Abstract
Objective
Culturally relevant recruitment strategies may be an important approach for recruiting ethnic minorities for interventions. Previous research has examined associations between recruitment strategies and enrollment of African Americans (AA), but has not explored more deeply the role of incorporating sociocultural values into recruitment strategies. Our current study explores whether sociocultural recruitment mediums were associated with demographics, interest and enrollment in a weight-loss intervention.
Method
Sociocultural mediums included community partnerships, culturally relevant ads, sociocultural events, or word-of-mouth. Non-sociocultural mediums included community/school events that did not specifically target AAs. Analyses examined whether demographics of enrolled families differed by recruitment strategy and if recruitment strategy predicted scheduling a baseline visit, enrolling in a run-in phase, and enrolling in the intervention program.
Results
Families recruited from culturally relevant ads, sociocultural events, or word-of-mouth were 1.96 times more likely to schedule a baseline visit (OR=1.96, 95% CI=1.05, 3.68) than families recruited from non-sociocultural mediums. No differences were found for sociocultural mediums on enrolling in the run-in phase or the intervention. However, among enrolled families, those recruited from sociocultural mediums were less likely to be employed (X2 [1, N=142] =5.53, P<.05) and more likely to have lower income (X2 [1, N=142] =13.57, P<.05).
Conclusion
Sociocultural mediums were associated with scheduling a baseline visit, but not enrollment. They were, however, effective in recruiting a more generalizable sample among enrolled participants based on demographic characteristics. Integrating sociocultural values into recruitment methods may be a valuable strategy for increasing interest in participation among underrepresented AA families.
Keywords: Recruitment, Sociocultural Values, Weight-loss Intervention, African Americans
Introduction
Almost 40% of African American adolescents and over 75% of African American adults are classified as overweight or obese nationally;1 thus, developing effective health promotion programs for underserved minorities has become a national priority. However, recruitment of minorities into health promotion interventions remains challenging due to significant barriers including competing demands on time,2 inconvenient locations, lack of transportation,3 and caution of participation in novel intervention strategies given historical treatment of African Americans in research.4-6
Lower recruitment and enrollment rates in health promotion trials among African Americans may, in part, result from the lack of integrating sociocultural values into recruitment strategies.7, 8 Consideration of sociocultural values provides understanding of social, environmental and historical contexts experienced by a group9,10 and can be used to identify recruitment mediums that are more culturally relevant. Sociocultural values identified as important for African Americans include: religiosity/spirituality, collectivism or family, and a connection with history or ancestors.9,10 Selecting recruitment mediums that align with these values, such as church-based events or family referrals, may enhance recruitment of minorities into interventions. Collaborations with organizations that serve the target population or individuals who are respected within the target population may be another sociocultural medium for recruitment.7,10-12 Examples of community partnerships used previously include the use of community advisory boards, community liaisons, and collaboration with local organizations such as churches and clinics.6,11,13,14 In addition to providing a better understanding of important sociocultural values, community partnerships increase participant trust and ownership.7,11,12 Previous research has primarily focused on examining associations between recruitment strategies and enrollment rates in health promotion programs13-15 and understanding the use of faith-based and community partnerships in recruitment.7,11-13 Results suggest that recruitment medium may be associated with enrollment rates and recruitment yield, with community-based sources and partnerships being most effective.13 Although past research has examined the success of different types of recruitment strategies, direct comparisons between sociocultural and non-sociocultural recruitment mediums have not been examined. Previous studies have not examined outcomes across the recruitment process such as scheduling a baseline visit (eg, screening) and enrollment into a run-in phase prior to participation. Our study expands on past research by comparing sociocultural and non-sociocultural recruitment mediums on recruitment and enrollment outcomes in a family-based weight-loss program16,17 to inform more effective recruitment methods for including underrepresented minorities in research.
Method
Study Design
Our study is a secondary analysis of recruitment data available for a randomized controlled trial examining the efficacy of a culturally tailored, family-based plus motivational weight-loss program among African American adolescents and their parents.16,17 The study aimed to examine potential relationships between the use of culturally relevant recruitment strategies and participant interest, enrollment and generalizability to the African American community. Specifically, we examined whether recruitment strategies channeled through sociocultural mediums had a greater effect on: 1) scheduling a baseline visit (eg, interest); 2) enrolling in a run-in phase (to assess barriers to participation and interest); and 3) enrolling in the intervention program. It was hypothesized that families recruited through sociocultural mediums and community partnerships would be more likely to engage at each phase of the enrollment process (baseline screening visit, enrollment to run-in, and enrollment to the intervention) compared with families recruited through more general methods. We also evaluated whether there were demographic differences between families recruited from sociocultural mediums compared with non-sociocultural mediums among families who ultimately enrolled in the intervention program. Results from our study will inform the utility of using sociocultural mediums, community partnerships, or more general recruitment strategies for engaging African Americans in health promotion trials.
Recruitment Procedure
Recruitment for the weight-loss trial was carried out by research staff who received training in recruitment strategies and cultural competency. For each event, recruitment team members set up tables with brochures and posters and approached families to provide information about the project. Interested families were given additional information, screened for eligibility, and offered a baseline visit appointment by phone. At the baseline visit, if eligibility criteria were met, families were given the opportunity to provide consent and enroll in the run-in phase. The two-week run-in phase allowed participants to learn more about the intervention and participant expectations and to complete baseline measures.15 This orientation allowed participants who experienced barriers to participation to drop out before enrolling in the intervention program. The purpose of the run-in phase was to maximize intervention enrollment of families with few barriers who are motivated to complete the 16-week intervention, a 1-year project commitment overall.18-20 After completing the two-week run-in phase, remaining families were enrolled into the intervention program.
Participants
Our study focused on recruitment efforts occurring between February 2012 and June 2015. Families were considered eligible if: 1) there was an African American adolescent aged 11-16 years; 2) the adolescent was overweight or obese; 3) a parent or caregiver who lived in the household was willing to participate; 4) the family had Internet access; and 5) the family lived within a 60-mile radius of our office. Exclusion criteria included having a medical condition that could interfere with physical activity or dietary behaviors, participation in another weight-loss program, or taking medication that could affect weight loss. A total of 145 families have been enrolled in the intervention thus far. All procedures were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all participants included in the study.
Classification of Recruitment Strategies
Recruitment strategies were classified based on whether they were channeled through mediums that included sociocultural values and are described below and presented in Table 1.9,10
Table 1. Recruitment strategies.
| Medium | Strategy | Definition | Examples |
| Sociocultural | Community partners | Partnerships with community organizations that serve African American populations | Parks and Recreation Center, Boys and Girls Club, Blue Choice, pediatric offices |
| Sociocultural | Culturally relevant ads | Print and radio ads placed in sociocultural mediums targeting African Americans | African American printed publications and hip hop and gospel music radio stations |
| Sociocultural | Sociocultural events | One-time events that targeted sociocultural values such as religiosity, collectivism or family, and connection with history or ancestors that were not identified through community partners | Black History Month events, events at African American churches |
| Sociocultural | Word-of-mouth | Referrals from past participants or friends and family members familiar with the program | Referrals from previous participants |
| Non-sociocultural | General community events | One-time family oriented events that targeted the general population | Back-to-school events, festivals, charity walks |
| Non-sociocultural | School events | Events at local middle schools | Presentations made to classes, health fairs, career fairs |
Sociocultural Mediums
Recruitment strategies channeled through sociocultural mediums were those that incorporated key sociocultural values of African Americans including religiosity, collectivism or family, and a connection with history or ancestors.9,10 Additionally, ongoing community partnerships with local organizations that held these sociocultural values and served the African Americans community assisted in recruiting participants.
Community Partnerships
Ongoing partnerships were established with several community organizations that primarily served African American communities and held sociocultural values consistent with this target group. For example, Parks and Recreation held events related to Black History month, which targeted the cultural value of connections with history and ancestors.
Culturally Relevant Ads
Advertisements were placed in sociocultural mediums that targeted the African American community. Print ads were placed in a local African American newspaper, and radio advertisements were aired at three separate time points on stations targeting African Americans communities. These media outlets addressed important sociocultural values such as religiosity and a connection with history and ancestors.
Sociocultural Community Events
Sociocultural community events included community events that incorporated African American sociocultural values. Some examples of sociocultural events that included religiosity values were health fairs at local African American churches, church events, and gospel choir performances. Family-focused events included community festivals in African American neighborhoods. Many events promoted connection with history and ancestors, such as Black History parades or events and hip hop festivals.
Word-of-Mouth
Several families were referred to the program through friends and family members who had already participated in the FIT program or learned about the program through community recruitment events. This recruitment strategy is channeled through the sociocultural values of communalism and connection with family or ancestors.
Non-sociocultural Mediums
Recruitment strategies that were channeled through non-sociocultural mediums were those that targeted a general audience, did not address sociocultural values of African Americans, and were not identified through community partnerships.
General Community Events
The recruitment team attended general community events targeting families of all racial backgrounds. Examples include back-to-school school supplies giveaways, annual community festivals, community job fairs, and charity walks or events. Attendees at these events were of all racial backgrounds, and the primary focus of these events or sponsoring organizations was on general populations not tailored to cultural values specific to African American populations.
School Events
The recruitment team attended career days and health fairs at local middle schools, offering health screenings and flyers about the study. Recruitment staff members also presented information about the study during classes, and school nurses sent information home to parents. The focus of information presented was on health promotion and prevention of chronic diseases such as hypertension and diabetes, and did not target African Americans populations or specific sociocultural values.
Measures
Recruitment and Enrollment Outcomes
Recruitment outcomes for the project included scheduling a baseline visit, enrollment in the run-in phase, and enrollment in the intervention program. All outcomes were coded dichotomously for the data analyses.
Demographic Characteristics
Child and caregiver sex and age were provided during the baseline visit. Families who enrolled in the intervention provided additional demographic and health information including information on marital status, employment status, education level, annual household income, and whether or not the caregiver had ever been diagnosed with cardiovascular disease, hypertension, or type 2 diabetes.
Anthropometric Data
Height (cm), weight (kg), and waist circumference (cm) were collected by trained measurement staff for participants who enrolled in the intervention. Anthropometric measurements were collected twice and averaged for increased accuracy. Body mass index (BMI) scores were calculated and standardized for age and sex using objective height and weight data.
Statistical Analysis
Each recruitment event was coded based on type of recruitment strategy and whether they were channeled through sociocultural mediums. Sociocultural mediums included two broad categories: community partnerships and culturally relevant ads, sociocultural events, or word-of-mouth. These two categories were used to allow for comparisons between community partnerships and sociocultural mediums that were not identified through partnerships to clarify if there was an added benefit to working with community partners. Non-sociocultural mediums included general community events and school events. Logistic regression was used to examine whether recruitment strategies channeled through sociocultural mediums (community partners compared with non-sociocultural mediums and culturally relevant ads, sociocultural events, or word-of-mouth compared with non-sociocultural mediums) predicted: 1) scheduling a baseline visit; 2) enrolling in the run-in phase; and 3) enrolling in the intervention program for one year. Descriptive statistics on demographic characteristics and anthropometric measurements were calculated for families who enrolled in the intervention based on recruitment strategy. Chi-square and t-tests were used to examine differences in demographic characteristics of enrolled families recruited from sociocultural mediums compared to non-sociocultural mediums.
Results
Initial Interest in Program
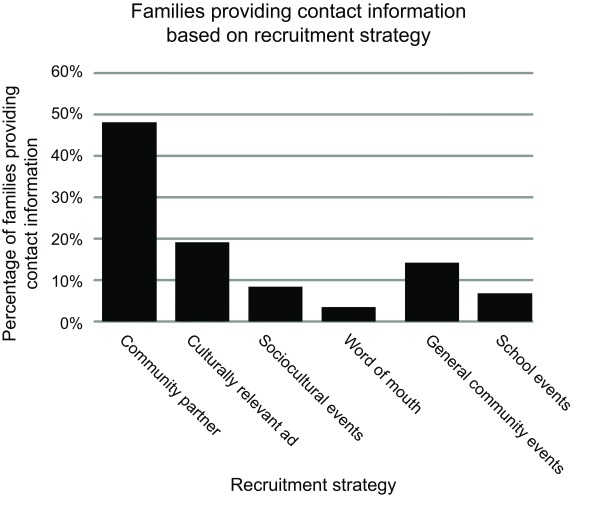
A total of 528 families were initially screened as eligible for the program. The majority of eligible participants were recruited through strategies channeled through sociocultural mediums (Figure 1). In total, 417 (79.0%) families were identified through strategies channeled through sociocultural mediums: 48.1% were identified through community partnerships, 19.1% were identified through culturally relevant advertisements, 8.3% were identified through sociocultural events, and 3.4% were identified by word-of-mouth. In total, 111 (21%) families were identified through strategies channeled through non-sociocultural mediums: 14.2% were identified through general community events and 6.8% of families were identified through school events.
Figure 1. Percentage of families initially interested in participation, by recruitment strategy.
Scheduling a Baseline Visit
Of families who were identified as eligible (n=528), 79.2% (n=418) scheduled a baseline visit. Logistic regression demonstrated that families recruited from culturally relevant ads, sociocultural events, or word-of-mouth were 1.9 times more likely to schedule a baseline visit than families recruited from non-sociocultural mediums (OR=1.96, 95% CI=1.05, 3.68). Being recruited from community partners vs non-sociocultural mediums was not associated with scheduling a baseline visit (OR=.95, 95% CI=.56, 1.60; Table 2).
Table 2. Logistic regression results for program outcomes by recruitment strategy.
| Scheduling Baseline Visit, n=528 | Enrollment in Run-In, n=388 | Participation in Intervention, n=224 | ||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| R2 | (.02) | (.01) | (.01) | |||
| Non-sociocultural mediums | Ref | Ref | Ref | |||
| Community partners | .95 | .56, 1.60 | .71 | .41, 1.22 | .71 | .34, 1.49 |
| Ads/sociocultural events/word-of-mouth | 1.96 | 1.05, 3.68a | .81 | .45, 1.43 | .58 | .27, 1.26 |
OR, odds ratio; 95% CI, 95% confidence interval. R2 values are Nagelkerke pseudo-R2 values.
a. Statistically significant findings.
Sample sizes were the total number of eligible participants.
Run-in Phase Enrollment
Among families who scheduled a baseline visit, 57.7% (n=224) enrolled in the run-in phase. There were no statistically significant differences in enrolling in the run-in phase among families recruited by culturally relevant ads, sociocultural events, or word-of-mouth vs non-sociocultural mediums (OR=.81, 95% CI=.45, 1.43) or among families recruited by community partners compared to non-sociocultural mediums (OR=.71, 95% CI=.41, 1.22; Table 2).
Intervention Enrollment
Among families enrolled in the run-in phase, 64.7% (n=145) enrolled in the intervention. There were no statistically significant differences in enrolling in the intervention among families recruited by culturally relevant ads, sociocultural events, or word-of-mouth compared to non-sociocultural mediums (OR=.58, 95% CI=.27, 1.26) or families recruited by community partners compared to non-sociocultural mediums (OR=.71, 95% CI=.34, 1.49; Table 2).
Demographic Characteristics by Recruitment Strategy
Tables 3 and 4 show the demographic and health characteristics of families enrolled in the intervention by recruitment strategy: community partners (n=64), culturally relevant ads, sociocultural events, or word-of-mouth (n=45), and general community events or school events (n=36). Parents recruited from sociocultural mediums were less likely to be employed (67.6%) compared to parents recruited from non-sociocultural mediums (88.2%; X2 (1, N=142) = 5.53, P<.05). Families recruited from sociocultural mediums were more likely to report an annual household income <$25,000 (44.4%) than families recruited from non-sociocultural mediums (20.6%; X2 (1, N=142) = 13.57, P<.05).
Table 3. Demographic characteristics based on recruitment strategy of families enrolled in the intervention.
| Characteristic | Community partners, n=64 | Ads, sociocultural events, and word-of-mouth, n=45 | General community events and school events, n=36 | |
| Child sex | ||||
| Male | 22 (34.4) | 17 (37.8) | 9 (25.0) | |
| Female | 42 (65.6) | 28 (62.2) | 27 (75.0) | |
| Child age | 13.84 (1.78) | 13.35 (1.71) | 13.15 (1.63) | |
| Child BMI (kg/m2) | 33.06 (7.42) | 33.75 (7.77) | 32.39 (6.10) | |
| Child WC (cm) | 90.68 (12.62) | 92.19 (14.36) | 89.63 (12.31) | |
| Parent sex | ||||
| Male | 4 (6.3) | 1 (2.2) | 2 (5.6) | |
| Female | 60 (93.8) | 44 (97.8) | 34 (94.4) | |
| Parent age | 44.19 (9.27) | 43.47 (6.97) | 42.99 (6.40) | |
| Parent marital status | ||||
| Married | 24 (37.5) | 17 (37.8) | 17 (47.2) | |
| Separated | 13 (20.3) | 11 (24.4) | 5 (13.9) | |
| Divorced | 10 (15.6) | 10 (22.2) | 5 (13.9) | |
| Widowed | 4 (6.3) | 0 (0) | 1 (2.8) | |
| Never married | 9 (14.1) | 3 (6.7) | 5 (13.9) | |
| In unmarried couple relationship | 3 (4.7) | 4 (8.9) | 1 (2.8) | |
| Unreported | 1 (1.6) | 0 (0) | 2 (5.6) | |
| Parent employment statusa | ||||
| Working | 39 (60.9) | 34 (75.6) | 30 (83.3) | |
| Unemployed | 7 (10.9) | 3 (6.7) | 3 (8.3) | |
| Retired | 3 (4.7) | 3 (6.7) | 0 (0) | |
| Disabled | 3 (4.7) | 2 (4.4) | 0 (0) | |
| Other | 11 (17.2) | 3 (6.7) | 1 (2.8) | |
| Unreported | 1 (1.6) | 0 (0) | 2 (5.6) | |
| Parent education | ||||
| HS or less | 17 (26.6) | 4 (8.9) | 1 (2.8) | |
| Some college | 22 (34.4) | 19 (42.2) | 13 (36.1) | |
| College degree or higher | 24 (37.5) | 22 (48.9) | 20 (55.6) | |
| Unreported | 1 (1.6) | 0 (0) | 2 (5.6) | |
| Annual household incomea | ||||
| <$10 K | 12 (18.8) | 6 (13.3) | 3 (8.3) | |
| $10-24 K | 18 (28.1) | 12 (26.7) | 4 (11.1) | |
| $25-39 K | 16 (25.0) | 12 (26.7) | 5 (13.9) | |
| $40 K+ | 17 (26.6) | 15 (33.3) | 22 (61.1) | |
| Unreported | 1 (1.6) | 0 (0) | 2 (5.6) | |
Child and parent age, BMI, and waist circumference (WC) reported as mean (standard deviation). All others reported as n (%).
a. P<.05, indicates a significant difference between families recruited through sociocultural mediums (including community partnerships, ads, sociocultural events, and word-of-mouth) and non-sociocultural mediums.
Table 4. Parent physical characteristics based on recruitment strategy of families enrolled in the intervention.
| Characteristic | Community partners, n=64 | Ads, sociocultural events, and word-of-mouth, n=45 | General community events and school events, n=36 | |
| Parent BMI (kg/m2) | ||||
| Mean (SD) | 36.23 (8.93) | 35.21 (8.71) | 35.89 (7.03) | |
| <25 | 4 (6.3) | 6 (13.3) | 2 (5.6) | |
| 25-<30 | 11 (17.2) | 8 (17.8) | 6 (16.6) | |
| ≥30 | 47 (73.4) | 31 (68.9) | 26 (72.2) | |
| Unreported | 2 (3.1) | 0 (0) | 2 (5.6) | |
| Parent waist circumference, cm, mean (SD) | 108.45 (18.29) | 107.16 (19.83) | 104.13 (13.35) | |
| Parent cardiovascular disease | ||||
| Yes | 5 (7.8) | 0 (0) | 0 (0) | |
| No | 56 (87.5) | 45 (100) | 34 (94.4) | |
| Don’t know | 2 (3.1) | 0 (0) | 0 (0) | |
| Unreported | 1 (1.6) | 0 (0) | 2 (5.6) | |
| Parent hypertension | ||||
| Yes | 27 (42.2) | 18 (40.0) | 12 (33.3) | |
| No | 35 (54.7) | 26 (57.8) | 22 (61.1) | |
| Don’t know | 1 (1.6) | 1 (2.2) | 0 (0) | |
| Unreported | 1 (1.6) | 0 (0) | 2 (5.6) | |
| Parent type 2 diabetes | ||||
| Yes | 14 (21.9) | 9 (20.0) | 3 (8.3) | |
| No | 49 (76.6) | 36 (80.0) | 30 (83.3) | |
| Don’t know | 0 (0) | 0 (0) | 1 (2.8) | |
| Unreported | 1 (1.6) | 0 (0) | 2 (5.6) | |
Data are n (%) unless noted otherwise.
Discussion
Our study aimed to determine whether there is benefit to using sociocultural recruitment mediums in interest, enrollment, and generalizability of the sample of a health promotion trial targeting African American families. Results of our study indicated that participants recruited via culturally relevant ads, sociocultural events, and word-of-mouth were more likely to schedule a baseline visit than families recruited from non-sociocultural mediums. While families recruited from strategies channeled through sociocultural mediums were not more likely to enroll in the run-in phase or enroll in the intervention program compared with families recruited from non-sociocultural mediums, these findings suggest that it is important to incorporate sociocultural recruitment strategies to encourage initial interest in participation.
Comparison of demographic factors of enrolled families by sociocultural recruitment strategies demonstrated that those recruited from sociocultural mediums had lower income and were less likely to be employed than families recruited from non-sociocultural mediums. Racial minorities of lower socioeconomic backgrounds are under-represented in health promotion interventions7,21 and past research has shown that individuals of lower socioeconomic status experience more barriers to participation and are less likely to enroll in interventions.22 Our findings suggest that sociocultural recruitment mediums may increase the diversity and generalizability of socioeconomic backgrounds among participants, but further research is needed to replicate these findings.
Some findings were not hypothesized. Sociocultural mediums may not have predicted further enrollment because sociocultural strategies were not used throughout the enrollment period. Recruitment through community partnerships may not have predicted interest or enrollment as a result of the extent to which partnerships were integrated into recruitment efforts. Community partners assisted in identifying relevant events, but were not involved with baseline visits or used to stay in touch with families during the two-week run-in phase. We are currently expanding recruitment efforts that use sociocultural mediums throughout the enrollment process to better utilize community resources. We have developed a community advisory board with prominent leaders in the local African American community that provide advice and assistance in recruiting participants in a culturally relevant way. Community liaisons are integrated into recruitment efforts such as developing testimonials from past study families to be used as a recruitment tool. Further research is needed to examine how continuing to address sociocultural values throughout the enrollment period affects enrollment of families.
This study suggests that recruitment strategies that incorporate sociocultural values are important in generating initial interest, but that other factors, such as participant barriers, may be important in predicting whether families enroll in a long-term intervention. Findings from examining barriers in our program indicated that competing demands, scheduling and transportation issues, and health problems may impede participants from enrolling into the long-term intervention programs which requires a greater commitment. Previous research has indicated that African American parents want more flexibility in scheduling, to complete program content at home, and assistance with child care and transportation in a health promotion program.23 Future investigators should build in flexibility to their recruitment approaches, enrollment process, and intervention,17 such as scheduling appointments on evenings or weekends, providing childcare, and assistance with transportation21 and integrating sociocultural values throughout the recruitment process.
There are several limitations of our study that should be noted. One limitation is that we were unable to calculate the recruitment yield of each our recruitment strategies. It is possible that more families were recruited from strategies channeled through sociocultural mediums because there were more recruitment events through sociocultural mediums than through non-sociocultural mediums. Our sample may not be generalizable to other populations given that it only targeted African American families living in one southeastern city. We were also unable to measure or account for other factors that may influence whether African Americans participate in research including the reputation of the research team, the level of trust held for the nature of the research, and the perceived benefit of participating. We also did not have baseline data on all participants so we could not control for covariates in our model. Despite these limitations, this is one of the first studies to systematically compare the use of sociocultural mediums on recruitment and enrollment rates in a large intervention trial in African Americans.
Conclusion
Our study extends upon existing research by directly comparing recruitment strategies channeled through sociocultural and non-sociocultural mediums on recruitment and enrollment outcomes. Results from this study highlight the importance of using culturally relevant recruitment strategies in initially scheduling families. Additionally, sociocultural mediums were effective in enrolling more diverse families which suggests that sociocultural mediums may be a useful strategy to obtain more generalizable samples in future intervention trials. Additional research is needed to examine whether continuing to address sociocultural values throughout the enrollment period will increase enrollment in health promotion interventions for underserved minority populations. Due to disproportionate rates of chronic diseases observed in African Americans, the use of sociocultural mediums may be important for increasing access and reducing barriers to enrollment in health promotion programs.
Acknowledgments
This work was supported by a grant from the National Institute of Child Health and Human Development to Dawn K. Wilson, PhD (R01HD072153), and in part by training grants from the National Institute of General Medical Sciences (T32 GM081740) to Lauren E. Huffman, M.A. and Haylee M. Gause, BS.
References
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806-814. 10.1001/jama.2014.732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilbur J, McDevitt J, Wang E, et al. Recruitment of African American women to a walking program: eligibility, ineligibility, and attrition during screening. Res Nurs Health. 2006;29(3):176-189. 10.1002/nur.20136 [DOI] [PubMed] [Google Scholar]
- 3.Staffileno BA, Coke LA. Recruiting and retaining young, sedentary, hypertension-prone African American women in a physical activity intervention study. J Cardiovasc Nurs. 2006;21(3):208-216. 10.1097/00005082-200605000-00009 [DOI] [PubMed] [Google Scholar]
- 4.Braunstein JB, Sherber NS, Schulman SP, Ding EL, Powe NR. Race, medical researcher distrust, perceived harm, and willingness to participate in cardiovascular prevention trials. Medicine (Baltimore). 2008;87(1):1-9. 10.1097/MD.0b013e3181625d78 [DOI] [PubMed] [Google Scholar]
- 5.Chandra A, Paul DP III. African American participation in clinical trials: recruitment difficulties and potential remedies. Hosp Top. 2003;81(2):33-38. 10.1080/00185860309598020 [DOI] [PubMed] [Google Scholar]
- 6.Dancy BL, Wilbur J, Talashek M, Bonner G, Barnes-Boyd C. Community-based research: barriers to recruitment of African Americans. Nurs Outlook. 2004;52(5):234-240. 10.1016/j.outlook.2004.04.012 [DOI] [PubMed] [Google Scholar]
- 7.Minkler M. Community-based research partnerships: challenges and opportunities. J Urban Health. 2005;82(2)(suppl 2):ii3-ii12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilson DK. New perspectives on health disparities and obesity interventions in youth. J Pediatr Psychol. 2009;34(3):231-244. 10.1093/jpepsy/jsn137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003;30(2):133-146. 10.1177/1090198102251021 [DOI] [PubMed] [Google Scholar]
- 10.Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999;9(1):10-21. [PubMed] [Google Scholar]
- 11.Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28(1):213-234. 10.1146/annurev.publhealth.28.021406.144016 [DOI] [PubMed] [Google Scholar]
- 12.Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312-323. 10.1177/1524839906289376 [DOI] [PubMed] [Google Scholar]
- 13.Breland-Noble AM, Bell CC, Burriss A, Poole HK, Board TAPAA; The AAKOMA Project Adult Advisory Board . The significance of strategic community engagement in recruiting African American youth and families for clinical research. J Child Fam Stud. 2012;21(2):273-280. 10.1007/s10826-011-9472-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wisdom K, Neighbors K, Williams VH, Havstad SL, Tilley BC. Recruitment of African Americans with type 2 diabetes to a randomized controlled trial using three sources. Ethn Health. 2002;7(4):267-278. 10.1080/1355785022000060727 [DOI] [PubMed] [Google Scholar]
- 15.Hartlieb KB, Jacques-Tiura AJ, Naar-King S, Ellis DA, Jen KL, Marshall S. Recruitment strategies and the retention of obese urban racial/ethnic minority adolescents in clinical trials: the FIT families project, Michigan, 2010-2014. Prev Chronic Dis. 2015;12:E22. 10.5888/pcd12.140409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wilson DK, Kitzman-Ulrich H, Resnicow K, et al. An overview of the Families Improving Together (FIT) for weight loss randomized controlled trial in African American families. Contemp Clin Trials. 2015;42:145-157. 10.1016/j.cct.2015.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alia KA, Wilson DK, McDaniel T, et al. Development of an innovative process evaluation approach for the Families Improving Together (FIT) for weight loss trial in African American adolescents. Eval Program Plann. 2015;49:106-116. 10.1016/j.evalprogplan.2014.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Audrain-McGovern J, Halbert CH, Rodriguez D, Epstein LH, Tercyak KP. Predictors of participation in a smoking cessation program among young adult smokers. Cancer Epidemiol Biomarkers Prev. 2007;16(3):617-619. 10.1158/1055-9965.EPI-06-0791 [DOI] [PubMed] [Google Scholar]
- 19.Goldberg JH, Kiernan M. Innovative techniques to address retention in a behavioral weight-loss trial. Health Educ Res. 2005;20(4):439-447. 10.1093/her/cyg139 [DOI] [PubMed] [Google Scholar]
- 20.Spring B, Duncan JM, Janke EA, et al. Integrating technology into standard weight loss treatment: a randomized controlled trial. JAMA Intern Med. 2013;173(2):105-111. 10.1001/jamainternmed.2013.1221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yancey AK, Ortega AN, Kumanyika SK. Effective recruitment and retention of minority research participants. Annu Rev Public Health. 2006;27(1):1-28. 10.1146/annurev.publhealth.27.021405.102113 [DOI] [PubMed] [Google Scholar]
- 22.Mendez JL, Carpenter JL, LaForett DR, Cohen JS. Parental engagement and barriers to participation in a community-based preventive intervention. Am J Community Psychol. 2009;44(1-2):1-14. 10.1007/s10464-009-9252-x [DOI] [PubMed] [Google Scholar]
- 23.Kitzman-Ulrich H, Wilson DK, Lyerly J. Qualitative perspectives from African American youth and caregivers for developing the Families Improving Together (FIT) for Weight Loss Intervention. Clin Pract Pediatr Psychol. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]