Abstract
This inaugural memorial lecture provides an opportunity to celebrate the life of Elijah B. Saunders, MD, FACC and pays tribute to his pioneering spirit in the quest to advance health equity in the prevention and control of hypertension and cardiovascular diseases. It also enables an assessment of the state of the global burden of hypertension and related disparities. Despite the remarkable biomedical research progress made over the last half-century, hypertension remains the leading risk factor for global disease burden and the major preventable contributor to cardiovascular and all-cause mortality. Additionally, disparities in hypertension-related morbidity and mortality remain pervasive worldwide. National hypertension control rates showing progress often mask important suboptimal treatment and control in population groups defined by sex, race, ethnicity, geography, and social and environmental determinants. Within these groups, many hypertension-related disparities remain largely unchanged while other gaps have widened. In essence, current research has been relatively ineffective in guiding large-scale, sustained elimination of hypertension-related disparities. An important explanation for these observations may be the significant advances made in observational epidemiological research, especially in improved surveillance and data collection that document the extent of disparities in marked contrast to the relative paucity of interventional disparities research. The paucity of these interventional research studies remains a continuing challenge. The time has come for renewed efforts in building strategic partnerships that leverage transdisciplinary, multi-sectoral expertise to provide global leadership in interventional implementation research for hypertension control and elimination of related disparities. Developing an appropriately skilled implementation research workforce will be crucial. The National Heart, Lung, and Blood Institute and its biomedical research funding partners remain committed to a strategic agenda of implementation research, training, and education for the prevention and control of hypertension and elimination of related disparities.
Keywords: Hypertension; Blood Pressure; Prevalence; Control Rate; Mortality; Disparities; Global, Low- and Middle-Income Countries
Introduction
“The patient, like art, is bigger than we are. He will have the last word. He will outlast us. His pain will be ours, and his terror, and his hopes, and finally, perhaps, his illness. For what are we all, ultimately, but patients.”
From JH Stone. The Patient as Art. The Pharos of Alpha Omega Alpha. 1974;37:9-10,31
Quoted in the preface to Hypertension in Blacks by Hall, Saunders, Shulman.1
The Inaugural Elijah B. Saunders Memorial Keynote Lecture at the 2015 National Medical Association Convention provided a unique opportunity to pay tribute to a quiet medical giant who touched the lives of numerous patients. Dr. Saunders (Figure 1) dedicated his life to patient care, teaching, clinical research, and community service. The patient was at the center of his professional activities. He was a pioneer in efforts to advance health equity in the prevention and control of hypertension for medically underserved communities in his native Baltimore, Maryland, and in other parts of the United States and globally.2-4 He was also among the first to recognize that effective prevention and control of hypertension required reaching beyond the clinic to engage patients and their families in their places of worship,5 through social media,6 and as part of community partnerships for action.7, 8 As one of the founders of the International Society of Hypertension in Blacks, Dr. Saunders was a strong advocate for advancing hypertension education, training, research, and patient care in Africa and the African diaspora worldwide. It was therefore considered quite appropriate that the inaugural lecture focus on the global consequences of hypertension and related health disparities. In this article, the content of that inaugural lecture is presented with emphasis on the global implications of raised blood pressure and related health disparities.
Figure 1. Elijah B. Saunders, MD, FACC, FACP, FAHA, FASH.

The Global Prevalence of Hypertension and Related Disparities
Hypertension is the leading risk factor for global disease burden9 and the major contributor to cardiovascular complications and mortality worldwide.10, 11 An estimated one billion adults live with hypertension worldwide – a prevalence that is projected to increase to 1.6 billion by 2025.12 Researchers have documented important disparities in hypertension prevalence and global trends in population mean systolic blood pressure.13 For example, in a systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants between 1980 and 2008, Danaei et al13 showed that average systolic blood pressure declined at the global level by 1.0 mm Hg per decade in women and 0.8 mm Hg per decade in men. However, this modest global decline masked some fairly dramatic regional trends. In Western Europe, Australasia, high-income North America, and Asia Pacific, systolic blood pressure declined significantly in both sexes. In contrast, systolic blood pressure appeared unchanged in the Caribbean and increased in Oceania, east Africa, and South and Southeast Asia for both sexes, and in West Africa for women.13 Although systolic blood pressure in women fell by as much as 3.5 mm Hg per decade or greater in Western Europe and Australasia, it increased by as much as 1.0 – 2.7 mm Hg per decade in women in South and Southeast Asia, and in East and West Africa. Similarly, systolic blood pressure in men was highest in some East and West African and some Baltic countries where the mean systolic blood pressure was at least 138 mm Hg.13 These data suggest worrisome trends for hypertension, especially in many low- and middle-income countries in comparison to observations in high-income countries.13
Data from nationally representative household assessments from 2007 to 2010 as part of the World Health Organization Study on Global Aging and Adult Health showed that hypertension prevalence in the six middle-income countries examined (China, Ghana, India, Mexico, Russia, and South Africa) ranged from 23% in India to 52% in Russia.14 Overall, hypertension prevalence in these six countries was 37%.14 Among all hypertensive persons, two-thirds were diagnosed and 90% were untreated.14 In multivariate analyses, advancing age, sex, health insurance status, and alcohol use were all important drivers of increased hypertension prevalence and rates of being undiagnosed in these middle-income countries.14
In another study of sample surveys that were national in scope and conducted in the 1990s in several European countries, Canada, and the United States, marked geographic disparities in the prevalence of hypertension were noted. The overall age- and sex-adjusted prevalence of hypertension was higher in the European countries (44%) than in the two North American countries (28%) when using a threshold systolic/diastolic blood pressure of 140/90 mm Hg to define hypertension.15 Similarly marked geographic disparities in the treatment and control of hypertension were found across these European countries, Canada, and the United States.16 For example, among persons aged 35 to 64 years who were taking medications to control hypertension to the 140/90 mmHg blood pressure target, control rates were 29% in the United States, 17% in Canada, and 10% or lower in Germany, Sweden, England, Spain, and Italy.16 More recent surveys show varying degrees of progress made in the treatment and control of hypertension in several countries. For example, Falaschetti et al17 examined cross-sectional data from the Health Survey for England and demonstrated that hypertension control among treated patients nearly doubled from 33% in 1994 to 63% in 2011. However, among all adults with survey-defined hypertension in 2011, hypertension was controlled in only 37%.17 Similarly, in the most recent analysis of five population-based data sources that included the Canadian Health Measures Survey to determine the latest directly measured prevalence, awareness and control estimates in 2012-2013, Padwal et al18 reported control rates of >68% among all hypertensive adults; this rate is significantly higher than corresponding control rates in China and the United States (~10% and 53%, respectively).18-21
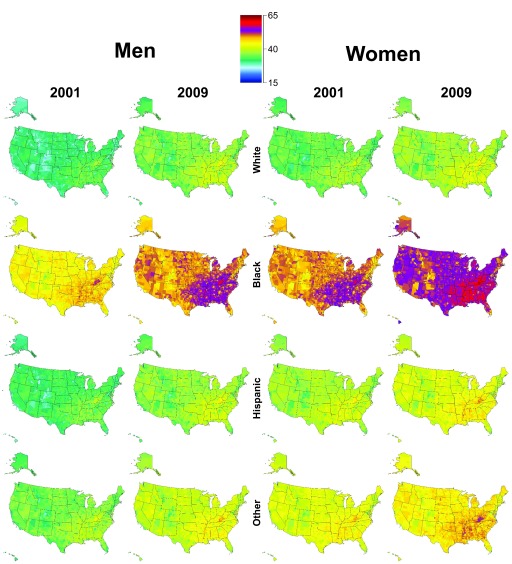
These national-level geographic differences mask an even worse picture of hypertension prevalence, treatment and control for many population groups and communities at the sub-national level. For example, the United States National Health and Nutrition Examination Survey (for non-institutionalized adults aged >18 years) in 2011-2014 showed a national hypertension prevalence of 29% but a much higher prevalence in non-Hispanic Blacks (41.2%).19 Similarly, the national prevalence of controlled hypertension in adults was 53%; but was much higher among non-Hispanic Whites (55.7%) than non-Hispanic Blacks (48.5%), non-Hispanic Asians (43.5%), or Hispanics (47.4%).19 In the Hispanic Community Study/Study of Latinos, Sorlie et al showed that, although the overall age-adjusted prevalence of hypertension was 26.1% for men and 25.3% for women, the corresponding prevalence was lowest in South American women (17.2%) and highest in Dominican men (34.3%).22 Figure 2 shows the age-standardized prevalence of total hypertension in United States counties by sex, race, and ethnicity among adults aged >30 years in 2001 and 2009. These disparities in prevalence and control of hypertension have major consequences and implications for hypertension-related fatal and non-fatal events at the county and national levels. They also highlight the important role race, ethnicity, geographic location, educational attainment, and other social and environmental determinants play in the consequences and complications of hypertension.
Figure 2. Age-standardized prevalence of total hypertension in US counties by sex, race, and Hispanic origin among adults 30 years and older in 2001 and 2009.
Reproduced from Olives C, Myerson R, Mokdad AH, Murray CJ, Lim SS. Prevalence, awareness, treatment, and control of hypertension in United States counties, 2001-2009. PLoS One 2013;8(4):e60308.
Disparities in Hypertension-Related Mortality
In one study comparing recent national survey data on prevalence, awareness, treatment and control of hypertension in England, United States and Canada, and correlated survey findings with each country’s stroke and ischemic heart disease (IHD) mortality, Joffres et al21 demonstrated that national-level differences in mortality rates from stroke and IHD paralleled the differences in hypertension awareness, treatment and control between these three countries. In addition, stroke and IHD mortality were strongly inversely correlated with mean systolic blood pressure in each country.21 These findings most likely also hold at the sub-national level. For example, in the United States, hypertension-related mortality is highest in African Americans who have the highest prevalence of hypertension and also have control rates lower than the national average rate or the control rates in non-Hispanic Whites.23 Trends in age-adjusted hypertension-related death rates in the United States are shown in Figure 3. Although the gap in hypertension-related mortality rates between non-Hispanic Blacks and non-Hispanic Whites is beginning to narrow, it remains approximately 70% higher in non-Hispanic Blacks.23 The gap is even starker when analyzed by sex. For example, in 2013, the death rates per 100,000 were nearly 52 for non-Hispanic Black men but 19 for non-Hispanic White men, and 20 for Hispanic men.24 The corresponding rates for women were 37 for non-Hispanic Black women, 16 for non-Hispanic White women, and 15 for Hispanic women.24
Figure 3. Age-adjusted hypertension-related death rates, by race and Hispanic origin: United States, 2000–2013.
Reproduced from Kung & Xu (2015) with permission from the Centers for Disease Control and Prevention (CDC) National Center for Health Statistics. The linear increases for the non-Hispanic White population from 2000 through 2013 and for the Hispanic and non-Hispanic Black populations from 2000 through 2005 are statistically significant at the P<.05 level. Linear decreases for the non-Hispanic Black population from 2005 to 2013 and for the Hispanic population from 2005 to 2009 are statistically significant at the P<.05 level. Hypertension-related deaths are identified using ICD–10 codes I10, I11, I12, I13, and I15 for underlying and contributing causes of death, according to the International Classification of Diseases, 10th revision (ICD–10). Data table for Figure 3 can be found at http://www.cdc.gov/nchs/data/databriefs/db193_table.pdf. SOURCE: CDC/NCHS, National Vital Statistics System, Mortality.
Although Hispanics/Latinos in the United States are considered as one ethnic group, significant differences in hypertension prevalence and related mortality have been demonstrated when the population is stratified by geographic origin as shown in the Hispanic Community Health Study/Study of Latinos that includes individuals of Cuban, Dominican, Mexican, Puerto Rican, Central American, and South American backgrounds.22,25 We have previously demonstrated that Puerto Rican Americans had consistently higher hypertension-related mortality rates than all other Hispanic subpopulations and non-Hispanic Whites.26,27
Advancing Research in Hypertension-Related Disparities
Despite the substantial investments in hypertension research and the wealth of available data on effective interventions, hypertension and related disparities in prevalence, morbidity and mortality remain pervasive worldwide. One possible explanation for this observation is the fact that most research investments in hypertension disparities have been made in areas that Kilbourne et al28 have considered first and second phases of health services-related research in disparities. In their conceptual framework to guide future health disparities research, phase 1 addresses “detecting differences in health and health care” while phase 2 focuses on “understanding the determinants that underlie disparities.”28 At the national and global level, we have much fewer research examples from the third phase that focuses on “development and implementation of interventions that reduce or eliminate disparities in health or health care.”28 Important issues related to phase 3 research within this conceptual framework include: appropriateness of the intervention for the communities of interest; acceptability and affordability of the interventions; availability of appropriate evaluation techniques; assessment of organizational readiness for the interventions; and importantly, development of strategies that are likely to inform and influence policy.28
To explore the challenge of limited phase 3 health services-related disparities research in hypertension in the United States, we identified 39 interventions and several state and national policy initiatives that were designed to address the reduction of racial and ethnic disparities in hypertension control.29 Most of the participants in these studies were African American patients. Among the completed interventions, 27 demonstrated some improvement in hypertension control or related process measures, while 7 did not. Of the 6 studies that specifically examined disparities, 3 reduced, 2 increased, and 1 had no effect on disparities.29 Thus, in our assessment, these findings call for the need to strengthen the evidence base for effective interventions that can guide dissemination and translation into policy and practice.29 There is also the concomitant need to stimulate rigorous evaluation of pragmatic, sustainable and multilevel interventions. Long-term success in these efforts will also require attention to building a pipeline for training an appropriate dissemination and implementation research workforce. Strategic transdisciplinary partnerships among payers, patients, providers, researchers, policymakers, and community-based organizations will be crucial in these endeavors.29
Conclusions
This inaugural keynote lecture has provided an opportunity to celebrate the life of Dr. Elijah Saunders and pay tribute to his pioneering spirit in the quest to advance health equity in the prevention and control of hypertension and cardiovascular diseases. It has also enabled an assessment of the state of the global burden of hypertension and related disparities. Although important progress has been made, the global consequences of uncontrolled hypertension remain dire. The paucity of interventional research studies to inform clinical and public health practice for the elimination of hypertension-related disparities remains the Achilles’ heel of health disparities research and a void that Dr. Saunders recognized and tirelessly promoted as critical to eliminating disparities.3,4 The time has come for renewed efforts in building strategic partnerships that leverage transdisciplinary, multi-sectoral expertise to provide global leadership in rigorously designed interventional studies that point the way to optimal prevention and control of hypertension and elimination of related disparities. The National Heart, Lung, and Blood Institute and its global alliance of biomedical research funding partners remain committed to a strategic agenda of implementation research, training and education for the prevention and control of hypertension and the elimination of related disparities.30, 31
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; National Institutes of Health; or the United States Department of Health and Human Services.
Presented as the Inaugural Elijah B. Saunders Memorial Keynote Lecture at the 2015 Annual Convention and Scientific Assembly of the National Medical Association, August 3, 2015.
References
- 1.Hall WD, Saunders E, Shulman NB. Hypertension in Blacks: Epidemiology, Pathophysiology and Treatment. Chicago: Year Book Medical Publishers; 1985. [Google Scholar]
- 2. .Association of American Medical Colleges In Memoriam: Elijah Saunders, MD. AAMC 2015 April 20;Available at: URL: https://www.aamc.org/newsroom/aamcstat/,a=430120. AccessedAugust 15, 2015.
- 3.Egan BM. Elijah Saunders in Memoriam. J Clin Hypertens (Greenwich). 2015;17(6):415-417. 10.1111/jch.12587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mensah GA, Norris KC. Advancing health equity: honoring the legacy of Dr. Elijah B. Saunders. Ethn Dis. 2015;25(4):381-382. 10.18865/ed.25.4.381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saunders E, Kong BW. A role for churches in hypertension management. Urban Health. 1983;12(5):49-51, 55. [PubMed] [Google Scholar]
- 6.Shaya FT, Chirikov VV, Daniel Mullins C, et al. Social networks help control hypertension. J Clin Hypertens (Greenwich). 2013;15(1):34-40. 10.1111/jch.12036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mullins CD, Shaya FT, Blatt L, Saunders E. A qualitative evaluation of a citywide Community Health Partnership program. J Natl Med Assoc. 2012;104(1-2):53-60. 10.1016/S0027-9684(15)30124-3 [DOI] [PubMed] [Google Scholar]
- 8.Johnson W, Shaya FT, Khanna N, et al. The Baltimore Partnership to Educate and Achieve Control of Hypertension (The BPTEACH Trial): a randomized trial of the effect of education on improving blood pressure control in a largely African American population. J Clin Hypertens (Greenwich). 2011;13(8):563-570. 10.1111/j.1751-7176.2011.00477.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224-2260. 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Forouzanfar MH, Alexander L, Anderson HR, et al. ; GBD 2013 Risk Factors Collaborators . Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(10010):2287-2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.GBD 2013 Mortality and Causes of Death Collaborators . Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385(9963):117-171. 10.1016/S0140-6736(14)61682-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005;365(9455):217-223. 10.1016/S0140-6736(05)70151-3 [DOI] [PubMed] [Google Scholar]
- 13.Danaei G, Finucane MM, Lin JK, et al. ; Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Pressure) . National, regional, and global trends in systolic blood pressure since 1980: systematic analysis of health examination surveys and epidemiological studies with 786 country-years and 5·4 million participants. Lancet. 2011;377(9765):568-577. 10.1016/S0140-6736(10)62036-3 [DOI] [PubMed] [Google Scholar]
- 14.Basu S, Millett C. Social epidemiology of hypertension in middle-income countries: determinants of prevalence, diagnosis, treatment, and control in the WHO SAGE study. Hypertension. 2013;62(1):18-26. 10.1161/HYPERTENSIONAHA.113.01374 [DOI] [PubMed] [Google Scholar]
- 15.Wolf-Maier K, Cooper RS, Banegas JR, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA. 2003;289(18):2363-2369. 10.1001/jama.289.18.2363 [DOI] [PubMed] [Google Scholar]
- 16.Wolf-Maier K, Cooper RS, Kramer H, et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension. 2004;43(1):10-17. 10.1161/01.HYP.0000103630.72812.10 [DOI] [PubMed] [Google Scholar]
- 17.Falaschetti E, Mindell J, Knott C, Poulter N. Hypertension management in England: a serial cross-sectional study from 1994 to 2011. Lancet. 2014;383(9932):1912-1919. 10.1016/S0140-6736(14)60688-7 [DOI] [PubMed] [Google Scholar]
- 18.Padwal RS, Bienek A, McAlister FA, Campbell NR; Outcomes Research Task Force of the Canadian Hypertension Education Program . Epidemiology of hypertension in Canada: an update. Can J Cardiol. 2016;32(5):687-694. 10.1016/j.cjca.2015.07.734 [DOI] [PubMed] [Google Scholar]
- 19.Yoon SS, Carroll MD, Fryar CD. Hypertension Prevalence and Control Among Adults: united States, 2011-2014. NCHS Data Brief. 2015;(220):1-8. [PubMed] [Google Scholar]
- 20.Wang J, Zhang L, Wang F, Liu L, Wang H; China National Survey of Chronic Kidney Disease Working Group . Prevalence, awareness, treatment, and control of hypertension in China: results from a national survey. Am J Hypertens. 2014;27(11):1355-1361. 10.1093/ajh/hpu053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joffres M, Falaschetti E, Gillespie C, et al. Hypertension prevalence, awareness, treatment and control in national surveys from England, the USA and Canada, and correlation with stroke and ischaemic heart disease mortality: a cross-sectional study. BMJ Open. 2013;3(8):e003423. 10.1136/bmjopen-2013-003423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sorlie PD, Allison MA, Avilés-Santa ML, et al. Prevalence of hypertension, awareness, treatment, and control in the Hispanic Community Health Study/Study of Latinos. Am J Hypertens. 2014;27(6):793-800. 10.1093/ajh/hpu003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kung HC, Xu J. Hypertension-related Mortality in the United States, 2000-2013. NCHS Data Brief. 2015;(193):1-8. [PubMed] [Google Scholar]
- 24.Mozaffarian D, Benjamin EJ, Go AS, et al. ; Writing Group Members; American Heart Association Statistics Committee; Stroke Statistics Subcommittee . Heart Disease and Stroke Statistics-2016 Update: A Report From the American Heart Association. Circulation. 2016;133(4):e38-e60. 10.1161/CIR.0000000000000350 [DOI] [PubMed] [Google Scholar]
- 25.Daviglus ML, Talavera GA, Avilés-Santa ML, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA. 2012;308(17):1775-1784. 10.1001/jama.2012.14517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zambrana RE, Ayala C, Pokras OC, Minaya J, Mensah GA. Disparities in hypertension-related mortality among selected Hispanic subgroups and non-Hispanic White women ages 45 years and older--United States, 1995-1996 and 2001-2002. Ethn Dis. 2007;17(3):434-440. [PubMed] [Google Scholar]
- 27.Ayala C, Moreno MR, Minaya JA, Croft JB, Mensah GA; Centers for Disease Control and Prevention (CDC) . Hypertension-related mortality among Hispanic subpopulations--United States, 1995-2002. MMWR Morb Mortal Wkly Rep. 2006;55(7):177-180. [PubMed] [Google Scholar]
- 28.Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: a conceptual framework. Am J Public Health. 2006;96(12):2113-2121. 10.2105/AJPH.2005.077628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mueller M, Purnell TS, Mensah GA, Cooper LA. Reducing racial and ethnic disparities in hypertension prevention and control: what will it take to translate research into practice and policy? Am J Hypertens. 2015;28(6):699-716. 10.1093/ajh/hpu233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mensah GA, Kiley J, Mockrin SC, et al. National Heart, Lung, and Blood Institute Strategic Visioning: setting an agenda together for the NHLBI of 2025. Am J Public Health. 2015;105(5):e25-e28. 10.2105/AJPH.2015.302605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tobe SW. Global Alliance for Chronic Diseases Hypertension Research Teams With the World Hypertension League. The Global Alliance for Chronic Diseases Supports 15 Major Studies in Hypertension Prevention and Control in Low- and Middle-Income Countries. J Clin Hypertens (Greenwich). 2016;18:600 [DOI] [PMC free article] [PubMed] [Google Scholar]