) | 73 (22) | 10 (22) | |
| Referred by provider | 137 (77) | 265 (78) | 35 (78) | |
| Total time in care Managementd, mean (SD), mins | 94 (11.4) | 106 (10.9) | 96 (12.1) | <.001 |
| Duration between first and last sessione, mean (SD), days | 65 (11.9) | 79 (11.1) | 69 (12.2) | <.001 |
BMI, body mass index; SD, standard deviation
a. 29 Hispanic, 19 Asian, 2 American Indian, 1 Pacific Islander, and 24 mixed race persons.
b. P from chi-square test for difference in proportions and F-test (ANOVA) for difference in means where appropriate.
c. Non-participants refers to the 10% random sample of non-participants.
d. Only includes participants in care management (partial completers and completers).
e. Only includes those who participated in at least two sessions.
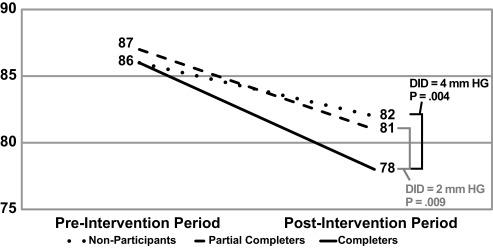
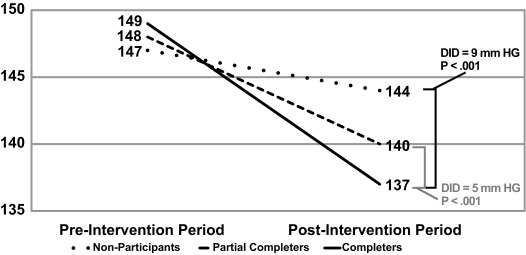
Figures 1 and 2 show the change in mean systolic BP (SBP) and diastolic BP (DBP) by level of participation in CM. BP declined between pre- and post-intervention. Completers obtained BP control at post-intervention (mean BP 137/78 mm Hg) and experienced the greatest BP improvement, namely a 9 mm Hg SBP (P<.001) and 4 mm Hg DBP (P=.004) greater improvement compared with non-participants. Completers demonstrated incremental benefit over partial completers: 5 mm Hg SBP (P<.001) and 2 mm Hg DBP (P=.009) greater improvement between pre- and post-intervention.
Figure 1. Blood pressure change over time by participation in care management with differences-in-differences to assess impact of care management - systolic blood pressure.
NOTE: Differences-in-differences (DID) provides a statistical test to determine whether the treatment condition (participation in all care management sessions) modified the time trend in blood pressure change between pre-intervention and post-intervention compared to non-participants and partial completer.
Figure 2. Blood pressure change over time by participation in care management with differences-in-differences to assess impact of care management - diastolic blood pressure.
NOTE: Differences-in-differences (DID) provides a statistical test to determine whether the treatment condition (participation in all care management sessions) modified the time trend in blood pressure change between pre-intervention and post-intervention compared to non-participants and partial completer.
Both White and Black completers on average reached BP control (Table 4). Black completers saw a larger drop in BP than White completers; therefore, disparities in pre-intervention systolic and diastolic BP between Blacks and Whites were no longer detected at post-intervention among CM completers (P=.19 and P=.42, respectively). However, after accounting for BP changes seen in their non-participant racial counterparts using DID analysis, the effectiveness of the intervention did not vary by race (P=.39 and P=.13 for interaction between race and SBP DID and DBP DID, respectively).
Table 4. Blood pressure change (mm Hg) over time by level of participation in care management with differences-in-differences to assess impact of care management, stratified by race.
| Pre-Intervention Blood Pressure, mm Hg | Post-Intervention Blood Pressure, mm Hg | DIDa Systolic Blood Pressure, mm Hg | DIDa Diastolic Blood Pressure, mm Hg | |
| Non-Hispanic White Patientsb | ||||
| Non-participants | 145/84 | 143/81 | Ref | Ref |
| vs | ||||
| Completers | 148/86 | 136/78 | 10 (P=.001)c | 5 (P=.009)c |
| Partial completers | 147/86 | 139/80 | Ref | Ref |
| vs | ||||
| Completers | 148/86 | 136/78 | 4 (P=.01)d | 2 (P=.02) |
| Black Patientsb | ||||
| Non-participants | 148/88 | 145/84 | Ref | Ref |
| vs | ||||
| Completers | 150/86 | 137/79 | 10 (P=.008)c | 3 (P=.01)c |
| Partial completers | 150/88 | 142/83 | Ref | Ref |
| vs | ||||
| Completers | 150/86 | 137/79 | 5 (P=.01)d | 2 (P=.02)d |
a. Differences-in-differences (DID): provides a statistical test to determine whether the treatment condition (participation in all care management sessions) modified the time trend in blood pressure change between pre-intervention and post-intervention compared with non-participants and partial completers.
b. As our primary interest was to investigate differences between non-Hispanic Whites and Black patients and with the small sample size and heterogonous group of “Others,” we restricted analysis to these two groups.
c. Tests of interaction between DID terms and race: P=.39 (SBP), P=.13 (DBP), based on likelihood ratio test from unadjusted time series regression model.
d. Tests of interaction between DID terms and race: P=.87 (SBP), P=.51 (DBP), based on likelihood ratio test from unadjusted time series regression model.
Interpretation of our main findings did not change with sensitivity analyses (Appendix Table illustrating sensitivity analyses is available from corresponding author). Patients participating in a greater number of sessions experienced greater benefit. Effectiveness did not vary by clinic site, PCP, or method of program entry.
Discussion
In our study, CM appeared to improve BP control and help mitigate disparities in BP control between participating White and Black patients. Care managers delivered health behavior change counseling to nearly every patient, and on two or more topics to over two-thirds of patients, at each session; 50% of patients received counseling about disparities-related barriers to treatment. However, the poor reach of CM and suboptimal rates of program completion may limit the population health impact of CM.
Patients completing the ReDCHiP CM program experienced a 9 mm Hg SBP and 4 mm Hg DBP greater improvement than non-participants, similar to estimates from meta-analyses evaluating other team-based interventions for hypertension care in randomized settings that involved assigning some patient care responsibilities to someone other than the patient’s physician.15-17 However, there has been little, if any, prior evidence confirming similar effectiveness in a pragmatic, routine clinical care setting.
The ReDCHiP CM program appeared equally effective among Blacks and Whites, allowing both Black and White patients completing the program on average to reach BP control. Although pharmacist-led interventions focusing on aggressive medication titration may be one of the most effective team-based models for BP management, this approach alone has been insufficient in addressing the disparities-related barriers to adherence often encountered by Blacks and other disadvantaged populations.18 Behavior change counseling and strategies that address disparities-related barriers in the ReDCHiP program may have contributed to its effectiveness among Blacks. Encouraging BP self-monitoring,19 providing tailored health education,20 and engaging in patient-centered approaches that uncover disparities-related barriers to adherence21 all improve BP control and reduce disparities in Black populations. Further, by incorporating RDs, the ReDCHiP CM model utilized only half an hour of pharmacist time per patient, making it a more viable model in health systems where pharmacists are scarce.
The primary limitations of CM as a population health intervention may be poor program completion and reach. Only 40% of patients completed all three ReDCHiP CM sessions, despite being less time-intensive than most programs in randomized trials.15-17 With a 20% to 40% patient no-show rate to PCP appointments,22 our completion rates for three appointments in three months may be expected. Efficacy trials in which patients received CM at least monthly have shown more BP improvement than those in which patients received CM less frequently.17 None, however, have directly compared care frequency on BP improvement. Our results suggest that CM visits every 6 to 8 weeks may be more feasible and still achieve the same benefits as monthly sessions.17 Even so, those who partially completed the program still experienced BP improvement; incremental benefit was seen with additional participation. Notably, program completion was not associated with race, severity of pre-intervention BP, BMI, PCP referral, PCP, or clinic site. In exploratory analysis, there were no differences in the proportion of patients reporting disparities-related challenges between partial completers and completers.
CM reach was also poor in the target population. We are unable to compare our estimates of reach with other hypertension interventions. There is limited literature on the reach of chronic disease interventions; clinical trials often employ strict inclusion criteria excluding patients most likely to require intervention in routine clinical settings and enumerating the target population can be challenging.14 The low estimate of reach in our study may be an artifact of an inflated denominator from registry data; patients in the registry may have switched their care to a new provider or health system. Physician referral was the more successful method of engagement in our program, potentially because PCPs engaged active patients on the physician’s panel. Often, participants in health interventions are those who need them the least;23 however, participants in ReDCHiP were representative of the target population based on characteristics available to us.
Care managers were unable to contact half of eligible patients, similar to other health systems using automated outreach.22 CM for complex disease management that is integrated with primary care has been shown to be most effective;8 however, program completion and/or reach may be improved if CM could be integrated within the daily routine of patients (at faith organizations, employment sites).24 Additional intervention components for high-risk and frail patients (home visits, community health workers) may improve reach and completion.8 Routinely gathering data on the reach of population health interventions, such as CM, will be essential for improving their population benefit.
Findings from our study must be interpreted in light of its limitations. Because this is a real world study, we implemented CM at clinic sites in the order of clinical urgency and preparedness for adoption; in lieu of randomization, we used a quasi-experimental analytic strategy employing non-participants as a control group. To counter the limitation that non-participants could be a self-selected group of non-adherent patients and to reduce observer bias, we also used partial completers as a second comparison group, who may be closer in health-seeking habits to completers than non-participants. Further, we used propensity score matching to statistically correct imbalance between control groups and completers, with no change in our findings. Although our comorbidity data are limited, pre-intervention BP is most likely to predict subsequent BP, which we included in our adjusted and propensity score models. PCPs may affect the success of CM; therefore, we controlled for and checked for variation in CM effectiveness by PCP and whether PCPs referred patients to CM, and also performed subset analysis including only partial completers who were both seen by their PCP prior to CM and again within the post-intervention period. CM reach may vary in other populations; however, we oversampled clinic sites caring for underserved and Black populations, and included only uncontrolled patients, the likely target of CM hypertension interventions. Geocoding and additional social determinants of health data may help explain barriers to reach in future studies. We extracted BPs from routine care visits for those who did not attend CM sessions; clinical staff at all six clinics received the same training in standardized BP measurement as care managers prior to implementation of CM, likely reducing measurement bias.11 Our follow-up period from session one was approximately three months; mean duration of follow-up for other studies has been closer to six months.17 However, follow-up from the time of CM outreach was on average greater than six months.
Summary and Conclusions
It may be possible to achieve BP control and reduce related disparities among previously uncontrolled, hypertensive Black and White patients after participating in a few CM sessions, potentially by coupling aggressive medication titration with motivational interviewing and problem solving around both health behaviors and disparities-related barriers to medication and lifestyle adherence. However, our study also highlights the urgency of considering program reach and completion in balance with effectiveness before relying on CM to address population chronic illness care in the pragmatic setting. The very limited reach, given the high population prevalence of uncontrolled hypertension, and patient challenges with program completion should raise caution with expecting CM alone to improve population BP control and reduce or eliminate related racial disparities in blood pressure control. Future research and innovation that may help improve the impact of CM include: more robust infrastructure for tracking and following vulnerable patients who do not seek regular care; new designs for delivering disease management and care coordination services that reach a broader population; and patient-centered strategies that keep participants engaged until program completion.
Acknowledgments
We are thankful to the care managers who provided care to patients in the ReDCHiP Care Management project: Whitney Franz, Emily Brown, Kara Taylor, Martin Bishop, Patricia Ross, Jessica Merrey, Leena Deshpande, Alona Williams, Ted Grabarczyk, and Sheeva Chopra.
This work was supported by grants from the National Heart, Lung and Blood Institute (P50HL0105187, K24HL083113, and 5T32HL007180-38), and by the Johns Hopkins Center to Eliminate Cardiovascular Health Disparities.
References
- 1.Yoon SSFC, Carroll MD. Hypertension prevalence and control among adults: United States, 2011–2014. NCHS data brief, no 220. Hyattsville, MD: National Center for Health Statistics; 2015. [PubMed] [Google Scholar]
- 2.Gu Q, Burt VL, Dillon CF, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health And Nutrition Examination Survey, 2001 to 2010. Circulation. 2012;126(17):2105-2114. 10.1161/CIRCULATIONAHA.112.096156 [DOI] [PubMed] [Google Scholar]
- 3.Hussain T, Allen A, Halbert J, Anderson CA, Boonyasai RT, Cooper LA. Provider perspectives on essential functions for care management in the collaborative treatment of hypertension: the P.A.R.T.N.E.R. framework. J Gen Intern Med. 2015;30(4):454-461. 10.1007/s11606-014-3130-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. .Center for Medicare and Medicaid Services Quality measures and performance standards. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Quality_Measures_Standards.html. Accessed Januar 21 2016.
- 5.Giles T, Aranda JM Jr, Suh DC, et al. Ethnic/racial variations in blood pressure awareness, treatment, and control. J Clin Hypertens (Greenwich). 2007;9(5):345-354. 10.1111/j.1524-6175.2007.06432.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong MD, Shapiro MF, Boscardin WJ, Ettner SL. Contribution of major diseases to disparities in mortality. N Engl J Med. 2002;347(20):1585-1592. 10.1056/NEJMsa012979 [DOI] [PubMed] [Google Scholar]
- 7. .Chronic Care Management Services https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/ChronicCareManagement.pdf. Accessed January 21, 2016.
- 8.Effectiveness of Outpatient Case Management for Adults With Medical Illness and Complex Care Needs Comparative Effectiveness Review Summary Guides for Clinicians. Rockville, MD: AHRQ; 2007. [PubMed] [Google Scholar]
- 9. .Agency for Healthcare Research and Quality Section 8: The Care Management Evidence Base. Rockville, MD. 2014. http://www.ahrq.gov/professionals/systems/long-term-care/resources/hcbs/medicaidmgmt/medicaidmgmt8.html. Accessed January 20, 2016.
- 10. .Baltimore City Health Department Cardiovascular Disease and the Health Disparities Initiative. http://www.baltimorehealth.org/cardiovascular.html. Accessed January 21 2016.
- 11.Cooper LA, Marsteller JA, Noronha GJ, et al. A multi-level system quality improvement intervention to reduce racial disparities in hypertension care and control: study protocol. Implement Sci. 2013;8(1):60. 10.1186/1748-5908-8-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cooper LA, Boulware LE, Miller ER III, et al. Creating a transdisciplinary research center to reduce cardiovascular health disparities in Baltimore, Maryland: lessons learned. Am J Public Health. 2013;103(11):e26-e38. 10.2105/AJPH.2013.301297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. .Zwarenstein M, Treweek S, Gagnier JJ, et al. ; CONSORT group ; Pragmatic Trials in Healthcare (Practihc) group. Improving the reporting of pragmatic trials: an extension of the CONSORT statement. BMJ. 2008;337(nov11 2):a2390. http://dx.doi.org/ 10.1136/bmj.a2390. PMID:19001484. [DOI] [PMC free article] [PubMed]
- 14.Glasgow RE, McKay HG, Piette JD, Reynolds KD. The RE-AIM framework for evaluating interventions: what can it tell us about approaches to chronic illness management? Patient Educ Couns. 2001;44(2):119-127. 10.1016/S0738-3991(00)00186-5 [DOI] [PubMed] [Google Scholar]
- 15.Walsh JM, McDonald KM, Shojania KG, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006;44(7):646-657. 10.1097/01.mlr.0000220260.30768.32 [DOI] [PubMed] [Google Scholar]
- 16.Carter BL, Rogers M, Daly J, Zheng S, James PA. The potency of team-based care interventions for hypertension: a meta-analysis. Arch Intern Med. 2009;169(19):1748-1755. 10.1001/archinternmed.2009.316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Santschi V, Chiolero A, Colosimo AL, et al. Improving blood pressure control through pharmacist interventions: a meta-analysis of randomized controlled trials. J Am Heart Assoc. 2014;3(2):e000718. 10.1161/JAHA.113.000718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mueller M, Purnell TS, Mensah GA, Cooper LA. Reducing racial and ethnic disparities in hypertension prevention and control: what will it take to translate research into practice and policy? Am J Hypertens. 2015;28(6):699-716. 10.1093/ajh/hpu233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bosworth HB, Olsen MK, Grubber JM, Powers BJ, Oddone EZ. Racial differences in two self-management hypertension interventions. Am J Med. 2011;124(5):468.e1-468.e8. 10.1016/j.amjmed.2010.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jackson GL, Oddone EZ, Olsen MK, et al. Racial differences in the effect of a telephone-delivered hypertension disease management program. J Gen Intern Med. 2012;27(12):1682-1689. 10.1007/s11606-012-2138-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cooper LA, Roter DL, Carson KA, et al. A randomized trial to improve patient-centered care and hypertension control in underserved primary care patients. J Gen Intern Med. 2011;26(11):1297-1304. 10.1007/s11606-011-1794-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kaplan-Lewis E, Percac-Lima S. No-show to primary care appointments: why patients do not come. J Prim Care Community Health. 2013;4(4):251-255. 10.1177/2150131913498513 [DOI] [PubMed] [Google Scholar]
- 23.Bull SS, Gillette C, Glasgow RE, Estabrooks P. Work site health promotion research: to what extent can we generalize the results and what is needed to translate research to practice? Health Educ Behav. 2003;30(5):537-549. 10.1177/1090198103254340 [DOI] [PubMed] [Google Scholar]
- 24.Kaspin LC, Gorman KM, Miller RM. Systematic review of employer-sponsored wellness strategies and their economic and health-related outcomes. Popul Health Manag. 2013;16(1):14-21. 10.1089/pop.2012.0006 [DOI] [PubMed] [Google Scholar]