Abstract
Objective
Using 2004 New York City Health and Nutrition Examination Survey (NYC HANES) data, we sought to examine variation in hypertension (HTN) prevalence across eight Asian and Hispanic subgroups.
Design
Cross-sectional.
Setting
New York City, 2004.
Main Outcome Measures
Logistic regression was performed to identify differences in HTN prevalence between ethnic subgroups controlling for age, sex, education and BMI.
Results
Overall HTN prevalence among NYC adults was 25.5% (95% CI: 23.4-27.8), with 21.1% (95% CI: 18.2-24.3) among Whites, 32.8% (95% CI: 28.7-37.2) Black, 26.4% (95% CI: 22.3-31.0) Hispanics, and 24.7% (95% CI: 19.9-30.3) Asians. Among Hispanic subgroups, Dominicans had the highest HTN prevalence (32.2%), followed by Puerto Ricans (27.7%), while Mexicans had the lowest prevalence (8.1%). Among Asian subgroups, HTN prevalence was slightly higher among South Asians (29.9%) than among Chinese (21.3%). Adjusting for age, Dominican adults were nearly twice as likely to have HTN as non-Hispanic (NH) Whites (OR=1.96, 95% CI: 1.24-3.12), but this was attenuated after adjusting for sex and education (OR=1.27, 95% CI: .76 – 2.12). When comparing South Asians with NH Whites, results were also non-significant after adjustment (OR=2.00, 95% CI: .90-4.43).
Conclusions
When analyzing racial/ethnic subgroups, NH Black and Hispanic adults from Dominican Republic had the highest HTN prevalence followed by South Asian and Puerto Rican adults. Mexican adults had the lowest prevalence of all groups. These findings highlight that ethnic subgroup differences go undetected when stratified by broader racial/ethnic categories. To our knowledge, this is the first population-based study using objective measures to highlight these differences.
Keywords: Hypertension, Race/Ethnicity, Hispanic Subgroups, Asian Subgroups, New York City
Introduction
Hypertension (HTN), a modifiable risk factor for cardiovascular disease,1 is a leading cause of death worldwide.2 In the United States, federal initiatives such as Healthy People 2010 and the US Million Hearts Campaign have targeted efforts toward reducing HTN prevalence. Yet, efforts have had little effect; the prevalence of HTN has remained at approximately 33% between 2009 and 2012.3 Healthy People 2020 has again included prevention and control of HTN as one of the most critical public health goals.4–6 Although this initiative lacks a focus on reducing racial/ethnic differences, numerous population-based studies have identified disparities in the prevalence of HTN, with non-Hispanic Blacks having the highest prevalence of HTN (32.8%-42.1%)1,2,7,8, while other racial/ethnic groups have a fairly similar range of prevalence estimates: non-Hispanic Whites (21.1%-29.8%),1,2,7–9 Hispanics (24.7%-29.3%),1,7–9 and non-Hispanic Asians (24.7%-25.6%).8,10
To date, many of the population-based studies examining racial/ethnic differences in HTN prevalence have focused on differences between broad minority groups; few have examined differences in Asian and Hispanic sub-populations.1,5,8 Even fewer have used population-based samples or examined differences between Asian or Hispanic subgroups.11–14 This paucity of evidence has led to a lack of specific recommendations of HTN guidelines for specific minority subgroups and potential oversight of subgroups with elevated HTN rates dissimilar to the ethnic group average.
We utilized the 2004 New York City Health and Nutrition Examination Survey (NYC HANES) to characterize racial/ethnic differences among minority subgroups, with the hypothesis that Asian and Hispanic subgroups are heterogeneous and differences in HTN exist among these groups.
Methods
Database
NYC HANES 2004, modeled after the National Health and Nutrition Examination Survey (NHANES),15 was a population-based, cross-sectional examination survey of all non-institutionalized New York City residents aged ≥20 years. This survey included non-English speakers, non-literate individuals, pregnant woman, and the mentally or developmentally disabled. NYC HANES used a comparable three-stage probability sampling to select a representative sample of adult New York City residents from June to December 2004. Survey components consisted of a physical examination, clinical and laboratory tests, a face-to-face computer-assisted personal interview, and an audio computer-assisted self-interview. Interviews were pre-translated into English and Spanish, and a translator was used for interviews conducted in other languages. Detailed information on data collection protocols, response rate and study design has been published in detail previously.16
Study Population
Our current study utilized NYC HANES data for all participants who answered a blood pressure screening interview questionnaire and had valid blood pressure measurements through clinical and laboratory tests. Study participants who had an invalid answer to country of birth/origin question were excluded (n=10). For each participant, 3 to 4 systolic/diastolic blood pressure measurements were taken with standardized NHANES protocols and equipment.1 For the purposes of our study, the first blood pressure measurement was excluded and the average of the remaining measurements was utilized. If only one valid measurement was available, it was used. A total of 24 participants were excluded for not having valid hypertension interview data or blood pressure examination values for a final sample size of 1,965.
Measures
Hypertension was defined as: 1) an average systolic blood pressure ≥ 140 mm Hg; 2) an average diastolic blood pressure ≥ 90 mm Hg; or 3) self-reported current use of prescribed antihypertensive medication.17 Hypertension prevalence was estimated across racial/ethnic subgroups based on socio-demographic characteristics and hypertension risk factors.
We re-categorized self-reported race and Hispanic origin and then combined with country of birth/origin to identify Hispanic and Asian subgroups of interest. Hispanic subgroups included Puerto Rican, Dominican, Mexican, Other Central/South American, and other Hispanic adults. Asian subgroups included Chinese, South Asian, and other Asian adults. Participants whose answers did not correspond to one category were categorized as “Other.” Estimates for this group were not shown because of the small sample size (n=28). For insurance coverage, participants reporting any private health insurance were classified as having private insurance. Otherwise, persons aged ≥65 years who reported having Medicare were classified as having Medicare, and other government coverage included all remaining participants who reported having Medicaid, Medicare, or another government program.
Statistical Analyses
Analyses were weighted to adjust for the complex sampling design and non-response; weights were post-stratified to represent the NYC adult population on age, sex, race/ethnicity, and borough of residence, then further adjusted to address component- and item-level non-response. Demographic and behavioral characteristics including age, sex, education, income, insurance coverage, and health status (smoking, alcohol use, BMI) were stratified by ethnic subgroup. Age-standardized prevalence estimates of hypertension were calculated for major and subgroup race/ethnicity. Prevalence estimates were age adjusted to the year 2000 US standard population aged ≥20 years. Statistical significance for differences in bivariate comparisons was determined at the α=.05 level. Relative standard errors and 95% confidence intervals were calculated for means and percentages. Estimates with relative standard errors of ≥30% were noted as unreliable. Multiple logistic regression was used to assess factors associated with hypertension prevalence, including age, sex, education and BMI. SUDAAN version 9.0 (Research Triangle Institute, Research Triangle Park, Cary, NC) was used to apply sample weights and to obtain standard error estimates by Taylor series linearization.
Results
Demographic data are presented in Tables 1 and 2. Race/ethnic differences were found in age, education, insurance coverage, alcohol use and BMI (P<.05). Overall, Hispanics were more likely to be uninsured (32.8%) and obese (31.5%) compared with non-Hispanic Whites (NH) (11.2% and 22.9%, respectively). Among Hispanic subgroups, Mexican adults were found to have the highest proportion of uninsured (79.6%). When analyzing BMI, adults from Puerto Rico had the highest prevalence of obesity (41.6%). NH Asians were found to have the lowest prevalence of obesity among all race/ethnic groups (8.9%), and ranged from .7% to 15.2% when analyzing NH Asian subgroups.
Table 1. Demographic and behavioral characteristics by ethnic subgroup among NYC adults, NYC HANES 2004.
| Major race/ethnic group | |||||
| All NYC Adults, (N=1965) | Non-Hispanic White, (n=611) | Non-Hispanic Black, (n=426) | Hispanic, (n=642) | Non-Hispanic Asian, (n=258) | |
| Age group c,d | |||||
| <50 | 1380 (62.7) | 387 (56.2) | 292 (60.8) | 490 (70.3) | 190 (71.3) |
| ≥50 | 585 (37.3) | 224 (43.9) | 134 (39.2) | 152 (29.7) | 68 (28.7) |
| Sex c | |||||
| Male | 816 (46.1) | 290 (51.1) | 159 (42.2) | 241 (41.2) | 113 (47.6) |
| Female | 1149 (54.0) | 321 (48.9) | 267 (57.8) | 401 (58.8) | 145 (52.4) |
| Education c,d,e | |||||
| < High school | 564 (27.1) | 60 (11.2) | 136 (31.9) | 248 (46.0) | 78 (29.4) |
| High school | 384 (19.4) | 96 (16.8) | 92 (21.6) | 140 (21.4) | 49 (18.3) |
| > High school | 1014 (53.6) | 454 (72.0) | 198 (46.5) | 217 (32.7) | 130 (52.3) |
| Incomec,d,e | |||||
| < $20,000 | 645 (31.5) | 103 (18.0) | 139 (32.1) | 307 (49.1) | 88 (36.5) |
| ≥ $20,000 | 1272 (68.5) | 496 (82.0) | 278 (67.9) | 321 (50.9) | 157 (63.5) |
| Insurance coverage c,d,e | |||||
| Private | 967 (52.9) | 444 (73.2) | 210 (51.0) | 214 (33.1) | 91 (35.0) |
| Medicare/government | 528 (26.2) | 86 (15.6) | 131 (29.7) | 211 (34.2) | 86 (34.0)) |
| Uninsured | 461 (20.9) | 79 (11.2) | 84 (19.3) | 214 (32.8) | 78 (30.9) |
| Health Status | |||||
| Smoker d | 469 (23.1) | 150 (23.0) | 103 (23.0) | 151 (23.1) | 55 (21.7) |
| Alcohol use, heavy c,d,e | 152 (7.2) | 59 (8.7) | 31 (6.3) | 46 (6.7) | 9 (3.2) |
| BMI, obese c,d,e | 506 (26.1) | 133 (22.9) | 145 (33.8) | 199 (31.5) | 24 (8.9) |
Data are n (%).
a. Other Hispanic includes Cuban, Cuban American, Other Latin American, and Other Hispanic.
b. Other Asian includes Canada, Ghana, Guyana, Japan, Kazakhstan, Kyrgyzstan, Macau, Myanmar, North Korea, Philippines, South Korea, Trinidad and Tobago, Thailand, and Viet Nam.
c. P<.05 across all major race/ethnic groups.
d. P<.05 across Hispanic subgroups.
e. P<.05 across Asian subgroups.
Table 2. Demographic and behavioral characteristics by ethnic subgroup among NYC adults, NYC HANES 2004.
| Hispanic subgroups | Asian subgroups | |||||||
| Puerto Rican, (n=178) | Dominican, (n= 168) | Central/South American, (n= 146) | Mexican, (n= 79) | Other Hispanica, (n=71) | Chinese, (n=101) | South Asian, (n=60) | Other Asianb, (n=97) | |
| Age group c,d | ||||||||
| <50 | 129 (65.8) | 126 (68.2) | 111 (71.1) | 76 (96.3) | 48 (59.2) | 67 (66.7) | 50 (79.7) | 73 (73.0) |
| ≥50 | 49 (34.2) | 42 (31.8) | 35 (28.9) | 3 (3.8) | 23 (40.8) | 34 (36.3) | 10 (20.3) | 24 (27.0) |
| Sex c | ||||||||
| Male | 65 (40.5) | 61 (39.1) | 50 (36.8) | 37 (52.8) | 28 (44.7) | 45 (47.3) | 30 (54.7) | 38 (43.5) |
| Female | 113 (59.5) | 107 (60.9) | 96 (63.2) | 42 (47.2) | 43 (55.3) | 56 (52.7) | 30 (45.4) | 59 (56.5) |
| Education c,d,e | ||||||||
| < High school | 70 (42.6) | 77 (48.5) | 64 (44.6) | 51 (61.7) | 22 (36.1) | 46 (45.6) | 20 (32.6) | 12 (12.8) |
| High school | 38 (21.3) | 33 (18.1) | 31 (21.0) | 20 (27.9) | 18 (23.2) | 25 (25.2) | 9 (13.9) | 15 (14.8) |
| > High school | 69 (36.1) | 58 (33.4) | 51 (34.4) | 8 (10.5) | 31 (40.7) | 30 (29.2) | 31 (53.6) | 69 (72.4) |
| Incomec,d,e | ||||||||
| < $20,000 | 69 (39.4) | 86 (53.8) | 70 (48.5) | 58 (76.2) | 24 (36.5) | 46 (51.2) | 21 (35.9) | 21 (24.1) |
| ≥ $20,000 | 105 (60.6) | 78 (46.2) | 75 (51.5) | 19 (23.8) | 44 (63.5) | 48 (48.8) | 37 (64.1) | 72 (75.9) |
| Insurance coverage c,d,e | ||||||||
| Private | 82 (47.2) | 53 (30.4) | 47 (32.2) | 9 (11.4) | 23 (30.1) | 30 (30.0) | 17 (28.2) | 44 (43.8) |
| Medicare/government | 66 (38.4) | 79 (47.3) | 38 (28.5) | 8 (9.0) | 20 (32.3) | 41 (40.8) | 27 (44.3) | 18 (21.6) |
| Uninsured | 27 (14.4) | 36 (22.3) | 61 (39.3) | 62 (79.6) | 28 (37.6) | 29 (29.2) | 16 (27.5) | 33 (34.6) |
| Health Status | ||||||||
| Smoker d | 70 (38.3) | 25 (15.9) | 25 (15.9) | 11 (13.5) | 20 (28.0) | 22 (22.6) | 9 (15.5) | 24 (24.6) |
| Alcohol use, heavy c,d,e | 22 (11.4) | 10 (5.7) | 5 (3.1) | 6 (7.8) | 3 (4.5) | 5 (4.8) | 0 (0) | 4 (3.8) |
| BMI, obese c,d,e | 72 (41.6) | 54 (35.0) | 41 (27.1) | 18 (22.2) | 14 (19.3) | 1 (.7) | 8 (15.2) | 15 (12.5) |
Data are n (%).
a. Other Hispanic includes Cuban, Cuban American, Other Latin American, and Other Hispanic.
b. Other Asian includes Canada, Ghana, Guyana, Japan, Kazakhstan, Kyrgyzstan, Macau, Myanmar, North Korea, Philippines, South Korea, Trinidad and Tobago, Thailand, and Viet Nam.
c. P<.05 across all major race/ethnic groups.
d. P<.05 across Hispanic subgroups.
e. P<.05 across Asian subgroups.
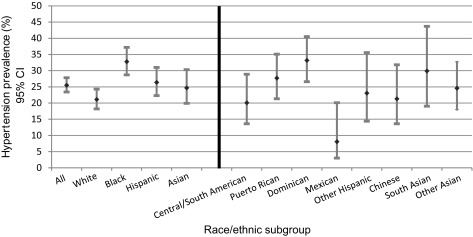
Overall hypertension prevalence among NYC adults was 25.5%, with 21.1% among NH Whites, 32.8% NH Blacks, 26.4% Hispanics, and 24.7% NH Asians (Figure 1). Among Hispanic subgroups, Dominicans were found to have the highest hypertension prevalence (32.2%), followed by Puerto Ricans (27.7%), while Mexicans had the lowest prevalence (8.1%). However, 96.3% of respondents in the Mexican subgroup were aged <50 years, potentially distorting the results. In a sensitivity analysis excluding pregnant women (n=29), results did not meaningfully change (data not shown). Adjusting for age, Dominican adults were nearly twice as likely to have hypertension as NH Whites (OR = 1.96, 95% CI: 1.24-3.12), but this increased risk was attenuated after also adjusting for sex and education (OR=1.27, 95% CI: .76 – 2.12) (Table 3).
Figure 1. Age standardized prevalence estimates of hypertension by major and subgroup race/ethnicity among NYC adults ≥20 years of age, NYC HANES, 2004.
Table 3. Logistic regression with race as a predictor for hypertension.
| Race/Ethnic group | Unadjusted OR (95% CI) | Adjusteda OR (95% CI) | Adjustedb OR (95% CI) |
| Non-Hispanic White | REF | REF | REF |
| Non-Hispanic Black | 1.47 (1.07-2.00) | 1.91 (1.33-2.76) | 1.51 (1.03-2.21) |
| Central/South American | .65 (.38-1.13) | .92 (.51-1.67) | .67 (.35-1.26) |
| Puerto Rican | 1.12 (.72-1.72) | 1.55 (.92-2.61) | 1.02 (.57-1.81) |
| Dominican Republic | 1.25 (.81-1.93) | 1.96 (1.24-3.12) | 1.27 (.76-2.12) |
| Mexican | .29 (.12-.72) | 1.06 (.40-2.83) | .64 (.23-1.76) |
| Other Hispanic | .89 (.45-1.77) | .94 (.46-1.95) | .73 (.34-1.57) |
| Chinese | .73 (.41-1.29) | .83 (.42-1.66) | .87 (.42-1.81) |
| South Asian | .94 (.47-1.85) | 2.02 (.90-4.51) | 2.00 (.90-4.43) |
| Other Asian | .70 (.38-1.32) | 1.08 (.58-2.03) | 1.21 (.60-2.42) |
a. Adjusted for age.
b. Adjusted for age, sex, education, and BMI.
Among Asian subgroups, South Asians had the highest hypertension prevalence (29.9%) and Chinese the lowest (21.3%). Differences between South Asians and NH Whites were still elevated, but non-significant after adjusting for age, and also age, sex, education and BMI (OR=2.00, 95% CI: .90-4.43) (Table 3).
Discussion
These findings demonstrate that sizable differences in HTN prevalence exist among ethnic subgroups that may go undetected when analyzing larger racial and ethnic groups; thus, subgroup-specific analyses should be undertaken when possible. When Hispanics and Asians were stratified by subgroups, Dominicans were found to have prevalence rates comparable to NH Blacks, with South Asians and Puerto Ricans having the next highest hypertension prevalance, respectively. In contrast, Mexicans were found to have the lowest prevalance compared with all groups, in part due to the young average age of this subgroup. Furthermore, when conducting age-adjusted analyses, Dominican and South Asian groups showed significant elevations in the odds of hypertension, attenuated only when adjusting further for sex and education. These findings suggest that Dominican and South Asian populations are at greater risk for HTN, potentially leading to cardiovascular disease. The excess risk for hypertension among South Asians has been reported previously;18 however, results have not been consistent.19 It should be noted that South Asians are a heterogeneous group with large variations in lifestyle patterns including diet and physical activity.20 Additionally, previous studies have identified that South Asians have an increased prevalence of diabetes, increasing the risk of cardiovascular disease.21 The lower average education level of these groups suggests greater focus must be placed on the creation of culturally sensative, low literacy educational approaches to improve HTN and cardiovascular diesease awareness.
The overall prevalence of HTN among NYC adults was 25.5%, which is lower than the national average (29.1%).8 However, the prevalence among ethnic subgroups was comparable to recent national health surveys,8 corroborating demonstrated disparities in disease distributions. Although factors related to these disparities were not identified here, previous analyses of African Americans and Hispanic populations noted the influence of several potential factors: hypercholesterolemia,22,23 obesity,1,22,23 smoking,22,23 low early-life socioeconomic status,24 low birth weight,25 salt sensitivity, and perceived discrimination.26 These factors have been shown to be further compounded by greater socioeconomic adversity, lower health literacy and the lack of health insurance.23 One could hypothesize that the impact of these factors could have a disproportional effect on ethnic subgroups when compared with the larger category. This may explain some of the differences noted between Dominicans and South Asians when compared with the larger racial group.
Our study has some limitations. The study population analyzed has a relatively small sample size resulting in potentially imprecise results, especially in the Mexican subgroup. The data for this study come from a single geographic area affecting the generalizability of our findings. However, NYC contains a diverse population including a high population of the studied minority subgroups, thus minimizing the potential for geographic bias. Finally, with the cross-sectional data available, we were unable to identify reasons for differences in racial subgroups, thus highlighting the need for further research.
HTN remains a global health challenge for all racial and ethnic subgroups; however, the findings presented here demonstrate that HTN prevalence varies within ethnic groups. Therefore, public health services should use this information to assist in the appropriate targeting of services to focus on high prevalence subgroups. Further research is needed to expand our knowledge related to disparities in HTN prevalence by ethnic subgroup and to identify underlying risk factors for these disparities.
References
- 1.Angell SY, Garg RK, Gwynn RC, Bash L, Thorpe LE, Frieden TR. Prevalence, awareness, treatment, and predictors of control of hypertension in New York City. Circ Cardiovasc Qual Outcomes. 2008;1(1):46-53. 10.1161/CIRCOUTCOMES.108.791954 [DOI] [PubMed] [Google Scholar]
- 2.Minor DS, Wofford MR, Jones DW. Racial and ethnic differences in hypertension. Curr Atheroscler Rep. 2008;10(2):121-127. 10.1007/s11883-008-0018-y [DOI] [PubMed] [Google Scholar]
- 3.Mozaffarian D, Benjamin EJ, Go AS, et al. ; American Heart Association Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29-e322. 10.1161/CIR.0000000000000157 [DOI] [PubMed] [Google Scholar]
- 4. .Healthy People 2020. U.S. Department of Health & Human Services. https://www.healthypeople.gov/2020/topics-objectives/topic/heart-disease-and-stroke/objectives. Accessed February 2, 2015.
- 5.Egan BM, Li J, Hutchison FN, Ferdinand KC. Hypertension in the United States, 1999 to 2012: progress toward Healthy People 2020 goals. Circulation. 2014;130(19):1692-1699. 10.1161/CIRCULATIONAHA.114.010676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sommers BD. Hypertension and Healthy People 2020: the role of health insurance expansion. Circulation. 2014;130(19):1674-1675. 10.1161/CIRCULATIONAHA.114.012874 [DOI] [PubMed] [Google Scholar]
- 7.Giles T, Aranda JM Jr, Suh D-C, et al. Ethnic/racial variations in blood pressure awareness, treatment, and control. J Clin Hypertens (Greenwich). 2007;9(5):345-354. http://www.ncbi.nlm.nih.gov/pubmed/17485970. Accessed January 26, 2015. 10.1111/j.1524-6175.2007.06432.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the United States: National Health and Nutrition Examination Survey, 2011-2012. NCHS Data Brief. 2013;(133):1-8. http://www.ncbi.nlm.nih.gov/pubmed/24171916. Accessed February 3, 2015. [PubMed] [Google Scholar]
- 9.Sorlie PD, Allison MA, Avilés-Santa ML, et al. Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2014;27(6):793-800. 10.1093/ajh/hpu003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aoki Y, Yoon SS, Chong Y, Carroll MD. Hypertension, abnormal cholesterol, and high body mass index among non-Hispanic Asian adults: united States, 2011-2012. NCHS Data Brief. 2014;(140):1-8. http://www.ncbi.nlm.nih.gov/pubmed/24429341. Accessed February 3, 2015. [PubMed] [Google Scholar]
- 11.Zhao B, Jose PO, Pu J, et al. Racial/Ethnic Differences in Hypertension Prevalence, Treatment, and Control for Outpatients in Northern California 2010-2012. Am J Hypertens. 2014;(October). 10.1093/ajh/hpu189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ye J, Rust G, Baltrus P, Daniels E. Cardiovascular risk factors among Asian Americans: results from a National Health Survey. Ann Epidemiol. 2009;19(10):718-723. 10.1016/j.annepidem.2009.03.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pabon-Nau LP, Cohen A, Meigs JB, Grant RW. Hypertension and diabetes prevalence among U.S. Hispanics by country of origin: the National Health Interview Survey 2000-2005. J Gen Intern Med. 2010;25(8):847-852. 10.1007/s11606-010-1335-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Borrell LN, Menendez BS, Joseph SP. Racial/ethnic disparities on self-reported hypertension in New York City: examining disparities among Hispanic subgroups. Ethn Dis. 2011;21(4):429-436. http://www.ncbi.nlm.nih.gov/pubmed/22428346. Accessed January 26, 2015. [PubMed] [Google Scholar]
- 15. .National Center for Health Statistics : NHANES Analytic Guidelines. http://www.cdc.gov/nchs/data/nhanes/analytic_guidelines_11_12.pdf. Published 2013. Accessed February 2, 2015.
- 16.Thorpe LE, Gwynn RC, Mandel-Ricci J, et al. Study design and participation rates of the New York City Health and Nutrition Examination Survey, 2004. Prev Chronic Dis. 2006;3(3):A94. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1637802&tool=pmcentrez&rendertype=abstract. Accessed January 23, 2015. [PMC free article] [PubMed] [Google Scholar]
- 17.Gee ME, Campbell N, Sarrafzadegan N, et al. Standards for the uniform reporting of hypertension in adults using population survey data: recommendations from the World Hypertension League Expert Committee. J Clin Hypertens (Greenwich). 2014;16(11):773-781. 10.1111/jch.12387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. .Anand SS, Yusuf S, Vuksan V, et al. Differences in risk factors, atherosclerosis, and cardiovascular disease between ethnic groups in Canada: the Study of Health Assessment and Risk in Ethnic groups (SHARE). Lancet (London, England). 2000;356(9226):279-284. http://www.ncbi.nlm.nih.gov/pubmed/11071182. Accessed March 22, 2016. [DOI] [PubMed]
- 19. .Enas EA, Garg A, Davidson MA, Nair VM, Huet BA, Yusuf S. Coronary heart disease and its risk factors in first-generation immigrant Asian Indians to the United States of America. Indian Heart J. 48(4):343-353. http://www.ncbi.nlm.nih.gov/pubmed/8908818. Accessed March 22, 2016. [PubMed]
- 20.Gupta M, Brister S, Verma S. Is South Asian ethnicity an independent cardiovascular risk factor? Can J Cardiol. 2006;22(3):193-197. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=2528919&tool=pmcentrez&rendertype=abstract. Accessed March 22, 2016. 10.1016/S0828-282X(06)70895-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thorpe LE, Upadhyay UD, Chamany S, et al. Prevalence and control of diabetes and impaired fasting glucose in New York City. Diabetes Care. 2009;32(1):57-62. 10.2337/dc08-0727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Daviglus ML, Talavera GA, Avilés-Santa ML, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17):1775-1784. 10.1001/jama.2012.14517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Daviglus ML, Pirzada A, Talavera GA. Cardiovascular disease risk factors in the Hispanic/Latino population: lessons from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prog Cardiovasc Dis. 2014;57(3):230-236. 10.1016/j.pcad.2014.07.006 [DOI] [PubMed] [Google Scholar]
- 24.James SA, Van Hoewyk J, Belli RF, Strogatz DS, Williams DR, Raghunathan TE. Life-course socioeconomic position and hypertension in African American men: the Pitt County Study. Am J Public Health. 2006;96(5):812-817. 10.2105/AJPH.2005.076158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bergvall N, Iliadou A, Tuvemo T, Cnattingius S. Birth characteristics and risk of high systolic blood pressure in early adulthood: socioeconomic factors and familial effects. Epidemiology. 2005;16(5):635-640. http://www.ncbi.nlm.nih.gov/pubmed/16135939. Accessed February 16, 2016. 10.1097/01.ede.0000172134.45742.49 [DOI] [PubMed] [Google Scholar]
- 26.Sims M, Diez-Roux AV, Dudley A, et al. Perceived discrimination and hypertension among African Americans in the Jackson Heart Study. Am J Public Health. 2012;102(S2)(suppl 2):S258-S265. 10.2105/AJPH.2011.300523 [DOI] [PMC free article] [PubMed] [Google Scholar]