Abstract
Introduction:
The commonest mitral regurgitation etiologies are degenerative (60%), rheumatic post-inflammatory, 12%) and functional (25%). Due to the large number of patients with acute MI, the incidence of ischaemic MR is also high. Ischaemic mitral regurgitation is a complex multifactorial disease that involves left ventricular geometry, the mitral annulus, and the valvular/subvalvular apparatus. Ischaemic mitral regurgitation is an important consequence of LV remodeling after myocardial infarction.
Research Objectives:
The objective of this study is to determine the role of echocardiography in detecting and assessment of mitral regurgitation mechanism, severity, impact on treatment strategy and long term outcome in patients with myocardial infarction during the follow up period of 5 years. Also one of objectives to determine if the absence or presence of ischaemic MR is associated with increased morbidity and mortality in patients with myocardial infarction.
Patients and methods:
The study covered 138 adult patients. All patients were subjected to echocardiography evaluation after acute myocardial infarction during the period of follow up for 5 years. The patients were examined on an ultrasound machine Philips iE 33 xMatrix, Philips HD 11 XE, and GE Vivid 7 equipped with all cardiologic probes for adults and multi-plan TEE probes. We evaluated mechanisms and severity of mitral regurgitation which includes the regurgitant volume (RV), effective regurgitant orifice area (EROA), the regurgitant fraction (RF), Jet/LA area, also we measured the of vena contracta width (VC width cm) for assessment of IMR severity, papillary muscles anatomy and displacement, LV systolic function ± dilation, LV regional wall motion abnormality WMA, LV WMI, Left ventricle LV remodeling, impact on treatment strategy and long term mortality.
Results:
We analyzed and follow up 138 patients with previous (>16 days) Q-wave myocardial infarction by ECG who underwent TTE and TEE echocardiography for detection and assessment of ischaemic mitral regurgitation (IMR) with baseline age (62 ± 9), ejection fraction (EF 41±12%), the regurgitant volume (RV) were 42±21 mL/beat, and effective regurgitant orifice area (EROA) 20±16 mm2, the regurgitant fraction (RF) were 48±10%, Jet/LA area 47±12%. Also we measured the of vena contracta width (VC width cm) 0,4±0,6 for assessment of IMR severity. During 5 years follow up, total mortality for patients with moderate/severe IMR–grade II-IV (54.2±1.8%) were higher than for those with mild IMR–grade I (30.4±2.9%) (P<0.05), the total mortality for patients with EROA ≥20 mm2(54±1.9%) were higher than for those with EROA <20 mm2(27.2±2.7%) (P<0.05), and the total mortality for patients with RVol ≥30 mL (56.8±1.7%) were higher than for those with RVol<30ml (29.4±2.9%) (P<0.05). After assessment of IMR and during follow up period 64 patients (46%) underwent CABG alone or combined CABG with mitral valve repair or replacement. In this study, the procedure of concomitant down-sized ring annuloplasty at the time if CABG surgery has a failure rate around 24% in terms of high late recurrence rate of IMR during the follow period especially after 18–42 months.
Conclusion:
The presence of ischaemic MR is associated with increased morbidity and mortality. Chronic IMR, an independent predictor of mortality with a reported survival of 40–60% at 5 years. Ischaemic mitral regurgitation has important prognosis implications in patients with coronary heart disease. Recognizing the mechanism of valve incompetence is an essential point for the surgical planning and for a good result of the mitral repair. It is important that echocardiographers understand the complex nature of the condition. Despite remarkable progress in reparative surgery, further investigation is still necessary to find the best approach to treat ischaemic mitral regurgitation.
Keywords: Ischaemic mitral regurgitation, Myocardial infarction, Ventricular remodelling, Regurgitant volume (RV), Effective regurgitant orifice area (EROA), Regurgitant fraction (RF), Papillary muscle displacement, Mitral annulus dilation, Mitral leaflet tethering
1. INTRODUCTION
The MV comprises two leaflets, annular attachment at the atrioventricular junction, tendinous chords and the papillary muscles. Complete closure (coaptation) and correct apposition (symmetrical overlap, usually a minimum of 4-5mm) of both leaflets is essential in preventing regurgitation. The commonest mitral regurgitation etiologies are degenerative (60%), rheumatic (post-inflammatory, 12%) and functional (25%). Due to the large number of patients with acute MI, the incidence of ischaemic MR is also high. The secondary MR is not a primary valve disease but results from tethering (apical and lateral papillary muscle displacement, annular dilatation) and reduced closing forces, due to LV dysfunction (reduced contractility and/or LV dysynchrony). The diagnostic criteria of chronic IMR can be summarized as follows: MR occurring more than 16 days after myocardial infarction (MI) with one or more LV segmental wall motion abnormalities; significant coronary disease in a territory supplying the wall motion abnormalities and structurally normal MV leaflets and chordae tendinae. The third criterion is important to exclude patients with organic MR and associated CAD.
The underlying pathophysiologic mechanisms of IMR are often complex, resulting from several different structural changes involving left ventricular geometry, the mitral annulus, and the valvular/subvalvular apparatus. IMR occurs despite a structurally normal mitral valve as a consequence of a ventricular disease. Ischaemic mitral regurgitation is a complex multifactorial disease that involves global and regional left ventricular remodeling as well as dysfunction and distortion of the components of the mitral valve including the chordae, annulus and leaflets. Ischaemic MR affects patients’ prognosis, doubling mortality following myocardial infarction and heart failure.
In patients with ischaemic mitral regurgitation after myocardial infarction, the mitral annulus enlargement is one of the determinants of the regurgitant volume and of the effective regurgitant orifice area. Echocardiographic diagnosis and assessment of ischaemic mitral regurgitation are critical to gauge its adverse effects on prognosis and to attempt to tailor rational treatment strategy (Figure 1).
Figure 1.
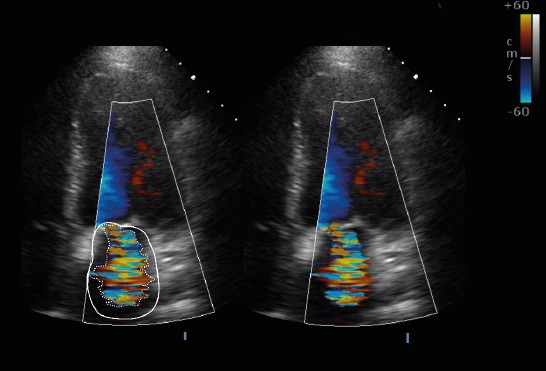
MR quantification by ratio of maximal distal jet area to left atrial area. Assessment of MR severity by distal jet area involves tracing the jet area (dashed white line) in the apical four chamber view and comparing the ratio of jet area to the left atrial area (solid white line)
2. RESEARCH OBJECTIVES
The objective of this study is to determine the role of echocardiography in detecting and assessment of mitral regurgitation mechanism, severity, impact on treatment strategy and long term outcome in patients with myocardial infarction during the follow up period of 5 years. Myocardial infarction was diagnosed based on medical history, hospital discharge documents, electrocardiography (ECG) and echocardiography findings. The evaluation of mitral regurgitation parameters and wall motion abnormalities of the left ventricle obtained by echocardiography (TTE and TEE) as a noninvasive diagnostic method. Also one of objectives to determine if the absence or presence of ischaemic MR is associated with increased morbidity and mortality in patients with myocardial infarction.
3. PATIENTS AND METHODS
The study covered 138 adult patients. All patients were subjected to echocardiography evaluation after acute myocardial infarction during the period of follow up for 5 years. The echocardiography examinations were performed using commercially available equipment and standard techniques. The patients were examined on an ultrasound machine Philips iE 33 xMatrix, Philips HD 11 XE, and GE Vivid 7 equipped with all cardiologic probes for adults and multi-plan TEE probes. Examinations consisted of multiple tomographic planes including long-axis and short-axis views with color Doppler and continuous wave Doppler for detection and assessment of myocardial function and valvular disease. Degree and severity of MR was assessed semi quantitatively and quantitatively which includes the regurgitant volume (RV), effective regurgitant orifice area (EROA), the regurgitant fraction (RF), mitral regurgitation jet direction, Jet/LA area, also we measured the of vena contracta width (VC width cm) for assessment of IMR severity according to the ASE guidelines 2003 and ESC guidelines 2012.
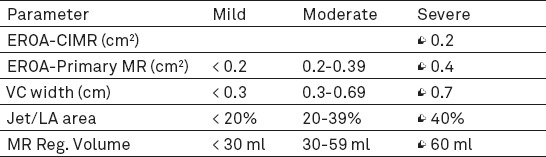
Table 1 presents AHA Guidelines - however 2014 American College of Cardiology/American Heart Association guidelines propose a new classification scheme of valvular disease severity, based on a combination of echocardiographic and symptomatic parameters, with stages of “at risk” to “progressive” to “asymptomatic severe” to “symptomatic severe”, papillary muscles anatomy and displacement, annular dimension, LV systolic function ± dilation, LV regional wall motion abnormality WMA, LV WMI, Left ventricle LV remodeling, impact on treatment strategy and long term mortality.
Table 1.
Guidelines based reference ranges for grading MR–2003 ASE guidelines
4. RESULTS
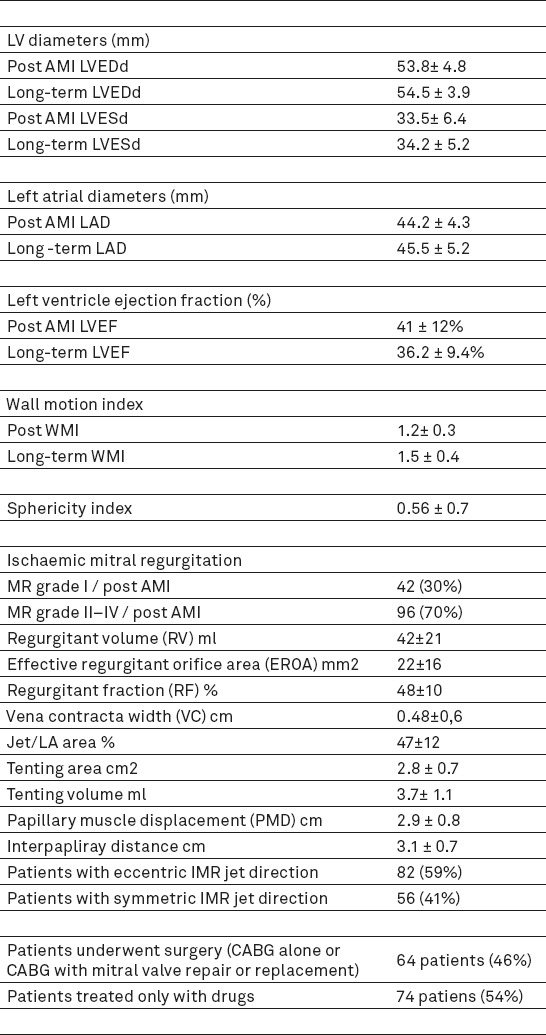
We analyzed and follow up 138 patients with previous (>16 days) Q-wave myocardial infarction by ECG who underwent TTE and TEE echocardiography for detection and assessment of chronic ischaemic mitral regurgitation (IMR). The demographic data, risk factors, clinical and comorbidity characteristics for all patients are shown on Table 2. The echocardiographic data and characteristics for all patients are shown on Table 3. The baseline age of patients was (62 ± 9), ejection fraction was (EF 35±14%), the regurgitant volume (RV) were 42±21 mL/beat, and effective regurgitant orifice area (EROA) 20±16 mm2, the regurgitant fraction (RF) were 48±10%, Jet/LA area was 47±12%. Also we measured the of vena contracta width (VC width cm) 0,48±0,6 for assessment of IMR severity. After assessment of IMR and during follow up period 64 patients (46%) underwent CABG alone or combined CABG with mitral valve repair or replacement.
Table 2.
Patient demographic, risk factors, clinical and comorbidity characteristics
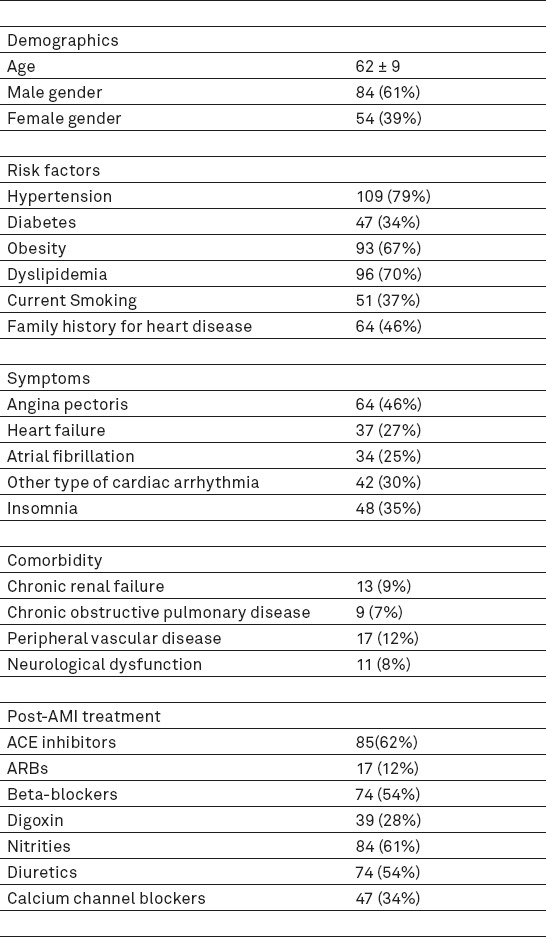
Table 3.
Echocardiographic characteristics
During 5 years follow up, total mortality for patients with moderate/severe IMR–grade II-IV (54.2±1.8%) were higher than for those with mild IMR–grade I (30.4±2.9%) (P<0.05) (Figure 2) the total mortality for patients with EROA ≥20 mm2(54±1.9%) were higher than for those with EROA <20 mm2(27.2±2.7%) (P<0.05) (Figure 3), and the total mortality for patients with RVol ≥30 mL (56.8±1.7%) were higher than for those with RVol<30ml (29.4±2.9%) (P<0.05) (Figure 4).
Figure 2.
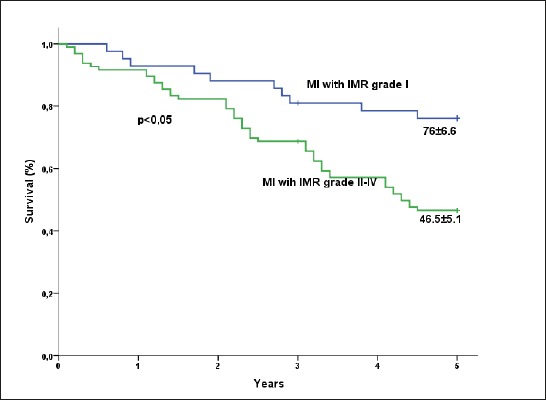
Survival (± SE) in patients with MI according to the degree of IMR as graded by echocardiography: IMR gr I and IMR grade II-IV
Figure 3.
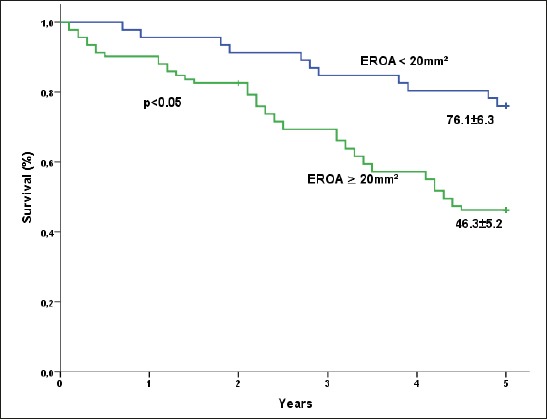
Survival (± SE) in patients according to the degree of IMR as graded by EROA ≥20mm2 or EROA <20mm2 estimated by echocardiography.
Figure 4.
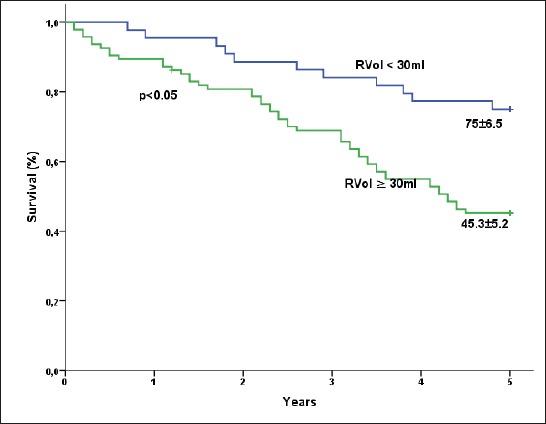
Survival (± SE) in patients according to the echocardiography degree of IMR as graded by RVol ≥30ml or RVol<30ml.
In this study, the procedure of concomitant down-sized ring annuloplasty at the time if CABG surgery has a failure rate around 24% in terms of high late recurrence rate of IMR during the follow period especially after 18–42 months.
Also the study shows that revascularization alone does not result in a significant change in IMR grade both in patients with mild IMR or with moderate-to-severe IMR, it seems that the effects of revascularization on closing pressure are likely to depend on the presence and extent of viable myocardium. Also a significant percentage of patients with mild-to moderate IMR has an increase in degree or recurrence rate of IMR during the follow-up period of 5 years. The risk of operative mortality is higher after combined CABG and MV repair or replacement than after revascularization alone (7.5% -12% vs 2–5%).
Different drugs and combinations are usually used in patients with IMR in order to reduce the severity of MR and to reverse or delay the LV remodeling process. This study confirmed that the use of ACE-inhibitors and beta blockers in combination with diuretics is an independent predictor of better long-term survival in patients with IMR and LV dysfunction.
5. DISCUSSION
Mitral regurgitation can be primary due to leaflet abnormalities and secondary due to dysfunction of the left ventricle usually after myocardial infarction with structurally normal MV as ischaemic mitral regurgitation. The prevalence rate of development of mild or more severe degree of mitral regurgitation after myocardial infarction has been estimated to be up to 50% and is associated with worse prognosis (1-6), reviewed the prevalence of IMR after myocardial infarction, and reported that any IMR is present in 21% of patients, and 3–13% have at least moderate IMR.
Ischaemic MR is not only a common but also a serious finding. The community based study of ischaemic MR among 30 day survivors of MI showed moderate or severe MR to be associated with a threefold increase in the risk of heart failure and increased risk of death at 5 year follow-up independent of age, gender, ejection fraction and Killip class (6). Mortality was increased even with mild MR (5).
Nesta et al (7) reported that anterior leaflet in the echocardiographic long axis view is convex toward the left atrium in normal subjects but is concave in patients with ischaemic MR, suggesting that the middle portion of the anterior leaflet is more tethered compared to the leaflet tip.
Schwammenthal et al (10) have found that ischaemic MR dynamically changes in severity within a cardiac cycle, with the severity often maximal in early and late systole and minimal in mid-systole with maximal LV pressure. Hung et al (8) also confirmed such dynamic MR even in patients with surgical ring annuloplasty, confirming the importance of closing force.
The classic pattern of ischaemic MR involves a posterior wall motion abnormality with regional remodelling, leading to posterolateral and apical displacement of the (posterior) papillary muscle, the apical component of which appears to be the most important. This regional remodelling appears to be related to the regional scar burden (5). As the papillary muscle contributes chordae to both leaflets, the consequences are: (1) displacement of the posterior leaflet posteriorly; (2) development of a hockey stick deformity of the anterior leaflet due to tethered secondary chordae; and (3) displacement of the mitral coaptation point posteriorly (causing an asymmetric shape). The consequence is anterior leaflet override with a posterior MR jet (11).
The presence of moderate and severe MR appears to identify a higher risk group of patients who often progress early to congestive heart failure because of irreversible LV dysfunction and are at a higher risk for sudden death. This fact emphasizes the importance of MR as a marker of adverse outcome and suggests a cautious approach of such patients following AMI (12). MR seems to be a common finding after AMI. Previous large-scale trials, such as the SAVE study (Survival And Ventricular Enlargement), suggested that even mild MR is associated with high mortality after AMI (2). In addition, it has been well established that the presence of ischaemic MR is influenced by the size and location of the infarction. The presence of MR is associated with the presence of a larger LV diameter, indicating more extensive changes in LV geometry following AMI (13, 14, 4).
Papillary muscle dysfunction
The concept of PM dysfunction was based on clinical observations that ischaemic MR occurred after inferior myocardial infarction and secondary dysfunction of the medial PM (15). Historically, the mechanism of chronic IMR was attributed to papillary muscle dysfunction. However, further studies demonstrated that ischemia of papillary muscles themselves fails to produce significant MR without damage of the underlying myocardial wall. Papillary muscle discoordination-the papillary muscles are the main contributors to acute ischaemic MR. Although traditionally incriminated in chronic ischaemic MR, the importance of associated regional LV dysfunction has been recognized for nearly 40 years (11, 16). The investigators observed that addition of PM dysfunction with ischemia attenuated leaflet tethering and MR. This concept was later explored in clinical patients by Uemura et al (17). The data indicate that PM dysfunction is not the primary cause of ischaemic MR and that it may result in attenuated tethering and MR. These observations, rather than disproving the tethering mechanism, actually confirm that the tethering distance from the PM tip to the mitral annulus is the final common pathway that determines the level of leaflet coaptation. Ischaemic MR was expected to result from leaflet prolapse due to the reduced longitudinal contraction of the PMs secondary to ischaemic dysfunction. Recent reports suggest the central role of tethering in ischaemic MR (18, 19).
Wall motion abnormalities are critically important in gauging local LV dysfunction in CIMR: the echocardiographer should identify and quantify wall motion as part of a comprehensive assessment of a global assessment of ischaemic burden. Indices of wall motion abnormalities underlying the posteromedial PM insertion are highly important in assessing CIMR (20). In patients with ischaemic mitral regurgitation after myocardial infarction, the mitral annulus enlargement is one of the determinants of the regurgitant volume and of the effective regurgitant orifice area. It seems that in the case of the mitral regurgitation with smaller regurgitant orifice area (<0.3 cm2), the importance of the regurgitation depends mainly on the enlargement of the annulus, on the other hand, in the case of the mitral regurgitation with larger regurgitant orifice area (>0.4 cm2) the leaflets restriction determined by the posterior papillary muscle displacement plays a very significant role (21). Measurement of vena contracta width may be a preferable means of assessing MR severity, although this is equally influenced by changes in LV pressure and dimensions. There is evidence that three dimensional echocardiography is superior to two dimensional techniques for the measurement of vena contracta, especially with eccentric jets (11, 22). Chronic IMR, an independent predictor of mortality with a reported survival of 40–60% at 5 years (5, 23, 24) is a progressive disorder in which MR-related LV volume overload promotes further LV remodelling, leading to worsened MR. Therefore, surgical correction, either by replacement or repair, is recommended for 3+ and 4+ IMR (25, 26).
The use of TEE intraoperatively and post-operatively in the evaluation of MR has been comprehensively reviewed by Sidebotham et al and Shakil et al (27, 28) TEE is important in assessment of patients undergoing surgical revascularization as it provides another opportunity to assess for CIMR. However, because of vasodilating effects of anesthesia, CIMR severity may be underestimated by intraoperative TEE.
It has clearly been demonstrated by Grigoni et al (5), that IMR aggravates prognosis after myocardial infarction corresponding with severity, and thus there is an absolute need for an effective treatment. Currently, the “gold-standard” treatment if IMR is concomitant down-sized ring annuloplasty at the time if CABG surgery. However, this procedure has a failure rate around 20-30% in terms of recurrent IMR after the first 2 - 4 years, and there are few, if any, other disciplines in cardiac surgery where we consider such a result a “gold standard”. This underscores that we still have not identified a truly effective and lasting treatment if IMR, that relieves patient suffering and improves survival. Therefore, IMR is very much an unsolved challenge (29-31).
Several studies had demonstrated that revascularization alone does not result in a significant change in IMR grade both in patients with mild-to-moderate IMR (1+or 2+) and with moderate-to-severe IMR (3+or 4+) and a significant percentage of patients with mild-to moderate IMR has an increase in degree or recurrence of IMR during follow-up (25, 29-35). However, revascularization alone appears to produce long-term survival similar to that for revascularization plus annuloplasty both in patients with moderate and severe IMR, whereas the risk of operative mortality is higher after combined revascularization and MV repair than after revascularization alone (9.5%-15% vs 3-5%). Kim et al (33) reported a 5-year actuarial survival in patients with 3+or4+IMR of 44%+5% after combined procedure and 41%+7% after revascularization alone. Wong et al (34) reported no significant difference in mortality for concomitant annuloplasty compared with revascularization alone in patients with 3+IMR with a 5-year survival of 67.5% in the whole group of patients (36). Whereas good results have been reported by Bax et al (37) - high late recurrence rates of MR after ring annuloplasty have been published McGee et al (24) reported a 28% recurrence rate of 3+ or 4+MR at 6 months. Furthermore, Serry et al (38) reported a recurrence rate of 36% for 2+MR and 20% for 3+to 4+MR at 28 months, while Tahta et al (39) reported a recurrence rate for 2+to 4+MR of 29% at 35 months.
Myocardial revascularization does not necessarily reverse ischaemic MR. In a study of coronary bypass surgery in 136 patients with moderate ischaemic MR, half showed an improvement in MR, but resolution of MR occurred in only 9%, and 40% had residual moderate or severe MR (25). The effects of revascularization on closing pressure are likely to depend on the presence and extent of viable myocardium. The mechanisms responsible for recurrence of CIMR after surgical revascularization and restrictive annuloplasty remain elusive. In some instances, the mechanism is ongoing adverse LV dilatation and spherical remodelling that worsens tethering (40, 41). The current medical therapy for heart failure includes vasodilators (ACE-inhibitors), diuretics and beta blockers, and its beneficial effects on symptoms of heart failure in patients with IMR and LV dysfunction may be dramatic.
Various combinations of these drugs are commonly used in these patients for two reasons: to reduce the severity of MR and to reverse or delay the LV remodeling process. The use of afterload-reducing agents, including ACE-inhibitors, might reduce the regurgitant volume and improve forward output by decreasing the pressure gradient between LV and left atrium. Vasodilators may effectively decrease regurgitant flow through the effect of systolic unloading on the regurgitant orifice area (3, 7). A similar effect of reduction in MR is obtained with preload reduction through the use of diuretics that decrease ventricular size and further reduce tethering with a consequent decrease in the regurgitant volume (3). The use of ACE-inhibitors and b-blockers is an independent predictor of better long-term survival in patients with IMR and LV dysfunction, as reported by Wu and colleagues (42). This could be due to the effects of ACE-inhibitors and b-blockers on progression of LV remodeling and prevention of sudden death (35).
6. CONCLUSION
The ischaemic mitral regurgitation has many specific features which differentiates it from organic regurgitations. The clinical signs of MR and its severity are unreliable in ischaemic MR. Ischaemic mitral regurgitation has important prognosis implications in patients with coronary heart disease. It should not be underestimated and this underlines the need for a complete evaluation but should be interpreted specifically, in particular as regards quantification of the regurgitation. Recognizing the mechanism of valve incompetence is an essential point for the surgical planning and for a good result of the mitral repair. In the patient’s candidates to surgery, the role of the echocardiographic exam is to identify the mechanisms of valve regurgitation and to quantify it. The excess mortality, which was considerable for ERO ≥20 mm2 and RVol ≥ 30mL, suggests that quantification of MR in the post-MI chronic phase is essential for risk stratification. Furthermore, the high risk associated with IMR suggests that such patients should be managed actively and that all therapeutic options of medical and surgical treatment should be considered promptly. Even today, we have no reliable predictors of recurrent and persistent mitral regurgitation.
The presence of ischaemic MR is associated with increased morbidity and mortality. Chronic IMR, an independent predictor of mortality with a reported survival of 40–60% at 5 years, Chronic IMR is a progressive disorder in which MR-related LV volume overload promotes further LV remodeling, leading to worsened MR. It is important that echocardiographers understand the complex nature of the condition. Despite remarkable progress in reparative surgery, further investigation is still necessary to find the best approach to treat ischaemic mitral regurgitation.
Footnotes
• Conflict of interest: None declared.
REFERENCES
- 1.Lancellotti P, Moura L, Pierard LA, Agricola E, Popescu BA, Tribouilloy C, et al. European association of echocardiography recommendations for the assessment of valvular regurgitation. Eur J Echo. 2010;11:307–32. doi: 10.1093/ejechocard/jeq031. [DOI] [PubMed] [Google Scholar]
- 2.Lamas GA, Mitchell GF, Flaker GC, et al. Clinical significance of mitral regurgitation after acute myocardial infarction:Survival and Ventricular Enlargement Investigators. Circulation. 1997;96:827–33. doi: 10.1161/01.cir.96.3.827. [DOI] [PubMed] [Google Scholar]
- 3.Stevenson LW, Bellil D, Grover-McKay M, Brunken RC, Schwaiger M, Tillisch JH, Schelbert HR. Effects of afterload reduction (diuretics and vasodilators) on left ventricular volume and mitral regurgitation in severe congestive heart failure secondary to ischaemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 1987;60:654–8. doi: 10.1016/0002-9149(87)90376-6. [DOI] [PubMed] [Google Scholar]
- 4.Feinberg MS, Schwammenthal E, Shlizerman L, Porter A, Hod H, Friemark D, Matezky S, Boyko V, Mandelzweig L, Vered Z, Behar S, Sagie A. Prognostic significance of mild mitral regurgitation by color Doppler echocardiography in acute myocardial infarction. Am J Cardiol. 2000;86:903–7. doi: 10.1016/s0002-9149(00)01119-x. [DOI] [PubMed] [Google Scholar]
- 5.Grigioni F, Enriquez-Sarano M, Zehr KJ, Bailey KR, Tajik AJ. Ischaemic mitral regurgitation:long-term outcome and prognostic implications with quantitative Doppler assessment. Circulation. 2001;103:1759–64. doi: 10.1161/01.cir.103.13.1759. [DOI] [PubMed] [Google Scholar]
- 6.Bursi F, Enriquez-Sarano M, Nkomo VT, et al. Heart failure and death after myocardial infarction in the community:the emerging role of mitral regurgitation. Circulation. 2005;111:295–301. doi: 10.1161/01.CIR.0000151097.30779.04. [DOI] [PubMed] [Google Scholar]
- 7.Levine RA, Hung J. Ischaemic mitral regurgitation, the dynamic lesion:clues to the cure. J Am Coll Cardiol. 2003;42:1929–32. doi: 10.1016/j.jacc.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Hung J, Guerrero JL, Handschumacher MD, Supple G, Sullivan S, Levine RA. Reverse ventricular remodeling reduces ischaemic mitral regurgitation:echo-guided device application in the beating heart. Circulation. 2002;106:2594–2600. doi: 10.1161/01.cir.0000038363.83133.6d. [DOI] [PubMed] [Google Scholar]
- 9.Nishimura RA, Otto CM, Bonow R, Carabello BA, Erwin JP, III, Guyton RA, O’Gara PT, Ruiz CE, Skubas NJ, Sorajja P, Sundt TM, III, Thomas JD. AHA/ACC Guidelines for the management of patients with valvular heart disease:a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;129:e521–e643. doi: 10.1161/CIR.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 10.Schwammenthal E, Chen C, Benning F, Block M, Breithardt G, Levine RA. Dynamics of mitral regurgitant flow and orifice area. Physiologic application of the proximal flow convergence method:clinical data and experimental testing. Circulation. 1994;90:307–22. doi: 10.1161/01.cir.90.1.307. [DOI] [PubMed] [Google Scholar]
- 11.Thomas H Marwick, Patrizio Lancellotti, Luc Pierard. Ischaemic mitral regurgitation:Mechanisms and diagnosis. Heart. 2009;95:1711–8. doi: 10.1136/hrt.2007.135335. [DOI] [PubMed] [Google Scholar]
- 12.Zamorano J, de Isla LP, Oliveros L, Almeria C, Rodrigo JL, Aubele A, et al. Prognostic influence of mitral regurgitation prior to a first myocardial infarction. Eur Heart J. 2005;26:343–9. doi: 10.1093/eurheartj/ehi065. [DOI] [PubMed] [Google Scholar]
- 13.Laneras MR, Nance ML, Streicher JT, et al. Pathogenesis of ischaemic mitral regurgitation. Ann Thorac Surg. 1994;57:432–9. doi: 10.1016/0003-4975(94)91012-x. [DOI] [PubMed] [Google Scholar]
- 14.Klein P, Braun J, Holman RE, Versteegh M, Verwey H, Dion R, Bax J, Klautz R. Management of mitral regurgitation during left ventricular reconstruction for ischaemic heart failure. European Journal of Cardio-Thoracic Surgery. 2012 Jan;41(1):74–81. doi: 10.1016/j.ejcts.2011.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burch GE, DePasquale NP, Phillips JH. Clinical manifestations of papillary muscle dysfunction. Arch Intern Med. 1963;112:112–7. doi: 10.1001/archinte.1963.03860010138015. [DOI] [PubMed] [Google Scholar]
- 16.Mittal AK, Langston M, Jr, Cohn KE, Selzer A, Kerth WJ. Combined papillary muscle and left ventricular wall dysfunction as a cause of mitral regurgitation:an experimental study. Circulation. 1971;44:174–80. doi: 10.1161/01.cir.44.2.174. [DOI] [PubMed] [Google Scholar]
- 17.Uemura T, Otsuji Y, Nakashiki K, Yoshifuku S, Maki Y, Yu B, et al. Papillary muscle dysfunction attenuates ischaemic mitral regurgitation in patients with localized basal inferior left ventricular remodeling:insights from tissue Doppler strain imaging. J Am Coll Cardiol. 2005;46:113–9. doi: 10.1016/j.jacc.2005.03.049. [DOI] [PubMed] [Google Scholar]
- 18.Yiu SF, Enriquez-Sarano M, Tribouilloy C, Seward JB, Tajik AJ. Determinants of the degree of functional mitral regurgitation in patients with systolic left ventricular dysfunction:A quantitative clinical study. Circulation. 2000;102:1400–6. doi: 10.1161/01.cir.102.12.1400. [DOI] [PubMed] [Google Scholar]
- 19.Otsuji Y, Handschumacher MD, Liel-Cohen N, Tanabe H, Jiang L, Schwammenthal E, Guerrero JL, Nicholls LA, Vlahakes GJ, Levine RA. Mechanism of ischaemic mitral regurgitation with segmental left ventricular dysfunction:three-dimensional echocardiographic studies in models of acute and chronic progressive regurgitation. J Am Coll Cardiol. 2001;37:641–8. doi: 10.1016/s0735-1097(00)01134-7. [DOI] [PubMed] [Google Scholar]
- 20.Dudzinski D, Hung J. Echocardiographic assessment of ischaemic mitral regurgitation Cardiovascular Ultrasound. 2014;12:46. doi: 10.1186/1476-7120-12-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Labecka A, Firek B, Szymanski P, Kowalik I, Szwed H, Pasierski T. Transthoracic and transesophageal echocardiographic evaluation of the ischaemic mitral regurgitation determinants. European Journal of Echocardiography. 2006 Dec;7(suppl 1):S66. [Google Scholar]
- 22.Little SH, Pirat B, Kumar R, et al. Three-dimensional color Doppler echocardiography for direct measurement of vena contracta area in mitral regurgitation:in vitro validation and clinical experience. J Am Coll CardiolI. 2008;1:695–704. doi: 10.1016/j.jcmg.2008.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grossi EA, Woo YJ, Patel N, Goldberg JD, Schwartz CF, Subramanian VA, Genco C, Goldman SM, Zenati MA, Wolfe JA, Mishra YK, Trehan N. Outcomes of coronary artery bypass grafting and reduction annuloplasty for functional ischaemic mitral regurgitation:a prospective multicenter study (Randomized Evaluation of a Surgical Treatment for Off-Pump Repair of the Mitral Valve) J Thorac Cardiovasc Surg. 2011 Jan;141(1):91–7. doi: 10.1016/j.jtcvs.2010.08.057. [DOI] [PubMed] [Google Scholar]
- 24.McGee EC, Gillinov AM, Blackstone EH, Rajeswaran J, Cohen G, Najam F, Shiota T, Sabik JF, Lytle BW, McCarthy PM, Cosgrove DM. Recurrent mitral regurgitation after annuloplasty for functional ischaemic mitral regurgitation. J Thorac Cardiovasc Surg. 2004;128:916–24. doi: 10.1016/j.jtcvs.2004.07.037. [DOI] [PubMed] [Google Scholar]
- 25.Aklog L, Filsoufi F, Flores KQ, et al. Does coronary artery bypass grafting alone correct moderate ischaemic mitral regurgitation? Circulation. 2001;104:168–75. doi: 10.1161/hc37t1.094706. [DOI] [PubMed] [Google Scholar]
- 26.Gelsomino S, Lorusso R, DeCicco G, Capecchi I, Rostagno C, Caciolli S, Romagnoli S, Da Broi U, Pierluigi S, Gensini GF. Five-year echocardiographic results of combined undersized mitral ring annuloplasty and coronary artery bypass grafting for chronic ischaemic mitral regurgitation. European Heart Journal. 2008;29:231–40. doi: 10.1093/eurheartj/ehm468. [DOI] [PubMed] [Google Scholar]
- 27.Sidebotham DA, Allen SJ, Gerber IL, Fayers T. Intraoperative transesophageal echocardiography for surgical repair of mitral regurgitation. J Am Soc Echocardiogr. 2014;27:345–66. doi: 10.1016/j.echo.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 28.Shakil O, Jainandunsing JS, Ilic R, Mahmood F. Ischaemic mitral regurgitation:an intraoperative echocardiographic perspective. J Cardiothorac Vasc Anesth. 2013;27:573–85. doi: 10.1053/j.jvca.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Salgo IS, Gorman JH, 3rd, Gorman RC, Jackson BM, Bowen FW, Plappert T, et al. Effect of annular shape on leaflet curvature in reducing mitral leaflet stress. Circulation. 2002;106:711–7. doi: 10.1161/01.cir.0000025426.39426.83. [DOI] [PubMed] [Google Scholar]
- 30.Jensen H. Surgical Treatment of Functional Ischaemic Mitral Regurgitation. Dan Med J. 2015;62(3):B4993. [PubMed] [Google Scholar]
- 31.Gelsomino S, Lorusso R, De Cippa G, Capecchi I, Rostagno C, Caciolli S, Romagnolo S, Ferrari M, Dabroi U, Stefano P, Gensini G. Five-year echocardiographic results of combined undersized mitral ring annuloplasty and coronary artery bypass grafting for chronic ischaemic mitral regurgitation. Eur Heart J. 2008;29:231–240. doi: 10.1093/eurheartj/ehm468. [DOI] [PubMed] [Google Scholar]
- 32.Mallidi HR, Pelletier MP, Lamb J, Desai N, Sever J, Christakis GT, et al. Late outcomes in patients with uncorrected mild to moderate mitral regurgitation at the time of isolated coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2004;127:636–44. doi: 10.1016/j.jtcvs.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 33.Kim YH, Czer LS, Soukiasian HJ, De Robertis M, Magliato KE, Blanche C, et al. Ischaemic mitral regurgitation:revascularization alone versus revascularization and mitral valve repair. Ann Thorac Surg. 2005;79:1895–901. doi: 10.1016/j.athoracsur.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 34.Wong DR, Agnihotri AK, Hung JW, Vlahakes GJ, Akins CW, Hilgenberg AD, et al. Long-term survival after surgical revascularization for moderate ischaemic mitral regurgitation. Ann Thorac Surg. 2005;80:570–7. doi: 10.1016/j.athoracsur.2005.03.034. [DOI] [PubMed] [Google Scholar]
- 35.Von Oppell UO, Stemmet F, Brink J, Commerford PJ, Heijke SA. Ischaemic mitral valve repair surgery. J Heart Valve Dis. 2000;9:64–73. [PubMed] [Google Scholar]
- 36.Agricola E, Oppizzi M, Pisani M, Meris A, Maisano F, Margonato A. Ischaemic mitral regurgitation:mechanisms and echocardiographic classification. European Journal of Echocardiography. 2008;9:207–21. doi: 10.1016/j.euje.2007.03.034. [DOI] [PubMed] [Google Scholar]
- 37.Bax JJ, Braun J, Somer ST, Klautz R, Holman ER, Versteegh MI, Boersma E, Schalij MJ, van der Wall EE, Dion RA. Restrictive annuloplasty and coronary revascularization in ischaemic mitral regurgitation results in reverse left ventricular remodeling. Circulation. 2004;110(Suppl. II):II103–II108. doi: 10.1161/01.CIR.0000138196.06772.4e. [DOI] [PubMed] [Google Scholar]
- 38.Serri K, Bouchard D, Demers P, Coutu M, Pellerin M, Carrier M, Perrault LP, Cartier R, Page P, Cossette M, Basmadjian AJ. Is a good perioperative echocardiographic result predictive of durability in ischaemic mitral valve repair? J Thorac Cardiovasc Surg. 2006;131:523–9. doi: 10.1016/j.jtcvs.2005.09.037. [DOI] [PubMed] [Google Scholar]
- 39.Tahta SA, Oury JH, Maxwell JM, Hiro SP, Duran CM. Outcome after mitral valve repair for functional ischaemic mitral regurgitation. J Heart Valve Dis. 2002;11:11–9. [PubMed] [Google Scholar]
- 40.Hung J, Otsuji Y, Handschumacher MD, Schwammenthal E, Levine RA. Mechanism of dynamic regurgitant orifice area variation in functional mitral regurgitation:physiologic insights from the proximal flow convergence technique. J Am Coll Cardiol. 1999;33:538–45. doi: 10.1016/s0735-1097(98)00570-1. [DOI] [PubMed] [Google Scholar]
- 41.Magne J, Pibarot P, Dumensil JG, Sénéchal M. Continued global left ventricular remodeling is not the sole mechanism responsible for late recurrence of ischaemic mitral regurgitation after restrictive annuloplasty. J Am Soc Echocardiogr. 2009;22:1256–64. doi: 10.1016/j.echo.2009.07.029. [DOI] [PubMed] [Google Scholar]
- 42.Wu AH, Aaronson KD, Bolling SF, Pagani FD, Welch K, Koelling TM. Impact of mitral valve annuloplasty on mortality risk in patients with mitral regurgitation and left ventricular systolic dysfunction. J Am Coll Cardiol. 2005;45:381–7. doi: 10.1016/j.jacc.2004.09.073. [DOI] [PubMed] [Google Scholar]
- 43.Srichai MB, Grimm RA, Stillman AE, et al. Ischaemic mitral regurgitation:impact of the left ventricle and mitral valve in patients with left ventricular systolic dysfunction. Ann Thorac Surg. 2005;80:170–8. doi: 10.1016/j.athoracsur.2005.01.068. [DOI] [PubMed] [Google Scholar]
- 44.Nesta F, Otsuji Y, Handschumacher MD, Messas E, Leavitt M, Carpentier A, Levine RA, Hung J. Leaflet concavity:a rapid visual clue to the presence and mechanism of functional mitral regurgitation. J Am SocEchocardiogr. 2003;16:1301–8. doi: 10.1067/j.echo.2003.09.003. [DOI] [PubMed] [Google Scholar]


