Abstract
Objective
Controversy exists regarding perceived benefits of early tracheostomy to facilitate weaning among mechanically-ventilated (MV) patients, potentially leading to significant practice-pattern variation with implications for outcomes and resource utilization. We sought to determine practice-pattern variation and outcomes associated with tracheostomy timing in the United States.
Design
In a retrospective cohort study, we identified mechanically-ventilated patients with the most common causes of respiratory failure leading to tracheostomy: pneumonia/sepsis and trauma. ‘Early tracheostomy’ was performed within the first week of MV. We determined between-hospital variation in early tracheostomy utilization and the association of early tracheostomy with patient outcomes using hierarchical regression.
Setting
2012 National Inpatient Sample.
Patients
6,075 pneumonia/sepsis patients and 12,030 trauma patients with tracheostomy.
Interventions
None
Measurements and Main Results
Trauma patients were twice as likely as pneumonia/sepsis patients to receive early tracheostomy (44.5% vs 21.7%, p<0.001). Admission to hospitals with higher early tracheostomy-to-total-tracheostomy ratios was associated with increased risk for tracheostomy among MV trauma patients (adjusted OR=1.04, 95% CI 1.01–1.07) but not pneumonia/sepsis (adjusted OR=1.00, 95% CI 0.98–1.02). We observed greater between-hospital variation in early tracheostomy rates among trauma patients (21.9% to 81.9%) compared to pneumonia/sepsis (14.9% to 38.3%) (p<0.0001). We found no evidence of improved hospital mortality. Pneumonia/sepsis patients with early tracheostomy had fewer feeding tube procedures and higher odds of discharge home.
Conclusion
Early tracheostomy is potentially overused among mechanically-ventilated trauma patients, with nearly half of tracheostomies performed within the first week of MV and large unexplained hospital variation, without clear benefits. Future studies are needed to characterize potentially differential benefits for early tracheostomy between disease subgroups and to investigate factors driving hospital variation in tracheostomy timing.
Keywords: Tracheostomy; Respiration, Artificial; Pneumonia; Wounds/Injuries; United States; Outcome Assessment (Health Care)
Introduction
Nearly 1 million adults in the United States (US) required invasive mechanical ventilation (MV) in 2012.1 Many patients who require MV for more than 48 hours will require prolonged MV2 (≤21 days3 or continued after hospital discharge4). Prolonged MV generally necessitates tracheostomy; the decision to place a tracheostomy has substantial implications for quality of life, costs, morbidity, and mortality.2,5–8
The optimal timing of tracheostomy for patients who may face prolonged MV is unclear. Some studies suggest potential benefits to early tracheostomy [e.g. improved respiratory physiology9, decreased sedative use10,11, and increased mobility12]. However, recent randomized controlled trials have failed to show short- or long-term mortality benefits to early tracheostomy13,14. Given our current inability to accurately predict which patients will require prolonged MV15, delaying the decision to pursue tracheostomy may allow patients at high risk for prolonged MV to be liberated from the ventilator and avoid unnecessary tracheostomy. Although little evidence currently supports patient-centered clinical outcome benefits to early tracheostomy for patients at risk for prolonged MV, rates of early tracheostomy have been on the rise in the United States16.
Controversy surrounding the optimal timing of tracheostomy for patients predicted to require prolonged MV may lead to substantial practice-pattern variation in timing of the tracheostomy, a procedure with potentially substantial implications for patient quality of life, hospital and societal costs. How real-world variation in tracheostomy timing relates to tracheostomy utilization and outcomes is unclear. Using a nationally representative, population-based database, we sought to quantify between-hospital variation in early tracheostomy utilization and identify factors associated with between-hospital variation in tracheostomy timing. Further, we investigated the association between early tracheostomy rates and total tracheostomy utilization rates within hospitals, and explored patient outcomes associated with early tracheostomy. Some have theorized17–19 that a heterogeneous case-mix of patients included in studies of tracheostomy timing11,20–28 may obscure potential benefits of early tracheostomy; therefore, we evaluated utilization and outcomes separately among patients with the two most common indications for tracheostomy – trauma and pneumonia/sepsis.
Methods
Data Source
We used the US Agency for Healthcare Research and Quality’ Healthcare Cost and Utilization Project’s (HCUP) National Inpatient Sample (NIS) from 2012. The NIS represents a stratified probability sample of all non-federal, US, acute care hospitalizations and contains de-identified administrative claims data extrapolated from 20% of all discharges from more than 4,000 hospitals across 44 states.29
Patients
We identified adult (≥18 years) patients who required MV30 and tracheostomy31 via International Classification of Disease, Ninth Revision, Clinical Modification (ICD9-CM) procedure codes. We excluded patients with a Diagnosis Related Group for tracheostomy related to face, head, and neck pathology. Please refer to the Online Supplement Methods for specific codes and details for inclusion and exclusion criteria.
We stratified analyses based on the most common causes of prolonged respiratory failure for medical and surgical patients, determined by a frequency analysis of principal diagnoses. Pneumonia/sepsis was the most common “medical condition,” defined by an ICD9-CM principal diagnosis of pneumonia or sepsis32 without a major therapeutic operating room procedure other than tracheostomy33. Trauma was the most common “surgical condition” defined by any ICD9-CM codes for trauma.34 (Table E2)
Outcomes
We determined patient and hospital characteristics that were associated with early tracheostomy. We calculated hospital risk-adjusted early tracheostomy rates (# of early tracheostomy/# total tracheostomies) to determine between-hospital variation in timing of tracheostomy. We investigated whether MV patients admitted to hospitals utilizing more early tracheostomies were at greater risk for tracheostomy and whether hospitals with high early tracheostomy rates performed more total tracheostomy procedures among MV patients. Finally, we explored associations between early tracheostomy and hospital mortality, hospital length of stay (LOS) among survivors, discharge home, and surgical/endoscopic placement of feeding tube.
Statistical Analysis
We used survey-weighted methods to generate national estimates for variables of interest. We compared categorical variables using Chi-Square tests, and continuous variables with Student’s t-test or Wilcoxon Rank Sum tests as indicated. We used multivariable hierarchical logistic regression models35 with hospital-level random intercepts to 1) quantify between-hospital variation with individual hospital risk-adjusted early tracheostomy rates, 2) to determine factors associated with between-hospital variation, and 3) to identify outcomes associated with early tracheostomy. We measured unexplained hospital variation in early tracheostomy with intra-class correlation coefficients36 and compared between-hospital variation for trauma and pneumonia/sepsis using coefficients of variation.37 We used similar models to calculate hospital risk-adjusted total tracheostomy rates and determine the association between hospital risk-adjusted early tracheostomy rates and hospital risk-adjusted total tracheostomy rates. We used Spearman correlation coefficients with linear regression to demonstrate associations. With the exception of analysis of the association between hospital early tracheostomy rates and risk for receiving tracheostomy (conducted among all mechanically ventilated patients), other analyses were performed among patients receiving tracheostomy. Please refer to the Online Supplemental Methods for further details.
Sensitivity Analyses
We performed a sensitivity analysis using time-stamped procedure codes for organ supportive therapies instituted prior to tracheostomy as an alternative method to adjust for severity of illness. We performed a second sensitivity analysis excluding patients with head injuries from the trauma cohort (Online Supplemental Methods).
Statistical testing was two-tailed with alpha=0.05 conducted with SAS v9.3 (Cary, NC). This study was deemed exempt from review by the Boston University Medical Campus Institutional Review Board.
Results
We identified 82,350 (16,470 unweighted) patients who received a tracheostomy in 2012.Among the 48,920 (9,784 unweighted) cases receiving tracheostomy in 2012 who met our inclusion/exclusion criteria, we identified 12.4% (6,075 weighted; 1,215 unweighted patients) with pneumonia/sepsis among 573 hospitals and 24.6% (12,030 weighted; 2,406 unweighted patients) with trauma across 491 hospitals (Figure E1).
Factors Associated with Early Tracheostomy
Trauma patients were twice as likely as pneumonia/sepsis patients to receive an early tracheostomy (44.5% vs 21.7%, p<0.0001). Among pneumonia/sepsis cases, patient and hospital characteristics did not differ by tracheostomy timing. However, trauma patients who received an early tracheostomy tended to be younger, more likely to be white, and have fewer comorbidities than trauma patients receiving routine tracheostomy (Table 1). In multivariable analysis for both conditions, generally markers of acute illness severity (e.g. shock and acute renal failure) were associated lower odds of early tracheostomy. (Table 2, Table E4a and E4b).
Table 1.
Patient and Hospital Characteristics Based on Tracheostomy Timing
| Trauma | Pneumonia/Sepsis | |||||
|---|---|---|---|---|---|---|
| Early Tracheostomy (n=5,280) |
Routine Tracheostomy (n=6,580) |
p-value | Early Tracheostomy (n=1,300) |
Routine Tracheostomy (n=4,685) |
p-value | |
| Tracheostomy Time*, days, median (IQR) | 4.0 (4.0) | 11.5 (6.0) | <0.0001 | 5.0 (3.0) | 14.0 (6.0) | <0.0001 |
| Age (y), mean (SE) | 49.9 (0.6) | 52.9 (0.5) | 0.0002 | 64.9 (0.9) | 64.1 (0.5) | 0.46 |
| Female (%) | 25.0 | 28.5 | 0.06 | 44.6 | 46.7 | 0.55 |
| Race/Ethnicity (%) | 0.01 | 0.98 | ||||
| White | 64.9 | 61.0 | 58.1 | 59.2 | ||
| Black | 15.2 | 13.4 | 21.5 | 21.1 | ||
| Hispanic | 9.4 | 12.3 | 9.2 | 9.2 | ||
| Other& | 10.5 | 13.3 | 11.2 | 10.5 | ||
| Payer (%) | 0.0008 | 0.29 | ||||
| Medicare | 23.7 | 29.6 | 69.2 | 63.2 | ||
| Medicaid | 20.3 | 19.7 | 15.4 | 16.4 | ||
| Private Insurance | 34.8 | 35.0 | 12.3 | 14.8 | ||
| Self-Pay | 10.6 | 9.0 | 2.3 | 3.5 | ||
| Other& | 10.6 | 6.8 | 0.8 | 2.0 | ||
| Median Income of Zip Code (%) | 0.11 | 0.34 | ||||
| $1–38,999 | 38.1 | 35.5 | 34.9 | 33.2 | ||
| $39,000–47,999 | 24.8 | 23.7 | 28.2 | 24.6 | ||
| $48,000–62,999 | 21.1 | 21.0 | 21.6 | 22.6 | ||
| >$63,000 | 15.9 | 19.8 | 15.3 | 19.6 | ||
| Comorbidities (#), median (IQR) | 2.0 (3.0) | 3.0 (2.0) | <0.0001 | 5.0 (3.0) | 5.0 (3.0) | 0.75 |
| Hospital Bed Size (%) | 0.28 | 0.16 | ||||
| Small | 2.6 | 3.7 | 6.5 | 4.9 | ||
| Medium | 20.5 | 20.1 | 18.8 | 23.9 | ||
| Large | 77.0 | 76.1 | 74.6 | 71.2 | ||
| Hospital Location/Teaching Status (%) | 0.03 | 0.39 | ||||
| Rural | 0.7 | 0.8 | 2.3 | 1.2 | ||
| Urban Non-Teaching | 11.6 | 15.4 | 35.4 | 35.3 | ||
| Urban Teaching | 87.7 | 83.8 | 62.3 | 63.5 | ||
| Hospital Region (%) | <0.0001 | 0.16 | ||||
| Northeast | 13.1 | 19.5 | 21.1 | 27.7 | ||
| Midwest | 17.4 | 16.0 | 18.1 | 14.8 | ||
| South | 52.5 | 44.2 | 37.3 | 35.3 | ||
| West | 17.0 | 20.2 | 23.5 | 22.1 | ||
| Hospital Control (%) | 0.16 | 0.33 | ||||
| Government | 22.6 | 23.9 | 8.5 | 8.0 | ||
| Private (Non-Profit) | 70.0 | 66.9 | 70.8 | 75.0 | ||
| Private (Invest-Own) | 7.4 | 9.3 | 20.8 | 17.0 | ||
Abbreviations: IQR – interquartile range. y – years. SE – standard error
Defined as time from initiation of invasive mechanical ventilation to tracheostomy
Includes patients with missing data
Table 2.
Patient and Hospital Factors Associated with Early Tracheostomy
| Adjusted Odds Ratio* (95% Confidence Interval) | ||
|---|---|---|
| Trauma | Pneumonia/Sepsis | |
| Age | 1.00 (0.99–1.01) | 1.00 (0.99–1.02) |
| Female Gender | 0.80 (0.64–0.99) | 0.89 (0.65–1.22) |
| Race/Ethnicity | ||
| White | Ref | Ref |
| Black | 1.26 (0.94–1.71) | 1.03 (0.68–1.55) |
| Hispanic | 0.87 (0.62–1.22) | 1.00 (0.56–1.77) |
| Other& | 0.90 (0.66–1.23) | 1.24 (0.74–2.09) |
| Payer | ||
| Medicare | Ref | Ref |
| Medicaid | 1.08 (0.77–1.51) | 0.95 (0.59–1.53) |
| Private Insurance | 1.06 (0.80–1.41) | 0.77 (0.47–1.27) |
| Self-Pay | 1.22 (0.82–1.82) | 0.62 (0.23–1.69) |
| Other& | 1.46 (0.98–2.18) | 0.37 (0.08–1.84) |
| Median Income of Zip Code | ||
| $1–38,999 | Ref | Ref |
| $39,000–47,999 | 1.01 (0.79–1.30) | 1.14 (0.77–1.70) |
| $48,000–62,999 | 1.01 (0.77–1.32) | 0.97 (0.63–1.49) |
| >$63,000 | 0.99 (0.73–1.34) | 0.87 (0.53–1.42) |
| Major Operating Room Procedure | 0.88 (0.69–1.12) | N/A |
| Hospital Bed Size | ||
| Small | Ref | Ref |
| Medium | 1.52 (0.75–3.08) | 0.57 (0.27–1.19) |
| Large | 1.54 (0.80–2.99) | 0.74 (0.37–1.48) |
| Hospital Location/Teaching Status | ||
| Rural | Ref | Ref |
| Urban Non-Teaching | 1.15 (0.32–4.13) | 0.44 (0.13–1.52) |
| Urban Teaching | 1.29 (0.37–4.42) | 0.49 (0.15–1.65) |
| Hospital Region | ||
| Northeast | Ref | Ref |
| Midwest | 1.78 (1.17–2.70) | 1.36 (0.80–2.30) |
| South | 1.57 (1.07–2.29) | 1.28 (0.80–2.04) |
| West | 1.48 (0.96–2.27) | 1.31 (0.79–2.23) |
| Hospital Control | ||
| Government | Ref | Ref |
| Private (Non-Profit) | 1.11 (0.79–1.56) | 0.83 (0.44–1.57) |
| Private (Invest-Own) | 0.87 (0.50–1.52) | 1.00 (0.53–2.10) |
| Shock | 0.67 (0.53–0.85) | 0.58 (0.42–0.79) |
| Renal Failure | 0.61 (0.47–0.79) | 0.55 (0.39–0.77) |
| Hematologic Failure | 0.78 (0.60–1.02) | 0.90 (0.60–1.33) |
| Hepatic Failure | 0.40 (0.18–0.92) | 0.94 (0.51–1.70) |
| Neurologic Failure | 1.04 (0.82–1.31) | 0.92 (0.67–1.27) |
| Metabolic Acidosis | 0.90 (0.68–1.18) | 0.98 (0.68–1.40) |
Hierarchical logistic regression models with hospital-level random effects were adjusted for patient demographics (age, gender, race/ethnicity, primary insurance payer, and median income of patient’s zip code), hospital characteristics (bed size, location/teaching status, region, and hospital control/ownership), presence of a major therapeutic operating room procedure in the trauma cohort, Elixhauser comorbidities, and acute organ failures
Includes patients with missing data
Hospital-Level Early Tracheostomy Variation
We identified greater between-hospital variation in hospital risk-adjusted early tracheostomy rates for patients with trauma (risk adjusted early tracheostomy rate range: 21.9 to 81.9%, coefficient of variation 22.7%, 95% CI 21.3–24.3%) than patients with pneumonia/sepsis (range: 14.9 to 38.3%, coefficient of variation 17.3% 95% CI 16.3–18.4%) (p<0.0001 for comparison of coefficients of variation) (Figure 1). After adjusting for patient and hospital characteristics, we found that 16.0%, (95% CI 12.1–22.1%) of between-hospital variation in early tracheostomy rates was unexplained by measured patient or hospital factors for trauma patients and 11.2%, (95% CI 5.9–27.5%) of variation was unexplained for patients with pneumonia/sepsis (p=0.33).
Figure 1.
Between-Hospital Variation in Risk-Adjusted Early Tracheostomy Rates. (A) Patients with trauma. (B) Patients with pneumonia/sepsis. The x-axis intersects the y-axis at the national unadjusted early tracheostomy rate for each condition. The error bars indicate 95% confidence for hospital risk-adjusted early tracheostomy rates towards the national average early tracheostomy rate only for hospitals whose practice-patterns significantly deviated from the national average.
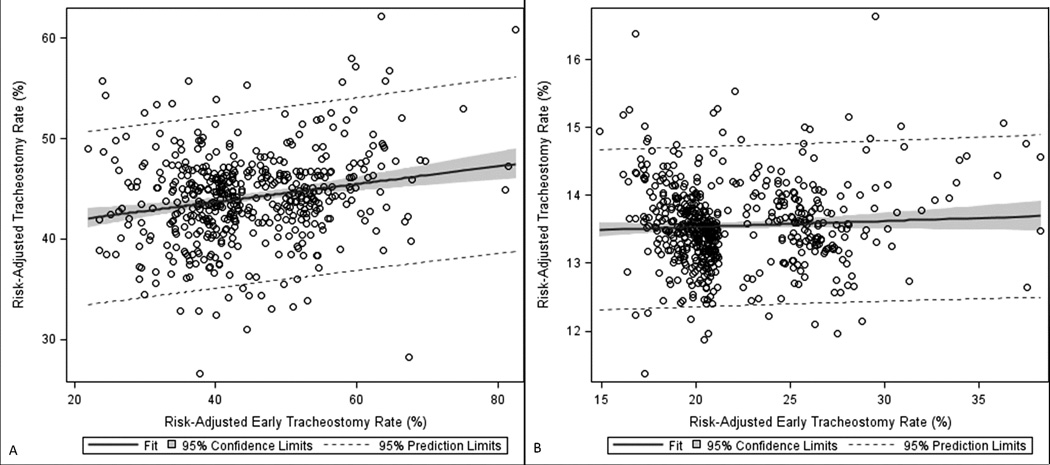
Hospital with higher risk-adjusted early tracheostomy rates tended to have higher risk-adjusted total tracheostomy rates for patients with trauma (r = 0.17, p<0.0001) but not pneumonia/sepsis (r = −0.07, p=0.11) (Figure 2). Additionally, MV trauma patients admitted to a hospital with higher early tracheostomy rates were more likely to receive tracheostomy than MV patients at hospitals with lower early tracheostomy rates (adjusted OR per 10% increase in early tracheostomy rate = 1.04, 95% CI 1.01–1.07) but not MV pneumonia/sepsis patients (adjusted OR per 10% increase in early tracheostomy rate = 1.00, 95% CI 0.98–1.02).
Figure 2.
Risk-Adjusted Early Tracheostomy Rates verses Risk-Adjusted Total tracheostomy Rates. We determined the correlation of hospital risk-adjusted early tracheostomy rates with hospital risk-adjusted total tracheostomy rates. (A) Trauma – r = 0.17, p<0.0001. (B) Pneumonia/Sepsis – r = −0.07, p=0.11.
Outcomes
In-hospital mortality did not differ based on tracheostomy timing for either trauma or pneumonia/sepsis (Table 3). Among pneumonia/sepsis patients, we observed higher odds of discharge home (adjusted OR=1.75, 95% CI 1.02–3.01), and lower odds of surgical/endoscopic feeding tube procedures (adjusted OR=0.64, 95% CI 0.48–0.86) with early tracheostomy compared to routine tracheostomy, findings that were not observed among patients with trauma. We also identified significantly shorter hospital LOS among survivors for early tracheostomy compared to routine tracheostomy for pneumonia/sepsis (median 17.0 vs 26.0 days; adjusted RR=0.75, 95% CI 0.69–0.81) and trauma (median 23.0 vs 31.0 days; adjusted RR 0.82, 95% CI 0.78–0.86).
Table 3.
Association of Early Tracheostomy with Patient-Centered Outcomes
| Trauma | Pneumonia/Sepsis | |||||
|---|---|---|---|---|---|---|
| Early Tracheostomy (n=5,995) |
Routine Tracheostomy (n=7,045) |
aOR* (95% CI) |
Early Tracheostomy (n=1,600) |
Routine Tracheostomy (n=5,185) |
aOR* (95% CI) |
|
| Survivor Length of Stay, median d, (IQR) | 23.0 (17.0) | 31.0 (21.0) | 0.82+ (0.78–0.86) | 17.0 (12.0) | 26.0 (16.0) | 0.75+ (0.69–0.81) |
| Hospital Mortality (%) | 6.4 | 9.1 | 0.98 (0.69–1.41) | 14.2 | 17.2 | 0.93 (0.61–1.42) |
| Discharged Home (%) | 18.5 | 13.6 | 1.09 (0.86–1.39) | 9.2 | 7.0 | 1.75 (1.02–3.01) |
| Feeding Tube (%) | 51.0 | 51.9 | 1.15 (0.94–1.40) | 39.2 | 50.7 | 0.64 (0.48–0.86) |
Abbreviations: aOR – adjusted odds ratio. CI – confidence interval. d – days. IQR=interquartile range
Hierarchical logistic regression models with hospital-level random effects were adjusted for patient demographics (age, gender, race/ethnicity, primary insurance payer, and median income of patient’s zip code), hospital characteristics (bed size, location/teaching status, region, and hospital control/ownership), and presence of a major therapeutic operating room procedure in the trauma cohort, Elixhauser comorbidities, and acute organ failures
Adjusted mean length of stay calculated for survivors only
Indicates adjusted Relative Risk (RR)
Sensitivity Analysis
Sensitivity analyses adjusting for organ support procedures instituted prior to tracheostomy (Table E5 and Figure E2) or excluding trauma patients with head injuries (Table E6 and Figure E3) showed similar results as our primary analysis.
Discussion
In a representative, population-based sample of patients hospitalized in the US, we investigated hospital-level variation in early tracheostomy utilization and patient outcomes associated with early tracheostomy. In order to reduce confounding by case-mix that may have affected previous studies13,14,38,39, we separately examined patient populations that represent the most common indications for tracheostomy (pneumonia/sepsis and trauma). Among MV patients hospitalized with trauma, we found high utilization and wide variation in use of early tracheostomy. Although nearly half of tracheostomies placed among trauma patients were performed within the first week of MV, we did not find associations between early tracheostomy and improved patient outcomes. MV trauma patients admitted to hospitals with high early tracheostomy rates were more likely to receive a tracheostomy than similar patients admitted to hospitals performing more routinely timed tracheostomy. Thus, our findings suggest potential overuse of early tracheostomy among MV patients hospitalized with trauma.
Compared to patients with trauma, MV patients with pneumonia/sepsis underwent lower rates of early tracheostomy, with less between-hospital variation in early tracheostomy rates, and no association identified between hospital early tracheostomy rate and hospital total tracheostomy utilization. Our results also suggest higher rates of discharge home and lower rates of feeding tubes placed among patients with pneumonia/sepsis who received early tracheostomy. However, potential benefits for early tracheostomy observed for patients with pneumonia/sepsis should be viewed as hypothesis-generating: we were unable to identify patients predicted early during hospitalization to be at risk for prolonged MV who ultimately were liberated from MV prior to receiving tracheostomy. Differences in outcomes based on indication for tracheostomy suggest the need for future studies to stratify analyses based on the indication for MV.
Few studies have examined population-based, real-world tracheostomy timing practices. Nathens et al27 investigated hospital variation in tracheostomy rates (but not timing), speculating that observed variation was the result of between-hospital differences in tracheostomy timing. Our data provide support for the assertion that hospitals conducting earlier tracheostomy generally conduct more tracheostomies. Our results differed substantially from those of Scales et al,40 Villwock et al,41 and Shaw et al,42 who found that hospital mortality was lower among patients receiving early tracheostomy. Similar to results of multiple clinical trials23–26,43, we found no association between early tracheostomy and mortality. Further contrasting with findings of Villwock et al41 and Shaw et al,42 we did not identify significant racial or demographic characteristics associated with early tracheostomy, a difference likely explained by our use of methods to account for hospital-level clustering of patient characteristics.44 Differences between prior studies and our findings also reflect the importance of defining etiology of acute respiratory failure when evaluating tracheostomy practice patterns and outcomes.
High early tracheostomy rates, wide between-hospital variability, and lack of observed patient-centered outcome benefits raise concern for potential overuse of early tracheostomy among patients with trauma. Importantly, patients admitted to hospitals with high use of early tracheostomy were more likely to receive a tracheostomy, an observation that further suggests potential overuse of early tracheostomy among MV patients with trauma. Our real-world results are consistent with clinical trials demonstrating that more than 40% of patients presumed to require prolonged MV who were randomized to late tracheostomy arms were liberated from MV prior to their assigned tracheostomy date13,14, obviating need for tracheostomy. Thus, increasing rates of early tracheostomy in the United States16 may result in a substantial number of unnecessary tracheostomies, and expose patients to potential complications (adverse event rates associated with tracheostomy range from 7–39%)13,14 without strong evidence for benefits.
Hospital tracheostomy practice-patterns and outcomes differed between patients with pneumonia/sepsis and patients with trauma. Among patients with pneumonia/sepsis, fewer received early tracheostomy and between-hospital variation was lower. Although early tracheostomy rates for pneumonia/sepsis were lower than trauma, nearly one-fourth of patients with pneumonia/sepsis who received a tracheostomy had one placed early, and in some hospitals the early tracheostomy rate approached 40%. Based on our exploratory analysis of clinical outcomes, potentially patient-centered clinical outcomes following tracheostomy such as discharge home and need for a feeding tube should be evaluated in future clinical trials as we found potentially improved outcomes in these areas that have not previously been described. Differences in tracheostomy practice-patterns between mechanically ventilated patients with pneumonia/sepsis and trauma may be driven by multiple factors, including fundamental differences in underlying physiology, access to tracheostomy proceduralists, severity of illness early during hospitalization, or different views regarding tracheostomy among surgical and medical specialties. Our analysis contrasting pneumonia/sepsis and trauma demonstrated different practice-patterns and outcomes arising from the indication for tracheostomy and suggests that stratification by disease be considered for future tracheostomy studies.
In both trauma and pneumonia/sepsis, early tracheostomy was associated with shorter hospital LOS. However, whether acute care hospital LOS after tracheostomy reflects an outcome that benefits patients or society is currently unclear and warrants further study. First, we could not measure the outcomes of patients who were spared tracheostomy by waiting > 1 week to perform tracheostomy. Second, shorter acute care hospital LOS was coupled with higher rates of discharge to long-term care facilities; whether overall burdens on the health care system are reduced by shorter acute hospital LOS45,46 when patients who received early tracheostomy spend unknown lengths of time in long term care hospitals is also unclear. Patients with tracheostomy and prolonged mechanical ventilation have significant morbidity and mortality after acute care hospital discharge7; because the ‘full picture’ of patients’ trajectories post-discharge is unavailable in the NIS data, we cannot currently advocate for increased early tracheostomy rates with the goal of shorter acute care hospital LOS.
Factors driving the potential overuse of early tracheostomy are unclear. We speculate that a number of processes may result in high early tracheostomy utilization. Although mortality has not been shown to be improved with early tracheostomy, some physicians may pursue early tracheostomy for other perceived benefits such as improved respiratory physiology9, decreased sedative use10,11, and increased mobility12. Future studies should investigate outcomes of tracheostomy that are most important to patients, as well as how use of shared decision-making tools for patients facing prolonged mechanical ventilation47,48 may affect variation in tracheostomy timing practices. We also encourage further studies to investigate how regional differences in healthcare economics or local availability of long term care hospitals may potentially contribute to variation in tracheostomy timing.
Our study has several limitations. We used administrative data which relies on ICD9-CM and DRG coding to identify patients and may suffer from misclassification biases. However, MV and tracheostomy receive high levels of reimbursement and are unlikely to be misclassified.49 While the NIS’s strength is the large sample size and national estimates, it lacks granularity which can lead to unmeasured confounding. Our findings regarding a lack of mortality benefits and potentially beneficial outcomes among patients with pneumonia/sepsis should be further interpreted in light of a potential bias towards improved outcomes for patients receiving early tracheostomy, who appeared to have lower severity of illness. Greater severity of illness identified among patients with later tracheostomy may also indicate a decision to delay the procedure until patients were more stable, thus unmeasured severity of illness between hospitals has potential to confound our estimates of hospital variation. Furthermore, outcomes measured at the time of hospital discharge may inadequately capture patient-centered outcomes as multiple significant events in the care of patients with tracheostomy occur post-discharge7. Furthermore, several trials and meta-analyses related to tracheostomy timing14,17,19,50 were published after 2012 and could have affected tracheostomy timing practice-patterns after our study period; changes in practice patterns after 2012 require further study. Additionally, conditions suspected at the time of admission which could have affected decisions regarding tracheostomy timing but were ultimately not confirmed, such as suspected cervical spine injury, could not be captured by the NIS. Finally, unmeasured differences in case-mix among trauma patients may also have contributed to our findings. However, reducing heterogeneity of case-mix by excluding patients with head trauma did not substantively change our results.
Conclusion
We investigated practice-patterns and outcomes associated with early tracheostomy in a nationally representative sample of US patients with two of the most common indications for tracheostomy. We observed wide between-hospital variation in early tracheostomy utilization without mortality benefits. Our findings suggest large variation and potential overuse of early tracheostomy for trauma patients, with high hospital rates of early tracheostomy associated with increased risk for receiving any tracheostomy. Drivers of decisions to pursue earlier tracheostomy are unclear and future studies are needed to investigate clinician and local health system factors that may influence large variation regarding tracheostomy timing in the US. Observed differences in non-mortality outcomes for early tracheostomy based on etiology of respiratory failure also require further study. Future studies should examine non-mortality outcomes of prolonged mechanical ventilation that matter most to patients, and focus on long-term, patient centered outcomes among patients at risk for prolonged mechanical ventilation.
Supplementary Material
Acknowledgments
Funding: This material is the result of work supported in part by NIH T32 86308 (ABM), AHRQ K08HS020672 (CRC), NIH NHLBI K01HL116768 (AJW). This study was also supported by resources from a Boston University School of Medicine Department of Medicine Career Investment Award (AJW) and the Edith Nourse Rogers Memorial VA Hospital, Bedford, MA (RSW). The funding agencies did not have a role in the conduct of the study, in the collection, management, analysis, interpretation of data, or in the preparation of the manuscript.
Copyright form disclosures: Dr. Mehta received support for article research from the National Institutes of Health (NIH). His institution received funding from the NIH, Agency For Healthcare Research and Quality (AHRQ), and NIH NHLBI. Dr. Cooke’s institution received funding from the AHRQ. Dr. Wiener received support for article research from the NIH. Her institution received funding from the NIH. Dr. Walkey received support for article research from the NIH and received funding from UpToDate. His institution received funding from the NIH/NHLBI and Wallace Coulter Foundation.
Footnotes
Author Contributions: ABM: Study and database design, statistical analysis, principal manuscript preparation. CRC: Study design, manuscript preparation. RSW: Study and database design, manuscript preparation. AJW: Study design, statistical analysis, manuscript preparation, study supervision.
Disclosures: No authors listed have any financial, professional or personal conflicts of interest of disclosures.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the US Government.
References
- 1.HCUPnet. Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality. [Accessed 2015 May 20]; Available online at: http://hcupnet.ahrq.gov/
- 2.Carson SS, Bach PB. The epidemiology and costs of chronic critical illness. Crit Care Clin. 2002;18:461–476. doi: 10.1016/s0749-0704(02)00015-5. [DOI] [PubMed] [Google Scholar]
- 3.MacIntyre NR, Epstein SK, Carson S, et al. Management of patients requiring prolonged mechanical ventilation: Report of a NAMDRC consensus conference. Chest. 2005;128:3937–3954. doi: 10.1378/chest.128.6.3937. [DOI] [PubMed] [Google Scholar]
- 4.Scheinhorn DJ, Hassenpflug MS, Votto JJ, et al. Ventilator-dependent survivors of catastrophic illness transferred to 23 long-term care hospitals for weaning from prolonged mechanical ventilation. Chest. 2007;131:76–84. doi: 10.1378/chest.06-1079. [DOI] [PubMed] [Google Scholar]
- 5.Cox CE, Carson SS, Govert JA, et al. An economic evaluation of prolonged mechanical ventilation. Crit Care Med. 2007;35:1918–1927. doi: 10.1097/01.CCM.0000275391.35834.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cox CE, Carson SS, Lindquist JH, et al. Differences in one-year health outcomes and resource utilization by definition of prolonged mechanical ventilation: A prospective cohort study. Crit Care. 2007;11:R9. doi: 10.1186/cc5667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unroe M, Kahn JM, Carson SS, et al. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: A cohort study. Ann Intern Med. 2010;153:167–175. doi: 10.1059/0003-4819-153-3-201008030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kahn JM, Werner RM, David G, et al. Effectiveness of long-term acute care hospitalization in elderly patients with chronic critical illness. Med Care. 2013;51:4–10. doi: 10.1097/MLR.0b013e31826528a7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brook AD, Sherman G, Malen J, et al. Early versus late tracheostomy in patients who require prolonged mechanical ventilation. Am J Crit Care. 2000;9:352–359. [PubMed] [Google Scholar]
- 10.Nieszkowska A, Combes A, Luyt CE, et al. Impact of tracheotomy on sedative administration, sedation level, and comfort of mechanically ventilated intensive care unit patients. Crit Care Med. 2005;33:2527–2533. doi: 10.1097/01.ccm.0000186898.58709.aa. [DOI] [PubMed] [Google Scholar]
- 11.Trouillet JL, Luyt CE, Guiguet M, et al. Early percutaneous tracheotomy versus prolonged intubation of mechanically ventilated patients after cardiac surgery: A randomized trial. Ann Intern Med. 2011;154:373–383. doi: 10.7326/0003-4819-154-6-201103150-00002. [DOI] [PubMed] [Google Scholar]
- 12.Clum SR, Rumbak MJ. Mobilizing the patient in the intensive care unit: The role of early tracheotomy. Crit Care Clin. 2007;23:71–79. doi: 10.1016/j.ccc.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 13.Terragni PP, Antonelli M, Fumagalli R, et al. Early vs late tracheotomy for prevention of pneumonia in mechanically ventilated adult ICU patients: A randomized controlled trial. JAMA. 2010;303:1483–1489. doi: 10.1001/jama.2010.447. [DOI] [PubMed] [Google Scholar]
- 14.Young D, Harrison DA, Cuthbertson BH, et al. Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation: The TracMan randomized trial. JAMA. 2013;309:2121–2129. doi: 10.1001/jama.2013.5154. [DOI] [PubMed] [Google Scholar]
- 15.Figueroa-Casas JB, Connery SM, Montoya R, et al. Accuracy of early prediction of duration of mechanical ventilation by intensivists. Ann Am Thorac Soc. 2014;11:182–185. doi: 10.1513/AnnalsATS.201307-222OC. [DOI] [PubMed] [Google Scholar]
- 16.Mehta AB, Syeda SN, Bajpayee L, et al. Trends in tracheostomy for mechanically ventilated patients in the United States, 1993–2012. Am J Respir Crit Care Med. 2015;192:446–454. doi: 10.1164/rccm.201502-0239OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andriolo BN, Andriolo RB, Saconato H, et al. Early versus late tracheostomy for critically ill patients. Cochrane Database Syst Rev. 2015;1:CD007271. doi: 10.1002/14651858.CD007271.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Griffiths J, Barber VS, Morgan L, et al. Systematic review and meta-analysis of studies of the timing of tracheostomy in adult patients undergoing artificial ventilation. BMJ. 2005;330:1243. doi: 10.1136/bmj.38467.485671.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu CC, Livingstone D, Dixon E, et al. Early versus late tracheostomy: A systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2014 doi: 10.1177/0194599814561606. [DOI] [PubMed] [Google Scholar]
- 20.Blot F, Guiguet M, Antoun S, et al. Early tracheotomy in neutropenic, mechanically ventilated patients: Rationale and results of a pilot study. Support Care Cancer. 1995;3:291–296. doi: 10.1007/BF00335304. [DOI] [PubMed] [Google Scholar]
- 21.Rumbak MJ, Newton M, Truncale T, et al. A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med. 2004;32:1689–1694. doi: 10.1097/01.ccm.0000134835.05161.b6. [DOI] [PubMed] [Google Scholar]
- 22.Zheng Y, Sui F, Chen XK, et al. Early versus late percutaneous dilational tracheostomy in critically ill patients anticipated requiring prolonged mechanical ventilation. Chin Med J (Engl) 2012;125:1925–1930. [PubMed] [Google Scholar]
- 23.Bouderka MA, Fakhir B, Bouaggad A, et al. Early tracheostomy versus prolonged endotracheal intubation in severe head injury. J Trauma. 2004;57:251–254. doi: 10.1097/01.ta.0000087646.68382.9a. [DOI] [PubMed] [Google Scholar]
- 24.Ahmed N, Kuo YH. Early versus late tracheostomy in patients with severe traumatic head injury. Surg Infect (Larchmt) 2007;8:343–347. doi: 10.1089/sur.2006.065. [DOI] [PubMed] [Google Scholar]
- 25.Alali AS, Scales DC, Fowler RA, et al. Tracheostomy timing in traumatic brain injury: A propensity-matched cohort study. J Trauma Acute Care Surg. 2014;76:70–76. doi: 10.1097/TA.0b013e3182a8fd6a. discussion 76-8. [DOI] [PubMed] [Google Scholar]
- 26.Barquist ES, Amortegui J, Hallal A, et al. Tracheostomy in ventilator dependent trauma patients: A prospective, randomized intention-to-treat study. J Trauma. 2006;60:91–97. doi: 10.1097/01.ta.0000196743.37261.3f. [DOI] [PubMed] [Google Scholar]
- 27.Nathens AB, Rivara FP, Mack CD, et al. Variations in rates of tracheostomy in the critically ill trauma patient. Crit Care Med. 2006;34:2919–2924. doi: 10.1097/01.CCM.0000243800.28251.AE. [DOI] [PubMed] [Google Scholar]
- 28.Dunham CM, Ransom KJ. Assessment of early tracheostomy in trauma patients: A systematic review and meta-analysis. Am Surg. 2006;72:276–281. doi: 10.1177/000313480607200316. [DOI] [PubMed] [Google Scholar]
- 29.Overview of the National (Nationwide) Inpatient Sample (NIS) Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality. [Accessed 2014 December 18]; Available online at: http://www.hcup-us.ahrq.gov/nisoverview.jsp.
- 30.Mehta AB, Syeda SN, Wiener RS, et al. Epidemiological trends in invasive mechanical ventilation in the United States: A population-based study. J Crit Care. 2015;30:1217–1221. doi: 10.1016/j.jcrc.2015.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quan H, Parsons GA, Ghali WA. Validity of procedure codes in international classification of diseases, 9th revision, clinical modification administrative data. Med Care. 2004;42:801–809. doi: 10.1097/01.mlr.0000132391.59713.0d. [DOI] [PubMed] [Google Scholar]
- 32.Lindenauer PK, Lagu T, Shieh MS, et al. Association of diagnostic coding with trends in hospitalizations and mortality of patients with pneumonia, 2003–2009. JAMA. 2012;307:1405–1413. doi: 10.1001/jama.2012.384. [DOI] [PubMed] [Google Scholar]
- 33.Procedure Classes 2015. Healthcare Cost and Utilization Project (HCUP). Agency for Healthcare Research and Quality. [Accessed 2014 December 18]; Available online at: http://www.hcup-us.ahrq.gov/toolssoftware/procedure/procedure.jsp.
- 34.Hicks CW, Hashmi ZG, Velopulos C, et al. Association between race and age in survival after trauma. JAMA Surg. 2014;149:642–647. doi: 10.1001/jamasurg.2014.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Houchens R, Chu B, Steiner C. Hierarchical modeling using HCUP data. HCUP methods series report # 2007-01 online. U.S. Agency for Healthcare Research and Quality; 2007. Online. [Google Scholar]
- 36.Seymour CW, Iwashyna TJ, Ehlenbach WJ, et al. Hospital-level variation in the use of intensive care. Health Serv Res. 2012;47:2060–2080. doi: 10.1111/j.1475-6773.2012.01402.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.A Likelihood Ratio Test of the Equality of the Coefficients of Variation of k Normally Distributed Populations. United States Forest Service; [Accessed 2015 July 28]. Available online at: http://www1.fpl.fs.fed.us/covtestk.html. [Google Scholar]
- 38.Arabi YM, Alhashemi JA, Tamim HM, et al. The impact of time to tracheostomy on mechanical ventilation duration, length of stay, and mortality in intensive care unit patients. J Crit Care. 2009;24:435–440. doi: 10.1016/j.jcrc.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 39.Blot F, Similowski T, Trouillet JL, et al. Early tracheotomy versus prolonged endotracheal intubation in unselected severely ill ICU patients. Intensive Care Med. 2008;34:1779–1787. doi: 10.1007/s00134-008-1195-4. [DOI] [PubMed] [Google Scholar]
- 40.Scales DC, Thiruchelvam D, Kiss A, et al. The effect of tracheostomy timing during critical illness on long-term survival. Crit Care Med. 2008;36:2547–2557. doi: 10.1097/CCM.0b013e31818444a5. [DOI] [PubMed] [Google Scholar]
- 41.Villwock JA, Jones K. Outcomes of early versus late tracheostomy: 2008–2010. Laryngoscope. 2014;124:1801–1806. doi: 10.1002/lary.24702. [DOI] [PubMed] [Google Scholar]
- 42.Shaw JJ, Santry HP. Who gets early tracheostomy?: Evidence of unequal treatment at 185 academic medical centers. Chest. 2015 doi: 10.1378/chest.15-0576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sugerman HJ, Wolfe L, Pasquale MD, et al. Multicenter, randomized, prospective trial of early tracheostomy. J Trauma. 1997;43:741–747. doi: 10.1097/00005373-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 44.Mayr FB, Yende S, D'Angelo G, et al. Do hospitals provide lower quality of care to black patients for pneumonia? Crit Care Med. 2010;38:759–765. doi: 10.1097/CCM.0b013e3181c8fd58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Angus DC. When should a mechanically ventilated patient undergo tracheostomy? JAMA. 2013;309:2163–2164. doi: 10.1001/jama.2013.6014. [DOI] [PubMed] [Google Scholar]
- 46.Scales DC. The implications of tracheostomy for discharge destination. Am J Respir Crit Car Med. 2015;192:404–405. doi: 10.1164/rccm.201505-1007ED. [DOI] [PubMed] [Google Scholar]
- 47.Cox CE, Lewis CL, Hanson LC, et al. Development and pilot testing of a decision aid for surrogates of patients with prolonged mechanical ventilation. Crit Care Med. 2012;40:2327–2334. doi: 10.1097/CCM.0b013e3182536a63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cox CE, Wysham NG, Walton B, et al. Development and usability testing of a web-based decision aid for families of patients receiving prolonged mechanical ventilation. Ann Intensive Care. 2015;5 doi: 10.1186/s13613-015-0045-0. 6-015-0045-0. eCollection 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wynn BO, Beckett MK, Hillborne LH, Scott MM, Bahney B. Evaluations of Severity-Adjusted DRG Systems: Report WR-434-CMS. RAND Corporation. [Accessed 2014 August 21]; Available online at: www.rand.org/pubs/working_papers/WR434/ [Google Scholar]
- 50.Siempos II, Ntaidou TK, Filippidis FT, et al. Effect of early versus late or no tracheostomy on mortality and pneumonia of critically ill patients receiving mechanical ventilation: A systematic review and meta-analysis. Lancet Respir Med. 2015;3:150–158. doi: 10.1016/S2213-2600(15)00007-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.