Abstract
Objective:
To provide a conceptual framework for managing diabetic patient care, and creating an information network for clinical research.
Background:
A wide range of information technology (IT) based interventions such as distance learning, diabetes registries, personal or electronic health record systems, clinical information systems, and clinical decision support systems have so far been used in supporting diabetic care. Previous studies demonstrated that IT could improve diabetes care at its different aspects. There is however no comprehensive conceptual framework that defines how different IT applications can support diverse aspects of this care. Therefore, a conceptual framework that combines different IT solutions into a wide information network for improving care processes and for research purposes is widely lacking. In this study we describe the theoretical underpin of a big project aiming at building a wide diabetic information network namely DIANET.
Research design and methods:
A literature review and a survey of national programs and existing regulations for diabetes management was conducted in order to define different aspects of diabetic care that should be supported by IT solutions. Both qualitative and quantitative research methods were used in this study. In addition to the results of a previous systematic literature review, two brainstorming and three expert panel sessions were conducted to identify requirements of a comprehensive information technology solution. Based on these inputs, the requirements for creating a diabetes information network were identified and used to create a questionnaire based on 9-point Likert scale. The questionnaire was finalized after removing some items based on calculated content validity ratio and content validity index coefficients. Cronbach’s alpha reliability coefficient was also calculated (αTotal= 0.98, P<0.05, CI=0.95). The final questionnaire was containing 45 items. It was sent to 13 clinicians at two diabetes clinics of endocrine and metabolism research institute in order to assess the necessity level of the requirements for diabetes information network conceptual framework. The questionnaires were returned by 10 clinicians. Each requirement item was labeled as essential, semi-essential, or non-essential based on the mean of its scores.
Results:
All requirement items were identified as essential or semi-essential. Thus, all of them were used to build the conceptual framework. The requirements were allocated into 11 groups each one representing a module in the conceptual framework. Each module was described separately.
Conclusion:
We proposed a conceptual framework for supporting diabetes care and research. Integrating different and heterogeneous clinical information systems of healthcare facilities and creating a comprehensive diabetics data warehouse for research purposes, would be possible by using the DIANET framework.
Keywords: Diabetes Mellitus, Diabetes information network, Clinical information system, Electronic health record, Personal health record
1. INTRODUCTION
Diabetes mellitus is a pervasive chronic disease and a leading cause of death due to increased risk of coronary artery disease and stroke. However most of those cases would be preventable (1, 2).
Several information technology (IT) based interventions were applied to enhance blood glucose monitoring, promote clinical outcomes and diabetes management. Previous evidence demonstrated that IT can improve diabetes management through better metabolic control and help in the global care of diabetic peoples (3-5). Our previously performed systematic review showed that information technology based interventions have led to better management of diabetes with different effect of intervention on various clinical findings (6). While in most previous studies, use of one specific intervention has been reviewed or proposed; we know that use of heterogeneous and diverse clinical information systems is pervasive in diabetic care facilities. It is noteworthy that diabetic patients need multidisciplinary care offered by different medical specialty, located in different places, and using different IT systems with different data models. This problem makes it very difficult to create a nation-wide integrated diabetics database for research purposes.
A successful diabetes information network should efficiently cover and integrate all needed dimension diabetic management such as screening and registration, patient empowerment, good clinical findings documentation, interoperability and information exchange between heterogeneous point of care systems, research, and analytical processing at national, regional, and local levels. Thus, a comprehensive framework for developing diabetes information network and solving mentioned issues, is needed.
There is however no comprehensive conceptual framework that defines how different IT applications can support diverse aspects of diabetic care. Therefore, a conceptual framework that combines different IT solutions into a wide information network for improving care processes and for research purposes is widely lacking. In this article, a conceptual framework for managing diabetes mellitus, which includes the combination of several IT based interventions, was proposed.
The authors described the architecture of a wide information network, namely DIANET that meets the requirements for better diabetes management, promoted diabetes care, and advanced population-wide research. The DIANET framework will support national and regional programs for management of diabetes mellitus and developing related researches.
2. BACKGROUND
A wide variety of information technology based interventions are currently executed in diabetic care environment. Adaji et al. performed a literature review about the use of information technology to enhance diabetes management. They demonstrated that promoting a good interaction between patient and healthcare provider by using information technology based interventions can lead to improve diabetes care (7).
Distance learning is another type of intervention. According to Lau et al.’s study, providing medical education for diabetic patients and increasing their knowledge and self-care capacities were associated with better clinical outcomes and improved diabetes management (8). In this context, distance learning can be associated with better health and patient satisfaction and acceptance (9-11).
Creating diabetics registration system was one of another activities in this field. Disease registries have been shown to be important components of health care management (12). Previously, several efforts have been done to create diabetes registration systems (13, 14). However, none of the currently available diabetic registries have used an integrated and holistic approach.
Reed et al. demonstrated that use of an electronic health record was associated with improvements in diabetes care and clinical outcomes such as HbA1C and LDL levels in diabetic patients especially in poorly controlled cases. Furthermore, other studies have presented similar results (15-17).
The CDSS-based diabetes care was reportedly achieved better glycemic control with less hypoglycemia than routine care, and might provide effective and safe diabetes management in elderly patients (18, 19). However different results were reported in previous studies of diabetes decision support intervention targeted at both providers and patients (20-24).
As noted by research guidance group, the number of mobile health applications has more than doubled in only 2.5 years to reach more than 100,000 applications in 2014. Patients with chronic health conditions are one of the main target groups in mobile health domain. In this area diabetes has the highest business potential and remote monitoring and consultation applications have the highest expected market potential in the near future (25). Also previous studies have demonstrated that mobile health technology could help patients to manage their diabetes and related conditions and make important life style changes (26-29).
A number of telephone-based interventions in diabetic population have been performed in the world. Some of these studies demonstrated a positive effect on reducing HbA1c levels, blood pressure, LDL levels, BMI and other outcomes in people with diabetes (30-34).
The main focus of this research was to propose of conceptual framework for use of information technology in monitoring and management of diabetes in patients and developing a wide information network for clinical researches.
3. RESEARCH DESIGN AND METHODS
At first, in order to problem statement, a literature review and a survey of national programs and regulations for diabetes management were done. Since a systematic review was conducted by authors in previous study (6), the result of this study was used as available evidence.
Requirement analysis
In order to identify requirements, we used brainstorming, and expert panel sessions. Ten persons, including one manager and two officers at diabetes office of Ministry of health, three researchers at national diabetes research network, and one manager and three general practitioners at Diabetes clinic in endocrinology & metabolism research institute participated in two brainstorming sessions. Through the brainstorming sessions, we stated the problem and developed 42 detailed concepts within eight categories.
With these concepts, we conducted three expert panel sessions. Seven expert panelists were invited to participate according to their publications, knowledge and experience, and identification as endocrinologists who had managed more than 500 cases. Experts were allowed to discuss, comment, and advise on each identified concept or propose new ones through the session. Thereupon ten items were changed, remove or added as a result of these sessions.
Based on these various inputs include the results of previous systematic review, literature review, document analysis and expert panel sessions, the requirements of diabetes information network were identified. The initial item pool was further reduced to contain only items that were clear and not redundant. Thereupon 51 items within the twelve categories were listed. We used these items to create the requirements of diabetes information network questionnaire for assessing the necessity level of the items. The resulting questionnaire was consisted of 51 items, and responses to each item were based on a nine-point Likert scale ranging from strongly agree to strongly disagree.
In order to validity measurement, content validity ratio coefficient was calculated for each item. The expert panel was consisted of 10 specialists in diabetic care domain. Qualitative content validity was determined based on ‘grammar’, ‘wording’, ‘item allocation’, and ‘scaling’ indices. All items were checked and the expert panel’s recommendations were inserted into the questionnaire. Content validity ratio (CVR) and Content Validity Index (CVI) were calculated in order to perform quantitative content validity. For calculating CVR, the expert panel of was asked to evaluate each item using a 3-point Likert scale: 1 = essential, 2 = useful but not essential and 3 = unessential. Then, according to Lawshe’s table (35), items with CVR score of 0.62 or above were selected (n=45). After removing 6 rejected items, the calculated CVI was greater than 0.8 and considered satisfactory. (CVI=0.98) Finally, 45 items within eleven categories were remained in the questionnaire.
Then, Cronbach’s alpha reliability coefficient was calculated on the standardized scores for each category and total scale to measure internal consistency. The calculated Cronbach’s alpha coefficient for all categories was greater than 0.7 and considered satisfactory (αTotal= 0.98, P<0.05, CI=0.95). All statistical analyses were performed using the IBM SPSS version 20.
The final 45-item questionnaire with a 9-point Likert scale was sent to all clinicians (n=13) at two diabetes clinics in endocrine and metabolism research institute in order to the needs assessment for proposing diabetes information network conceptual framework. Figure 1 shows the order of the methods and the result of them.
Figure 1.
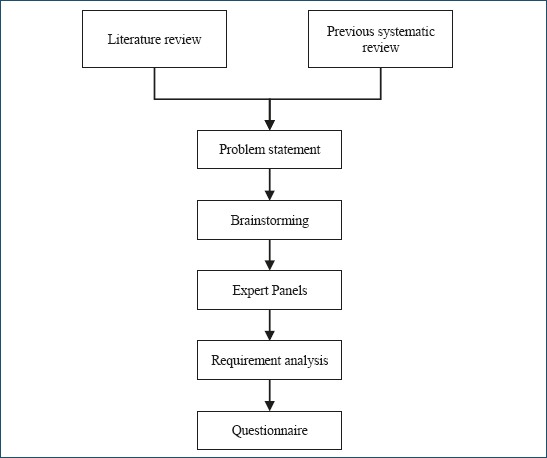
The order of the methods
4. RESULTS
The questionnaire was returned by 10 clinicians. The percentage of missing value was low for all items and ranged from zero (n=35) to 30% (n=1). Each item was placed in one of the following groups based on the mean of item scores: essential (8 ≤ m ≤ 10), semi-essential (6 ≤ m < 8) and non-essential (m < 6).
Table 1 shows the summary of data analysis result for each category. Also, the supplementary file contains the result of data analysis in more details.
Table 1.
Summary of requirement analysis result. * SD = Standard deviation
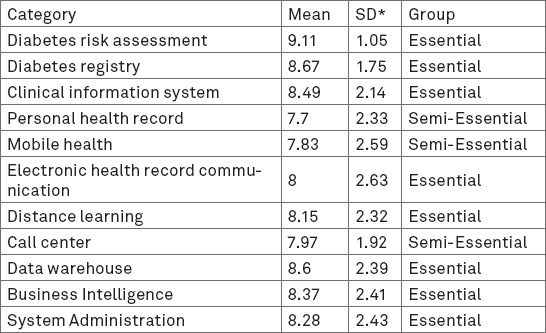
The calculated total mean for all items was 8.33 and the standard deviation of all categories was equal to 0.42. No category was defined as non-essential and all categories were placed in essential and semi-essential groups.
The obtained results was shown that all identified requirements in all categories were important. Thus, we used all of them to design the final conceptual framework.
Conceptual framework of diabetes information network
This section presents the new conceptual framework that was developed following the problem and requirement analysis. To better understand the issue, we presented a graphical conceptual framework that depicts how the above mentioned concepts are organized around the diabetic care (Figure 2).
Figure 2.
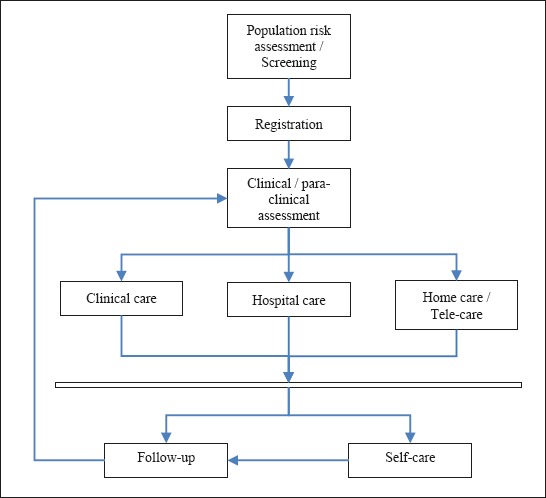
Diabetic care components
Overall architecture
The information network consists of integrated applications, core modules and services, and related databases. Integrated applications include and are not limited to DIANET integrated portal for accessing patients and providers to information and services, also mobile applications, research specific applications, management information systems, and many different clinical information systems.
Risk assessment, diabetes registry, diabetes clinical information system with decision support, personal health record, mobile health, electronic health record communication, distance learning, call center, diabetic patients’ data warehouse and business intelligence, and system administration are core modules and services of the final framework.
Databases were designed to define and store basic data such as terminologies, master patient index data, diabetes registration data, clinical information, and multidimensional data as an integrated data warehouse.
Figure 3 shows the overview of DIANET architecture and its components. Each components was formulated and designed based on available literatures obtained from our previous study. Core modules and services have explained in the next section.
Figure 3.
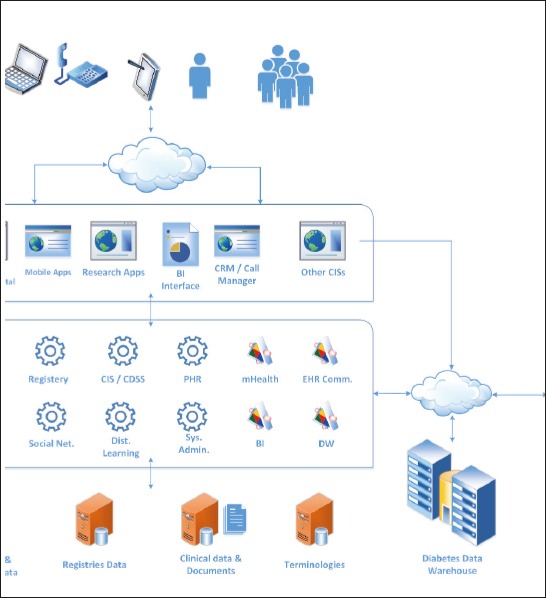
DIANET architecture overview
Core modules of DIANET framework
Risk assessment
The aim of this module is to identify diabetic or pre-diabetic patients and invite them in order to register and receive diabetes care.
In comparison to the previous efforts, this web-based tool provides a simple, self-administered, user-friendly, method to identify persons at high risk of type 2 diabetes who might benefit from interventions to prevent or delay its onset. To maximize ease of use, it uses only information commonly known to the general population. In this regard we applied self-assessment diabetes screening score proposed by Band et al. (36) and currently being used in American Diabetes Association (ADA) website as a major source guide the care of people with diabetes (http://www.diabetes.org/assets/pdfs/at-risk/risk-test-paper-version.pdf).
For maximizing the number of people to register and use this module of the network, they should be encouraged through supporting policy and public campaigns.
Diabetes registry
The aim of this module is to register diabetic or pre-diabetic patients for prevention and therapeutic programs. It also provides a facility for research purposes and better planning for diabetes management.
The diabetes registry module collects core clinical and laboratory data on patients with type I, type II or gestational diabetes or in pre-diabetic stages. This module is fully integrated to other components such as clinical information system with decision support and personal health record.
This module could be used by receptionist at diabetes clinics or patients in self-reporting format. It is noticeable that in the case of self-reporting mode, providing primary visit and setting up a consultation session at diabetes clinic to verify information and proof patient status will be necessary. For this purpose, the module suggests a list of the nearest diabetes clinics after registration, so that the patients may select the ideal clinic for receiving diabetes care.
Diabetes clinical information system with decision support
This module provides the ability to view complete patient’s chronic care records for physicians and other related clinicians (rule-based access) at the point of care. Also a summary of patient’s status including several charts such as HbA1C level, blood pressure, and lipid profile along the time are generated automatically by this module.
In order to reduce medical errors and increase adherence to guidelines, a decision support component is developed based on diabetes care clinical guidelines. This component actively suggests any decision that is needed during diagnosis or treatment processes. Healthcare providers are authorized to accept or reject the suggestions made by the system.
This component also was integrated in personal health record module in order to increase diabetic patient’s knowledge and their empowerment. In this case, the CDSS component provides some recommendations for better home-care according to the data registered in the personal health record module.
Personal health record
Personal health record module is a web-based tool which provides patients with Online access to their health information. The primary purpose of creating this module was to facilitate recording homecare activities and increase the rate of patients’ involvement in their diabetes care. Providing alerts and reminders for the registered patients and managing risk factors are other objectives of this module.
Personal health record module is integrated to the clinical information system. This integration enables clinicians to have access to all data recorded during home-care.
Mobile health
This module consists of two main components each one residing in server-side or client-side. Server-side component provides the ability of communication between mobile devices and DIANET modules such as personal health record, clinical information system, and call center. It also can send short message texts to patients, healthcare providers, and researchers following the events occurred in DIANET environment. These messages may be sent as reminders for appointments, performing essential periodic laboratory tests, and using drugs, or as alarms for the need to follow-up, and so on.
Client-side component is a set of mobile smartphone applications that facilitates access to the patient’s data available in personal health record or clinical information system modules. This component provides electronic healthcare services such as reminders, alerts, diaries and monitoring tools, information delivery on diabetes prevention and awareness raising, calculators and nutrition support. It also can communicate with other devices (e.g. glucometers) for sending data to PHR through mobile gateway. It is recommended that these mobile applications would be developed on Android or iOS platforms. Because Android and iOS are the dominant platforms in mobile health field (25).
Since problems with the Internet connection were reported as system breakdown, the client-side component can play the role of an offline-application, store patient’s data and send information to DIANET infrastructure when Internet connectivity becomes available.
Electronic health record communication
The SEPAS (an abbreviation of Iranian electronic health record system in Persian language meaning “Thanks”) project supported by ministry of health is the greatest information technology project in health sector in Iran. SEPAS was developed based on ISO 13606 standard and OpenEHR framework in order to collect and integrate data from point of care information systems and provide an interoperable environment.
Since in Iran diabetic patients don’t usually refer to a specific clinic or hospital and because many different information systems are in use in healthcare facilities, a major problem appeared here. Data of diabetic patients and their care is distributed on local and regional health information systems and data aggregation into an integrated health information network for providing a national database becomes very hard.
We consider a solution for solving this important issue. Most of applications used to provide care for patients throughout the country are either integrated or are going to be integrated into SEPAS. The EHR communication module could communicate to SEPAS for sending and receiving diabetic patients’ data. By using this solution, there will be no necessity to communicate with diverse information systems that applied to collect diabetic patients’ data. Yet still, using national and international standards for data registration and meeting requirements for interoperable communication remain as a challenge at the level of healthcare facilities.
Distance learning
This module produces the ability to provide virtual courses and group learning for diabetic patients and peoples at risk of diabetes. Healthcare providers prepare learning content in various media formats. These real-time and non-real-time courses can be accessible for patients through the distance learning module.
Call center
This module provides the ability for patients to contact with consultant physicians at the call center. It also provides the ability for healthcare providers to call patients and follow up patients’ health status. The information exchanged through this channel, could be recorded and integrated into electronic patient record by using suitable customer relationship management (CRM) and call manager solutions.
Diabetic patients’ data warehouse and business intelligence
In order to aggregate and integrate diabetes data, this module extracts and transforms data from different data sources and prepares data for analytical processing. The business intelligence module, then, prepares data for visualization. Other stakeholders such as managers, policy makers and researchers also benefit from the result of this module.
System administration
This module helps with the defining basic tables, terminologies, different users and their roles. It provides administrative tools such as logging and auditing tools and establishing systemic features such as single-sign on. Also other non-functional requirements such as performance and security issues were considered in this section.
5. DISCUSSION
We described a new framework for developing a wide information network for managing diabetes mellitus and improving diabetes care in comparison to the current isolated information technology based tools that have had limited impact on improving diabetes care (37-39).
As discussed in Pollard et al.’s study, a basic electronic registry assisted in improving care practices and clinical outcomes for patients with diabetes (40). Electronic health record data can also be valuable for improving identification and treatment of diabetic and pre-diabetic patients (41).
Some of diabetes decision support interventions that were not delivered at the point of care, had been associated with negative findings and no effects on patient’s clinical outcomes. These negative findings highlight the importance of delivering decision support interventions that are both timely and actionable (20).
According to Sarkar et al.’s study, persons who utilized patient portal managed their risk factors more effectively than those who did not (42). Also previous studies have shown that the use of patient portals leads to improved clinical outcomes for diabetic patients (42-44, 8).
As demonstrated by Weingarten et al. performance feedback to healthcare providers can improve medical practice (45-46).
There are various studies about information technology based intervention in diabetes management with different results and diverse impacts on clinical outcomes. The following items are the strengths of our presented conceptual framework called DIANET compared with single or combined interventions that presented in previous studies:
Using the results of previous systematic review that has been conducted by authors, and performing a good requirement analysis provided credible evidences.
Combining multiple information technology based interventions and creating a national information network to achieve better results in diabetes care and facilitate clinical researches is a unique property of described framework.
Integration with the personal health record was a missing element in many applications. We considered this important issue in DIANET framework designing.
Personalized education could be done using distance learning module in relation to the clinical information existed in the network.
Integrating clinical information systems into the new technologies such as mobile smart phone applications, and electronic health record is another strong point.
There will be no problem for using different regional clinical information systems in diabetes clinics over the country. Integrating to the national electronic health record system (SEPAS) establishes an infrastructure for accessing past and current medical record of diabetic patients by healthcare providers.
We desire using mobile health, call center and personal health record modules together will significantly increase patient-provider and patient-patient relationship in diabetes care.
DIANET provides an ability to run further clinical researches in a wide information environment will lead to promote healthcare services.
We define clinical decision support module for increasing guideline adherence. As noted by Sáenz et al. matching technology with treatment decisions can help providers to optimize the patient’s clinical outcomes (47).
Studying the effect of DIANET components and services on clinical outcomes in registered diabetic patients and running related clinical trials would be the suggested future program. The evaluation of the cost-effectiveness of DIANET implementation and its limitation should also be addressed.
6. CONCLUSION
In this paper, we proposed a conceptual framework of diabetes information network for managing diabetes mellitus, and creating an infrastructure for clinical research. Based on the results of requirement analysis, the framework consists of multiple integrated modules and combines some information technology based interventions.
In this regard, integrating many heterogeneous clinical information systems in healthcare facilities and creating a comprehensive diabetics data warehouse for research purposes may be possible by using the presented framework.
Our next step and future direction is to develop some parts of presented framework as initial prototypes and validate them in a driving context.
Acknowledgment
We gratefully acknowledge the helpful contribution of Dr. Habibollah Pirnejad in reviewing this manuscript and providing valuable comments.
Footnotes
• Conflicts of interest: The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest in the subject matter or materials discussed in this manuscript.
REFERENCES
- 1.Cho HN, Whiting D, Guariguata L, Montoya PA, Forouhi N, Hambleton I, et al. IDF Diabetes Atlas. 6th ed. International Diabetes Federation; 2013. [Google Scholar]
- 2.Baghbanian A, Tol A. The introduction of self-management in Type 2 Diabtes care:A narrative review. J Educ Health Promot. 2012;1:35. doi: 10.4103/2277-9531.102048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pradeepa R, Prabu AV, Jebarani S, Subhashini S, Mohan V. Use of a Large Diabetes Electronic Medical Record System in India:Clinical and Research Applications. J Diabetes Sci Technol. 2011;5(3):543–52. doi: 10.1177/193229681100500309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Holtz B, Lauckner C. Diabetes Management via Mobile Phones:A Systematic Review. TELEMEDICINE and e-HEALTH. 2012;18(3):175–84. doi: 10.1089/tmj.2011.0119. [DOI] [PubMed] [Google Scholar]
- 5.Polisena J, Tran K, Climon K, Hutton B, McGill S, Palmer K. Home telehealth for diabetes management:a systematic review and meta-analysis. Diabetes, Obesity and Metabolism. 2009;11:913–30. doi: 10.1111/j.1463-1326.2009.01057.x. [DOI] [PubMed] [Google Scholar]
- 6.Riazi H, Larijani B, Langarizadeh M, Shahmoradi L. Managing diabetes mellitus using information technology:a systematic review. Journal of Diabetes & Metabolic Disorders. 2015;14:49. doi: 10.1186/s40200-015-0174-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adaji A, Schattner P, Jones K. The use of information technology to enhance diabetes management in primary care:a literature review. Informatics Primary Care. 2008;16:229–37. doi: 10.14236/jhi.v16i3.698. [DOI] [PubMed] [Google Scholar]
- 8.Lau M, Campbell H, Tang T, Thompson DJS, Elliott T. Impact of Patient Use of an Online Patient Portal on Diabetes Outcomes. Canadian journal of Diabetes. 2014;38(1):17–21. doi: 10.1016/j.jcjd.2013.10.005. doi:http://dx.doi.org/10.1016/j.jcjd.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 9.Moattari M, Hashemi M, Dabbaghmanesh MH. The impact of electronic education on metabolic control indicators in patients with diabetes who need insulin:a randomised clinical control trial. Journal of Clinical Nursing. 2012;22:32–8. doi: 10.1111/j.1365-2702.2012.04200.x. doi:10.1111/j.1365-2702.2012.04200.x. [DOI] [PubMed] [Google Scholar]
- 10.Kearns JW, Bowerman D, Kemmis K, Izquierdo RE, Wade M, Weinstock RS. Group Diabetes Education Administered Through Telemedicine:Tools Used and Lessons Learned. TELEMEDICINE and e-HEALTH. 2012 Jun;18(5):347–53. doi: 10.1089/tmj.2011.0165. doi:10.1089/tmj.2011.0165. [DOI] [PubMed] [Google Scholar]
- 11.Jennings A, Powell J, Armstrong N, Sturt J. A Virtual Clinic for Diabetes Self-Management:Pilot Study. J Med Internet Res. 2009;11(1):e10. doi: 10.2196/jmir.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Griffin SJ, Kinmouth AL. Systems for Routine Surveillance for People With Diabetes Mellitus. Cochrane Database of Systematic Reviews. 2009 doi: 10.1002/14651858.CD000541.pub2. doi:10.1002/14651858.CD000541.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Russell KG, Rosenzweig J. Improving outcomes for patients with diabetes using Joslin Diabetes Center’s Registry and Risk Stratification system. J Health Inf Manag. 2007:26–3. [PubMed] [Google Scholar]
- 14.Al-Rubeaan KA, Youssef AM, Subhani SN, Ahmad NA, Al-Sharqawi AH, Ibrahim HM. A Web-Based Interactive Diabetes Registry for Health Care Management and Planning in Saudi Arabia. J Med Internet Res. 2013 Sep;15(9):e202. doi: 10.2196/jmir.2722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Reed M, Huang J, Graetz I, Brand R, Hsu J, Fireman B, et al. Outpatient electronic health records and the clinical care and outcomes of patients with diabetes mellitus. Ann Intern Med. 2012;157:482–9. doi: 10.7326/0003-4819-157-7-201210020-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Herrin J, da Graca B, Nicewander D, Fullerton C, Aponte P, Stanek G, et al. The Effectiveness of Implementing an Electronic Health Record on Diabetes Care and Outcomes. Health Services Research. 2010;47(4):1522–40. doi: 10.1111/j.1475-6773.2011.01370.x. doi:10.1111/j.1475-6773.2011.01370.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cebul RD, Love TE, Jain AK, Hebert CJ. Electronic Health Records and Quality of Diabetes Care. N Engl J Med. 2011;365:825–33. doi: 10.1056/NEJMsa1102519. [DOI] [PubMed] [Google Scholar]
- 18.Lim S, Kang SM, Shin H, Lee HJ, Won Yoon J, Yu SH, et al. Improved glycemic control without hypoglycemia in elderly diabetic patients using the ubiquitous healthcare service, a new medical information system. Diabetes Care. 2011;34:308–13. doi: 10.2337/dc10-1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fogel SL, Baker CC. Effects of Computerized Decision Support Systems on Blood Glucose Regulation in Critically Ill Surgical Patients, Computer Decision Support and Blood Glucose. 2013;216(4):828–33. doi: 10.1016/j.jamcollsurg.2012.12.015. [DOI] [PubMed] [Google Scholar]
- 20.MacLean CD, Gagnon M, Callas P, Littenberg B. The Vermont Diabetes Information System:A Cluster Randomized Trial of a Population Based Decision Support System. J Gen Intern Med. 2009;24(12):1303–10. doi: 10.1007/s11606-009-1147-x. doi:10.1007/s11606-009-1147-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peterson KA, Radosevich DM, O’Connor PJ, Nyman JA, Prineas RJ, Smith SA, et al. Improving diabetes care in practice:findings from the TRANSLATE trial. Diabetes Care. 2008;31(12):2238–43. doi: 10.2337/dc08-2034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cleveringa FGW, Gorter KJ, van den Donk M, Rutten GE. Combined task delegation, computerized decision support, and feedback improve cardiovascular risk for type 2 diabetic patients:a cluster randomized trial in primary care. Diabetes Care. 2008;31(12):2273–5. doi: 10.2337/dc08-0312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grant RW, Cagliero E, Sullivan CM, Dubey AK, Estey GA, Weil EM, et al. A controlled trial of population management:diabetes mellitus:putting evidence into practice (DM-PEP) Diabetes Care. 2004;27(10):2299–305. doi: 10.2337/diacare.27.10.2299. [DOI] [PubMed] [Google Scholar]
- 24.Glasgow RE, Nutting PA, King DK, Nelson CC, Cutter G, Gaglio B, et al. Randomized effectiveness trial of a computer-assisted intervention to improve diabetes care. Diabetes Care. 2005;28(1):33–9. doi: 10.2337/diacare.28.1.33. [DOI] [PubMed] [Google Scholar]
- 25.mHealth App Developer Economics. 2014:The State of the Art of mHealth App Publishing research2guidance. 2014. [Accessed December 2014]. www.mHealthEconomics.com .
- 26.Sieverdes JC, Treiber F, Jenkins C. Improving Diabetes Management With Mobile Health Technology. Am J Med Sci. 2013;345(4):289–95. doi: 10.1097/MAJ.0b013e3182896cee. [DOI] [PubMed] [Google Scholar]
- 27.Nes AA, van Dulmen S, Eide E, Finset A, Kristjánsdóttir OB, Steen IS, et al. The development and feasibility of a web-based intervention with diaries and situational feedback via smartphone to support self-management in patients with diabetes type 2. Diabetes research and clinical practice. 2012;97(2012):385–93. doi: 10.1016/j.diabres.2012.04.019. [DOI] [PubMed] [Google Scholar]
- 28.Mulvaney SA, Anders S, Smith AK, Pittel EJ, Johnson KB. A pilot test of a tailored mobile and web-based diabetes messaging system for adolescents. Journal of Telemedicine and Telecare. 2012;18:115–18. doi: 10.1258/jtt.2011.111006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Faridi Z, Liberti L, Shuval K, Northrup V, Ali A, Katz DL. Evaluating the impact of mobile telephone technology on type 2 diabetic patients’ self-management:the NICHE pilot study. Journal of Evaluation in Clinical Practice. 2008;14(2008):465–9. doi: 10.1111/j.1365-2753.2007.00881.x. [DOI] [PubMed] [Google Scholar]
- 30.Jordan RE, Lancashire RJ, Adab P. An evaluation of Birmingham Own Health®telephone care management service among patients with poorly controlled diabetes. a retrospective comparison with the General Practice Research Database. BMC Public Health. 2011;11:707. doi: 10.1186/1471-2458-11-707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fischer HH, Eisert SL, Everhart RM, Durfee MJ, Moore SL, Soria S, et al. Nurse-Run, Telephone-Based Outreach to Improve Lipids in People with Diabetes. Am J Manag Care. 2012;18(2):77–84. [PubMed] [Google Scholar]
- 32.Ferrara A, Hedderson MM, Ching J, Kim C, Peng T, Crites YM. Referral to telephonic nurse management improves outcomes in women with gestational diabetes. Am J Obstet Gynecol. 2012 Jun;206(6):491.e1–491.e5. doi: 10.1016/j.ajog.2012.04.019. doi:10.1016/j.ajog.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Graziano JA, Gross CR. A Randomized Controlled Trial of an Automated Telephone Intervention to Improve Glycemic Control in Type 2 Diabetes. Advances in Nursing Science. 2009;32(3):E42–E57. doi: 10.1097/ANS.0b013e3181b117a9. [DOI] [PubMed] [Google Scholar]
- 34.Orr PM, McGinnis MA, Hudson LR, Coberley SS, Crawford A, Clarke JL, et al. A Focused Telephonic Nursing Intervention Delivers Improved Adherence to A1c Testing. Disease management. 2006;9(5):277–83. doi: 10.1089/dis.2006.9.277. [DOI] [PubMed] [Google Scholar]
- 35.Lawshe CH. A quantitative approach to content validity. Personnel Psych. 1975;28:563–75. [Google Scholar]
- 36.Bang H, Edwards AM, Bomback AS, Ballantyne CM, Brillon D, Callahan MA, et al. Development and Validation of a Patient Self-assessment Score for Diabetes Risk. Ann Intern Med. 2009;151:775–83. doi: 10.1059/0003-4819-151-11-200912010-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Linder JA, Ma J, Bates DW, Middleton B, Stafford RS. Electronic health record use and the quality of ambulatory care in the United States. Arch Intern Med. 2007;167(13):1400–5. doi: 10.1001/archinte.167.13.1400. [DOI] [PubMed] [Google Scholar]
- 38.Jackson CL, Bolen S, Brancati FL, Batts-Turner ML, Gary TL. A systematic review of interactive computer-assisted technology in diabetes care. J Gen Intern Med. 2006;21(2):105–110. doi: 10.1111/j.1525-1497.2005.00310.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Garg AX, Adhikari NK, McDonald H, Rosas-Arellano MP, Devereaux PJ, Beyene J, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes:a systematic review. JAMA. 2005;293(10):1223–38. doi: 10.1001/jama.293.10.1223. [DOI] [PubMed] [Google Scholar]
- 40.Pollard C, Bailey KA, Petitte T, Baus A, Swim M, Hendryx M. Electronic Patient Registries Improve Diabetes Care and Clinical Outcomes in Rural Community Health Centers. The journal of rural health. 2009;25(1):77–84. doi: 10.1111/j.1748-0361.2009.00202.x. [DOI] [PubMed] [Google Scholar]
- 41.Schmittdiel JA, Adams SR, Segal J, Griffin MR, Roumie CL, Ohnsorg K, et al. Novel Use and Utility of Integrated Electronic Health Records to Assess Rates of Prediabetes Recognition and Treatment:Brief Report From an Integrated Electronic Health Records Pilot Study. Diabetes Care. 2014;37(2014):565–8. doi: 10.2337/dc13-1223. doi:10.2337/dc13-1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sarkar U, Karter AJ, Liu JY, Adler NE, Nguyen R, López A, Schillinger D. Social disparities in internet patient portal use in diabetes:evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;18:318e21. doi: 10.1136/jamia.2010.006015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.McMahon GT, Gomes HE, Hickson Hohne S, Hu TM, Levine BA, Conlin PR. Web-based Care Management in Patients with Poorly Controlled Diabetes Mellitus. Diabetes Care. 2005;28(7):1624–9. doi: 10.2337/diacare.28.7.1624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tenforde M, Nowacki A, Jain A, Hickner J. The Association Between Personal Health Record Use and Diabetes Quality Measures. J Gen Intern Med. 2011;27(4):420–4. doi: 10.1007/s11606-011-1889-0. doi:10.1007/s11606-011-1889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback:effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2012 Jun 13;:6–CD000259. doi: 10.1002/14651858.CD000259.pub3. doi:10.1002/14651858.CD000259.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Weingarten S, Henning JM, Badamgarav E, Knight K, Hasselblad V, Gano A, Jr, et al. Interventions used in disease management programmes for patients with chronic illness-which ones work? meta-analysis of published reports. BMJ. 2002;325:925–42. doi: 10.1136/bmj.325.7370.925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sáenz A, Brito M, Morón I, Torralba A, García-Sanz E, Redondo J. Development and Validation of a Computer Application to Aid the Physician’s Decision-Making Process at the Start of and during Treatment with Insulin in Type 2 Diabetes:A Randomized and Controlled Trial. Journal of Diabetes Science and Technology. 2012;6(3):581–8. doi: 10.1177/193229681200600313. [DOI] [PMC free article] [PubMed] [Google Scholar]


