Abstract
Aim:
Self-perceived health is considered a suitable health indicator, based on a single item asking individuals to rate their health. It has been recommended as a reliable factor to assess the population health. Several socio-demographic and lifestyle determinants of self-perceived health status have been documented in different population. The aim of our study was to assess the socio-demographic and lifestyle correlates of self-perceived health status in a population-based sample of Albanian adult men and women.
Methods:
Data from 12,554 individuals aged ≥35 years collected by the Albania Living Standard Measurement Survey (LSMS) 2012, which is a national population-based cross-sectional study, were analyzed. The study participants rated their health in five categories: very good, good, average, poor and very poor, which in the analyses were dichotomized into “not poor” and “poor health”. Other variables included demographic characteristics, economic level, employment status, smoking and alcohol intake. Binary logistic regression was used to assess the association of self-perceived health with demographic and lifestyle factors.
Results:
Upon multivariate adjustment for all covariates in a backward stepwise elimination procedure, strong and significant “predictors” of poor self-perceived health status were older age (OR=3.0, 95%CI=2.4-3.7), unemployment (OR=5.6, 95%CI=4.0-7.8), male gender (OR=1.2, 95%CI=1.0-1.5), low education (OR=2.0, OR=1.3-3.0), current smoking (OR=1.7, 95%CI=1.2-2.4) and alcohol abstinence (OR=1.4, 95%CI=1.1-1.7).
Conclusions:
Our findings indicate that the low socioeconomic groups in Albania have a significantly lower self-perceived health status. Furthermore, smoking was a significant “determinant” of poor self-perceived health in this study population, which is compatible with previous reports from other countries.
Keywords: lifestyle factors, Living Standard Measurement Survey, self-perceived health, socio-demographic factors
1. INTRODUCTION
Since the World Health Organization defined health as “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity”, self-perceived health (SPH) is considered a suitable health indicator (1). SPH is based on a single item asking individuals to rate their health (3, 4). It is argued that SPH is a multidimensional concept though which is widely used as a health outcome measure (2). Furthermore, according to population-based studies, SPH has been recommended as a reliable factor to assess population health (5-7). Moreover, it is associated not only to mortality and morbidity, but also to socio-demographic and lifestyle factors (8). Several socio-demographic and lifestyle determinants of self-perceived health status have been documented in different populations (9-11). In addition, many studies have compared socio-demographic and lifestyle determinants of SPH among Western European countries (11-16), as well as between Western and East European countries (17, 18). These studies have shown that SPH determinants vary widely among different populations and countries. Despite the growing evidence on the consistent relationship between socio-demographic factors and SPH in Western and Central European countries, studies in Southeast European countries are rare. Furthermore, there are no studies determining the impact of socio-demographic and lifestyle factors on the SPH in Albania, a Southeast European country. Identifying SPH determinants could help policymakers in Albania and may provide evidence for health promotion in a country still in the process of transition.
Therefore, the aim of our study was to assess the socio-demographic and lifestyle correlates of self-perceived health status in a population-based sample of Albanian adult men and women.
2. METHODS
This study was based on data from Living Standard Measurement Survey (LSMS) in Albania conducted in September 2012 for a period of four weeks. LSMS is a multi-purpose survey conducted near households and one of the main sources of information to measure living conditions, income, level of education, access to health care perceived health, information on chronic diseases and fertility in order to ensure a necessary tool to help policymakers in monitoring and developing health and social programs.
The main objective of LSMS was to collect information for measuring the Albanian household’s welfare and to identify its related determinants. Welfare was measured by the consumption aggregate, providing information on the level and distribution of welfare in the country. LSMS makes possible assessment of health and social costs. The LSMS included a sample of 6671 households. The sample was chosen randomly by two rounds of selection. The sample was provided from the Population and Housing Census 2011. In order for the sample estimates from the 2012 Albania LSMS to be representative of the population, the data were multiplied by a sampling weight. The basic weight for each sample household was equal to the inverse of its probability of selection (calculated by multiplying the probabilities at each sampling stage). For the first time in Albania, the LSMS 2012 had a module dedicated to health. The health module comprised two parts: Part A–General health status containing 96 questions and the main objective was to assess the perceived health, the level of health care services and the financial effect of health services, and; Part B–Access to health care that contained 10 questions and the main objective was to assess the access to health care. In our study, we included all individuals aged ≥35 years (N=12554) pertinent to the sample of 6671 households. A detailed description of data collection procedures and questionnaires employed in this study can be found at: http://microdata.worldbank.org/index.php/catalog/1970/get_microdata/http://www.instat.gov.al/en/figures/micro-data.aspx The main outcome variable was the assessment of general self-perceived health. All study participants were asked the following question: “In general, how would you rate your health?” Participants rated their health in five categories: very good, good, average, poor and very poor, which in the analyses were dichotomized into “not poor” and “poor health”. Independent variables, based on a detailed literature review, included demographic characteristics, economic level, employment status, smoking and alcohol intake.
Sample estimates of socio-demographic characteristics, lifestyle factors and self-perceived health status were standardized with the respective strata of the overall Albanian population aged 35 years and above. Absolute numbers and their respective percentages from the study sample, and standardized (population-weighted) percentages with their respective 95% confidence intervals (95%CIs) were reported. Binary logistic regression was used to assess the association of self-perceived health with demographic and lifestyle factors. All variables were included in a backward stepwise elimination procedure with a p-value to exit set at >0.10. Odds ratios (poor health vs. not poor health status), their respective 95%CIs and p-values were calculated. All the logistic models were checked to comply with the requirements of Hosmer-Lemeshow goodness-of-fit test (all the reported models satisfied the goodness-of-fit criterion). SPSS (Statistical Package for Social Sciences, version 19.0) was used for all the statistical analyses.
3. RESULTS
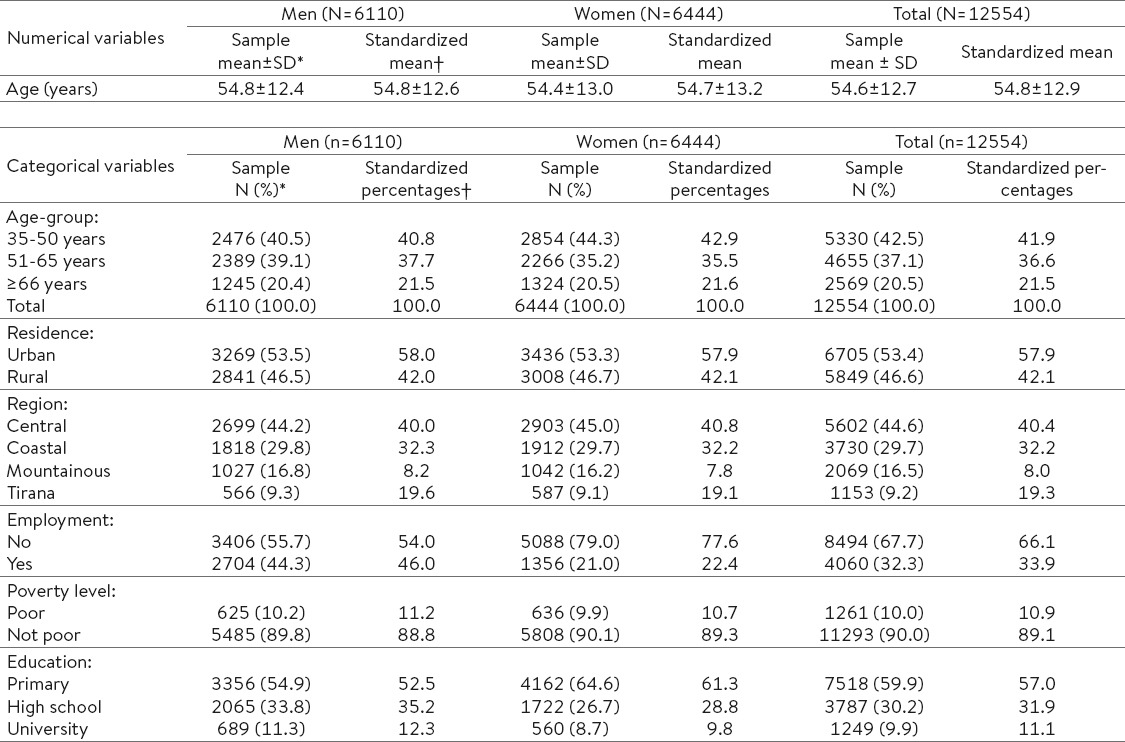
Table 1 presents the distribution of demographic and socioeconomic characteristics of male and female participants included in this study. Mean age of men and women was 54.8±12.4 years and 54.4±13.0 years, respectively. Overall, about 43% of the study sample was 35-50 years old, whereas the proportion of older people (66 years and older) was 21%. About 53% of participants were residing in urban areas and about 9% were based in Tirana, the capital of Albania. The employment level was considerably higher in men compared to women (44% vs. 21%, respectively). The overall prevalence of self-perceived poverty was 10%. Finally, about 11% of men and 9% of women had obtained a university degree (Table 1).
Table 1.
Socio-demographic characteristics of a population-based sample of adults in Albania, 2012 * Mean values (and their respective standard deviations) and absolute numbers (and their respective column percentages) in the actual study sample. †Population standardized (weighted) mean values and column percentages.
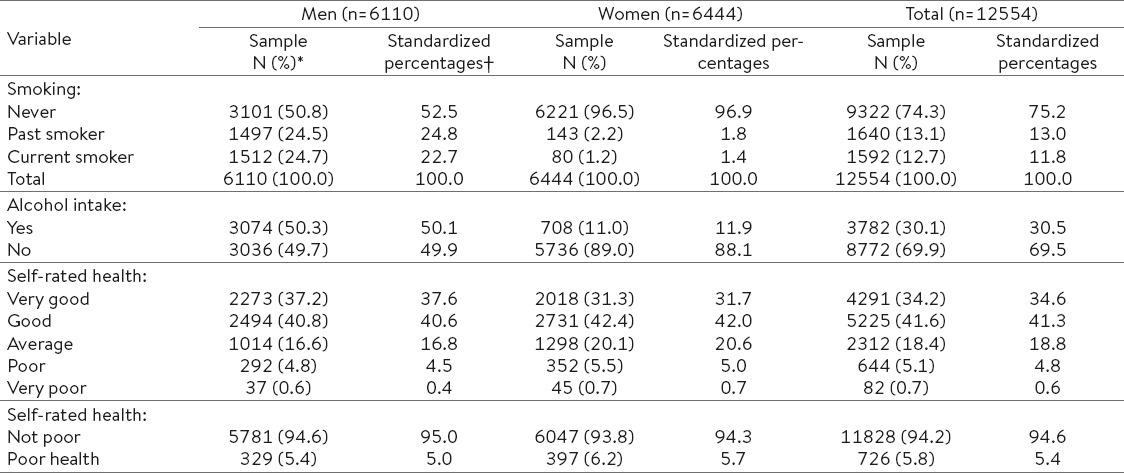
The prevalence of current smoking was 25% in men, but only 1% in women (Table 2). About 50% of men and 11% of women consumed alcohol. The prevalence of self-reported poor health was 4.8% in men and 5.5% in women, whereas very poor health was reported by only 37 men (0.6% of them) and 45 women (0.7%). On the other hand, 37% of men and 31% of women rated their health as very good (Table 2).
Table 2.
Lifestyle characteristics and self-perceived health status in a population-based sample of adult men and women in Albania, 2012 * Mean values (and their respective standard deviations) and absolute numbers (and their respective column percentages) in the actual study sample. †Population standardized (weighted) column percentages.
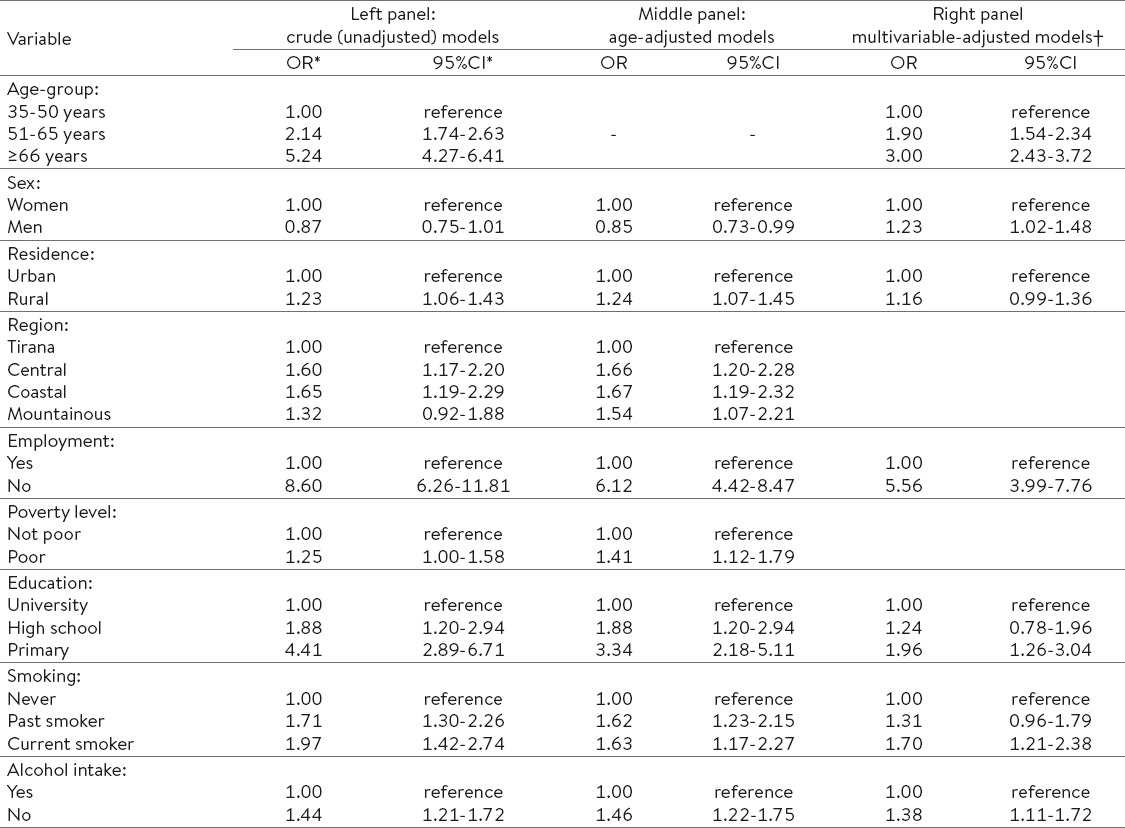
In crude (unadjusted) analysis (Table 3 – left panel), there was a strong graded positive association of age with self-perceived poor health [OR(51-65 years vs. 35-50 years)=2.1, 95%CI=1.7-2.6 and OR(≥66 years vs. 35-50 years)=5.2, 95%CI=4.3-6.4]. There was no significant relationship with sex, but a positive association with rural residence (OR=1.2, 95%CI=1.1-1.4). Tirana residents had the lowest odds of self-rated poor health. There was a very strong relationship of poor health with unemployment (OR=8.6, 95%CI=6.3-11.8), but less so with poverty level (OR=1.2, 95%CI=1.0-1.6). There was evidence of a graded association with educational attainment [OR(high school vs. university)=1.9, 95%CI=1.2-2.9 and OR(primary vs. university)=4.4, 95%CI=2.9-6.7]. Similarly, there was a graded relationship of poor health with smoking status [OR(past smokers vs. never smokers)=1.7, 95%CI=1.3-2.3 and OR(current smokers vs. never smokers)=2.0, 95%CI=1.4-2.7]. Furthermore, alcohol abstainers had a higher level of poor self-reported health (OR=1.4, 95%=1.2-1.7) [Table 3 – left panel]. Adjustment for age (Table 3 – middle panel) slightly attenuated the positive association of poor health with unemployment (OR=6.1, 95%CI=4.4-8.5) and low education (OR=3.3, 95%CI=2.2-5.1), but it accentuated the relationship with poverty level (OR=1.4, 95%CI=1.1-1.8). The association with current smoking was attenuated, whereas the relationship with alcohol consumption was not affected by age adjustment (Table 3 – middle panel). Upon multivariate adjustment for all covariates in a backward stepwise elimination procedure (Table 3 – right panel), strong and significant “predictors” of poor self-perceived health status were older age (OR(≥66 years vs. 35-50 years)=3.0, 95%CI=2.4-3.7), unemployment (OR=5.6, 95%CI=4.0-7.8), low education (OR=2.0, OR=1.3-3.0), current smoking (OR=1.7, 95%CI=1.2-2.4) and alcohol abstinence (OR=1.4, 95%CI=1.1-1.7). Interestingly, in multivariate-adjusted models, the association with sex changed direction, with males exhibiting a higher level of poor self-reported health compared to their female counterparts (OR=1.2, 95%CI=1.0-1.5) [Table 3 – right panel].
Table 3.
Association of self-perceived health status with socio-demographic characteristics and lifestyle factors; odds ratios from binary logistic regression * Odds ratios (OR: poor health vs. not poor health status) and 95% confidence intervals (95%CI) from binary logistic regression. † All variables were included in a backward stepwise elimination procedure with a p-value to exit set at >0.10. Empty cells refer to the variables excluded from the model.
4. DISCUSSION
To our knowledge, our study is one of the first reports informing about the association of different socio-demographic indicators (levels of education, self-rated economic status, employment status) and lifestyle factors (smoking and alcohol intake) with self-perceived health status in Albania population. We found that 10.2% of men and 9.9% of women perceived poor health and the overall prevalence of self-perceived poverty was 10% which is higher than those found in western population (15, 16). One possible explanation is that the socio-demographic and lifestyle determinants of SPH can vary in strength between countries. In the present study, strong and significant “predictors” of poor self-perceived health status in the Albanian population were older age, male gender, low education, unemployment, current smoking and alcohol abstinence. The relationship with the greatest magnitude was found for employment status. Compared to employed individuals, the unemployed had 5.6 times higher chances to assess their health status as poor after adjusting for other socio-demographic variables, smoking and alcohol intake. Our findings are generally consistent with those reported from previous studies (9, 11, 19). Limm et al. found that poor self-perceived health was more frequent among German long-term unemployed (9). Also, an earlier study in Serbia reported that employment status was strongly associated with self-perceived health (11). The association of employment status and health is be-directional: poor health is often considered as a barrier to employment or it can cause job loss; on the other hand, long-term unemployment can impair the mental health or can cause poorer health (19). According to the findings of the present study, low education was also strongly associated with poor self-perceived health. We found that both men and women with primary education had poorer self-rated health in fully-adjusted logistic regression models. These findings are consistent with results of cross-sectional studies from the neighboring countries (10, 11). Also, similar results were reported from other western and east countries (14, 20). The benefits of education on health may relate to the fact that higher education help people to improve the abilities for achieving life goals, asses a full time and well-paid job and employ a healthy lifestyle (21). Our study also demonstrates a close relationship between poor SPH and age and gender. In agreement with other studies, our findings confirmed that older age was linked with worse self perceived health (10, 22). On the other hand, some studies have shown no relationship between age and SPH levels (11, 23), whereas a study conducted in Spain found that people older than 50 years old are more likely to report better SPH (24). Gender effect on the self-perceived health has been shown in many previous studies and, in almost all of them, women have reported lower levels of SPH (10, 21, 25). Some studies though did not show any difference in SPH between men and women (14, 26). In contrast to the findings from previous studies, we found that men rated their health significantly poorer compared to women. A possible explanation for this finding may be driven by different use of tobacco and alcohol between males and females in our study. Our findings support the fact that males and females perceive their health differently and highlight the need to address health promotion messages for men and women separately, and according to age-groups, as well. Another insight provided in our study is the influence of lifestyle factors on SPH. In the present study, two such factors were evaluated: smoking and alcohol consumption. In our study, smoking has been found to be an important predictor of poor health. The evidence of relationship of smoking and SPH from cross-national studies is inconsistent. Some studies have shown that current smokers had the worst perceived health status (24, 27) in line with our findings, whereas some other studies have shown a non-significant impact of smoking on self-perceived health (10, 28), or have shown that smoking was strongly associated with good self-perceived health (11, 29). With regard to the alcohol consumption, good self-perceived health in alcohol abstainers confirms results of cross-national studies conducted in East or Mediterranean European countries (11, 24, 29). A possible explanation for our results may be related to the selection bias according to Bobak et al (29): people without illness and health problems smoke and drink while people with poor health do not. Also, in Albania, as well as in other Mediterranean countries, the alcohol consumption is more frequent during socialand leisureactivities that contribute to a betterSPH (24). However, these findings deserve further exploration in prospective studies. This is one of the first reports providing evidence on the socio-demographic and lifestyle determinants of SPH status in Albania after adjustment for a board range of possible confounders. Also, our research provides valuable baseline data to monitor future changes of health status in this transitional population. However, this study has some limitations related to its cross-sectional design and the lack of other important covariates such as physical activity and dietary assessment.
5. CONCLUSION
Our findings indicate that the low socioeconomic groups in Albania have a significantly lower self-perceived health status. Furthermore, smoking was a significant “determinant” of poor self-perceived health in this study population, which is compatible with previous reports from other countries.
Footnotes
• Conflict of interest: None declared.
REFERENCES
- 1.de Bruin A, Picavet HSJ, Nossikov A. Health interview surveys. Towards international harmonization of methods and instruments. WHO Reg Publ Eur Ser. 1996;58:i–xiii. 1-161. [PubMed] [Google Scholar]
- 2.Simon JG, De Boer JB, Joung1 IMA, Bosma H, Mackenbach JP. How is your health in general? A qualitative study on self-assessed health. European Journal of Public Health. 2005;15(2):200–8. doi: 10.1093/eurpub/cki102. [DOI] [PubMed] [Google Scholar]
- 3.Manderbacka K. Examining what self-rated health question is understood to mean by respondents. Scand J Soc Med. 1998;26:145–53. doi: 10.1177/14034948980260020301. [DOI] [PubMed] [Google Scholar]
- 4.Ame´lie Quesnel–Vallée. Self-rated health: caught in the crossfire of the quest for ‘true’ health? International Journal of Epidemiology. 2007;36:1161–4. doi: 10.1093/ije/dym236. [DOI] [PubMed] [Google Scholar]
- 5.Miilunpalo S, Vuori I, Oja P, Pasanen M, Urponen H. Self-rated health status as a health measure: the predictive value of self-reported health status on the use of physician services and on mortality in the working-age population. J Clin Epidemiol. 1997;50:517–28. doi: 10.1016/s0895-4356(97)00045-0. [DOI] [PubMed] [Google Scholar]
- 6.Pappa E, Niakas D. Assessment of health care needs and utilization in a mixed public-private system: The case of the Athens area. BMC Health Serv. Res. 2006;6:146. doi: 10.1186/1472-6963-6-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Latham K, Peek C.W. Self-rated health and morbidity onset among late midlife U.S. adults. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2013;68(1):107–16. doi: 10.1093/geronb/gbs104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Robine J-M, Jagger C, Egidi V. Selection of a coherent set of health indicators. Final draft. A first step towards a user’s guide to health expectancies for the European Union. Montpellier (France): Euro-REVES; 2000. Jun, [Google Scholar]
- 9.Limm H, Heinmüller M, Liel K, Seeger K, Gündel H, Kimil A, Angerer P. Factors associated with differences in perceived health among German long-term unemployed. BMC Public Health. 2012;12:485. doi: 10.1186/1471-2458-12-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Darviri C, Fouka G, Gnardellis C, Artemiadis K.A, Tigani X, Alexopoulos C.E. Determinants of Self-Rated Health in a Representative Sample of a Rural Population: A Cross-Sectional Study in Greece. Int. J. Environ. Res. Public Health. 2012;9:943–54. doi: 10.3390/ijerph9030943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Janković J, Janević T, von dem Knesebeck O. Socioeconomic inequalities, health damaging behavior, and self-perceived health in Serbia: a cross-sectional study. Croat Med J. 2012;53:254–62. doi: 10.3325/cmj.2012.53.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alvarez-Galvez J, Rodero-Cosano ML, Motrico E, Salinas-Perez JA, Garcia-Alonso C, Salvador-Carulla L. The impact of socio-economic status on self-rated health: study of 29 countries using European Social Surveys (2002–2008) Int J Environ Res Public Health. 2013;10:747–61. doi: 10.3390/ijerph10030747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eikemo TA, Huisman M, Bambra C, Kunst AE. Health inequalities according to educational level in different welfare regimes: a comparison of 23 European countries. Sociol Health Illn. 2008;30:565–82. doi: 10.1111/j.1467-9566.2007.01073.x. [DOI] [PubMed] [Google Scholar]
- 14.von dem Knesebeck O, Verde PE, Dragano N. Education and health in 22 European countries. Soc Sci Med. 2006;63:1344–51. doi: 10.1016/j.socscimed.2006.03.043. [DOI] [PubMed] [Google Scholar]
- 15.Gray L, Merlo J, Mindell J, Hallqvist J, Tafforeau J, O’Reilly D, et al. International differences in self-reported health measures in 33 major metropolitan areas in Europe European Journal of Public Health. 2012;22(1):40–7. doi: 10.1093/eurpub/ckq170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu Y, van Lenthe JF, Borsboom JG, Looman WNC, Bopp M, Burström B, et al. Trends in socioeconomic inequalities in self-assessed health in 17 European countries between 1990 and 2010. JECH Online First, published on January 19. 2016 doi: 10.1136/jech-2015-206780. 10.1136/jech-2015-206780. [DOI] [PubMed] [Google Scholar]
- 17.Per Carlson. Self-perceived health in East and West Europe: another european health divide. Soc. Sci. Med. 1998;46(10):1355–66. doi: 10.1016/s0277-9536(97)10093-4. [DOI] [PubMed] [Google Scholar]
- 18.Helasoja V, Lahelma E, Praättälä R, Patja K, Klumbiene J, Pudule I, et al. Determinants of daily smoking in Estonia, Latvia, Lithuania, and Finland in 1994–2002. Scandinavian Journal of Public Health. 2006;34:353–62. doi: 10.1080/14034940500414766. [DOI] [PubMed] [Google Scholar]
- 19.Artazcoz L, Benach J, Borrell C, Cortes I. Unemployment and mental health: Understanding the interactions among gender, family roles, and social class. Am J Public Health. 2004;94(1):82–8. doi: 10.2105/ajph.94.1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Monden CWS. Changing social variations in self-assessed health in times of transition? The Baltic States 1994–1999. Eur J Public Health. 2005;15:498–503. doi: 10.1093/eurpub/cki019. [DOI] [PubMed] [Google Scholar]
- 21.Cullati S, Rousseaux E, Gabadinho A, Courvoisier DS, Burton-Jeangros C. Factors of change and cumulative factors in self-rated health trajectories: A systematic review. Advances in Life Course Research. 2014;19:14–27. doi: 10.1016/j.alcr.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 22.Andersen F.K, Christensen K, Frederiksen H. Self-rated health and age: A cross-sectional and longitudinal study of 11,000 Danes aged 45–102. Scand J Public Health. 2007;35:164–71. doi: 10.1080/14034940600975674. [DOI] [PubMed] [Google Scholar]
- 23.Wang N, Iwasaki M, Otani T, Hayashi R, Miyazaki H, Xiao L, et al. Perceived health as related to income, socio-economic status, lifestyle, and social support factors in a middle-aged Japanese. Journal of Epidemiology. 2005;15(5):155–62. doi: 10.2188/jea.15.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Girón P. Determinants of self-rated health in Spain: differences by age groups for adults. European Journal of Public Health. 2012;22(1):36–40. doi: 10.1093/eurpub/ckq133. [DOI] [PubMed] [Google Scholar]
- 25.Crimmins EM, Kim JK, Solé-Auró A. Gender differences in health: Results from SHARE, ELSA and HRS. Eur J Public Health. 2011;21:81–91. doi: 10.1093/eurpub/ckq022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parna K, Ringmets I. Comparison of socioeconomic differences in self-perceived health in Estonia and Finland. Scand J Public Health. 2010;38:129–34. doi: 10.1177/1403494809357259. [DOI] [PubMed] [Google Scholar]
- 27.Ho SY, Lam TH, Fielding R, Janus ED. Smoking and perceived health in Hong Kong Chinese. Soc Sci Med. 2003 Nov;57(9):1761–70. doi: 10.1016/s0277-9536(03)00021-2. [DOI] [PubMed] [Google Scholar]
- 28.Gilmore ABC, McKee M, Rose R. Determinants of and inequalities in self-perceived health in Ukraine. Social Science & Medicine. 2002;55:2177–88. doi: 10.1016/s0277-9536(01)00361-6. [DOI] [PubMed] [Google Scholar]
- 29.Bobak M, Pikhart H, Hertzman C, Rose R, Marmot M. Socioeconomic factors, perceived control and self-reported health in Russia. A cross- sectional survey. Soc Sci Med. 1998;47(2):269–79. doi: 10.1016/s0277-9536(98)00095-1. [DOI] [PubMed] [Google Scholar]


