Abstract
Objective
This study evaluates a parent-teen skills-based therapy for ADHD blended with motivational interviewing (MI) to enhance family engagement. Supporting Teens’ Academic Needs Daily (STAND) is an adolescent-specific treatment for ADHD that targets empirically identified adolescent (i.e., organization, time management, and planning; OTP skills) and parent-based (i.e., monitoring and contingency management) mechanisms of long-term outcome through individual parent-teen sessions.
Method
The current randomized trial (N=128) evaluates efficacy at post-treatment and six-month follow-up. Participants were ethnically diverse teens (7.7% non-Hispanic White, 10.8% African-American, 78.5% Hispanic, 3.0% other) randomly assigned to STAND or Treatment As Usual (TAU).
Results
Primary findings were that: (1) STAND was delivered in an MI-adherent fashion and most families fully engaged in treatment (85% completed), (2) STAND produced a range of significant acute effects on ADHD symptoms, OTP skills, homework behavior, parent-teen contracting, implementation of home privileges, parenting stress, and daily homework recording, and (3) six months after treatment ceased, effects on ADHD symptom severity, OTP skills, and parenting stress maintained, while parent use of contracting and privilege implementation strategies, as well as teen daily homework recording and homework behavior gains, were not maintained.
Conclusions
Skills-based behavior therapy blended with MI is an acutely efficacious treatment for adolescents with ADHD although more work is needed to establish the nature of long-term effects.
Public Health Significance
A skills-based parent-teen behavior therapy blended with MI successfully engages families and leads to long-term improvement in parent-reported ADHD symptoms, organization skills, and parenting stress. Effects on school setting variables were less robust, requiring continued work to enhance these outcomes.
Attention Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder characterized by impairing levels of inattention, overactivity, and poor impulse control that affects 5–10% of individuals (Centers for Disease Control, 2013). Though historically characterized as a childhood disorder, it is now well accepted that ADHD continues to afflict adolescents and adults (Molina et al., 2009) and is associated with very negative adult outcomes (e.g., criminal behavior, high school dropout, drug abuse, educational and vocational underachievement; Barkley, Fischer, Smallish, & Fletcher, 2002; Hechtman et al., 2015; Mannuzza, Klein, & Mouton, 2008), even after controlling for the influence of comorbidities (Barkley, Murphy, & Fischer, 2008).
Longitudinal studies reveal that ADHD treatments delivered in childhood (i.e., stimulant medication, behavioral interventions) do not prevent long-term negative outcomes (Biederman et al., 2008; Mannuzza et al., 2008; Molina et al., 2009). In fact, level of functioning during the critical adolescent years appears to be more indicative of adjustment in adults with ADHD (Molina et al., 2012, 2014; Sibley, Pelham, et al., 2014). For example, in the Multimodal Treatment of ADHD study (MTA), assigned treatment group (medication, behavior management, combined, and community control) did not differ on any of 30 outcomes at eight years after baseline, indicating that the initial relative benefits of medication and behavioral treatments disappeared by adolescence (Molina et al., 2009). By contrast, ADHD symptom persistence through adolescence was the strongest predictor of young adult vocational, educational, substance use, criminal, and risky sexual outcomes (Hechtman et al., 2015). Thus, when childhood treatments fail to produce long-term effects, successfully treated children with ADHD may return to maladjustment in adolescence, and these problems often escalate over time (Molina et al., 2012, 2014). As a result, effective treatment of ADHD must include continued intervention delivery past childhood (Sibley, Kuriyan, Evans, Waxmonsky & Smith, 2014) to target symptom desistance and impairment reduction during the teen years.
There may be multiple reasons that childhood treatments fail to influence teen functioning. First, changing environmental demands in adolescence require new skills. For example, at the transition to secondary school, the academic environment becomes increasingly complex as students must independently transition between classes with separate teachers, keep track of assigned work and deadlines, and complete multistep academic tasks and projects (Eccles, 2004). Second, from a social-developmental perspective, the adolescent period marks a time in which normative teen autonomy seeking and identity building processes require navigation of increasingly complex relationships with parents and peers that may influence the adolescent’s functioning (Steinberg & Morris, 2001). Third, from a biological perspective, important changes in brain function occur during the adolescent period with the onset of puberty (Sisk & Foster, 2004). For example, dopaminergic circuits produce particularly strong responses to socially and emotionally rewarding stimuli at a time when prefrontal regions that inhibit behavioral impulses remain underdeveloped (Casey, Jones, & Hare, 2008). As such, many adolescents gravitate toward activities with perceived high incentives (i.e., social media, video games, substance use, rule breaking behaviors, risky sexual behavior), even when choosing to engage in these behaviors incurs serious negative consequences (i.e., neglect of responsibilities, legal problems, pregnancy, addiction; Flory et al., 2007; Molina et al., 2012).
Adolescents with ADHD possess specific deficits that exacerbate each of the above new challenges. First, executive functioning (i.e., organization, time management, and planning; OTP) and motivation deficits (i.e., aversion to boring or difficult tasks) are prominent among teens with ADHD (Sonuga-Barke, 2003). These neurocognitive deficits may prevent mastery of secondary school demands when teens with ADHD tend toward disorganization, forgetfulness, and schoolwork avoidance (Langberg, Dvorsky, & Evans, 2013). Furthermore, the effects of these deficits on academic and household tasks may lead to increased arguments with parents (Medina & Sibley, 2015), while a teen with ADHD’s verbal impulsivity may increase the intensity of normative parent-teen arguments about independence and limit-setting (Edwards, Barkley, Laneri, Fletcher, & Metevia, 2001). Finally, the executive functioning and motivation problems endemic to ADHD (Toplak, Jain, & Tannock, 2005) further exacerbate irresponsible adolescent decision-making (Casey et al., 2008), leading teens with ADHD to elevated rates of risky, rule-breaking, and idle behavior (Chan & Rabinowitz, 2006; Lee & Hinshaw, 2004).
Contemporary psychosocial interventions for adolescents with ADHD (i.e., Challenging Horizons Program; Evans, Schultz, DeMars, & Davis, 2011; Homework, Organization, and Planning Skills; Langberg, Epstein, Becker, Girio-Herrera, & Vaughn, 2012) teach teens compensatory skills for OTP problems and engage adults (i.e., teachers, college students, school counselors) in contingency management to promote skill use in the presence of motivation deficits. These treatments produce sizable effects across a range of adolescent domains and are primarily delivered in school settings (for review: Sibley, Kuriyan, et al., 2014). Despite demonstrated efficacy in controlled trials (Evans et al., 2011; Langberg et al., 2012; Molina et al., 2008), adolescent-specific treatments for ADHD remain underutilized. For example, in a large follow-up study of children with ADHD, Bussing and colleagues (2011) reported that a majority of impaired adolescents with ADHD (58%) had not received mental health services in the past year. Similarly, the Pittsburgh ADHD Longitudinal Study reported steadily declining treatment utilization in adolescence such that only 20% of older teens with ADHD received psychosocial treatment in the past year (Biswas et al., 2009). Notably, desistance of psychosocial treatment and stimulant medication occurs at a similar rate during adolescence. Despite rising rates of prescriptions to adolescents (Visser et al., 2014), a majority of teens with validated ADHD diagnoses report finding their medications unpalatable and decline to take them (Biswas et al., 2009; Molina et al., 2009). As a result, most individuals with ADHD are untreated during the critical adolescent years.
One source of treatment underutilization may be that skills-based treatments for adolescents with ADHD remain undeveloped for clinical settings. This trend is surprising as clinic-based approaches are successful at teaching developmentally relevant skills to younger children with ADHD (Abikoff et al., 2013; Power et al., 2012) and at reducing conflict between adolescents with ADHD and their parents (Barkley, Guevremont, Anastopoulos, & Fletcher, 1992; Barkley, Edwards, Laneri, Fletcher, & Metevia, 2001). Clinic-based treatment of teens allows for the involvement of parents, which promotes remediation of problems at home (in addition to school). Parent involvement components are critical to the treatment of most adolescent mental health disorders (i.e., conduct problems: Henggeler & Lee, 2003; substance use; Liddle et al., 2001; eating disorders: Le Grange, Lock, Loeb & Nicholls, 2010; suicide prevention: King, Hovey, Brand, Wilson, & Ghaziuddin, 1997). As adolescents increase their independence, parents remain a key to these treatments due to their influence on adolescent behavior and ability to supervise and reinforce therapy skills practice (Weisz & Hawley, 2002).
A primary reason for underutilization of clinic-based approaches may be difficulty engaging parents and teens with ADHD in collaborative therapy. Prior to the development of skills-based OTP interventions, the promise of clinical interventions for adolescents with ADHD was demonstrated in two evaluations (Barkley et al., 1992, 2001). These studies reported significant reductions in home conflict over time for families of teens with ADHD who completed parent behavior management and problem solving communication training. One important finding of these studies was notable attrition (up to 38% of families failed to complete treatment), which the authors attributed to poor engagement by conflict-ridden dyads, who may perceive treatment as an additional source of arguments (Barkley et al., 2001; Weisz & Hawley, 2002). This finding is not surprising as: (1) teens with ADHD report relatively low willingness to attend therapy (Bussing et al., 2012), (2) parents of teens with ADHD may struggle with their own ADHD symptoms and subsequently fail to engage in treatment (Chronis et al., 2011), and (3) parents of teens with ADHD tend not to engage in school-based OTP treatments when invited to do so (Evans et al., 2011). Thus, successful parent-teen collaborative interventions for adolescents with ADHD may require targeted engagement components to optimize uptake, completion, and efficacy.
In consideration of these factors, we designed a clinic-based OTP skills intervention for adolescents with ADHD delivered in the style of Motivational Interviewing (MI; Miller & Rollnick, 2013) to enhance parent and teen engagement in therapy. Supporting Teens’ Academic Needs Daily (STAND; BLINDED) targets empirically identified adolescent (e.g., OTP skills, motivation deficits) and parent-based (e.g., behavior management strategies to promote appropriate home structure and independent teen skill practice) mechanisms of outcome. STAND employs MI to support parents in considering changes to their parenting practices and to increase adolescent openness to treatment. In consideration of the heterogeneous deficits and circumstances of families of teens with ADHD, we designed a flexible manual that offers families autonomy in choosing skills that they would like to learn during treatment.
In a pilot evaluation of STAND (BLINDED), 36 school staff-referred adolescents with ADHD were randomly assigned to receive STAND or Treatment as Usual (TAU). All participants completed STAND and reported that it was a positive experience for their family—improving upon retention rates for parent-teen treatments in this population (e.g., Barkley et al., 2001). Overall, families rated STAND as logical, acceptable, and enjoyable, reporting high satisfaction, and therapists implemented STAND with high fidelity. In addition, compared to TAU, families who received STAND displayed large acute gains in teen academic habits (d=1.30), organization skills (d=.64–5.15), and ADHD symptom severity (d=1.42), with additional reductions in parent stress level (d=.39) and home conflict (d=.65; BLINDED).
Following the pilot evaluation, STAND’s evolution continued with the addition of increasingly sophisticated MI components to approximate a full MI-blended treatment approach (Moyers & Houck, 2011). As such, emphasis throughout the course of treatment was placed on helping the parent identify their own change goals (e.g., finding ways to motivate adolescent, reducing reminders during homework time, increasing accountability for homework completion, consistently monitoring teen after school) and revisiting progress on these goals during each session. In the spirit of MI (Miller & Rollnick, 2013), we also increased focus on seeking collaboration with family members in session planning, emphasizing parent and teen autonomy in tailoring skills components to their everyday lives, and affirming the strengths and efforts of family members as they forged new habits.
The current trial is a larger randomized evaluation of STAND’s efficacy (N=128) with a focus on parent and adolescent changes made across two settings (home and school). STAND and TAU control participants were compared over baseline (BL), post-test (PT), and six-month follow-up (FU) assessments on a multimethod battery of adolescent and parent-centered variables. We hypothesized that relative to TAU, STAND would lead to large gains across a range of home and school setting measures of adolescent functioning and parent psychological variables. Because intended treatment mechanisms were home-based, we hypothesized that effects would be larger in the home setting than in the school setting. We also hypothesized that there would be maintenance of STAND gains (relative to TAU) from PT to FU.
Method
Participants
Participants were 128 adolescents with ADHD between the ages of 11–15 in a large ethnically diverse eastern U.S. city. Participants attended 81 different schools: 77.8% attended public school in a large centralized school district and 22.2% private school. Participants were required to: (a) meet DSM-IV-TR (American Psychiatric Association, 2000) criteria for ADHD, (b) be enrolled in sixth through eighth grade, (c) display significant academic impairment, (d) have an estimated IQ > 80, and (e) have no history of an autism spectrum disorder. Placement in a self-contained classroom was exclusionary. Adolescents with comorbidities were permitted to remain in the study. Participants were randomly assigned to STAND (N=67) or TAU (N=61). Groups were matched on medication status using a stratified randomization procedure and slight over-randomization of participants to STAND was necessary to maintain medication equivalence given rolling enrollment. Parent and adolescent characteristics of each group are listed in Tables 1 and 2. Two of seventeen comparisons indicated group differences (p < .10). Participants in the STAND group had slightly higher IQ scores and higher rates of ADHD-Predominantly Inattentive Type. These two variables served as covariates in all analyses.
Table 1.
Diagnostic and Demographic Characteristics of Adolescents at Baseline
| STAND (N=67) | TAU (N=61) | |
|---|---|---|
|
|
||
| Diagnostic Variables at Baseline | ||
| WASI estimated Full-Scale IQ* | 102.77 (12.09) | 98.56 (12.57) |
| WIAT Reading Achievement | 105.31 (10.03) | 103.57 (10.25) |
| WIAT Math Achievement | 100.86 (15.25) | 97.41 (17.39) |
| ADHD Subtype* | ||
| ADHD-Predominantly Inattentive (%) | 47.8 | 29.5 |
| ADHD-Combined (%) | 52.2 | 70.5 |
| ODD/CD (%) | 53.7 | 62.3 |
| Affective Problems | 16.9 | 22.0 |
| Anxiety Problems | 18.5 | 20.3 |
| Learning Disability | 7.7 | 10.0 |
| Current ADHD Medication (%) | 34.4 | 34.4 |
| Childhood ADHD Medication (%) | 59.4 | 60.0 |
| Childhood Psychosocial Treatment (%) | 51.6 | 53.3 |
| Demographic Variables
|
||
| Age (M, SD) | 12.65 (.85) | 12.85 (.87) |
| Male (%) | 61.2 | 68.9 |
| Race/Ethnicity (%) | ||
| White Non-Hispanic | 7.7 | 10.0 |
| Black Non-Hispanic | 10.8 | 5.0 |
| Hispanic Any Race | 78.5 | 76.7 |
| Other | 3.0 | 8.3 |
Note.
Participants in the treatment group had slightly higher IQs and higher rates of ADHD-P/I subtype (p<.10). All other group differences were non-significant. Affective and Anxiety Problems represent elevated T-scores on the Youth Self Report Form (Achenbach, 1987). Learning disabilities were reported by parents at baseline.
Table 2.
Parent Characteristics at Baseline
| STAND (N=67) | TAU (N=61) | |
|---|---|---|
|
|
||
| Relationship to Teen | ||
| Mother (%) | 80.6 | 91.8 |
| Father (%) | 16.4 | 8.2 |
| Grandmother (%) | 3.0 | 0.0 |
| Parent Age | 43.38 (6.72) | 44.12 (4.78) |
| Single Parent (%) | 38.8 | 31.1 |
| Parent Education Level | ||
| High School Grad, GED, or less (%) | 10.9 | 20.8 |
| Part College or Specialized Training (%) | 23.6 | 11.3 |
| College or University Grad (%) | 43.6 | 37.7 |
| Graduate Professional Training (%) | 21.8 | 30.2 |
Note. No significant group differences on parenting variables.
Procedures
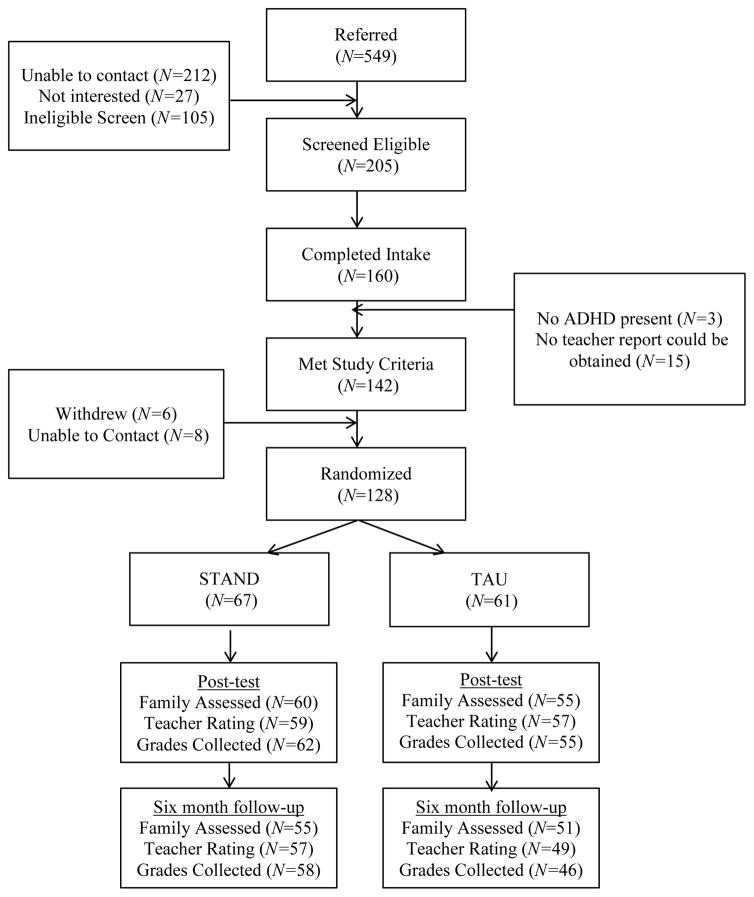
All procedures were approved by the university’s institutional review board. Participants were recruited through referral from local schools and parent inquiry at the university clinic. For all potential participants, a brief phone screen containing the DSM-IV-TR ADHD symptoms and questions about impairment was administered to the primary caretaker. Families were invited to an intake assessment if the parent endorsed on the phone screen: (1) four or more symptoms of either Inattention or Hyperactivity/Impulsivity (APA, 2000) and (2) clinically significant problems at home and school (at least a “3” on a “0 to 6” impairment scale). Figure 1 contains the study’s consort flow diagram. In total, 310 families completed a phone screen, with 205 families invited to an intake assessment. Of these, 160 families attended the intake appointment.
Figure 1.
Consort Flow Diagram
At intake, informed parental consent and youth assent were obtained. The primary caretaker participated in the assessment and treatment aspects of the project, and when available, other parents were encouraged to contribute. During intake, ADHD diagnosis was assessed through a combination of parent structured interview (Computerized-Diagnostic Interview Schedule for Children; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000) and parent and teacher ratings of symptoms and impairment, as is recommended practice (Pelham, Fabiano, & Massetti, 2005). These data were combined using an “or rule,” which identifies the presence of a symptom if endorsed by either informant (Bird, Gould, & Staghezza, 1992). Additionally, a brief intelligence test (Wechsler Abbreviated Scale of Intelligence; Wechsler, 1999), achievement testing (Wechsler Individual Achievement Test-II; Wechsler, 2002), and parent and adolescent ratings scales were administered to assess demographic information, treatment history, comorbid symptoms, and psychosocial functioning. Symptom and impairment ratings were obtained from a core academic teacher. Dual Ph.D. level clinician review was used to determine diagnosis and eligibility. As part of this process, clinicians used all available information to consider age of onset, chronicity, comorbid symptoms, and settings of impairment when making ADHD diagnoses. When disagreement occurred (twice), a third clinician was consulted. Of the 160 participants who attended an intake (see Figure 1), 142 met study criteria and 128 enrolled and were randomized to STAND or TAU. Families were enrolled in three waves (Winter 2011/2012, Fall 2012, Spring 2013) and began treatment at the commencement of the forthcoming academic quarter.
Participants in both groups were permitted to seek or continue additional medication and psychosocial treatments during the study and all treatment utilization was monitored. Both groups participated in BL, PT, and six-month FU assessments during which direct product measures, and objective, self, teacher, and parent ratings of symptoms and functioning were obtained. Data was obtained from three sources: a family assessment, mailed or electronically completed teacher ratings, and school records. Complete baseline data was required for study entry. At post-treatment, all participants had data from at least one source and 95% of participants had data from at least two sources. At follow-up, 97% had data from at least one source and 87% had data from at least two sources. There were no group differences in data collection rates (see Figure 1). Participants who completed (97%) and did not complete (3%) were not significantly different on any baseline variables. Families received $50 and teachers $20 for completed assessments. No incentives were given for participation in treatment activities.
TAU
TAU families were encouraged to seek services in the community, including school and local providers during BL to PT. No direct referrals were provided unless requested. TAU families were offered low intensity group behavioral treatment immediately after the FU assessment to incentivize retention. TAU service utilization is described in the Results.
Therapy Description
The specifics for each component are detailed in a manual (BLINDED). Families were assigned to clinicians based upon preferred language (Spanish vs. English) and scheduling availability. All clinicians (N=13) participated in a three-day training that included a one-day MI workshop conducted by a member of the Motivational Interviewing Network of Trainers (MINT) and two days focused on the application of MI spirit and skills to parents and adolescents with ADHD, training in parent-teen contracting and organization skills training, and an orientation to STAND procedures. Clinicians were required to demonstrate mastery of the STAND manual (behavior therapy and MI components) through a score of at least 80% on a written procedural test. Clinician training level included graduate student (61.5%), master’s level (23.1%), and doctoral level clinicians (15.4%). Caseload ranged from three to five per wave and three to eleven cumulatively. Clinician ethnicity was 30.8% Hispanic. All STAND clinicians received weekly supervision from a licensed clinical psychologist with advanced training in MI and extensive experience with families of adolescents with ADHD.
STAND consists of ten 50-minute manualized family therapy sessions attended by the parent and teen. In Session 1, therapists (a) provide an overview of STAND, (b) discuss case conceptualization and provide feedback on assessment results, (c) discuss parent and adolescent strengths and values, (d) discuss common behavior patterns among parents of teens with ADHD, and (e) examine discrepancies between parent values and current parenting patterns. In Session 2, therapists work with family members to (a) identify and prioritize parent and adolescent areas for change, (b) identify treatment goals, and (c) select modular skills based components from a treatment menu. The STAND menu contains seven possible modular sessions, of which families selected four: (a) recording homework daily, (b) creating a homework contract, (c) organizing school materials, (d) prioritizing and managing time out of school, (e) note-taking in class, (f) preparing for tests and quizzes, and (g) troubleshooting problems at home.
For each modular session, a skill is introduced, a plan for applying the skill is devised, and a parent-teen contract is created to detail contingencies associated with appropriate and consistent skill use during the upcoming week. During skills based sessions, therapists use MI in a blended manner to increase the family’s openness to trying a new strategy and empower lasting changes at home. As part of each skill contract, parents detail a monitoring plan to hold teens accountable for consistent skill use. Each session, families review the past weeks’ skill use and contract implementation and the therapist engages the family in MI to consider whether they will continue skill use and monitoring. Four concluding sessions address school collaboration, creating a routine for implementation of new skills, developing and modifying home contracts, and reviewing progress and next steps.
In this study, in addition to the weekly family sessions, parents were invited to attend four monthly group sessions facilitated by a STAND therapist. These sessions offered parents an open forum to discuss adolescent progress and troubleshoot home interventions, but were not well attended: (21.9–51.6% attendance per session).
Measures of Therapy Process
Treatment Fidelity
Clinicians audiotaped each weekly family session. Research assistants were trained to code audiotape sessions using a standard dichotomously coded treatment fidelity checklist for each session that was employed in previous trials of STAND (BLINDED). Twenty percent of sessions were randomly selected for fidelity coding. These tapes were double coded and average agreement across indicators was 95.5% across sessions.
Therapist MI Adherence
The Motivational Interviewing Treatment Integrity (MITI 4.1; Moyers, Manuel, & Ernst, 2014) version 4.1 was used to code therapy tapes for MI adherence. The MITI is a behavioral coding system that has been used to measure MI treatment integrity across numerous clinical trials and possesses strong reliability and predictive validity (Moyers, Martin, Manuel, Hendrickson, & Miller, 2005). MITI coding yields global scores of MI implementation quality on four dimensions rated from a minimum of “1” to a maximum of “5”: Cultivating Change Talk, Softening Sustain Talk, Partnership, and Empathy. MITI behavior counts were tallied for each clinician utterance using ten categorical behaviors representing MI adherent (e.g., affirm, seek collaboration, emphasize autonomy) and nonadherent (e.g., confront, persuade) behaviors. Technical skill indices (i.e., reflection to question ratio, % complex reflection) were also calculated. One audio recording was randomly selected for each STAND case (N=67) and twenty minutes of each session were randomly selected for coding. Three coders who attended formal training in MITI coding independently double coded sessions. Intraclass correlation coefficients (ICC) were calculated to measure inter-rater reliability. One index could not be evaluated with ICCs due to restriction of range (Softening Sustain Talk); however, coding pairs were within one point of each other on this index for 98.5% of tapes. Average ICC was .74 indicating “good” inter-rater agreement (Landis & Koch, 1977).
Attendance
Weekly attendance and module participation for each family session was measured from therapist contact notes. For attendance, therapists coded families as (0=not present or 1= present) for each session.
Satisfaction
Parents and adolescents provided ratings of treatment satisfaction at post-treatment using a standard satisfaction questionnaire developed for ADHD treatments (MTA Cooperative Group, 1999) that was adapted for STAND (BLINDED). Respondents in both groups indicated their degree of satisfaction for 15 aspects of treatment using a 7-point Likert Scale (1=Strongly Disagree – 7=Strongly Agree). Mean overall satisfaction and satisfaction with the demands of the intervention were calculated for each rater. Alpha for this scale was .64 for the parent version and .70 for the adolescent scale.
Measures of Therapy Outcome and Mechanisms
Because STAND is designed to elicit adolescent changes at home and school, there were two primary outcomes in this study. Based on our previous work with STAND, OTP problems at home was selected as the primary measure of adolescent home setting change and GPA was selected as the primary measure of adolescent school setting change. Secondary measures of outcome were also collected. Each measure is described below.
OTP Problems, Homework Behavior, and Classroom Behavior
The parent and teacher versions of the 24-item Adolescent Academic Problems Checklist (AAPC; BLINDED) measure observable secondary-school specific academic problem behaviors and are validated for use in samples of adolescents with ADHD (BLINDED). The parent and teacher AAPCs possess two distinct factors with strong internal reliability and concurrent validity (BLINDED). The 17-item Academic Skills subscale measures adolescent use of secondary-school specific OTP skills. The six-item disruptive behavior subscale measures rule-breaking behavior during academic tasks. Alphas for the AAPC were strong in the current study (.90–91).
ADHD Symptom Severity
Each participant’s level of ADHD severity was measured using the Disruptive Behavior Disorder Rating Scale (DBD; Pelham, Gnagy, Greenslade, & Milich, 1992). The DBD is a DSM-IV-TR symptom rating scale completed by parents and teachers. Respondents were asked to rate symptoms of ADHD as not at all present (0), just a little (1), pretty much (2), or very much (3). To calculate an index of ADHD symptom severity, the average level (0–3) of each item on the subscale was calculated. The psychometric properties of the DBD rating scale are very good, with empirical support for distinct, internally consistent subscales (Pelham et al., 1992; Pillow, Pelham, Hoza, Molina, & Stultz, 1998). In the current study, alphas on the DBD ranged from .91 to .94.
Parent-Teen Conflict
The adolescent version of the Conflict Behavior Questionnaire- 20 (CBQ-20; Robin & Foster, 1989) was used to assess the teen’s view of conflict with the parent. Teens were asked to answer statements about their parents on a five-point Likert scale. The CBQ-20 is a 20-item scale that was adapted from the 73-item CBQ (Prinz, Foster, Kent, & O'Leary, 1979). The CBQ-20 items are the CBQ items that best discriminated distressed from non-distressed families. It yields a single score that correlates .96 with the CBQ but is faster to complete than the long-form of the measure (Robin & Foster, 1989). In the current study, reliability for the CBQ-20 was strong (alpha= .91).
Internalized Parenting Stress
Parenting stress was measured by the 21-item Caregiver Strain Questionnaire (CSQ; Brannan, Heflinger, & Bickman, 1997). At each assessment, the parent indicated how his/her child’s problems affected the parents and family over the past four weeks. Responses were scored on a 5-point scale ranging from not at all to very much a problem. The CSQ shows strong internal reliability and concurrent validity for three distinct subscales (Brannan et al., 1997). In this study, the six-item internalized subjective strain scale (Brannan et al., 1997) was used as an index of parenting stress (alpha= .61).
Parent OTP Involvement
The PAMS is a 16-item checklist that was developed to measure the frequency with which parents monitor (e.g., check to see if your child wrote in a daily planner), assist with (e.g., help your child organize school materials), and reinforce (e.g., use a home academic contract) a range of adolescent OTP skills. Adolescent OTP skills included on the PAMS reflect empirically supported strategies included in psychosocial interventions for teens with ADHD (Evans et al., 2011; Langberg et al., 2012). Parents indicated the number of days during the past school week (0 to 5) that they performed each activity. The PAMS possesses strong psychometric properties as evidenced by good internal consistency, concurrent validity, and predictive validity (BLINDED). Given diversity in treatment targets for adolescents in STAND, targeted parental OTP management strategies also varied by family. Thus, the decision was made to use two strategies that are ubiquitous to STAND (parent-teen contracting and contingent use of home privileges) as outcome measures in this trial.
Official School Grades
Electronic gradebook data were obtained directly from schools or parents at the end of each academic quarter. Quarterly GPA was calculated by converting all academic grades (i.e., Language Arts, Math, Science, Social Studies, Foreign Language) to a 5-point scale (i.e., 4.0=A, 3.0=B, 2.0=C, 1.0=D, 0.0=F). Grades were not weighted for class level (e.g. Honors vs. Regular). We also calculated the % of work completed each quarter by dividing the total number of assignments coded as “missing” by teachers in the grade book by the total number of assignments in the quarter. The quarter in which the adolescent enrolled in the study was considered BL. The quarter immediately following termination of treatment was considered PT. The quarter during which the follow-up assessment occurred was FU.
Recorded Homework
Photocopies of student planners were obtained at each visit. Observations of planner use during the past week assessed the degree to which students actively recorded homework assignments at school. Percentage of classes in which homework was recorded (or some indication of no homework) was calculated for the last five days the student attended school. Planner use percentage was calculated as the mean of daily planner use scores. If an adolescent used an electronic device to record homework, screenshots were obtained and printed for coding. If the adolescent did not utilize a planner or other device for recording homework assignments, he/she received a score of zero. Twenty percent of baseline planners were double coded for inter-rater reliability; intraclass correlation (ICC) was .98.
Bookbag Organization
At each assessment, observations of bookbag organization were obtained using an adaptation of the Organization Checklist (Evans et al., 2009). Trained research assistants assessed dichotomously scored items on the organization checklist such as “Is the adolescent’s bookbag free from loose papers?” and “does the adolescent have a folder/binder for each core academic class?” Organization checklist scores are shown to correlate with teacher ratings of impairment in adolescents with ADHD (Evans et al., 2009).
Analytic Plan
Linear mixed models (LMMs) with random effects were conducted in SPSS 22 using an intent-to-treat design. Separate LMMs were conducted for each outcome variable. Fixed effects of linear time, quadratic time, intervention group, and the interactions of group with the time factors were included. Random intercepts were also included in each model. Prior to analyses, the distributions of all dependent measures were examined to detect outliers and for normality. IQ (continuous variable measured by the WASI) and ADHD subtype (Predominantly Inattentive=0, Combined Type=1) were included as covariates in all models.
An advantage of LMM is that all participants with at least one observation are included in analyses (West, Welch, & Galecki, 2006), minimizing the impact of missing data. A robust Maximum Likelihood estimator was employed in all models. All outcome variables were measured at approximately six months apart at BL, PT, and FU assessments. Our measure of time was coded as a continuous, subject-specific measure that reflects months since the baseline measurement. The baseline measurement time is coded 0; the intercept reflects the predicted outcome value at baseline and the linear effect reflects the instantaneous linear change in the outcome at baseline. Intervention group was dummy coded with TAU as the reference (TAU=0, STAND=1). For each outcome, the following level 1 and level 2 specifications of a mixed model were evaluated.
Of particular interest are the group x linear trend effect (given by the β13 fixed effect) and the group x quadratic trend effect (given by the β23 fixed effect). These values and their significance reflect average differences between the TAU and STAND groups in instantaneous linear trend at the beginning of the study and in their quadratic trends, respectively. The group difference in intercepts (the β03 fixed effect) reflects group differences prior to randomization, so we did not expect differences in that effect. To further probe model results, estimated marginal means from LMMs were used to calculate standardized group differences at PT and at FU using the standard deviation of the outcome at baseline (Morris, 2008). Outcomes where classified as showing acute (PT only) or maintenance (PT and FU) effects based on Cohen’s (1988) recommendations: (.80=large, .50=medium, .20=small). To evaluate the statistical significance of acute and maintenance effects, all LMMs were conducted a second and third time with the time variable recentered at PT and then at FU. Significance of group effect in the former models indicated an acute effect at PT. Significance of the group effect in the latter models indicated a maintenance effect at FU.
Results
TAU and STAND Service Utilization
At PT, TAU activities were systematically assessed for the BL to PT period. Aside from medication use (34.4% in both groups; see Table 1), 8.2% of TAU parents reported that their child attended academic tutoring, 50.8% received educational accommodations at school, and 8.2% obtained individual therapy in the community. Similarly, 13.4% of STAND families reported academic tutoring, 40.3% received educational accommodations at school, and 4.5% obtained individual therapy in the community. In addition, there were no significant group differences at either PT or FU in the number of participants who started a new medication (PT: STAND= 4.5%, TAU= 8.2%, χ2=.99, p=.609; FU: STAND= 4.5%, TAU= 6.6%, χ2=2.04, p=.361) or made a dosing adjustment during the study (PT: STAND= 14.5%, TAU= 9.8%, χ2=1.37, p=.505; FU: STAND= 19.4%, TAU= 23.0%, χ2=1.33, p=.722) Results below did not differ on the basis of participant medication status, psychosocial treatment utilization, or educational accommodations.
Therapy Process
Average STAND fidelity score for probed sessions was 96.4%. Using the MITI 4.1, all mean global scores were above the neutral point on the scale indicating that sessions were MI consistent: Cultivating Change Talk (M=3.76, SD=.87), Softening Sustain Talk (M=4.12, SD=.56), Partnership (M=3.82, SD=.95), and Empathy (M=3.87, SD=.63). Excellent MI quality (four or higher) was demonstrated on a majority of tapes (cultivating change talk: 67.2%; softening sustain talk: 89.6%; partnership: 70.2%; empathy: 74.6%). Technical benchmark means also exceeded high standards (Moyers et al., 2014; reflection to question ratio=2.11:1; % complex reflection=58.6%; MI adherent statements=5.33; MI non-adherent statements=1.19). Overall, 85.1% of families completed all STAND sessions, and on average, 8.34 sessions were attended per family. Therapy was delivered in Spanish to 16.4% of families. Family participation in modular sessions was as follows: recording homework daily (95.5%), creating a homework contract (92.5%), organizing school materials (91.0%), prioritizing and managing time out of school (26.9%), note-taking in class (28.4%), preparing for tests and quizzes (44.8%), troubleshooting problems at home (10.4%). Mean overall satisfaction for parents was 6.00 (SD=1.47) and for adolescents was 4.96 (SD=1.80). Mean satisfaction with the demands of the intervention were 5.95 for parents (SD=1.64) and 5.26 for adolescents (SD=1.62).
Therapy Outcome
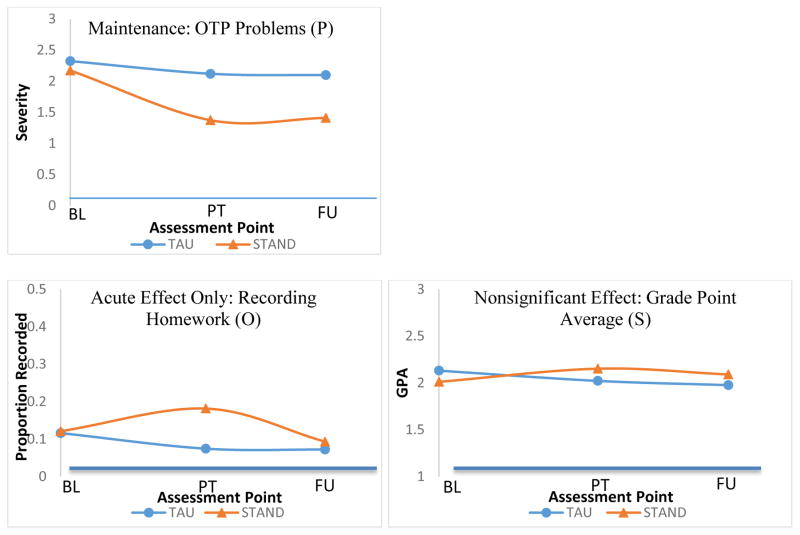
LMM results (see Table 3, Group x Time Interaction columns) indicated significant group x time quadratic effects for home setting OTP problems (p<.001), parent rated disruptive behavior (p=.005), home setting ADHD symptom severity (p=.001), internalized parenting stress (p=.032), parent-teen contracting (p<.014), use of contingent home privileges (p<.001), and observations of homework recording (p=.025). Group x time effects were nonsignificant for adolescent-reported parent-teen conflict (p=.547), teacher rated OTP problems (p=.594), teacher rated disruptive behavior (p=.254), teacher rated ADHD symptoms (p=.604), bookbag organization (p=.343), GPA (p=.118), and work completion (p=.944). Despite nonsignificant group x time interactions, there were significant linear effects for time indicating reductions in teacher rated OTP problems (p=.038) and observed bookbag organization (p=.045) for the STAND group, but not for the TAU group. The STAND and TAU columns of Table 3 show linear and quadratic trajectories separately for the STAND and TAU groups. For example, use of contingent privileges showed a significant Group x quadratic Time interaction, reflecting group differences in the quadratic time trend; the quadratic trend values for the STAND group (-.03) and for the TAU group (.01) are therefore significantly different from one another. Figure 2 displays patterns of treatment response across outcome variables.
Table 3.
LMM Group x Time Interaction Effects for STAND Outcome Measures
| STAND | TAU | Group x Time Interaction | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Linear | Quadratic | Linear | Quadratic | Linear | Quadratic | |||||||
| b | p | b | p | b | p | b | p | b | p | b | p | |
| Home Setting: Adolescent Outcomes | ||||||||||||
| OTP Problems (P) | −.19 | .000 | .01 | .000 | −.04 | .031 | .00 | .184 | −.14 | .000 | .01 | .000 |
| Disruptive Behavior (P) | −.06 | .002 | .01 | .001 | .01 | .536 | .00 | .419 | −.08 | .009 | .01 | .005 |
| ADHD Symptom Severity (P) | −.12 | .000 | .01 | .000 | −.01 | .478 | .00 | .808 | −.11 | .000 | .01 | .001 |
| Home Setting: Parent Outcomes | ||||||||||||
| Internalized Parenting Stress (P) | −.13 | .000 | .01 | .008 | .00 | .995 | .00 | .625 | −.13 | .004 | .01 | .032 |
| Parent-Teen Conflict (A) | −.04 | .134 | .00 | .176 | −.01 | .581 | .00 | .727 | −.02 | .547 | .00 | .520 |
| Home Setting: Parent Mechanisms | ||||||||||||
| Parent-Teen Contracting (P) | .31 | .000 | −.02 | .000 | .06 | .466 | .00 | .889 | .25 | .027 | −.02 | .014 |
| Use of Contingent Privileges (P) | .36 | .000 | −.03 | .000 | −.15 | .051 | .01 | .075 | .51 | .000 | −.04 | .000 |
| School Setting: Adolescent Outcomes | ||||||||||||
| OTP Problems (T) | −.06 | .038 | .00 | .087 | −.04 | .265 | .00 | .572 | −.02 | .594 | .00 | .521 |
| Classroom Behavior (T) | −.03 | .246 | .00 | .143 | .01 | .623 | .00 | .299 | −.04 | .254 | .00 | .084 |
| ADHD Symptom Severity (T) | −.04 | .072 | .00 | .308 | −.02 | .369 | .00 | .986 | −.02 | .604 | .00 | .509 |
| Recording Homework (O) | .02 | .020 | .00 | .006 | −.01 | .381 | .00 | .573 | .03 | .027 | .00 | .025 |
| Bookbag Organization (O) | .02 | .045 | .00 | .067 | .01 | .584 | .00 | .404 | .02 | .343 | .00 | .544 |
| Cumulative GPA (S) | .04 | .116 | .00 | .150 | −.02 | .473 | .00 | .776 | .06 | .118 | .00 | .265. |
| % of Work Turned In (S) | .00 | .918 | .00 | .928 | .00 | .858 | .00 | .825 | .00 | .944 | .00 | .818 |
Note. Tests of significant group by time linear and quadratic interaction terms controlling for group, time, time*time, IQ, and subtype in each LMM. P= Parent, A=Adolescent T=Teacher, O=Direct Observation, S=School Records. STAND and TAU columns reflect the average linear and quadratic (if applicable) change for each group. The Group x Time Interaction column reflects a test of the difference between the STAND and TAU groups.
Figure 2.
Patterns of Treatment Response: Sample Outcomes
Note. BL = baseline, PT= post-treatment, FU= follow-up; PT and FU represent mean functioning for each group at the mean number of months since BL that PT and FU assessments occurred. The maintenance pattern was present for parent-rated OTP skills, parent-rated ADHD symptoms, and parenting stress; acute effects only were present for recording homework, disruptive behavior at home, parent-teen contracting, and parent-teen contracting. Nonsignificant effects were present for directly observed organization and grade point average.
Examination of standardized group difference effect sizes (see Table 4) indicated large acute effects relative to the TAU group for OTP problems (d=1.12), ADHD symptom severity (d=.81), and parent use of contingent privileges (d=1.07) in the home setting. Relative to TAU, medium acute effects were present for internalized parenting stress (d=.60), with small acute effects for disruptive behavior at home (d=.40), parent-teen contracting (d=.49), and recording daily homework assignments at school (d=.45). Small acute effects were also present for cumulative GPA (d=.33) and observed bookbag organization (d=.29); however, these two effects were nonsignificant in LMM models. At FU, there was variability in maintenance (see Figure 2). The maintenance pattern indicated that treatment effects remained similar in magnitude at follow-up for OTP problems in the home setting (d=1.01), ADHD symptoms in the home setting (d=.63), parenting stress (d=.52), observed bookbag organization (d=.31; nonsignificant), and GPA (d=.31; nonsignificant). The acute effects only pattern indicated no maintenance for parent use of contingent privileges, parent-teen contracting, recording homework assignments, and disruptive behavior at home. No effects were present for adolescent report of parent-teen conflict, % of work turned in, and teacher reports of OTP problems, disruptive behavior, and ADHD symptom severity.
Table 4.
Means, SDs, and Standardized Effect Sizes
| STAND | TAU | Cohen’s d | |||||||
|---|---|---|---|---|---|---|---|---|---|
| BL | PT | FU | BL | PT | FU | ||||
| M (SD) | M (SD) | M(SD) | M (SD) | M (SD) | M(SD) | BL-PT | BL-FU | PT-FU | |
| Home Setting: Adolescent Outcomes | |||||||||
| OTP Problems (P) | 2.17(.55) | 1.37(.62) | 1.41(.71) | 2.32(.51) | 2.12(.60) | 2.10(.64) | 1.12* | 1.01* | −.11* |
| Disruptive Behavior (P) | 1.01(.57) | .82(.54) | 1.00(.87) | 1.05(.53) | 1.08(.70) | 1.01(.52) | .40* | −.06 | −.46 |
| ADHD Symptom Severity (P) | 1.85(.60) | 1.31(.58) | 1.29(.60) | 1.87(.62) | 1.76(.61) | 1.64(.51) | .81* | .63* | −.19* |
| Home Setting: Parent Outcomes | |||||||||
| Internalized Parenting Stress (P) | 3.48(.92) | 2.87(.91) | 2.81(.91) | 3.49(.89) | 3.43(.97) | 3.29(.98) | .60* | .52 | −.08* |
| Parent-Teen Conflict (A) | 2.55(.75) | 2.42(.76) | 2.49(.82) | 2.66(.67) | 2.60(.77) | 2.59(.78) | .09 | −.01 | −.10 |
| Home Setting: Parent Mechanisms | |||||||||
| Parent-Teen Contracting (P) | 1.33(1.71) | 2.43(1.96) | 1.81(1.74) | .91(1.23) | 1.29(1.83) | 1.53(1.91) | .49* | −.10 | −.59 |
| Use of Contingent Privileges (P) | 1.08(1.42) | 2.32(1.80) | 1.59(1.70) | 1.68(1.91) | 1.14(1.81) | 1.44(1.81) | 1.07* | .45 | −.62 |
| School Setting: Adolescent Outcomes | |||||||||
| OTP Problems (T) | 1.92(.73) | 1.68(.81) | 1.72(.88) | 1.97(.79) | 1.79(.87) | 1.74(.85) | .08 | −.05 | −0.13 |
| Disruptive Behavior (T) | .81(.63) | .75(.61) | .86(.69) | .92(.66) | .91(.78) | .76(.67) | .08 | −.32 | −.40 |
| ADHD Symptom Severity (T) | 1.52(.73) | 1.31(.64) | 1.26(.72) | 1.54(.62) | 1.38(.75) | 1.24(.72) | .06 | −.07 | −.13 |
| Recording Homework (O) | .12(.25) | .18(.37) | .09(.23) | .12(.20) | .07(.18) | .07(.24) | .45* | .07 | −.38 |
| Bookbag Organization (O) | .47(.26) | .55(.28) | .50(.32) | .45(.25) | .46(.27) | .41(.28) | .29 | .31 | .01 |
| Cumulative GPA (S) | 2.01(.77) | 2.15(.76) | 2.09(.79) | 2.13(.76) | 2.02(.82) | 1.98(.78) | .33 | .31 | −.02 |
| % of Work Turned In (S) | .85(.13) | .85(.13) | .84(.16) | .86(.16) | .85(.13) | .86(.15) | −.02 | −.12 | −.10 |
Note. Means are marginal estimates after controlling for covariates (IQ and ADHD Subtype). Positive effect sizes indicate relative improvement in the STAND group compared to TAU. P= Parent, A=Adolescent T=Teacher, O=Direct Observation, S=School Records. Cohen’s standardized d is difference between group change scores divided by baseline pooled standard deviation. *Indicates significant group differences at assessment.
Discussion
This study evaluated a parent-teen skills-based behavior therapy blended with MI for adolescents with ADHD. LMMs (see Figures 2a-b) indicated that relative to TAU, STAND produced statistically significant effects on seven outcomes that included parent-rated ADHD symptom severity, OTP problems, and disruptive behavior, observed daily homework recording, parent-teen contracting, parent implementation of home privileges, and parenting stress. Examination of LMMs and standardized effect sizes indicated variability in whether acute effects were maintained at six-month follow-up. Maintenance was present for parent-rated ADHD symptom severity, OTP problems, and parenting stress. Group differences diminished at follow-up for parent use of behavior management strategies, teen use of the daily planner, and disruptive behavior during homework time. Relative to the TAU group, no effects for STAND were detected on five outcomes that included: teacher ratings of ADHD severity, OTP problems, and disruptive behavior, adolescent ratings of parent-teen conflict, and % of work turned in. Using effect size benchmarks, two outcomes (observed bookbag organization and GPA) showed evidence of small relative treatment effects that maintained at follow-up (d=.31-.33; see Table 4); however, these smaller effects did not meet the significance threshold in LMMs.
As in the STAND pilot (which had 100% treatment completion among 18 families), treatment was implemented with high fidelity and a majority of families completed all ten sessions (85%). This finding is promising due to evidence that parent-teen collaborative programs for ADHD show lower completion rates (74%; Barkley et al., 2001) than similarly dosed parent (91%; Barkley et al., 2001) and teen-only programs (95%; Boyer et al., 2014). Poorer completion for parent-teen therapy has been attributed to difficulties with dyadic engagement (Weisz & Hawley, 2002). Thus, it is possible that STAND’s high completion rate stems from MI engagement components that were implemented with high integrity. Supporting this possibility, at the end of treatment, a majority of parents and teens were satisfied with STAND and reported that the demands of the intervention were reasonable. However, additional research is needed to determine whether MI components in STAND actively promote engagement and retention.
The proposed mechanism of STAND is teaching OTP strategies to the teen (e.g., writing in a daily planner, keeping a bookbag organization system, using lists and planning strategies to enhance time management, taking notes at school), while engaging parents to support strategy practice through parent-teen contingency contracting. Relative to TAU, adolescents in STAND displayed reductions in OTP problems at home that maintained at follow-up (see Table 3)–providing evidence for successful uptake of new skills. In fact, while TAU deficits remained constant from BL to FU, OTP problems in the STAND group reduced by over a standard deviation–leaving the clinically impaired range (BLINDED). Parent-rated OTP improvements were partly corroborated by direct observational data indicating that the STAND group experienced medium improvements in recording homework assignments and small improvements in bookbag organization relative to the TAU (see Figure 2). Overall, maintained reductions in OTP problems for the STAND group are promising given that executive functioning deficits are a key mechanism of developmental risk among youth with ADHD (Miller, Nevado-Montenegro, & Hinshaw, 2012).
In support of teen OTP skill use, parents in STAND increased their use of academic and behavior management practices (i.e., contracting and contingency management; see Table 3) during the acute treatment phase. Parents in STAND also indicated reduced parenting stress relative to TAU parents, which maintained at follow-up. One criticism of a parent-directed behavior therapy approach is that parents may find home interventions burdensome and straining; however, our satisfaction data and parenting stress outcome suggest the opposite. Our findings are consistent with the STAND pilot, which suggested that most parents found home interventions to be manageable and fit well with their needs (BLINDED). Despite large increases in parent academic and behavior management practices from BL to PT, parents demonstrated only partial continuation of contingency management and appeared to largely cease parent-teen contracting at FU (see Table 4). Desistance of contracting may indicate that OTP habits formed by skill practice reduced the need for parent skill supervision. On the other hand, it is also possible that some parents stopped contracting with teens and reduced contingency management in spite of continued problems. For example, disruptive behavior at home (d=.40) and recording homework at school (d=.45) improved during treatment compared to TAU; however, these effects reversed by FU–possibly due to reduced oversight and contingency management by parents. These findings indicate that additional work is needed to promote long-term utilization of parenting strategies after weekly sessions terminate.
The primary school outcome in this trial was adolescent GPA. Despite increases in OTP skill use at home, adolescents in STAND made very small improvements in GPA (d=.33) relative to TAU. Despite maintenance of this small effect at follow-up (d=.31), LMM group x time effects were not statistically significant and represented relative change of less than a quarter of a GPA point (see Figure 2). Our failure to find robust GPA effects is consistent with research on school-based OTP interventions for adolescents with ADHD, which also report modest improvement to student grades (Evans, Serpell, Schultz, & Pastor, 2007; Evans et al., 2011). In a long-term study of an OTP intervention delivered to middle school students with ADHD, Evans and colleagues (2007) reported that the largest benefits to student GPA emerged three years after intervention delivery began. Thus, the impact of OTP interventions on GPA may increase slowly over time, as skills become increasingly habitual. Finally, one unique aspect of STAND is that for a subset of families, the goal of treatment is to transfer homework responsibilities from an intrusively involved parent to the adolescent. Thus, for some families in this trial, appropriate reductions in parent homework intrusion may have come at a cost to work quality, work completion rate, and GPA. As stated by one parent in her final session of STAND, “he’s still getting B’s, but now it’s his B, not my B.”
One of the most promising findings of this trial was that, over the course of a single year, STAND was associated with a half standard deviation reduction in parent-rated ADHD symptoms relative to the TAU group. A reduction of this magnitude is equivalent to four years of maturational symptom decline in adolescents with ADHD (Sibley, Pelham et al., 2014). ADHD symptom desistence in adolescence is perhaps the strongest mitigator of long-term risk in this population (Biederman et al., 2011; Hechtman et al., 2015) and these maintenance effects are especially compelling because the majority of our sample received treatment in childhood (see Table 1), yet displayed persistent symptoms and impairment in adolescence. Though these effects are promising, additional treatment studies with longer follow-up periods are necessary to determine their robustness; for example, in the MTA, initial acute effects slowly ebbed for about four years post-treatment (Molina et al., 2009).
It is important to note that significant effects were limited to parent report and direct observational data–adolescents and teachers did not report BL-PT change on any variables (see Tables 3 & 4). Failure to find meaningful treatment effects for self and teacher reported outcomes is common in controlled treatment outcome research with adolescents with ADHD (Langberg et al., 2012; Pelham et al., 2013). For one, adolescents with ADHD are notoriously poor reporters of their own functioning (Fischer, Barkley, Fletcher, & Smallish, 1993) and may not report changes during treatment if they did not perceive problems at outset. Secondary school teachers often offer inconsistent reports of adolescents with ADHD due to cursory student-teacher interactions in secondary schools, the subjective nature of ADHD symptoms, and/or negative halo effects (Evans, Allen, Moore, & Strauss, 2005). Thus, it is possible that some teachers do not notice student improvements in OTP skills–particularly when they are not engaged to monitor skill practice. The inconsistency in our findings across raters further underscores the need to collect objective outcome data in research with adolescents with ADHD. Nonsignificant teacher effects may also indicate adolescent failure to implement new OTP skills in the classroom. Lack of skill use at school may occur because the adolescent is unsure how to apply skills in the school setting–indicating a need for setting specific instruction in OTP skills. On the other hand, motivation deficits may lead adolescents to avoid skill use in the absence of adult accountability (i.e., consistent monitoring and contingency management). Therefore, one way to enhance school setting effects is to enhance oversight of skill use and contingency management in the school setting. Future work is needed to devise realistic ways to do so within the resource constraints of typical secondary schools.
Our study possesses limitations that should be considered. First, this study was conducted with early to middle adolescents, and findings may not generalize to older adolescents. The majority of participants were Hispanic with a parent who held a bachelor’s degree, and so results may not generalize to all adolescents with ADHD. As such, it will be important for future work to evaluate cultural factors that enhance or undermine engagement in STAND. Most clinicians represented well-supervised trainees with a lower case load than most community providers and so the extent to which STAND is generalizable in professional settings is yet to be determined. Support group attendance was poor and further work is needed to understand whether there is incremental benefit to these components, and if so, how to engage families to simultaneously attend group and individual treatment components. TAU parent expectations of eventual treatment may have reduced motivation to pursue outside services. Thus, future trials of skills-based behavior therapy for teens with ADHD would be strengthened by an attention control condition. Parents were required to commute to the university clinic each week for treatment, which may have prevented enrollment from parents with certain barriers (see Figure 1). After randomization, the two groups were not equivalent on ADHD subtype and IQ, and so we had to include these variables as covariates in all models. Finally, as with any study, sample size limits the ability to detect effects below a certain size. The sample size of this study, while adequate to detect effects of the size that are common in studies of ADHD interventions, limited our ability to detect small effects (d <.40).
In sum, this study offers promise of a parent-teen skills-based therapy blended with MI to engage families in treatment and improve the symptoms and impairments of adolescents with ADHD–largely in the home setting. During the BL-PT period, the TAU and STAND groups accessed equivalent community and school-based services and effects did not vary as a function of TAU activities; thus, these improvements reflect the incremental benefit of STAND above typically accessed services for teens with ADHD (mainly supports at school and medication). Despite this promise, further refinement of this approach is indicated. For example, perhaps brief MI sessions after treatment terminates would serve as a realistic means of strengthening parent commitment to continue contracting and contingency management–highlighting the possibility that brief treatment models are insufficient for chronic disorders such as ADHD (Barkley et al., 2008). One important implication of this study is the need to evaluate treatments for teens with ADHD that integrate care across home and school settings to enhance cross-contextual effects. Moving forward, the true test of an approach, such as STAND, will be community dissemination into mental health care systems, and evaluation in professional settings.
Acknowledgments
This project was supported by R34MH092466 from the NIMH and, in part, by R324A120169 from the Institute for Education Science, and the Klingenstein 3rd Generation Foundation.
References
- Abikoff H, Gallagher R, Wells K, Murray D, Huang L, Lu F, et al. Remediating organizational functioning in children with ADHD:Immediate and long-term effects from a randomized controlled trial. Journal of consulting and clinical psychology. 2013;81:113–128. doi: 10.1037/a0029648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 2000. [Google Scholar]
- Barkley R, Edwards G, Laneri M, Fletcher K, Metevia L. The efficacy of problem-solving communication training alone, behavior management training alone, and their combination for parent–adolescent conflict in teenagers with ADHD and ODD. Journal of Consulting and Clinical Psychology. 2001;69:926–941. [PubMed] [Google Scholar]
- Barkley R, Fischer M, Smallish L, Fletcher K. The persistence of attention deficit hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. Journal of Abnormal Psychology. 2002;111:279–289. [PubMed] [Google Scholar]
- Barkley R, Guevremont DC, Anastopoulos AD, Fletcher KE. A comparison of three family therapy programs for treating family conflicts in adolescents with attention-deficit hyperactivity disorder. Journal of Consulting and Clinical Psychology. 1992;60:450. doi: 10.1037/0022-006X.60.3.450. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Murphy KR, Fischer M. ADHD in Adults: What the Science Says. New York: Guilford; 2008. [Google Scholar]
- Biederman J, Monuteaux M, Spencer T, Wilens T, MacPherson H, Faraone S. Stimulant therapy and risk for subsequent substance use disorders in male adults with ADHD: a naturalistic controlled 10-year follow-up study. American Journal of Psychiatry. 2008;165:597–603. doi: 10.1176/appi.ajp.2007.07091486. [DOI] [PubMed] [Google Scholar]
- Biederman J, Petty C, Clarke A, Lomedico A, Faraone S. Predictors of persistent ADHD: an 11-year follow-up study. Journal of Psychiatric Research. 2011;45:150–155. doi: 10.1016/j.jpsychires.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird HR, Gould MS, Staghezza B. Aggregating data from multiple informants in child psychiatry epidemiological research. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:78–85. doi: 10.1097/00004583-199201000-00012. [DOI] [PubMed] [Google Scholar]
- Biswas A, Gnagy E, Molina B, Pelham W. Examining the decline of treatment use in adolescents with ADHD. Poster presented at the annual meeting of the Association for Behavioral and Cognitive Therapies; New York, NY. 2009. [Google Scholar]
- Brannan AM, Heflinger CA, Bickman L. The caregiver strain questionnaire measuring the impact on the family of living with a child with serious emotional disturbance. Journal of Emotional and Behavioral Disorders. 1997;5:212–222. [Google Scholar]
- Bussing R, Koro M, Noguchi K, Mason D, Mayerson G, Garvan C. Willingness to use ADHD treatments: a mixed methods study of perceptions by adolescents, parents, health professionals and teachers. Social science & medicine. 2012;74:92–100. doi: 10.1016/j.socscimed.2011.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussing R, Zima BT, Mason DM, Porter PC, Garvan CW. Receiving treatment for attention-deficit hyperactivity disorder: do the perspectives of adolescents matter? Journal of Adolescent Health. 2011;49:7–14. doi: 10.1016/j.jadohealth.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Jones RM, Hare TA. The adolescent brain. Annals of the New York Academy of Sciences. 2008;1124:111–126. doi: 10.1196/annals.1440.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Mental health Surveillance Among Children– United Sates, 2005–2011. MMWR. 2013;62(Suppl 2):1–35. [PubMed] [Google Scholar]
- Chan P, Rabinowitz T. A cross-sectional analysis of video games and attention deficit hyperactivity disorder symptoms in adolescents. Annals of General Psychiatry. 2006;5:1–10. doi: 10.1186/1744-859X-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chronis-Tuscano A, O’Brien KA, Johnston C, Jones HA, Clarke TL, Raggi VL, et al. The relation between maternal ADHD symptoms & improvement in child behavior following brief behavioral parent training is mediated by change in negative parenting. Journal of abnormal child psychology. 2011;39:1047–1057. doi: 10.1007/s10802-011-9518-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analyses for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Eccles JS. Schools, academic motivation, and stage-environment fit. Handbook of adolescent psychology. 2004;2:125–153. [Google Scholar]
- Edwards G, Barkley R, Laneri M, Fletcher K, Metevia L. Parent–adolescent conflict in teenagers with ADHD and ODD. Journal of abnormal child psychology. 2001;29:557–572. doi: 10.1023/a:1012285326937. [DOI] [PubMed] [Google Scholar]
- Evans SW, Schultz BK, White LC, Brady C, Sibley MH, Van Eck K. A school-based organization intervention for young adolescents with attention deficit/hyperactivity disorder. School Mental Health. 2009;1:78–88. [Google Scholar]
- Evans S, Schultz B, DeMars C, Davis H. Effectiveness of the Challenging Horizons program for young adolescents with ADHD. Behavior Therapy. 2011;42:462–474. doi: 10.1016/j.beth.2010.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans S, Allen J, Moore S, Strauss V. Measuring symptoms and functioning of youth with ADHD in middle school. Journal of abnormal child psychology. 2005;33:695–706. doi: 10.1007/s10802-005-7648-0. [DOI] [PubMed] [Google Scholar]
- Evans SW, Serpell ZN, Schultz BK, Pastor DA. Cumulative benefits of secondary school-based treatment of students with attention deficit hyperactivity disorder. School Psychology Review. 2007;36:256. [Google Scholar]
- Fischer M, Barkley R, Fletcher K, Smallish L. The stability of dimensions of behavior in ADHD and normal children over an 8-year followup. Journal of Abnormal Child Psychology. 1993;21:315–337. doi: 10.1007/BF00917537. [DOI] [PubMed] [Google Scholar]
- Flory K, Molina BS, Pelham WE, Jr, Gnagy E, Smith B. Childhood ADHD predicts risky sexual behavior in young adulthood. Journal of Clinical Child and Adolescent Psychology. 2006;35:571–577. doi: 10.1207/s15374424jccp3504_8. [DOI] [PubMed] [Google Scholar]
- Hechtman LT, Swanson JM, Sibley MH, Stehli A, Arnold LE MTA Cooperative Group. Functional Adult Outcomes 16 years after Childhood Diagnosis of Attention Deficit/Hyperactivity Disorder: MTA Results. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henggeler SW, Lee T. Multisystemic treatment of serious clinical problems. In: Kazdin AE, Weisz JR, editors. Evidence-based psychotherapies for children and adolescents. New York: Guilford; 2003. [Google Scholar]
- King CA, Hovey JD, Brand E, Wilson R, Ghaziuddin N. Suicidal adolescents after hospitalization: parent and family impacts on treatment follow-through. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:85–93. doi: 10.1097/00004583-199701000-00021. [DOI] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977:159–174. [PubMed] [Google Scholar]
- Langberg JM, Epstein JN, Becker SP, Girio-Herrera E, Vaughn AJ. Evaluation of the homework, organization, and planning skills (HOPS) intervention for middle school students with attention deficit hyperactivity disorder as implemented by school mental health providers. School Psychology Review. 2012;41:342. [PMC free article] [PubMed] [Google Scholar]
- Langberg JM, Dvorsky MR, Evans SW. What specific facets of executive function are associated with academic functioning in youth with attention-deficit/hyperactivity disorder? Journal of Abnormal Child Psychology. 2013;41:1145–1159. doi: 10.1007/s10802-013-9750-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Grange D, Lock J, Loeb K, Nicholls D. Academy for eating disorders position paper: The role of the family in eating disorders. International Journal of Eating Disorders. 2010;43:1–5. doi: 10.1002/eat.20751. [DOI] [PubMed] [Google Scholar]
- Lee SS, Hinshaw SP. Severity of adolescent delinquency among boys with and without attention deficit hyperactivity disorder: predictions from early antisocial behavior and peer status. Journal of Clinical Child and Adolescent Psychology. 2004;33:705–716. doi: 10.1207/s15374424jccp3304_6. [DOI] [PubMed] [Google Scholar]
- Liddle HA, Dakof GA, Parker K, Diamond GS, Barrett K, Tejeda M. Multidimensional family therapy for adolescent drug abuse: Results of a randomized clinical trial. The American journal of drug and alcohol abuse. 2001;27:651–688. doi: 10.1081/ada-100107661. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Moulton J. Lifetime criminality among boys with attention deficit hyperactivity disorder: A prospective follow-up study into adulthood using official arrest records. Psychiatry Research. 2008;160:237–246. doi: 10.1016/j.psychres.2007.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina D, Sibley MH. Situational and Behavioral Antecedents to Arguments Between Parents and Adolescents With ADHD. Poster presented at the Annual Meeting of the Association for Behavioral and Cognitive Therapies; Chicago, IL. 2015. Nov, [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Helping people change. Guilford Press; 2013. [Google Scholar]
- Miller M, Nevado-Montenegro AJ, Hinshaw SP. Childhood executive function continues to predict outcomes in young adult females with and without childhood-diagnosed ADHD. Journal of Abnormal Child Psychology. 2012;40:657–668. doi: 10.1007/s10802-011-9599-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina B, Flory K, Bukstein O, Greiner A, Baker J, Krug V, et al. Feasibility and preliminary efficacy of an after-school program for middle schoolers with ADHD a randomized trial in a large middle school. Journal of Attention Disorders. 2008;12:207–217. doi: 10.1177/1087054707311666. [DOI] [PubMed] [Google Scholar]
- Molina B, Hinshaw S, Swanson J, Arnold L, Vitiello B, et al. The MTA at 8 years: Prospective follow-up of children treated for combined-type ADHD in a multisite study. Journal of American Academy of Child & Adolescent Psychiatry. 2009;48:484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BS, Pelham WE, Jr, Cheong J, Marshal MP, Gnagy EM, Curran PJ. Childhood attention-deficit/hyperactivity disorder (ADHD) and growth in adolescent alcohol use: The roles of functional impairments, ADHD symptom persistence, and parental knowledge. Journal of abnormal psychology. 2012;121:922. doi: 10.1037/a0028260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina BS, Walther CA, Cheong J, Pedersen SL, Gnagy EM, Pelham WE., Jr Heavy alcohol use in early adulthood as a function of childhood ADHD: Developmentally specific mediation by social impairment and delinquency. Experimental and clinical psychopharmacology. 2014;22:110. doi: 10.1037/a0035656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris SB. Estimating effect sizes from pretest–posttest–control group designs. Organizational Research Methods. 2008;11:364–386. [Google Scholar]
- Moyers TB, Houck J. Combining motivational interviewing with cognitive- behavioral treatments for substance abuse: Lessons from the COMBINE research project. Cognitive and Behavioral Practice. 2011;18:38–45. [Google Scholar]
- Moyers TB, Manuel JK, Ernst D. Motivational Interviewing Treatment Integrity Coding Manual 4.1. Unpublished Manual 2014 [Google Scholar]
- Moyers T, Martin T, Manuel J, Hendrickson S, Miller W. Assessing competence in the use of motivational interviewing. Journal of substance abuse treatment. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 1999;56:1073. doi: 10.1001/archpsyc.56.12.1073. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Fabiano GA, Massetti GM. Evidence-based assessment of attention-deficit/hyperactivity disorder in children and adolescents. Journal of Clinical Child and Adolescent Psychology. 2005;34:449–476. doi: 10.1207/s15374424jccp3403_5. [DOI] [PubMed] [Google Scholar]
- Pelham W, Gnagy E, Greenslade K, Milich R. Teacher ratings of DSM-III--R symptoms for the disruptive behavior disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1992;31:210–218. doi: 10.1097/00004583-199203000-00006. [DOI] [PubMed] [Google Scholar]
- Pillow D, Pelham W, Hoza B, Molina B, Stultz C. Confirmatory factor analyses examining attention deficit hyper- activity disorder symptoms and other childhood disruptive behaviors. Journal of Abnormal Child Psychology. 1998;26:293–309. doi: 10.1023/a:1022658618368. [DOI] [PubMed] [Google Scholar]
- Power TJ, Mautone JA, Soffer SL, Clarke AT, Marshall SA, Sharman J, et al. A family–school intervention for children with ADHD: Results of a randomized clinical trial. Journal of Consulting and Clinical Psychology. 2012;80:611. doi: 10.1037/a0028188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prinz R, Foster S, Kent R, O'Leary K. Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. Journal of applied behavior analysis. 1979;12:691–700. doi: 10.1901/jaba.1979.12-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robin AL, Foster SL. Negotiating parent-adolescent conflict: A behavioral-family systems approach. NY: Guilford Press; 1989. [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Kuriyan AB, Evans SW, Waxmonsky JG, Smith BH. Pharmacological and psychosocial treatments for ADHD in adolescents: An updated systematic review of the literature. Clinical Psychology Review. 2014;34:218–232. doi: 10.1016/j.cpr.2014.02.001. [DOI] [PubMed] [Google Scholar]
- Sibley MH, Pelham WE, Molina BSG, Coxe S, Kipp H, Lahey The Role of Early Childhood ADHD and Subsequent CD in the Initiation and Escalation of Adolescent Cigarette, Alcohol, and Marijuana Use. Journal of Abnormal Psychology. 2014 doi: 10.1037/a0036585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonuga-Barke EJ. The dual pathway model of AD/HD: an elaboration of neuro-developmental characteristics. Neuroscience & Biobehavioral Reviews. 2003;27:593–604. doi: 10.1016/j.neubiorev.2003.08.005. [DOI] [PubMed] [Google Scholar]
- Steinberg L, Morris AS. Adolescent development. Journal of Cognitive Education and Psychology. 2001;2:55–87. [Google Scholar]
- Toplak M, Jain U, Tannock R. Executive and motivational processes in adolescents with Attention-Deficit-Hyperactivity Disorder. Behavioral and Brain Functions. 2005;1:8. doi: 10.1186/1744-9081-1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser SN, Danielson M, Bitsko RH, Holbrook JR, Kogan M, Ghandour, et al. Trends in the Parent-Report of Health Care Provider-Diagnosed and Medicated Attention-Deficit/Hyperactivity Disorder: United States, 2003–2011. Journal of the American Academy of Child & Adolescent Psychiatry. 2014;53:34–46. doi: 10.1016/j.jaac.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler abbreviated scale of intelligence (WASI) San Antonio: Harcourt; 1999. [Google Scholar]
- Wechsler D. Wechsler individual achievement tests. 2. San Antonio: Harcourt; 2002. [Google Scholar]
- Weisz JR, Hawley KM. Developmental factors in the treatment on adolescents. Journal of Consulting and Clinical Psychology. 2002;70:21. doi: 10.1037//0022-006x.70.1.21. [DOI] [PubMed] [Google Scholar]
- West BT, Welch KB, Galecki AT. Linear mixed models: a practical guide using statistical software. CRC Press; 2006. [Google Scholar]