Abstract
Purpose:
The main aim of this study is to investigate the occurrence and severity of FSD in women working in tertiary hospitals.
Material and methods:
The study sample was drawn from health care women between the ages of 20 and 65 years, working in two hospitals in Greece. This descriptive study used a structured Greek questionnaire and sexual function screener and quality of life sectors were consisted of rated scale questions. Eighty eight questionnaires were returned properly completed. The statistical analysis used the SPSS statistical program.
Results:
Female sexual dysfunction is a highly prevalent health issue whose exact incidence is not well defined. Factors that can contribute to female sexual dysfunction may be psychogenic, physical, mixed or unknown. Each of these factors consists of individual components that influence the sexual response; however their precise impact in FSD development and progression is unknown. Moreover, the role of circadian rhythm disorders (especially that of shift work sleep disorder) to the development and progression of FSD has been poorly investigated.
Conclusion:
Working environment and patterns of work schedules may play a role in FSD however it has been difficult to specify in what extent they contribute to FSD development.
Keywords: Female, sexual dysfunction, quality of life, sleep disorder
1. INTRODUCTION
Sexuality is an important and integral part of every woman’s life, and in fact female sexual dysfunction can lead to personal distress and anxiety. Under the term “female sexual dysfunction” is included a variety of disorders associated with components of sexual function such as sexual desire, arousal and orgasm and pain related to sexual intercourse as well (1). Female sexual dysfunction (FSD) can occur at any stage of life, may be lifelong or acquired; situation-specific or generalized; and mild, moderate, or severe based on the degree of distress it causes to the woman. The etiology is multifactorial (1).
In general, factors that can contribute to its development may be psychogenic, physical and mixed. Each of these factors consists of individual components that influence the sexual response; however their precise impact in FSD development and progression is unknown (1). Moreover, the role of circadian rhythm disorders (especially that of shift work sleep disorder) to the development and progression of FSD has been poorly investigated. The main aim of this study is to investigate the occurrence and severity of FSD in women working in urban hospitals. A secondary aim is to investigate the incidence FSD in women whose work hours overlap with the typical sleep period.
2. MATERIAL AND METHODS
The study sample was drawn from women between the ages of 20 and 65 years, who work standard daytime hours, rotate shifts or work at night in variable frequency, at the Tzaneion General Hospital of Piraeus and Evangelismos General Hospital of Athens. This descriptive study used a structured Greek questionnaire divided into five sections: Personal demographic information (age, educational level, frequency of shifts rotation or night work, age at menarche/age at menopause, family and marital status), sexual function screener (SFS) (investigating disorders of desire/libido, arousal, pain/discomfort and inhibited orgasm), quality of life (QoL), shift work sleep disorder (SWSD) and FSD related medical history (current medications and past medical history, including trauma and past psychiatric history). SFS and QoL sectors were consisted of rated scale questions (0 to 4) while SWSD sector consisted of ‘Yes/No’ questions. The questionnaire has been previously validated and tested (2). We analyzed only those respondents reporting having at least 1 partner in the prior 12-month period. A score of zero in SFS indicated that no sexual activity during this period had been reported. Respondents who were sexually inactive were excluded.
The study protocol was reviewed and approved by the local ethics committees. The participants signed the informed consent forms and strict anonymity was observed throughout the study.
2.1 Statistical analysis
125 questionnaires were handed out and 88 of them were returned properly completed. The response rate was 70.4%. After that we entered the data into an electronic database for further analysis using the SPSS statistical program. Percent prevalence rates and their 95% confidence intervals were calculated by age and 2x2 tables with chi square tests were used to examine differences in proportions. A p value of less than 0.05 was considered significant.
3. RESULTS
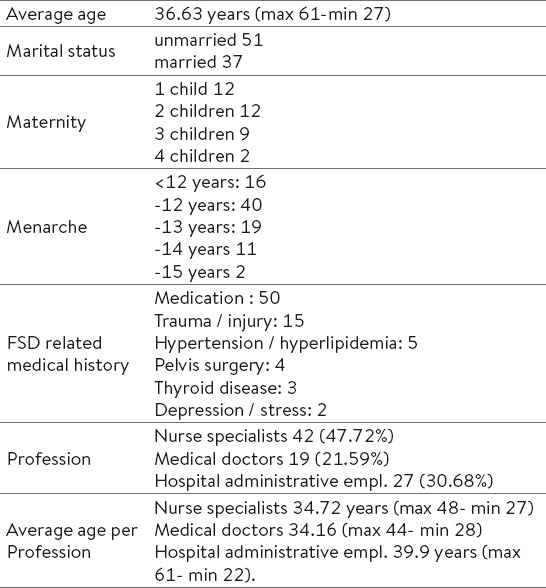
The average age was 36.63 (max 61-min 27) years. Fifty one women were unmarried and 37 were married at the time of the survey. Τwelve women reported having one child, twelve women reported two, nine reported three and two reported four. Sixteen reported early menarche (<12 years), 40 reached menarche by the age of 12 years, 19 by the age of 13 years, 11 reported menarche at 14 and finally, 2 at 15 years. Seventy subjects reported no FSD related medical history, seven reported trauma or injury in the vertebral column region, five reported hypertension and/or hyperlipidemia, four reported pelvis surgery, three thyroid disease and two depression and stress. Thirty seven participants reported recent and/or long-term non-steroidal anti-inflammatory drugs (NSAIDs) use; five were under anti-hypertension treatment, two received anti-lipidemic drugs, two received T4 (thyroxine 50mg) and four received sedatives, antidepressants, antipsychotics and anticonvulsants respectively.
Most of the participants were nurse specialists (42/88) while the remaining were medical doctors and hospital administrative employees (19 and 27 respectively).
Demographic characteristics of the study population are briefly presented on the Table 1.
Table 1.
Personal demographic characteristics of the study population
Sixty one out of the 88 (69.31%) participants reported sexual dysfunction of variable degree (SFS score 4-18). For research analysis purposes, SFS and QoL scores were examined in association with individual characteristics such as specialty and educational level, age, pattern of work schedule, maternity and number of children as well.
The average SFS score of nurse specialists was 18.02 and the average QoL score was 3.11. Similarly, the average SFS score of medical doctors was 18.10; however, their average QoL score was 1.47. In contrast, the average SFS score of hospital administrative employees was 8.81 while their average QoL score was 1.95. Difference in total SFS score between healthcare professionals and administrative employees was statistically significant (p<0.05). in contrast, difference in total QoL score between healthcare professionals and administrative employees was not statistically significant (p>0.05).
The average age of nurse specialists was 34.72 years (max 48- min 27), the average age of medical doctors was 34.16 (max 44- min 28) and the average age for hospital administrative employees was 39.9 years (max 61- min 22).
With regard to age, subjects were divided in four groups: 20-29 (17 women), 30-39 (45 women), 40-49 (22 women), and >50 (4 women). The average SFS score for the age group 20-29 was 15.82 while the average QoL score was 1.68. Regarding the age group 30-39, the average SFS score was 16.63 while the average QoL score was 1.88. The average SFS score for the age group 40-49 was 11.95 and the average QoL score was 2.54. Finally, the average SFS score for the age group >50 was 19.5 and the average QoL score was 3 (Table 2). Several differences in average SFS between age groups were important but not of statistical significance (p>0.05).
Table 2.
Results overview
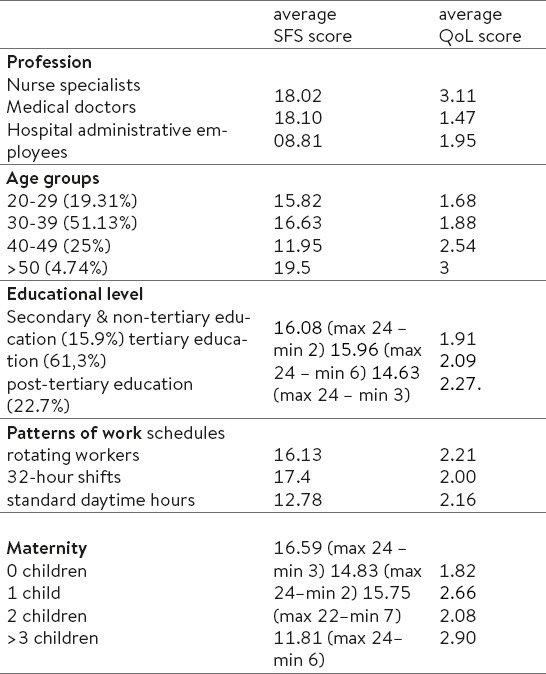
Subjects were also divided in three groups according to educational level [lower secondary education, upper secondary and post-secondary non-tertiary education (14), tertiary education (54) and post-tertiary education (20)]. The average SFS score of participants with secondary education was 16.08 and the average QoL score was 1.91. The average SFS score of participants with tertiary education was 15.96 and the average QoL score was 2.09. The average SFS score of participants with post-tertiary education was 14.63 and the average QoL score was 2.27 (Table 2).
Three patterns of work schedules were reported: Most of the participants (44/88) reported rotating shift work schedule, 14 reported 32-hour shifts bimonthly and 30 standard daytime hours. The manifestations of SWSD were quite variable and corresponded to the shift work schedule: 36.3% of rotating workers (16/44), 37.7% of those working 32-hour shifts (5/14) and 20% of day workers (6/30) reported at least 1 symptom (mainly unrefreshing or insufficient sleep and lack of energy). The average SFS score for the group of rotating workers was 16.13 that of the group of 32-hour shift workers was 17.4, while that of daytime workers was 12.78.
Women with no children had an average SFS score of 16.59. The average QoL score was 1.82. Women with one child had an average SFS score of 14.83. The average QoL score was 2.66. Women with two children had an average SFS score of 15.75 and an average QoL score of 2.08. Women with more than three children had the lowest average SFS score (11.81) and the higher average QoL score (2.9).
With regard to NSAIDs, the average SFS and QoL scores for the users were 14.67 and 2.38 respectively. Regarding to antihypertensive drugs users the average SFS and QoL scores were 7.5 and 3.5 respectively. For thyroxine users the average scores were 16 and 1 while for hyperlipidemics were 18.5 and 3.5.
Regarding individuals reporting trauma or injury in the vertebral column region the average SFS and QoL scores were 11 and 2.28 respectively, while that of individuals reporting pelvis surgery were 18 and 1.8.
4. DISCUSSION
The high prevalence rate of sexual dysfunction in females in this study is similar with that of previous studies (3-5), however the precise incidence remains unclear. According to the Sexual Advice Association, sexual problems affect around 50% of women (6) while other researchers report even lower rates (up to 25%) (7). Actually, data from survey and clinical samples provide different estimations. Lack of consistent methodology and variability of the criteria applied for FSD definition partly explain why the prevalence rates of FSD differ in the various studies. Τhere are three main definitions for FSD that are generally accepted and have been used in the existent epidemiological research. Each one focuses on specific conditions that contribute to FSD development and progression: the ICD-10 classification focuses on physical factors that influence sexual response, the Diagnostic and Statistical Manual (DSM) IV underlines the emotional and psychological factors involved in FSD, and that of the American Foundation of Urological Disease (AFUD) combines the previous with the cyclic sexual response model (8).
In fact, it was shown that classification criteria greatly influence the FSD incidence. For example, the addition of sexual distress in the definition of FSD results in lower prevalence rates (9%) in the general population (7). Moreover, FSD may take different forms (including lack of sexual desire, impaired arousal, inability to achieve orgasm, or pain during sexual activity) in question-based community surveys and clinical studies. Thus, disorders of desire are more common in clinical settings while orgasm disorders are more common in community studies. In contrast, arousal disorders are equally prevalent (2, 9, 10). The above may cause a great deal of uncertainty regarding FSD incidence, given that most of women mainly complain of one sexual problem (2). In addition, variability in levels of normal sexual function and the importance of sexual function to individuals and cultural beliefs also complicate the classification and determination of FSDs (11).
High educational attainment is negatively associated with experience of sexual problems for both sexes. These differences are especially marked between women who do not have high school diplomas and those who have college degrees. Controlling for other demographic characteristics, women who have graduated from college are roughly half as likely to experience low sexual desire, problems achieving orgasm and sexual pain as women who have not graduated from high school (12). Surprisingly, in our study lower educational attainment was associated with higher SFS score (16.08 for secondary, 15.96 for tertiary and 14.63 for post-tertiary education). It should be mentioned however that in our study almost all participants in the secondary education group (12/14) completed upper secondary and post-secondary non-tertiary education. Thus all three educational groups in this study fall in the high educational attainment category of most of the similar studies (11, 12). Another important finding is the trend of the average QoL (1.91 for secondary, 2.09 for tertiary and 2.27 for post-tertiary education) of these individuals to be inversely proportional to that of the average SFS score. This finding is not in accordance with that of other researchers’ who showed that all categories of sexual dysfunction–low sexual desire, arousal disorder, sexual pain–have strong positive associations with low feelings of physical and emotional satisfaction and low feelings of happiness (11). Although the reason justifying our result is not known, a possible explanation is that highly educated career women who have to be able to manage their multiple roles often give less attention to sexual problems (13).
It is not known whether profession affects sexual health. However a survey in an international group of sexuality professionals suggests that there are few differences between sexuality professionals and the general public since most health professionals reported that their profession has positive effects on their sexual functioning (14). Similarly to the above, in our study, a significant difference in average SFS score was noted between health professionals and non-health professionals (18.02 and 18.10 for nurse specialists and medical doctors versus 8.81 for hospital administrative employees). Similar trends were recorded in the relative QoL levels (3.11 versus 1.95 average QoL score of nurse specialists and hospital administrative employees respectively). Despite the relative high average SFS score, the associated average QoL score of medical doctors was low (1.47). The reason explaining the above finding is practically unknown. Actually, the experience of sexual dysfunction is highly associated with a number of unsatisfying personal experiences and relationships and it has been shown that medical doctors are highly susceptible to stress at work and experience more negative outcomes of stress than other health care professionals (15). For this reason, occupational stress is more likely to have an additional impact on female doctors’ sexual dysfunction related QoL (16).
The notable difference in average SFS and QoL scores between nurse specialists and hospital administrative employees can be also attributed to the age difference (on average 34.72 and 39.9 years respectively). In fact FSD tends to become more common as women get older: Dennerstein et al showed that FSD prevalence increased from 42% to 88% from the early to late menopause period (17). In our study a slight decrease in FSD prevalence was found between 30 and 39 years. Following a significant increase between 40 and 49 years (average SFS score: 11.95), FSD prevalence decreases from age 50 onward (average SFS score: 19.5). Actually data are scant and uncertainty exists with regard to the effect of ageing in FSD.
It seems however that an indirect association between ageing and FSD exists and indeed, evidence suggests that while a woman’s sexual function clearly declines with age, the prevalence of most sexual difficulties or dysfunctions changes little (18). Given that this decline begins in a woman’s late 20s to late 30s, gradual decrease in levels of desire, followed by decrease in frequency of orgasm, and frequency of sexual intercourse are considered normal by older women. Moreover, longitudinal studies have shown patterns of stability and improved sexual function for short periods of time in ageing women. Also, Laumann et al demonstrated that FSD is closely associated to the presence of initial desire. The last typically lessens with age but increases with a new partner at any age (3)..
While the causal relationship between QoL and sexual dysfunction remains to be investigated, a study in Greek middle-age women showed that other factors than sexual function predict high QoL score (being married, good financial status, physical exercise) (19). This may explain why in our study the average QoL score was steadily increasing with age.
According to the available data, no notable link between a woman’s childbirth history and low sexual desire exists. In addition, neither the total number of deliveries nor type of delivery is likely to have a substantial long-term detrimental effect on sexual function (20). With regard to maternity and the number of children our findings were somehow controversial: Women with no children had the higher average SFS score (16.59) and the lower average QoL score (1.82), while women with more than three children had the lowest average SFS score (11.81) and the higher average QoL score (2.9). It is not known whether, and independently to their prevalence, sexual dysfunctions may not affect significantly interpersonal functioning and overall quality of life in working women. Thus, variables of social and marital status may be additionally investigated in order to assess how sexual function affects QoL.
People who work on shifts may experience a variety of symptoms such as excessive sleepiness, insomnia, unrefreshing or insufficient sleep, difficulty in concentrating, lack of energy, irritability or depression and difficulty with personal relationships. SWSD can be caused by night shifts, rotating shifts, or even an early morning shift and can cause chronic sleep deprivation. Actually it is not known whether SWSD can cause FSD. It should be mentioned that individuals with sleep disorders often report mood changes such as increased irritability that can impact their interactions with spouses. Since a woman’s sexual response cycle is strongly influenced by the quality of her relationship with her partner, SWSD may contribute to the development of FSD In our study however an inverse association was shown (average SFS score for the groups of rotating and 32-hour shifts workers: 16.13 and 17.4 vs 12.78 of day workers). Our findings may be biased of course by the fact that the average age in the first two groups is lower than that of the third. Therefore an interaction between SWSD and ageing that causes FSD is not to be excluded. This interaction is probably hormone mediated. In fact, as women age, levels of hormone-associated sleep disruptions occur across their lifetime. Among others, the hormones estrogen, progesterone, and testosterone may play a role in the regulation of human circadian rhythms (21). On the other hand, estrogen levels and woman’s sexual function decline with age. As estrogens influence sexual response, low estrogen activity may contribute to sexual dysfunction through dysregulation of human circadian rhythms.
NSAIDs are prescribed for a variety of conditions, including arthritis, sports injuries, and headaches. A large, recent study showed that regular NSAIDs use is associated with erectile dysfunction in men. In this study, age and comorbidity increased the incidence of NSAIDs related erectile dysfunction (22). However there is no information with regard to FSD (23). Although our findings suggest an association between NSAIDs and FSD, scarce information regarding duration of use, underlying diseases and comorbidity does not allow for definitive conclusions. An association between antipsychotic, antidepressant and several antihypertensive agents with FSD has been suggested in the past (22). However, the fact that the exact type of anti-hypertensives wasn’t specified on the questionnaire as well as the small number of individuals receiving lipidemic drugs, thyroxine, sedatives, antidepressants, antipsychotics and anticonvulsants does not allow for notable commentary.
Research findings have supported the hypothesis that the sympathetic nervous system is regulatory for psychogenic genital vasocongestion and that orgasm is a reflex response of the autonomic nervous system (24). Based on these results, individuals reporting trauma or injury in the vertebral column region may present FSD. Although our findings suggest an association, the fact that the exact type of trauma or injury in the vertebral column region wasn’t specified on the questionnaire does not also allow for notable commentary. Similarly our finding of no association between pelvis surgery and FSD is in agreement with what is known, since only major surgical operations and radiation therapies were related to FSD.
Our study showed that it is FSD highly prevalent among working women. Given that the sexual response cycle in women is mediated by the interaction of psychological and physiologic factors, problems affecting one domain may interact with other disorders in a complex fashion. Working environment and patterns of work schedules may play a role inFSD however it has been difficult to specify in what extent they contribute to FSD development.
Footnotes
• Abbreviations: Female sexual dysfunction (FSD), sexual function screener (SFS), quality of life (QoL), shift work sleep disorder (SWSD)
• Conflict of interest: none declared.
REFERENCES
- 1.Bancroft J, Loftus J, Long JS. Distress about sex: a national survey of women in heterosexual relationships. Arch Sex Behav. 2003;32:193–208. doi: 10.1023/a:1023420431760. [DOI] [PubMed] [Google Scholar]
- 2.Gardikou V, Dertimani M, Noulas E, Stamatiou K. Study of female sexual dysfunction in hospital staff. 6th National and 5th Scientific & Professional Nursing Conference. Lefkada, Greece: 2013. May, [Google Scholar]
- 3.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281:537–44. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 4.Spector IP, Carey MP. Incidence and prevalence of the sexual dysfunctions: a critical review of the empirical literature. Arch Sex Behav. 1990;19(4):389–408. doi: 10.1007/BF01541933. [DOI] [PubMed] [Google Scholar]
- 5.Amidu N, Owiredu WK, Woode E, Addai-Mensah O, Quaye L, Alhassan A, et al. Incidence of sexual dysfunction: a prospective survey in Ghanaian females. Reprod Biol Endocrinol. 2010;8:106. doi: 10.1186/1477-7827-8-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Female sexual problems. NHS choices. Available from: http://www.nhs.uk/Livewell/Goodsex/Pages/Femalesexualdysfunction.aspx .
- 7.Rosen RC. Prevalence and risk factors of sexual dysfunction in men and women. Curr Psychiatry Rep. 2000;2(3):189–95. doi: 10.1007/s11920-996-0006-2. [DOI] [PubMed] [Google Scholar]
- 8.Bargiota A, Dimitropoulos K, Tzortzis V, Koukoulis GN. Sexual dysfunction in diabetic women. Hormones. 2011;10(3):196–206. doi: 10.14310/horm.2002.1309. [DOI] [PubMed] [Google Scholar]
- 9.Rosen RC, Taylor JF, Leiblum SR, Bachmann GA. Prevalence of sexual dysfunction in women: Results of a survey study of 329 women in an outpatient gynecological clinic. J Sex Marital Ther. 1993;19(3):171–88. doi: 10.1080/00926239308404902. [DOI] [PubMed] [Google Scholar]
- 10.Simons J, Carey MP. Prevalence of Sexual Dysfunctions. Results from a Decade of Research. Arch Sex Behav. 2001;30(2):177–219. doi: 10.1023/a:1002729318254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA. 1999;281(6):537–544. doi: 10.1001/jama.281.6.537. [DOI] [PubMed] [Google Scholar]
- 12.Shifren JL, Monz BU, Russo PA, Segreti A, Johannes CB. Sexual problems and distress in United States women: prevalence and correlates. Obstet Gynecol. 2008;112:970. doi: 10.1097/AOG.0b013e3181898cdb. [DOI] [PubMed] [Google Scholar]
- 13.Poduval J, Poduval Μ. Working Mothers: How Much Working, How Much Mothers, And Where Is The Womanhood? Mens Sana Monogr. 2009;7(1):63–79. doi: 10.4103/0973-1229.41799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luria M1, Byers ES, Voyer SD, Mock M. Motivations and sexual attitudes, experiences, and behavior of sexuality professionals. J Sex Marital Ther. 2013;39(2):112–31. doi: 10.1080/0092623X.2011.606882. [DOI] [PubMed] [Google Scholar]
- 15.Phipps L. Stress among doctors and nurses in the emergency department of a general hospital. CMAJ. 1988;139:375–6. [PMC free article] [PubMed] [Google Scholar]
- 16.Swanson V, Power K, Simpson R. A comparison of stress and job satisfaction in female and male GPS and consultants. Stress Med. 1996;12:17–26. [Google Scholar]
- 17.Dennerstein L, Hayes RD. Confronting the challenges: epidemiological study of female sexual dysfunction and the menopause. J Sex Med. 2005;2(Suppl 3):118–32. doi: 10.1111/j.1743-6109.2005.00128.x. [DOI] [PubMed] [Google Scholar]
- 18.Hayes R, Dennerstein L. The impact of aging on sexual function and sexual dysfunction in women: a review of population-based studies. J Sex Med. 2005;2(3):317–30. doi: 10.1111/j.1743-6109.2005.20356.x. [DOI] [PubMed] [Google Scholar]
- 19.Giannouli P, Zervas I, Armeni E, Koundi K, Spyropoulou A, Alexandrou A, et al. Determinants of quality of life in Greek middle-age women: a population survey. Maturitas. 2012;71(2):154–61. doi: 10.1016/j.maturitas.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 20.Basson R. Clinical practice. Sexual desire and arousal disorders in women. N Engl J Med. 2006;354:1497. doi: 10.1056/NEJMcp050154. [DOI] [PubMed] [Google Scholar]
- 21.Andersen ML, Alvarenga TF, Mazaro-Costa R, Hachul HC, Tufik S. The association of testosterone, sleep, and sexual function in men and women. Brain Res. 2011;1416:80–104. doi: 10.1016/j.brainres.2011.07.060. [DOI] [PubMed] [Google Scholar]
- 22.Gleason JM1, Slezak JM, Jung H, Reynolds K, Van den Eeden SK, Haque R, et al. Regular nonsteroidal anti-inflammatory drug use and erectile dysfunction. J Urol. 2011;185(4):1388–93. doi: 10.1016/j.juro.2010.11.092. [DOI] [PubMed] [Google Scholar]
- 23.Finger WW, Lund M, Slagle MA. Medications that may contribute to sexual disorders. A guide to assessment and treatment in family practice. J Fam Pract. 1997;44:33–43. [PubMed] [Google Scholar]
- 24.Sipski ML, Arenas A. Female sexual function after spinal cord injury. Prog Brain Res. 2006;152:441–7. doi: 10.1016/S0079-6123(05)52030-2. [DOI] [PubMed] [Google Scholar]


