Abstract
Objective
The aims of this study were to evaluate the efficacy of the two types of couple-focused group interventions on couples’ psychological and relationship functioning, and to examine possible moderators for each intervention.
Methods
Three hundred and two women with early stage breast cancer who were recruited within one year of diagnosis and their spouses were randomly assigned to either an eight session enhanced couple-focused group intervention (ECG) or a couples’ support group (SG). Couples completed surveys at four time points: pre-intervention, one week post-group, six months, and one year.
Results
Analyses indicated that anxiety, depressive symptoms, and cancer-specific distress declined and positive well-being improved for couples enrolled in both ECG and SG. Thus, neither treatment was superior in terms of reduction of distress or improvements in positive well-being. Moderator effects indicated that, among patients reporting higher levels of cancer-specific pre-intervention distress, anxiety, depression, and well-being over the one year post-intervention time period were significantly lower among SG couples than ECG couples. When patient cancer-specific pre-intervention distress was low, these three outcomes were more positive in ECG relative to SG. A similar pattern with regard to anxiety was illustrated when the moderator effects for perceived partner unsupportive behavior was examined, and a similar pattern was seen for anxiety and well-being for pre-intervention marital satisfaction.
Conclusions
A couple-focused supportive group therapy may be more effective for distressed patients, whereas a structured, skills-based couples’ group therapy may be more effective for less distressed patients.
Public Health Relevance
This study highlights the importance of targeting different types of group therapy to cancer patients with different levels of distress.
Keywords: Breast cancer, couple-focused interventions, couples, group therapy
The diagnosis and treatment of non-metastatic breast cancer can be stressful and upsetting. Women manage the emotional consequences of being diagnosed with a life-threatening illness, cope with invasive medical treatments such as chemotherapy and radiation that can result in difficult side effects such as nausea, weight gain, and fatigue, and manage worries about future cancer recurrence. In addition to these emotional concerns, breast cancer diagnosis and treatment may result in day-to-day practical stressors for patients, particularly during the time that they are receiving chemotherapy and/or radiation. These stressors include changes in family roles, interference with social plans, and managing household responsibilities. Even after treatment is completed, patients negotiate the transition back to “normal” life, deal with concerns about recurrence, and may alter their life plans in the face of the realization that life may be foreshortened. These experiences can take an emotional toll on some patients. Although figures vary depending on the time of assessment and treatment regimen, between 12.7% and 42% of women with non-metastatic breast cancer report clinically-significant levels of depressive symptoms within the first year after diagnosis (Christensen et al., 2009; Deshields, Tibbs & Taylor, 2005; Ganz, Kwan, Stanton et al., 2011; Kawase et al., 2012; Luutonen et al., 2011; Vadnaninia et al., 2010), and between 12.5% and 48% of women report clinically-significant levels of anxiety within the first year after diagnosis (Karakoyun-Celik et al., 2010; So et al., 2010; Vahdaninia et al., 2010).
One way women manage this stressful life experience is to turn to their spouses or life partners for emotional and practical support. Indeed, among support providers, spouses are considered a primary confidante (Figueirdo, Fries & Ingram, 2004; Harrison, Maguire, & Picheathly, 1995). A number of studies have indicated that spouse emotional support is a key correlate of patients’ adaptation to breast cancer (Belcher et al., 2011; Manne et al., 2006) and that the quality of the communication between patient and spouse plays a key role in patients’ adaptation (Manne et al,. 2006; Manne et al., 2007; Manne, Badr, Zaider, Nelson & Kissane, 2010). Although spouses are a key source of support, spouses may also experience their own distress associated with the diagnosis of breast cancer. In fact, studies suggest that approximately 20% of spouses report clinically-significant levels of depression, anxiety, and other psychological problems (Lewis et al., 2008).
Due to the importance of the marital relationship in couples’ adjustment, a number of couple-focused interventions have been developed and evaluated for early stage breast cancer patients and their partners (Baucom et al., 2009; Christensen, 1983; Heinrichs et al., 2012; Kayser, Fledman, Borselmann & Daniels, 2010; Scott et al., 2004) as well as for couples coping with other types of cancer (e.g., Lambert et al., 2015 ; Manne et al., 2010; Porter et al., 2009; Reese et al., 2014). These studies have used an individual couples’ therapy approach (couples attend as a dyad) and have suggested that the couple-focused approach reduces both patient and partner global and cancer-specific distress as well as improves relationship satisfaction and communication. There has been limited research on interventions where couples attend a group therapy. Group interventions have shown efficacy for women diagnosed with breast cancer (Gudenkauf, et al., 2015; Helgeson, Cohen, & Schulz, 2000). Although there is no literature documenting therapeutic processes for couples who attend groups together, the well-documented beneficial effects of group therapy for cancer patients and, in general, for individuals coping with other difficult life experiences include peer support (Kissane et al., 2003; Yalom, 1975), a reduction of feelings of isolation (Yalom, 1975; Spiegal & Yalom, 1978, Spiegal & Classen, 2000), the opportunity to openly express troubling feelings in a safe environment and among others who are in a similar situation (Spiegal & Classen, 2000), modeling effective coping and improving self-understanding (Spiegal & Classen, 2000; Yalom, 1975). Although these processes have not been documented for couples who attend groups together, it is highly likely that couples may similarly observe other couples’ effective coping and open communication and thereby benefit in the same ways.
In our prior work, we developed and evaluated a six session couple-focused group intervention for early stage breast cancer patients and their spouses (Manne et al., 2005). This six session structured cognitive-behavioral couples’ intervention focused on bolstering relationship communication and couples’ coping skills such as problem solving and stress management as a dyad. Results indicated that patients reported lower depressive symptoms at the six month follow-up as compared with usual care. The couples’ group intervention reduced depression significantly more and improved positive well-being more among those patients who rated their spouses as unsupportive prior to beginning the intervention group.
Despite the fact that the couples’ group intervention was effective, there are a number of unanswered questions. Most importantly, the couple-focused group intervention was a structured and skill-based intervention. Common factors of group therapy, which include the provision of emotional support between group members, could also be responsible for the reductions in depressive symptoms in addition to the skill-based components. Indeed, common factors mediate effects of other types of group therapy (e.g., Day, Halpin & Thorn, 2015). As noted above, one of the primary benefits of groups for persons undergoing specific life stressors is that sharing common experiences facilitates a sense of community with group members and thereby reduces isolation. Second, although the original couple-focused group intervention reduced patient depression at a six month follow-up (Manne et al., 2005), longer-term outcomes and spouse outcomes were not assessed, dyadic-level analyses were not employed, and relationship outcomes (e.g., relationship satisfaction) were not evaluated. Third, because we were following couples for longer period of time, we enhanced the couple-focused group intervention in the current study with the goal of achieve a longer-term treatment effect by adding two sessions to the couples’ group intervention, more in-session skill practice, and more between-session skill practice. The enhanced intervention was called the Enhanced Couples Group (ECG). Finally, when evaluating the efficacy of an intervention, it is important to consider that interventions may not be efficacious for all participants. As noted above, we found that patient reported partner unsupportive behavior moderated the couples’ group effects (Manne et al., 2005). However, additional treatment moderators were not assessed. Pre-intervention relationship quality (Baucom et al., 2015) and patient distress (Hopko et al., 2015) have been shown to moderate both couple and individual therapy effects, respectively.
This study sought to advance the original couple-focused group intervention by enhancing practice of skills, by comparing it with an alternative treatment approach, by assessing spouse and relationship outcomes, by analyzing dyads (rather than individuals), and by testing additional treatment moderators. The study had two aims. The first aim was to evaluate the efficacy of the ECG intervention and a Support Group Intervention (SG) on couples’ psychological and relationship functioning. SG emphasized the participants’ expression of emotions and the provision of group support, but did not teach specific skills. We proposed that ECG would have stronger effects than SG on patient and partner distress, well-being, and relationship satisfaction. Although we did not predict differences in outcomes for patients and partners, we included a role variable in our analyses to assess whether such differences emerged. The data analytic models included a series of covariates, as well as all main effects and interactions for three variables: treatment condition, role, and time. The second aim was to examine the role of three moderators: patient’s pre-intervention distress, patient’s pre-intervention perceived partner unsupportive behavior, and patient’s pre-intervention relationship satisfaction. We proposed that ECG would be more effective than SG among couples in which the patient reported higher levels of pre-intervention distress, higher perceived partner unsupportive behavior, and lower levels of relationship satisfaction. That is, the skill-based intervention would be more effective in helping those who come into the intervention lacking social support from their spouses. To assess the second aim, we added initial status on each moderator to the models so that they included the covariates and all main effects and interactions between the moderator variable, treatment condition, role, and time.
Methods
Participants
Participants were 302 women with early stage breast cancer and their significant others (two female spouses). Patient participants were approached for study participation from the outpatient clinics of oncologists practicing in three comprehensive cancer centers in the Northeastern United States or in several smaller local community hospital oncology practices. Criteria for study inclusion were as follows: a) patient had a primary diagnosis of Ductal surgery in the last twelve months, but could be in active treatment (e.g., radiation or chemotherapy); c) patient and spouse were 18 years of age or older; d) patient and spouse were able to give informed consent; e) patient and spouse were English-speaking, f) patient currently married or living with a significant other of either sex, and; g) couple lives within one hour commuting distance to the center from which they were recruited. We included women with DCIS because the most studies suggest that levels of distress and fear about cancer recurrence are similar to levels reported by women with invasive breast cancer (Lauzier et al., 2010; Liu et al., 2011; van Gestel et al., 2006).
Procedures
Eligible patients were identified and approached either after an outpatient visit or by telephone contact or by mail. Patient and spouse were given a written informed consent document and the study questionnaire to complete and return by mail. Couples were randomly assigned to ECG or SG by a computerized program from the Biostatistics Program at Fox Chase Cancer Center (PRESAGE). Randomization was done after both partners’ consents and the Time 1 surveys were completed. The four assessment time points were baseline, one-week after the eight-week intervention, 6 months post-intervention, and 12 months post-intervention. Couples were paid $15 per person for completing the baseline survey, $20 per person for completing the Time 2 survey, $25 per person for completing the Time 3 survey, and $30 per person for completing the Time 4 survey. They were paid $15, $20, $25, $30, $35, $40, $45 and $50 for attending Groups 1 to 8, respectively. Enrollment began in March, 2008 and the last couple was enrolled in July, 2013. The Institutional Review Board for each site approved this study.
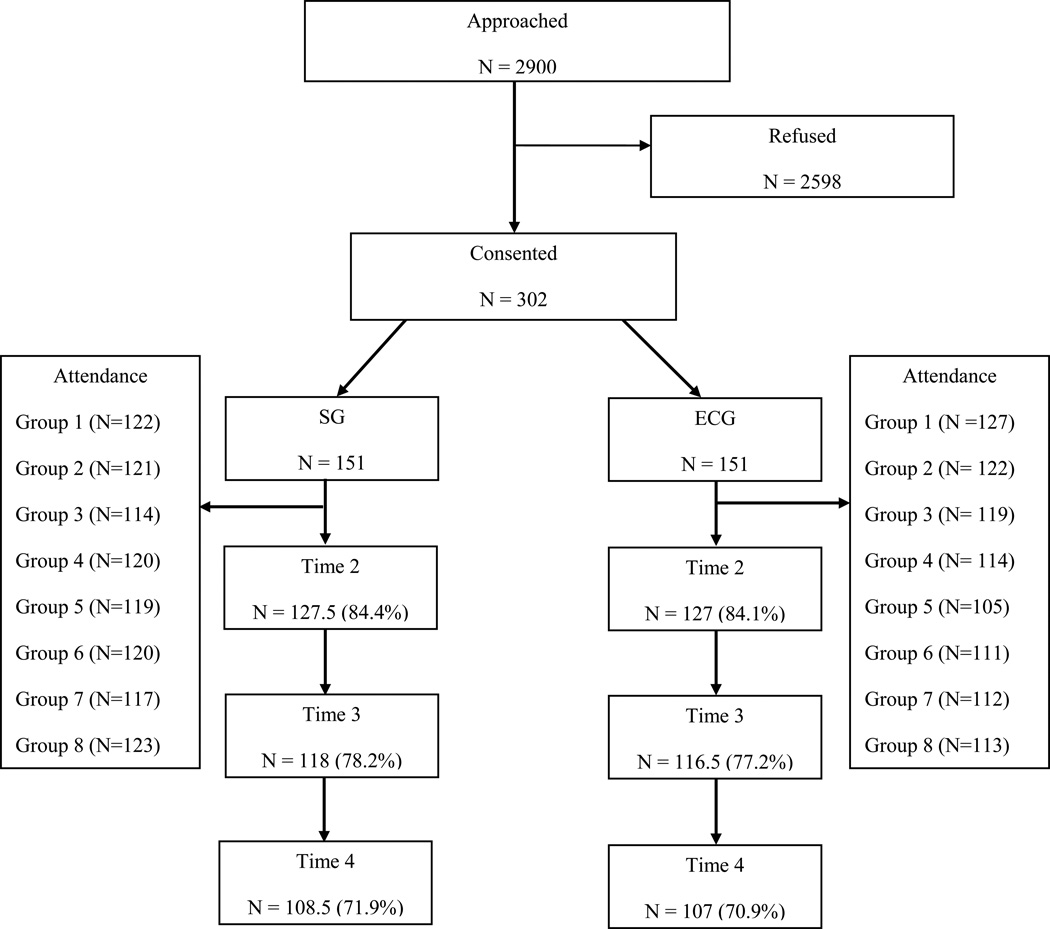
The CONSORT is shown in Figure 1. Of the 2900 eligible women approached for study participation, 302 couples consented and completed the baseline survey (10.4%). The most common reason for refusal provided was that the couple was not interested (18.4%) or participation would “take too much time” (15.7%). Many (26.7%) did not provide a reason. Comparisons were made between patient participants and refusers with regard to available data (age, race/ethnicity, cancer stage, performance status). Results indicated that patient participants were significantly younger than non-participants (M participants = 55.1, SD = 10.4, M refusers = 57.2, SD = 20.6, t (2850) = 2.9, p < .01) and patient participants had been diagnosed a significantly shorter period of time than non-participants (M participants = 4.8, SD = 2.5, M refusers = 10, SD = 7.5, t (2850) =12.0, p < .001). We were not able to compare spouse refusers with participants because there was no data collected on spouse refusers.
Figure 1.
Intervention Conditions
ECG
ECG consisted of eight 90 minute weekly groups led by two therapists. The goals of Session 1 were to orient participants, establish rapport with the group leaders, foster connections between group members, and facilitate expression of information and feelings about the cancer experience. Members discuss their experiences with one another and then engaged in a focused-breathing relaxation induction. Session 2 focused on constructive communication. Constructive communication skills, speaker-listener role-taking, and how to give negative feedback were presented and couples practiced the skills separately. Focused-breathing relaxation was practiced. Session 3 focused on identifying and expressing support needs. A group discussion about how couples handle worries and feelings occurred, which was followed by a presentation on support needs. Couples practiced discussing their support needs with one another and then created a “Wish List” for positive acts for their spouse to do for them. This was followed by progressive muscle relaxation as a group. Session 4 focused on being a good support to one’s partner. Couples discussed changes experienced and expressed how their partner could help them make a positive change in their lives (e.g., exercise). Progressive muscle relaxation was practiced. Session 5 focused on stress management and sexual intimacy. Couples discussed their stress responses, viewed a video on sexuality and cancer, engaged in separate couples’ discussion about sexuality, and created an intimacy deck, which is a list of activities to increase intimacy. Guided imagery was done as a group. Session 6 focused on problem solving. Couples practiced the problem-solving model using a cancer-related problem. Session 7 focused on emotion-focused coping and included partner-assisted cognitive restructuring practice. The group chose a relaxation skill to practice. Session 8 focused on assisting couples in identifying priorities and preparing the couple for the post-treatment “survivorship” phase. Home assignments were given to couples after Sessions 1 to 7 (e.g., relaxation practice, granting the wish on one’s partner’s Wish List). The ECG manual is available from the study’s first author.
SG
SG also involved eight 90-minute group sessions led by two therapists. The approach was person-centered and supportive in nature (Boy, 1990; Hobbs, 1964). The leaders encouraged participants to share their experiences with cancer, to express their emotions related to the experience, to voice problems they have in coping with the cancer, and to offer support to group members. Commonalities were drawn between members’ experiences. Each group had a topic for discussion: learning more about each other, making sure your needs are met, challenges with health providers, coping with physical and sexual changes, coping with family and friends, dealing with employment and life tasks, and coping with the future, and survivorship. No formal or didactic information related to relationship communication or coping/stress management was provided. The SG manual is available from the study’s first author.
Group leaders and supervision
Thirty-five interventionists served as leaders. The majority were master’s level social workers or psychologists (n = 25) or doctoral level psychologists (n = 8). Ninety-one percent had prior group therapy experience and 90% had prior couples’ therapy experience. Leaders underwent 6–8 hours of training in the manual-based ECG and equivalent training in SG with viewing of videotaped sessions and role play practices of groups. To facilitate treatment fidelity, the ECG manual was structured and contained in-session exercises and handouts for participants. The SG manual included readings on supportive group therapy and rules regarding what was considered supportive (e.g., reflection, transparency, validation) and what was not considered supportive (e.g., teaching coping skills).
Telephone supervision was provided after each group session (that is, the supervisor listened to all groups in this study). A video-recording was rated by the supervisor using a fidelity checklist, and written comments were provided. The ECG fidelity checklist contained ratings of whether each topic was addressed and whether home assignments were reviewed. The SG fidelity checklist contained ratings of the degree to which each group topic was explored and the degree to which supportive techniques were used (e.g., maintaining cancer focus, validation, and creating a sense of being understood).
Outcome Measures
Anxiety, Depression, and Psychological well-being
Participants completed the Anxiety (9 items) and Depression (4 items), and the Well-being (10 items) subscales of the Mental Health Inventory-38 (Veit & Ware, 1983). Participants used a 6-point Likert scale to rate their feelings over the past month. Internal consistencies for the patient scales ranged from .87 (Depression, Time 3) to .93 (Anxiety, Time 4), and internal consistencies for spouse scales ranged from .86 (Depression, Time 2) to .95 (Well-being, Time 4)
Cancer distress
Participants completed the Impact of Events Scale (IES, Horowitz, Wilner, & Alvarez, 1979), which is a 21-item measure focusing on intrusive and avoidant ideation associated with a stressor, in this case breast cancer and its treatment. Using a 4-point Likert scale, participants rated how true each statement was during the past week (scale range = 0–75). Internal consistencies ranged from .92 to .94 for patients and from .92 to .93 for spouses.
Relationship Satisfaction
Participants completed the Dyadic Adjustment Scale (DAS; Spanier, 1975). The DAS is a widely-used 32 item measure of satisfaction with intimate relationships. Higher scores indicated more satisfaction. The maximum score is 151, and the cutoff score that was used to indicate marital distress was 97. Cronbach’s alphas ranged from .93 to .94 for patients and spouses.
Moderator Measures
Perceived partner unsupportive behaviors (Manne & Schnoll, 2001)
Patients completed the 13-item perceived partner unsupportive behaviors scale, which assessed patient perceptions of critical responses from the spouse. Internal consistency was .91 for patient ratings.
Cancer distress and relationship satisfaction
Time 1 scores on the measures described above were included as moderators in the analyses.
Covariate Measures
Demographic measures
Participant age, sex, race were collected.
Medical variables
Data regarding current disease stage, date of diagnosis, and Eastern Cooperative Oncology Group performance status ratings (ECOG; Zubrod et al., 1960) were obtained from chart.
Physical impairment
The 26-item functional status subscale of the Cancer Rehabilitation Evaluation System (CARES: Schag & Heinrich, 1988) was used (range = 0–104). Cronbach’s alpha was .93.
Treatment evaluation and Treatment Fidelity
Treatment evaluation
A 21-item version of Borkovec and Nau’s (1972) scale was administered after the last group. Using Likert ratings, items assessed how logical and successful sessions were, how helpful leaders were, whether the participant learned something new, whether topics were important, interesting, and tuned into needs. Coefficient alphas for ECG were .81 for patients and .94 for spouses. Alphas for SG were .89 for patients and spouses.
Treatment Fidelity
The ECG checklist was created from the manual. Criteria consisted of topics covered in each session, whether in-session exercises were conducted, and whether home assignments were given (yes/no). The score consisted of the percentage of topics completed. The SG checklist was based on supportive group therapy techniques (Novalis et al., 1993, p.58). The checklist consisted of ratings of seven techniques (e.g., reflection, validation, draw commonalities) and techniques not consistent with the model (interruption) Occurrence of each technique in 10-minute segments was rated. Rater training consisted of a manual and criteria review and practice ratings using a ten sessions previously rated by the project manager. For SG, two raters coded together and consensus was reached for each code.
Data Analytic Approach
Dyadic growth models were estimated using multilevel modeling with restricted maximum likelihood. In these models, a person’s outcome (e.g., anxiety) at a particular time point was predicted to be a function of all main effects and interactions of three variables: the treatment condition (ECG versus SG), the person’s role (patient versus spouse), and a linear function of time. In addition to these key predictors, patient age, ethnicity (white versus nonwhite), cancer stage (0 and 1 versus 2a, 2b, 3a), patient physical impairment, recruitment site, and attendance status (yes/no) were treated as covariates. All dichotomous categorical predictors were effects coded (i.e., 1, −1), and quantitative predictors, including data collection wave, were grand-mean centered, and so the intercepts refer to the grand mean of the outcome. Random effects included in the models were random intercepts (i.e., the extent to which participants varied in their average responses), the dyadic correlation between the intercepts (e.g., if one person was high in average anxiety was the other partner also relatively high on average), random slopes for time and the dyadic correlation between the slopes (e.g., if one person’s anxiety is increasing over time, is the partner’s anxiety also increasing), random residuals, and the dyadic correlation between the residuals (e.g., if one person’s anxiety was especially high at a particular assessment point, was the partner’s anxiety also especially high).
Results
Descriptive Information about Enrollment, Attendance, and Participants
Enrollment, Attendance, and Attrition
Figure 1 illustrates the study flow. 302 couples consented and completed a Time 1 survey. Of these 302 couples, 151 were assigned to ECG and 151 were assigned to SG. In total, there were 29 ECG groups and 31 SG groups conducted. If one partner was not able to attend a group session, the other partner was permitted to attend. Twenty-five couples/one partner (16.6%) attended none or one ECG session and 27 couples/one partner (17.9%) attended none or one SG session. One hundred seven couples/one partner (71%) attended seven or all 8 ECG sessions and 119 couples/one partner (79%) attended all eight SG sessions. The average number of group sessions attended by one or both partners was 6.2 (SD = 2.99; range 0–8).
Survey completion is shown in Figure 1. Of the 302 couples who completed Time 1 surveys, 254 patients and 253 spouses completed Time 2 (84.3%), 235 patients and 236 spouses completed Time 3 (77.8%), and 215 patients and 214 spouses completed Time 4 (71.2%). Attrition analyses comparing patients who completed all surveys with patients who dropped after completing Time 1 on available variables indicated that completers were older (t (266) = 2.8, p < .01, M completers = 56.7, M dropped = 50.3) and married longer (t (264) = 2.4, p < .05, M completers = 26.1 years, M dropped = 20.5 years) than drops. Spouse completers were also significantly older than drops (t (264) =3.6, p < .001, M completers = 58.1 years, M dropped = 52 years).
Pre-intervention differences and distress characteristics
Table 1 contains summary data for the participants by study condition regarding demographic and medical characteristics. Multivariate analysis of covariance and chi-square tests, in which hospital site served as a covariate, revealed no differences between the two conditions regarding any of the demographic or medical variables included in Table 1. However, there were significant site differences on all primary outcomes such that one site was significantly higher on anxiety, depression, and lower on well-being and relationship satisfaction. To account for these site differences, a dichotomous site variable was created in which that particular site was coded as 1 and the other sites were coded as −1, and this variable was included as a covariate in all analyses.
Table 1.
Pre-Intervention Demographic and Disease Information by Intervention Group
| SG |
ECG |
|||
|---|---|---|---|---|
| Variable | Patients (n= 151) |
Spouses (n= 151) |
Patients (n= 151) |
Spouses (n=151) |
| Age (years) | 54.4 (9.9) | 55.5 (11.1) | 55.8 (10.9) | 57.1 (11.6) |
| Sex | ||||
| Female | 151 (100) | 0 (00) | 151 (100) | 2 (1.4) |
| Male | 0 (0) | 151 (100) | 0 (0) | 149 (98.6) |
| Race | ||||
| Non-hisp white | 130 (86.1) | 121 (80.1) | 129 (85.4) | 128 (84.1) |
| Black | 14 (9.3) | 13 (8.6) | 12 (7.9) | 13 (8.6) |
| Asian | 1 (0.7) | 1 (0.7) | 2 (1.3) | 2 (1.3) |
| Hispanic | 4 (2.6) | 11 (7.3) | 6 (4.0) | 4 (2.6) |
| Hawaiian/Pacific | 1 (0.7) | 0 (0) | 1 (0.7) | 0 (0) |
| Islander | ||||
| Other | 1 (0.7 | 3 (2.0) | 1 (0.7) | 2 (1.3) |
| Missing | 0 (0) | 2 (1.3) | 0 (0) | 2 (1.3) |
| Years of education | ||||
| < college | 60 (39.7) | 59 (39.1) | 67 (44.4) | 67 (44.3) |
| > college | 89 (58.9) | 92 (60.0) | 84 (55.6) | 82 (54.3) |
| Missing | 2 (1.3) | 0 | 0 | 2 (1.3) |
| Median income | $100,000 | $100,000 | $95,000 | $95,000 |
| Relationship Length (years) |
23.7 (13.3) | 25.5 (15.5) | ||
| Employment | ||||
| Full-time | 67 (44.4) | 96 (63.6) | 55 (36.4) | 90 (59.6) |
| Part-time | 18 (11.9) | 7 (4.6) | 19 (12.6) | 8 (5.3) |
| Not working | 65 (43.0) | 45 (27.8) | 77 (50.9) | 51 (31.1) |
| Missing | 1 (0.7) | 3 (2.0) | 0 (0) | 1 (.7) |
| Psych. Care (yes) | 75 (49.7) | 19 (12.6) | 147 (48.7) | 29 (19.2) |
| ECOG rating | ||||
| 0 | 132 (87.4) | 135 (89.4) | ||
| 1 | 14 (9.3) | 12 (7.9) | ||
| Missing | 5 (3.3) | 4 (2.6) | ||
| Stage of disease | ||||
| 0 | 42 (27.8) | 37 (24.5) | ||
| 1 | 56 (37.0) | 67 (44.3) | ||
| 2 | 47 (32.1) | 38 (25.2) | ||
| 3a | 6 (4.0) | 9 (5.6) | ||
| Months since dx | 4.8 (2.5) | 4.9 (2.5) | ||
| Range | < 1 −13.6 | 1 – 13.6 | ||
| Surgery | ||||
| Mastectomy | 74 (49.9) | 82 (54.3) | ||
| BCS | 77 (51.0) | 69 (45.7) | ||
| Current treatment | ||||
| None | 74 (49.0) | 70 (46.4) | ||
| Chemotherapy | 46 (30.5) | 39 (25.8) | ||
| Radiation | 27 (17.9) | 32 (21.2) | ||
| Chemo/Rad | 2 (1.3) | 3 (2.0) | ||
| Missing | 2 (1.3) | 7 (4.6) | ||
| Hospital Site | ||||
| Bryn Mawr | 6 (4.0) | 6 (4.0) | ||
| Christiana | 74 (49.0) | 75 (49.7) | ||
| CINJ | 6 (4.0) | 5 (3.3) | ||
| Cooper | 16 (10.6) | 17 (11.3) | ||
| FCCC | 33 (21.9) | 35 (23.2) | ||
| Virtua | 16 (10.6) | 13 (8.6) | ||
Note. Numbers in parentheses are percentages for categorical variables and standard deviations for continuous variables (age, relationship length). Sample sizes are pre-intervention figures. Dx = diagnosis, BCS = breast-conserving surgery, CINJ = Cancer Institute of New Jersey, FCCC = Fox Chase Cancer Center
Table 2 contains the pre-intervention means and standard deviations for the distress measures. To determine rates of depression, we used a cutoff of >1.5 SD above the normative mean (Veit & Ware, 1983). Using this cutoff, 38.4% of patients and 48.7% of spouses had high depressive symptom scores. In terms of cancer distress, the threshold for a high IES scores is greater than 19 (Horowitz, 1982). Using this criterion, 72% of patients and 54% of spouses scored over the IES threshold of 19 at Time 1 (Horowitz, 1982). DAS scores in the distressed marriage range (< 97; Spanier 1975) were low, with only 11% of patients and spouses reporting less than 97 at Time 1.
Table 2.
Means and Standard Deviations for Study Outcomes by Intervention Group
| SG |
ECG |
|||
|---|---|---|---|---|
| Variable | Patients | Spouses | Patients | Spouses |
| Depression | ||||
| Time 1 | 8.8 (3.4) | 8.4 (3.2) | 8.9 (3.5) | 8.4 (3.5) |
| Time 2 | 7.8 (2.9) | 7.3 (2.9) | 7.6 (3.2) | 7.4 (2.8) |
| Time 3 | 7.4 (2.9) | 7.0 (2.8) | 7.2 (3.0) | 7.1 (2.9) |
| Time 4 | 7.2 (2.9) | 6.7 (2.5) | 7.3 (3.6) | 7.0 (3.0) |
| Anxiety | ||||
| Time 1 | 20.5 (8.0) | 19.1 (6.9) | 21.1 (8.2) | 19.3 (7.1) |
| Time 2 | 18.4 (6.9) | 17.0 (5.7) | 18.7 (7.2) | 17.7 (6.4) |
| Time 3 | 18.0 (7.4) | 16.4 (5.7) | 17.6 (6.8) | 17.2 (6.4) |
| Time 4 | 17.2 (6.0) | 15.6 (4.7) | 17.8 (7.1) | 16.4 (6.3) |
| Cancer Distress | ||||
| Time 1 | 33.5 (21.6) | 26.1 (19.0) | 33.9 (21.9) | 24.2 (18.7) |
| Time 2 | 26.3 (20.4) | 19.2 (17.0) | 25.6 (19.3) | 18.4 (16.8) |
| Time 3 | 20.8 (18.8) | 15.6 (15.7) | 22.6 (19.8) | 15.3 (15.0) |
| Time 4 | 20.6 (18.2) | 14.1 (14.1) | 19.3 (20.5) | 13.4 (14.7) |
| Well-being | ||||
| Time 1 | 57.4 (13.3) | 56. 9 (12.1) | 57.0 (13.7) | 56.5 (13.5) |
| Time 2 | 61.0 (12.4) | 60.4 (11.7) | 61.5 (12.8) | 59.7 (12.4) |
| Time 3 | 62.3 (11.8) | 61.2 (12.5) | 62.9 (12.7) | 61.9 (11.0) |
| Time 4 | 62.7 (11.1) | 62.1 (12.5) | 62.4 (13.2) | 62.4 (12.1) |
| Relationship Satisfaction | ||||
| Time 1 | 116.9 (16.3) | 116.9 (16.8) | 115.9 (18.0) | 116.7 (17.2) |
| Time 2 | 119.4 (15.5) | 119.1 (17.0) | 121.3 (14.5) | 118.9 (17.0) |
| Time 3 | 117.7 (16.1) | 119.9 (14.8) | 120.3 (14.6) | 120.3 (11.0) |
| Time 4 | 117.3 (15.1) | 118.3 (15.4) | 119.6 (17.7) | 119.1 (16.8) |
Treatment evaluation
Patient ratings were high for ECG (item M = 4.3, scale range 1–5) and SG (item M = 4.2). Spouse ratings were high for ECG (item M = 4.0) and SG (item M = 4.2).
Treatment Fidelity
A random subset of 30% of each session (e.g., 30% of all Session 1s, 30% of all Session 4s, etc.) were rated for treatment fidelity. For ECG, mean fidelity ranged from 88% (Group 1) to 98% (Group 4). For SG, the occurrence of supportive interventions and interventions not consistent with supportive interventions (e.g., interpretation) was rated for each 10 minute segment. The average percentage of segments where leaders engaged in techniques consistent with the model ranged from 1% for skills not utilized frequently in this model (transparency; leader self-disclosure) to 99% for skills used in most sessions (e.g., reflection, foster emotional expression).
Intervention effects
Table 3 reports the fixed effect regression estimates for the analyses of the five outcomes. Looking first at the effects of the covariates, couples in which the patient was older tended to report significantly lower anxiety, depression, and cancer distress, as well as significantly higher well-being and relationship satisfaction. Effect sizes as calculated by Cohen’s ds ranged from d = .29 for anxiety to d = .55 for well-being. Couples in which the patient was white reported significantly higher anxiety (d = .22) and significantly lower well-being (d = .33). Physical impairment also related to four of the five outcomes such that when the patient experienced greater impairment, the couple on average reported significantly greater anxiety, depression, and cancer distress, as well as significantly lower well-being (ds ranged between .75 and .81). As noted previously, recruitment site also showed significant effects, with one of the six sites having significantly more negative/less positive outcomes (ds ranged between .24 and .38). Finally, cancer stage and session attendance did not predict any of the outcomes.
Table 3.
Multilevel modeling results for predicting outcomes as a function of condition, time, and role (patient versus spouse), controlling for covariates.
| Anxiety | Depression | Cancer Distress | Well-Being | Relationship Satisfaction |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| b | t (df) |
b | t (df) |
b | t (df) |
B | t (df) |
b | t (df) |
|
| Intercept | 18.15 | 7.76 | 22.21 | 60.91 | 114.79 | |||||
| Patient Age | −.063* | 2.42 (285) |
−.036** | 3.06 (282) |
−.209** | 2.99 (286) |
.233** | 4.61 (286) |
.235** | 2.97 (284) |
| Cancer Stage | −.370 | 1.29 (285) |
.017 | 0.13 (281) |
1.242 | 1.63 (287) |
−.094 | 0.17 (286) |
.069 | 0.08 (283) |
| White | .867* | 2.16 (378) |
.336 | 1.87 (379) |
1.222 | 1.16 (391) |
−2.496** | 3.32 (417) |
.133 | 0.12 (507) |
| Physical Impairment | .102** | 6.81 (286) |
.046** | 6.80 (283) |
.268** | 6.72 (287) |
−.185** | 6.38 (287) |
−.082 | 1.81 (284) |
| Treatment Site | .750* | 2.12 (303) |
.431** | 2.69 (302) |
1.184 | 1.25 (308) |
−2.246** | 3.28 (302) |
−3.100** | 2.83 (291) |
| Attended Sessions | −.255 | 0.70 (342) |
−.011 | 0.06 (348) |
1.067 | 1.04 (360) |
−.676 | 0.96 (337) |
1.315 | 1.20 (317) |
| Time | −.954** | 10.60 (241) |
−.454** | 9.96 (250) |
−3.965** | 13.62 (245) |
1.607** | 9.70 (240) |
.177 | 0.84 (191) |
| Role | .535* | 2.45 (282) |
.115 | 1.22 (281) |
3.331** | 6.22 (273) |
.630 | 1.82 (293) |
−.000 | 0.00 (276) |
| Time*Role | −.064 | 0.75 (233) |
−.025 | 0.66 (244) |
−.473 | 1.94 (241) |
.059 | 0.47 (248) |
−.082 | 0.51 (203) |
| Condition | .220 | 0.84 (286) |
.022 | 0.19 (280) |
−.040 | 0.06 (287) |
−.263 | 0.52 (287) |
−.227 | 0.29 (284) |
| Condition*Time | .052 | 0.58 (243) |
.033 | 0.73 (254) |
.114 | 0.40 (248) |
−.081 | 0.49 (243) |
.107 | 0.51 (193) |
| Condition*Role | .015 | 0.07 (282) |
.011 | 0.12 (281) |
.371 | 0.69 (273) |
.031 | 0.09 (293) |
.125 | 0.34 (276) |
| Condition*Time*Role | −.062 | 0.72 (233) |
−.024 | 0.64 (244) |
−.096 | 0.40 (241) |
−.031 | 0.25 (248) |
.083 | 0.52 (203) |
Note.
p < .05,
p < .01.
Physical impairment is for the patient. Cancer stage is coded stage = −1 if stage was 0 or 1 and stage = 1 if stage was 2a, 2b, or 3a. White was coded as 1 if the patient race was white and −1 otherwise. Attended sessions was 1 if at least one partner attended more than 2 sessions and −1 otherwise. Role was coded patient = 1, spouse= −1. Condition was coded 1 = ECG, −1 = SG. All quantitative variables were grand-mean centered prior to analysis.
The bottom half of Table 3 presents the estimates and tests of the key study predictors: condition, role, and time. As can be seen in the bottom four rows of the table, there were no main effects or interactions involving treatment condition. For example, the lack of condition main effects suggests that there were no statistically significant differences in average outcomes by intervention condition, averaging over time and role. Similarly, the lack of a condition by time interaction suggests that change over time was similar for ECG and SG couples. Indeed, the only significant effects were for the main effects of time and role. Specifically, negative outcomes (i.e., anxiety, depression, and cancer distress) decreased significantly over time, and well-being increased significantly over time (ds between 1.25 and 1.74). The two significant role effects indicate that patients reported significantly higher anxiety and cancer distress on average than did their spouses (ds .29 and .75 respectively). Finally, as shown in Table 3, there were no differences in relationship satisfaction as a function of time, role, or treatment condition.
Moderation Analyses
We examined the extent to which patient status on three variables measured at Time 1 moderated the effects of the treatment condition. All moderators were grand mean centered, and simple slopes analyses used to follow-up significant interactions were estimated for one standard deviation above and below the mean on the moderator. The moderator variables included the patient’s initial cancer distress, the patient’s perceived partner unsupportive behavior, and the patient’s initial relationship satisfaction. Table 4 shows the results for the moderation analyses for factors involving treatment condition (e.g., the moderator by condition interaction, the moderator by condition by time interaction). Note that although not included in Table 4, the moderation models included the same covariates as in the primary analyses, as well as all main effects and interactions between treatment condition, role, time, and the moderator. Results for the full models are available from the authors.
Table 4.
Moderation results testing whether patient’s initial distress, perceptions of unsupportive partner behavior, and relationship satisfaction moderate the effects of treatment condition, time, and role.
| Anxiety | Depression | Cancer Distress | Well Being | Relationship Satisfaction | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Moderator Variable | b | t (df) |
b | t (df) |
b | t (df) |
b | t (df) |
b | t (df) |
| Initial Cancer Distress (CD) | .103** | 8.84 (274) |
.040** | 7.19 (274) |
14.13 (291) |
−.137** | 5.59 (283) |
−.185** | 4.68 (280) |
|
| CD*Condition | .039** | 3.74 (277) |
.012* | 2.44 (274) |
−.011 | 0. 45 (283) |
−.063** | 2.81 (284) |
−.069 | 1.93 (282) |
| CD*Condition*Time | .002 | 0.60 (233) |
−.000 | 0.07 (247) |
−.003 | 0.28 (263) |
−.005 | 0.70 (239) |
−.006 | 0.58 (187) |
| CD*Condition*Role | −.031** | 3.25 (283) |
−.011* | 2.50 (282) |
−.022 | 1.01 (278) |
.041** | 2.67 (294) |
.017 | 0.99 (277) |
| CD*Condition*Time*Role | .007 | 1.72 (235) |
.001 | 0.39 (243) |
.009 | 0.80 (265) |
−.007 | 1.11 (252) |
−.008 | 1.07 (197) |
|
Initial Perceived Partner Unsupportive Behavior (UnSupp) |
.215** | 5.00 (286) |
.106** | 5.51 (281) |
.520** | 4.44 (289) |
−.519** | 6.36 (286) |
−1.27** | 11.14 (286) |
| UnSupp *Condition | .097* | 2.36 (288) |
.019 | 1.00 (283) |
.029 | 0.26 (291) |
−.041 | 0.53 (287) |
−.045 | 0.42 (287) |
| UnSupp *Condition*Time | .016 | 1.09 (427) |
.001 | 0.08 (257) |
.007 | 0.14 (253) |
−.017 | 0.61 (246) |
−.010 | 0.30 (191) |
| UnSupp *Condition*Role | −.066 | 1.90 (283) |
−.017 | 1.11 (283) |
−.027 | 0.31 (277) |
.078 | 1.38 (297) |
.071 | 1.21 (280) |
| UnSupp*Condition*Time*Role | .039** | 2.78 (366) |
.010 | 1.65 (245) |
.030 | 0.73 (248) |
−.037 | 1.76 (253) |
−.010 | 0.38 (204) |
|
Initial Relationship Satisfaction (Rel) |
−.090** | 5.57 (258) |
−.048** | 6.71 (257) |
−.147** | 3.25 (263) |
.262** | 9.23 (261) |
.669** | 23.59 (266) |
| Rel*Condition | −.015 | 0.95 (261) |
−.005 | 0.73 (259) |
.018 | 0.42 (265) |
.020 | 0.74 (262) |
.051 | 1.85 (260) |
| Rel*Condition*Time | −.015** | 2.65 (226) |
−.006 | 1.95 (240) |
−.004 | 0.21 (230) |
.028** | 2.74 (229) |
.022 | 1.89 (239) |
| Rel*Condition*Role | .004 | 0.29 (258) |
−.001 | 0.10 (259) |
−.060 | 1.74 (255) |
−.021 | 0.93 (268) |
−.035 | 1.65 (262) |
| Rel*Condition*Time*Role | −.002 | 0.36 (213) |
.000 | 0.12 (226) |
.011 | 0.71 (224) |
.002 | 0.23 (227) |
.001 | 0.15 (228) |
Note.
p< .05,
p < .01.
Data analysis models included all covariates as well as all main effects and interactions between condition, time, role, and the moderator. Table includes only results involving the moderator and interactions between the moderator and condition.
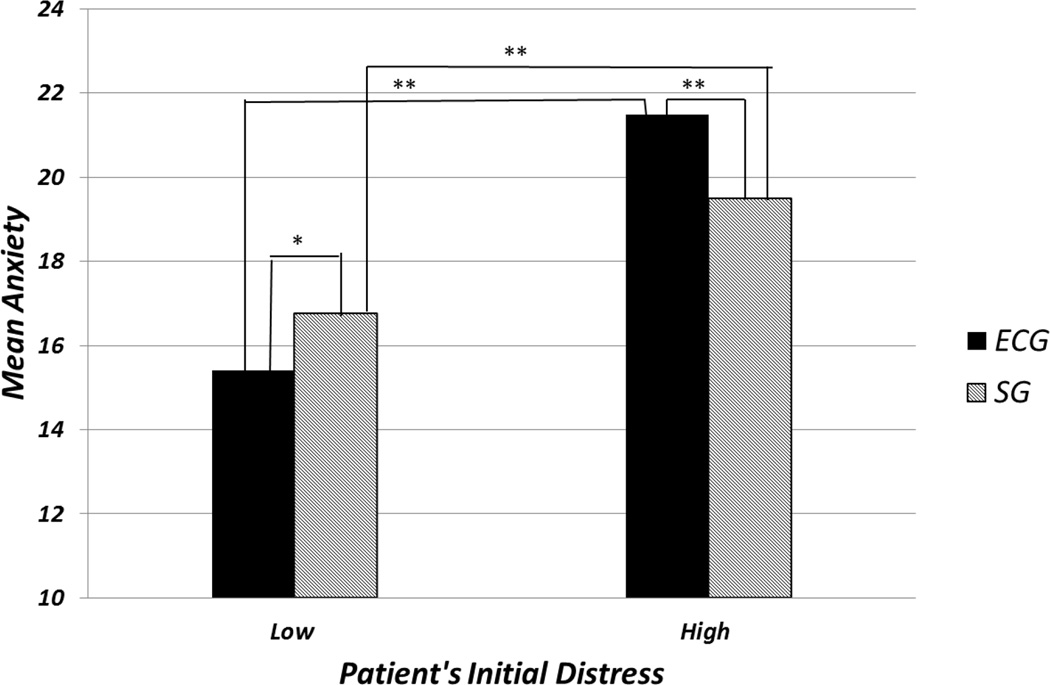
The patient’s initial level of cancer distress moderated the effect of the treatment condition as well as the interaction between treatment condition and role for three of the five outcomes. Note that, because time was grand-mean centered, these interactions, which do not involve time, assess differences in mean outcomes averaged over time. Looking first at the interaction between treatment condition and patient’s initial cancer distress, the same cross-over pattern emerged for anxiety (d = .45), depression (d = .29), and well-being (d = .33), such that when cancer distress was high (i.e., one standard deviation above average) average outcomes, averaging over the two partners and time, were more positive in SG relative to ECG, but when cancer distress was low, average outcomes were more positive in ECG relative to SG. For example, when cancer distress was high the estimated marginal mean for anxiety in SG was M = 19.48 (SE = .63), but in ECG, M = 21.49 (SE = .63). In contrast, when initial cancer distress was low, the estimated marginal mean for ECG was M = 15.40 (SE = .61) but for SG, M = 16.76 (SE = .62). This interaction is graphed in Figure 2. Similarly, for depression, when initial cancer distress was high in SG the estimated marginal mean was M = 8.42 (SE = .30) but in ECG the mean was M = 8.96 (SE = .30) and when initial cancer distress was low, the mean for ECG was M = 6.73 (SE = .29) but for SG M = 7.24 (SE = .29). When initial cancer distress was high, positive well-being was higher in SG, M = 59.22 (SE = 1.32), than in ECG, M = 56.16 (SE = 1.32), and the pattern was reversed when the initial cancer distress was low, ECG M = 64.71 (SE = 1.27) and SG M = 62.43 (SE = 1.28).
Figure 2.
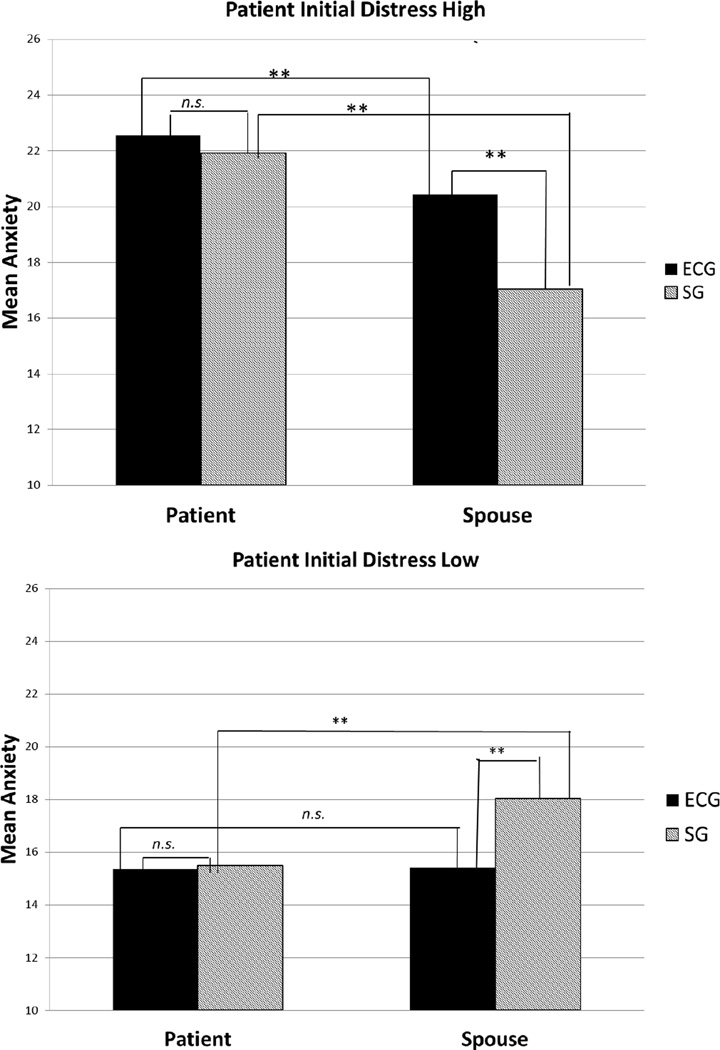
Interaction between treatment condition and patient’s initial cancer distress predicting anxiety. For mean comparisons * p < .05, ** p < .01
The interactions between initial cancer distress and treatment condition were somewhat qualified by individual role (patient versus spouse) in that there were three significant interactions between initial cancer distress, treatment condition, and individual role (ds ranged from .30 to .39). The estimated marginal means and standard errors for these interactions are presented in Table 5, and the interaction predicting anxiety is graphed in Figure 3. In SG, for the two negative outcomes (anxiety, depression) when patient’s initial distress was high, the patient’s negative outcomes were considerably higher than the spouse’s negative outcomes. In contrast, when the patient’s initial cancer distress was low, the spouses’ outcomes were more negative than the patient’s outcomes. The parallel pattern emerges for well-being. In ECG, when patient initial cancer distress was high, the patient’s outcomes were more negative than the spouse outcomes, but when initial cancer distress was low the patients’ and partners’ outcomes were similar. There is one divergence from this pattern. For well-being, when initial cancer distress was high, patients and partners in ECG were similar in well-being, but when initial cancer distress was low, patient well-being was higher than spouse well-being.
Table 5.
Estimated marginal means and standard errors describing the three-way interaction between patient initial cancer distress, treatment condition, and role
| ECG |
SG |
|||
|---|---|---|---|---|
| Patient | Spouse | Patient | Spouse | |
| M (SE) | M (SE) | M (SE) | M (SE) | |
| Anxiety | ||||
| Initial CD High | 22.55 (0.73) | 20.43 (0.77) | 21.92 (0.73) | 17.04 (0.78) |
| Initial CD Low | 15.37 (0.70) | 15.42 (0.77) | 15.48 (0.71) | 18.03 (0.76) |
| Depression | ||||
| Initial CD High | 9.32 (0.33) | 8.61 (0.37) | 9.24 (0.33) | 7.60 (0.37) |
| Initial CD Low | 6.61 (0.32) | 6.86 (0.37) | 6.67 (0.32) | 7.80 (0.36) |
| Well-Being | ||||
| Initial CD High | 56.21 (1.42) | 56.12 (1.52) | 57.30 (1.42) | 61.15 (1.53) |
| Initial CD Low | 66.15 (1.37) | 63.27 (1.50) | 65.42 (1.38) | 59.44 (1.49) |
Note. CD = Cancer Distress.
Figure 3.
Interaction between treatment condition, patient’s initial cancer distress, and role (patient vs. spouse) predicting anxiety. For mean comparisons within level of distress * p < .05, ** p < .01
Table 4 also shows that the patient’s initial perception of partner unsupportive behavior moderated the effect of condition for anxiety (d = .28), but not for the other outcomes. The moderated treatment effect for high and low partner unsupportive behavior revealed a pattern similar to that found for patient’s initial cancer distress. When the patient’s perceived partner unsupportive behavior was high, couples in SG, M = 18.49 (SE = .66), were less anxious on average (averaging over person and time) than were couples in ECG, M = 20.22 (SE = .69), but when the patient’s perceived partner unsupportive behavior by the spouse was low, average anxiety in ECG, M = 16.37 (SE = .69), was lower than in SG, M = 17.03 (SE = .71).
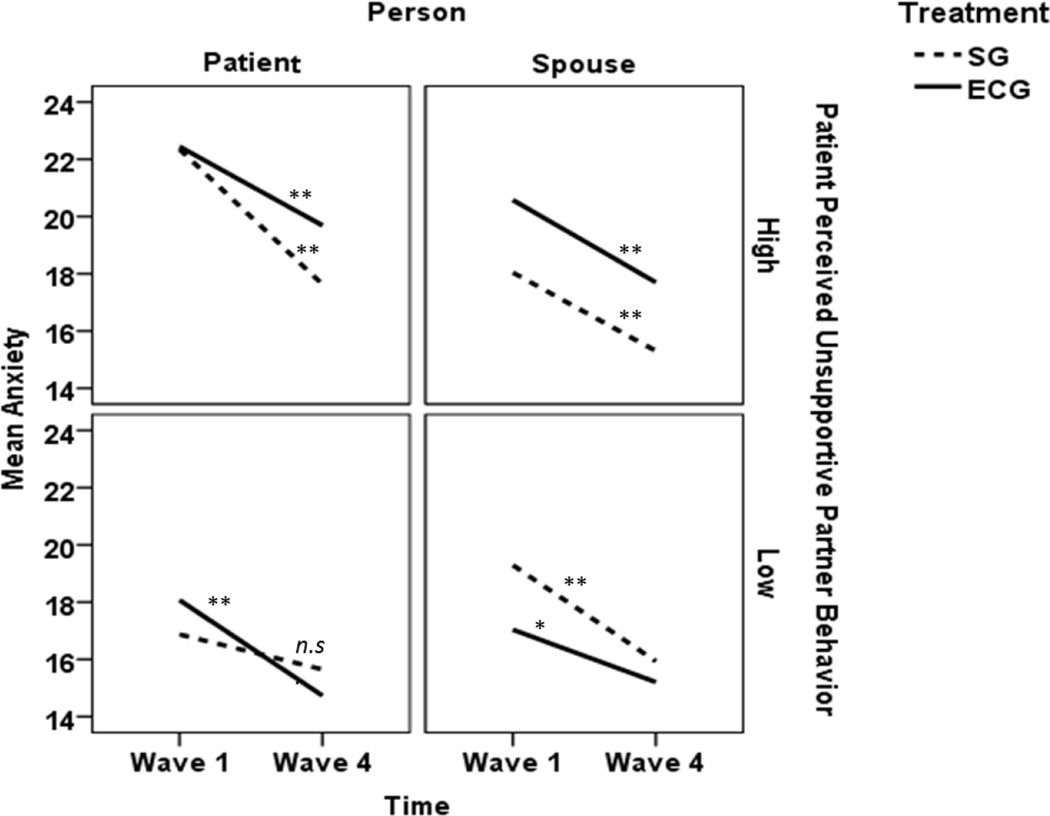
There was also a significant four-way interaction between patient initial perceived partner unsupportive behavior, time, treatment condition, and role for anxiety (d = .29; see Figure 4). Simple slopes analyses indicated that when partner unsupportive behavior was high, there was a marginally significant positive interaction between treatment and time for patients, b = .328, t (247) = 1.86, p = .064, but when partner unsupportive behavior was low, this interaction was significantly negative, b = −.353, t (246) = 2.04, p = .042. Neither interaction was significant for spouses. When the patient’s perceived partner unsupportive behavior was high, patients decreased in anxiety over time to a greater degree in SG, b = −1.575, t (236) = 6.58, p < .001, than in ECG, b = −.920, t (256) = 3.55, p < .001. In contrast, when patient perceived unsupportive partner behavior was low, patients in ECG dropped more over time, b = −1.114, t (245) = 4.62, p < .001 than in SG, b = −.408, t (247) = 1.64, p = .103.
Figure 4.
Interaction between treatment condition, role (patient vs spouse), and perceived partner unsupportive behavior predicting anxiety. Slopes are significantly different from zero if * p < .05, ** p < .01
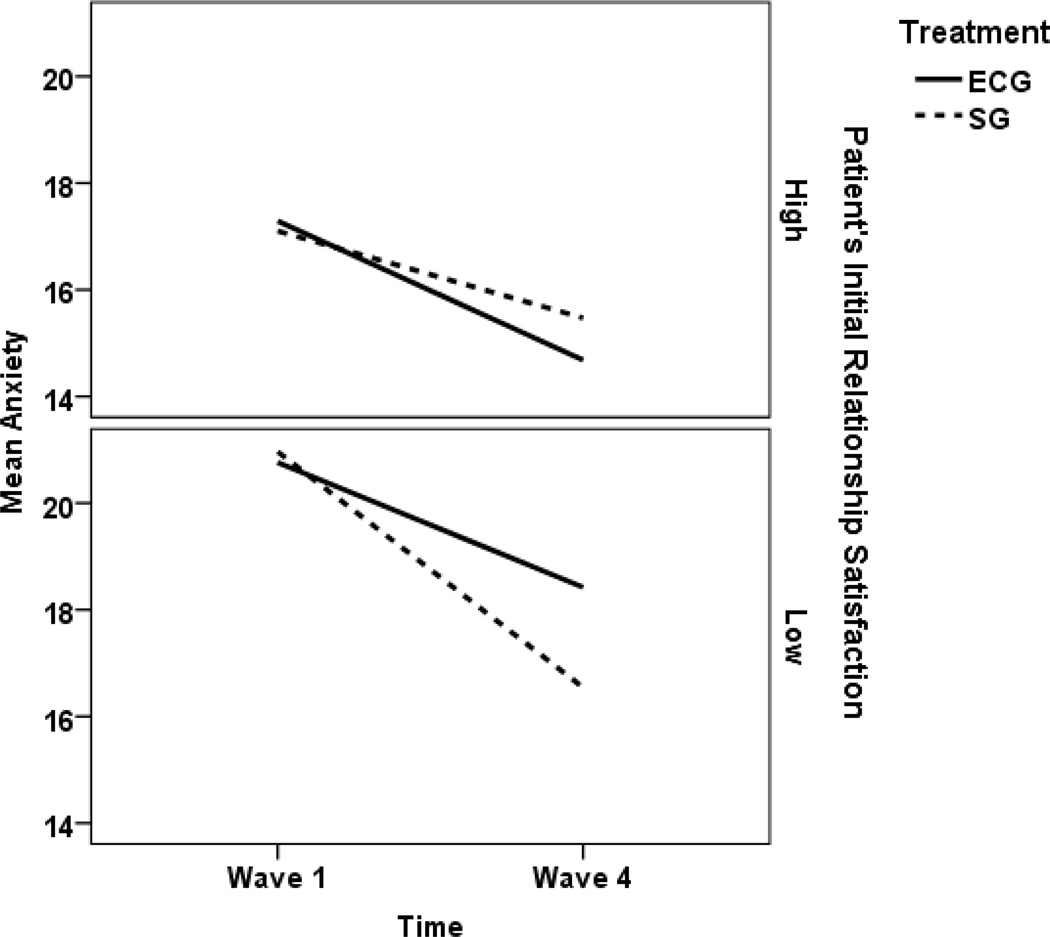
Finally, when patient’s initial relationship satisfaction was treated as a moderator, interactions between initial satisfaction, condition, and time emerged for anxiety (d = .35) and well-being (d = .36), but not for the other three outcomes. These interactions, one of which is graphed in Figure 5, suggest that although anxiety decreased over time and well-being increased over time, the patient’s initial relationship satisfaction had a much stronger effect in SG relative to ECG. That is, in ECG for patients with high initial relationship satisfaction, the change in anxiety over time was b = −.873, t (210) = 4.68, p < .001 and for patients in ECG with low initial relationship satisfaction, this change was similar b = −.785, t (239) = 3.94, p < .001. In contrast, in SG when the patient reported high initial relationship satisfaction both partners showed moderate decreases in anxiety over time, b = −.542, t (212) = 2.90, p = .004 but when initial relationship satisfaction was low, this decrease was especially strong, time b = −1.481, t (223) = 7.71, p < .001. The same pattern emerged for well-being, ECG with high initial relationship satisfaction, time b = 1.728, t (214) = 5.21, p < .001, ECG with low initial relationship satisfaction, time b = 1.513, t (241) = 4.31, p < .001, SG with high relationship satisfaction, time b = .958, t (215) = 2.88, p = .004, SG with low initial relationship satisfaction, time b = 2.622, t (224) = 7.72, p < .001.
Figure 5.
Interaction between treatment condition, time, and patient’s initial relationship satisfaction predicting anxiety. All simple slopes are significantly different from zero.
Discussion
This article is the first to report the results of a randomized, controlled couple-focused group intervention comparing two group therapy approaches for women treated for localized breast cancer and their spouses. The strength of this randomized controlled clinical trial included multilevel analyses which evaluated the impact of the interventions on dyads, the close attention to treatment fidelity to each model with weekly supervision, and the one year follow-up. The results did not support the study’s primary hypothesis. Depression, anxiety, and cancer distress declined and well-being improved for couples enrolled in both ECG and SG. That is, neither treatment was superior in terms of reduction of distress or improvements in well-being, and the effect sizes for these changes over time were quite large. Our results were not consistent with our moderator hypothesis that ECG would have stronger effects for more distressed patients. Rather, each group intervention was more effective for patients with different personal and relationship characteristics. Among patients reporting higher levels of pre-intervention cancer distress, average anxiety and depression were lower among SG couples than ECG couples over the one year time period patients were followed. However, when pre-intervention patient cancer distress was low, average anxiety and depression were lower among ECG couples relative to SG couples. The same effects were seen when psychological well-being was examined. Moreover, a similar pattern was illustrated when the moderator effect for pre-intervention patient-reported marital satisfaction was examined as a moderator and anxiety and well-being were evaluated as outcomes. For pre-intervention perceived unsupportive partner behavior, the same result was seen for anxiety: When patients’ perceived unsupportive partner behavior was high, average anxiety was lower in SG than in ECG, but when patients’ unsupportive partner behavior was low, anxiety was lower in ECG than in SG. Furthermore, when patients’ perceived unsupportive behavior was high, it was the patients in SG who decreased most in anxiety over time, but when patient’s perceived unsupportive behavior was low, the patients in ECG decreased in anxiety over time to a greater degree than patients in SG. This consistent pattern for anxiety, and to a lesser extent, for well-being, indicates that the SG was more effective for couples in which the patient reported more individual distress and/or relationship distress, and the skill-based ECG was more effective for couples in which the patient was not distressed, either individually or in their relationship. In terms of clinically-meaningful effects, the moderator effect sizes were consistently in the small to moderate range in size. Thus, our results suggest that the moderator effects may represent a clinically-significant change.
There are several studies indicating that distressed cancer patients may benefit more from psychological interventions (Helgeson, Lepore, & Eton, 2006; Scheier et al., 2007), but these studies evaluate individual therapy rather than group- or couple-based therapy. However, there is very little known about putative moderators for either group-based or couple-based approaches for cancer patients. Helgeson and colleagues (2000) compared an educational group with a peer-led discussion group for women diagnosed with early stage breast cancer. They found that educational groups showed greater benefits on the physical fu55nctioning of women who started the study with fewer psychological resources as compared with women with more psychological resources. They also found that peer-led discussion groups were helpful for women who lacked support from their partners or physicians, but harmful for women who had high levels of support. In our prior study evaluating the couple-focused skill-based group intervention which is similar in the approach used in the ECG, we found that the skill-based intervention had stronger effects on women who began the group experience with higher levels of perceived partner unsupportive behavior (Manne et al., 2005). When hypothesizing about the reasons why SG was more effective among couples where the patient was more distressed, less supported by her spouse, and/or less satisfied with her relationship, the explanation may lie in the SG’s processes and goal. The primary goal of SG was to foster the expression of feelings about the cancer experience, facilitate group support, and provide validation, reassurance, and a greater understanding among group members that they have experiences in common. There was a great deal more interaction between group members in SG as compared with ECG. Thus, distressed patients in SG may be able to obtain desired reassurance and support from other group members – both from other patients and other patients’ spouses. Patients reporting unsupportive responses from their spouse may be able to bolster their perceived support from other group members. Spouses who are unsupportive (perceived as such by the patient) may be able to observe other spouses providing empathy, validation, and support to both their own partner and other patients in the group. Because ECG was skill-based and couples practiced skills separately with one another during the group sessions, couples did not engage in group discussions where observing other couples interact was possible. Although an in-depth examination of group therapy processes is beyond the scope of this study, our preliminary results suggest that group engagement as measured by the Group Climate Questionnaire (GCQ; MacKensie, 1983) (e.g., the degree to which the group is characterized by mutual liking and caring, and by collaborative, problem solving efforts, active participation, and self-disclosure) and group support as measured by the Emotional Support Scale (Zimet et al., 1988) adapted for a group format (J. Johnson, personal communication, June 1, 2006) (defined as the degree of emotional support offered by the group to the participant) was significantly higher among patients and partners in SG as compared with ECG. In addition, group avoidance as measured by the GCQ (defined as the degree to which members are dependent on the leader, experience remoteness from other group members, and conform to norms) and the group conflict as measured by the GCQ (defined as friction and anger between group members) was rated significantly lower by SG participants than by ECG participants. These findings suggest that SG may have reduced distress among the most distressed patients due to offering them opportunities to express their feelings and obtain support. However, the exact reasons will require future attention to possible mediators.
It was interesting to note that ECG was more effective than SG for patients who had less psychological distress, among patients who perceived that their partners were less unsupportive, and among patients who reported higher levels of marital satisfaction. These findings are surprising in light of the fact that ECG’s focus was on enhancing relationship communication skills, dyadic problem solving, partner-assisted cognitive restructuring, and couples’ stress management, which would be important therapeutic targets for distressed women and/or women reporting less marital satisfaction. Future analyses evaluating the impact of ECG and SG on relationship communication may shed light on the reasons for this finding.
Before closing, it is important to point out limitations and future directions. Most importantly, we had a high rate of study refusal. There was also a relatively high rate of couples who dropped from the ECG and SG conditions before the groups began. While couples’ completion of seven to eight groups was acceptable (71–79%), it was not as high as anticipated. Participants were significantly younger and diagnosed a shorter period of time than study refusers. In addition, participants who completed all study surveys were older and married longer than participants, and their spouse were also older. This attrition may have affected the study’s results. Overall, the relatively high rate of drop and refusal raises concern about the acceptability of a couple-focused group intervention model for women with early stage breast cancer. A second limitation regards our sample composition, which was comprised of primarily Caucasian, relatively well-educated, and primarily heterosexual couples. Our intervention may have had a different impact for less educated, minority, or same-sex couples. Third, due to the large number of analyses that would have been required, we did not assess possible moderators such as patient emotional expressivity or coping strategies (Manne et al., 2007a), partner characteristics (e.g., partner distress) , or medical characteristics (e.g., disease stage). Fourth, the study did not include a no-treatment control condition. Thus, it is impossible to discern whether reductions in distress and improvements in well-being over time shown would have been found whether or not we intervened with the couples. Fifth, because the majority of spouses were men and all patients were women, the findings confounded sex and role. Future research should examine treatment effects for these couple-focused group interventions among a patient population that is comprised of mixed sex (e.g., colorectal cancer). Finally, we did not control for multiple comparisons, which may have inflated the significant findings.
The results of this study suggest that different couple-focused group intervention approaches may be a better “fit” for certain types of patients and add to the growing literature that “one size fits all” is not the case for psychotherapy for cancer patients (Helgeson, Lepore & Eton, 2006; Manne et al., 2007b; Scheier et al., 2007). Patients exhibiting greater distress and relationship dissatisfaction may benefit from a group support therapy, while those patients exhibiting less distress in more satisfying relationships may benefit from a more structured skill-based couples group. Future research should evaluate potential psychological mechanisms for the intervention effects, particularly indicators of group therapy processes, and whether our intervention is efficacious among women with other types of cancer and women with more advanced stages of cancer. Future work should also consider focusing on distressed patients or partners and/or distressed relationships. We did not screen for distressed individuals or distressed relationship, and less than half of the patients and partners endorsed elevated depressive symptom scores. Our results may have differed if distress levels among all group members were higher.
Acknowledgments
This work was funded by grant CA 77857 from the National Cancer Institute. We would like to acknowledge the assistance of the research staff members including project coordinators Sara Frederick, Lauren Pidgeon, Tina Gajda, Kristen Sorice, and Devaney Camburn, as well as the research assistants Kristen Sorice, Jennifer Burden, Kathryn Volpicelli, Jennifer Iacovone, Emily Richards, Danielle Ryan, Joanna Crincoli, and George Olekson. We would also like to thank the oncologists who referred patients to this study, in particular Eric Miller and Generosa Grana, the couples’ group leaders, Shannon Myers, who provided supervision, and the study participants.
Footnotes
Random effect variance estimates and intraclass correlations are available from the authors. Across all variables there were significant correlations between the two partners’ intercepts or average outcomes as well as significant correlations between the partners’ residuals. There were no significant correlations between the partners’ slopes over time.
References
- Baucom DH, Porter LS, Kirby JS, Gremore TM, Wiesenthal N, Aldridge W, Keefe FJ. A couple-based intervention for female breast cancer. Psycho-Oncology. 2009;18:276–283. doi: 10.1002/pon.1395. [DOI] [PubMed] [Google Scholar]
- Baucom BR, Atkins DC, Rowe LS, Doss BD, Christensen A. Prediction of treatment response at 5-year follow-up in a randomized clinical trial of behaviorally based couple therapies. Journal of Consulting and Clinical Psychology. 2015;83:103–114. doi: 10.1037/a0038005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belcher A, Laurenceau J, Graber El, Cohen L, Dasch K, Siegel S. Daily Support in couples coping with early stage breast cancer: Maintaining Intimacy during Adversity. Health Psychology. 2011;30:665–673. doi: 10.1037/a0024705. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Nau S. Credibility of analogue therapy rationales. Journal of Behavior Therapy and Experimental Psychiatry. 1972;3:117–126. [Google Scholar]
- Boy AV. The therapist in person centered groups. Person Centered Review. 1990;5:308–315. [Google Scholar]
- Christensen DN. Post mastectomy couple counseling: An outcome study of a structured treatment protocol. Journal of Sex & Marital Therapy. 1983;9:266–275. doi: 10.1080/00926238308410913. [DOI] [PubMed] [Google Scholar]
- Christensen S, Zacharie R, Jensen A, Vieth M, Moller S, Ravnsbaek J, von der Maase H. Prevalence and risk of depressive symptoms 3 −4 months post-surgery in a nationwide cohort study of Danish women treate for early stage breast cancer. Breast Cancer Research and Therapy. 2009;113:339–355. doi: 10.1007/s10549-008-9920-9. [DOI] [PubMed] [Google Scholar]
- Day MA, Halpin J, Thorn BE. An empirical examination of the role of common factors of therapy during a mindfulness-based cognitive therapy intervention for headache pain. The Clinical Journal of Pain. 2015 doi: 10.1097/AJP.0000000000000277. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Deshields T, Tibbs T, Fan M, Taylor M. Differences in patterns of depression after treatment for breast cancer. Psychooncology. 2005;15:398–406. doi: 10.1002/pon.962. [DOI] [PubMed] [Google Scholar]
- Figueiredo MI, Fries E, Ingram KM. The role of disclosure patterns and unsupportive social interactions in the well-being of breast cancer patients. Psycho-Oncology. 2004;13:96–105. doi: 10.1002/pon.717. [DOI] [PubMed] [Google Scholar]
- Ganz P, Kawan I, Stanton A, Bower J, Belin T. Physical and psychosocial recovery in the year after primary treatment of breast cancer. Journal of Clinical Oncology. 2011;29:1101–9. doi: 10.1200/JCO.2010.28.8043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudenkauf LM, Antoni MH, Stagl JM, Lechner SC, Jutagir DR, Bouchard LC, Carver CS. Brief cognitive-behavioral and relaxation training interventions for breast cancer: A randomized controlled trial. Journal Consulting and Clinical Psychology. 2015;83:677–688. doi: 10.1037/ccp0000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison J, Maguire P, Pitceathly C. Confiding in crisis: gender differences in pattern of confiding among cancer patients. Social Science and Medicine. 1995;41:1255–1260. doi: 10.1016/0277-9536(94)00411-l. [DOI] [PubMed] [Google Scholar]
- Heinrichs N, Zimmermann T, Huber B, Herschbach P, Russell DW, Baucom DH. Cancer distress reduction with a couple-based skills training: a randomized controlled trial. Annals of Behavioral Medicine. 2012;43:239–252. doi: 10.1007/s12160-011-9314-9. [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Cohen S, Schulz R, Yasko J. Group support interventions for women with breast cancer: who benefits from what? Health Psychology. 2000;19:107–114. doi: 10.1037//0278-6133.19.2.107. [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Lepore SJ, Eton DT. Moderators of the benefits of psychoeducational interventions for men with prostate cancer. Health Psychology. 2006;25:348–354. doi: 10.1037/0278-6133.25.3.348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobbs N. Group-centered psychotherapy. In: Kemp CG, editor. Perspectives on the group process. Boston: Houghton Mifflin; 1964. pp. 156–161. [Google Scholar]
- Hopko DR, Clark CG, Cannity K, Bell JL. Pretreatment depression severity in breast cancer patients and its relation to treatment response to behavior therapy. Health Psychology. 2015 doi: 10.1037/hea0000252. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine. 1979;41:209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Horowitz MJ. Stress response syndromes and their treatment. In: Goldberger L, Breznitz S, editors. Handbook of stress: Theoretical and clinical aspects. New York: Free Press; 1982. pp. 711–732. [Google Scholar]
- Karakoyun-Celik O, Gorken I, Sahin S, Orcin E, Alanyali H, Kinay M. Depression and anxiety levels in wmen under folllow up for breast cancer: Relationship to coping with cancer and quality of life. Medical Oncology. 2010;27:108–113. doi: 10.1007/s12032-009-9181-4. [DOI] [PubMed] [Google Scholar]
- Kayser K, Fledman BN, Borselmann N, Daniels A. The effects of a randomized Couple based intervention on the quality of life of breast cancer patients and their partners. Journal of Social Work. 2010;34:20–32. [Google Scholar]
- Kawase E, Karasawa K, Shimotsu S, Izawa H, Hirowatari J, Saito A, Ito K, Horikawa N. Estimate of anxiety and depression in patients with early stage breast cancer. Breast Cancer. 2012;19:147–157. doi: 10.1007/s12282-010-0220-y. [DOI] [PubMed] [Google Scholar]
- Kissane D, Bloch S, Smith G, Miach P, Clarke D, Ikin J, Love A, Raniery N, McKenzie D. Cognitive Existential group psychotherapy from women with primary breast cancer: A randomized clinical trial. Psycho Oncology. 2003;12:532–546. doi: 10.1002/pon.683. [DOI] [PubMed] [Google Scholar]
- Lambert SD, McElduff P, Girgis A, Levesque JV, Regan TW, Turner J, Chong P. A pilot, multisite, randomized controlled trial of a self-directed coping skills training intervention for couples facing prostate cancer: accrual, retention, and data collection issues. Support Care Cancer. 2015 doi: 10.1007/s00520-015-2833-3. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Lauzier S, Maunsell E, Levesque P, Mondor M, Robert J, Robidoux A, Provencher L. Psychological distress and physical health in the year after diagnosis of DCIS or invasive breast cancer. Breast Cancer Research and Treatment. 2010;120:685–691. doi: 10.1007/s10549-009-0477-z. [DOI] [PubMed] [Google Scholar]
- Lewis FM, Cochrane BB, Fletcher KA, Zahlis EH, Shands ME, Gralow JR, Schmitz K. Helping Her Heal. Psycho-Oncology. 2008;17:131–137. doi: 10.1002/pon.1203. [DOI] [PubMed] [Google Scholar]
- Liu Y, Perez M, Schootman M, Aft R, Gillanders W, Jeffe D. Correlates of fear of cancer recurrence in women with ductal carcinoma in situ and early invasive breast cancer. Breast Cancer Research and Treatment. 2011;130:165–173. doi: 10.1007/s10549-011-1551-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luutonen S, Vahlberg T, Eloranta S, Hyvari H, Salminen E. Breast cancer patients receiving post-operative radiotherapy: Distress, depressive symptoms and unmet needs of psychosocial support. Radiotherapy and Oncology. 2011;100:299–303. doi: 10.1016/j.radonc.2011.01.014. [DOI] [PubMed] [Google Scholar]
- MacKenzie K. The clinical application of the group measure. In: Dies R, MacKensie K, editors. Advances in Group Psychotherapy. New York: International Universities Press; 1983. pp. 159–170. [Google Scholar]
- Manne S, Schnoll R. Measuring supportive and unsupportive responses during cancer treatment: a factor analytic assessment of the partner responses to cancer inventory. Journal of Behavioral Medicine. 2001;24:297–321. doi: 10.1023/a:1010667517519. [DOI] [PubMed] [Google Scholar]
- Manne SL, Ostroff JS, Winkel G, Fox K, Grana G, Miller E, Frazier T. Couple-focused group intervention for women with early stage breast cancer. Journal of Consulting and Clinical Psychology. 2005;73:634–646. doi: 10.1037/0022-006X.73.4.634. [DOI] [PubMed] [Google Scholar]
- Manne SL, Ostroff JS, Norton TR, Fox K, Goldstein L, Grana G. Cancer related relationship communication in couples coping with early stage breast cancer. Psycho-Oncology. 2006;15:234–247. doi: 10.1002/pon.941. [DOI] [PubMed] [Google Scholar]
- Manne SL, Norton TR, Ostroff JS, Winkel G, Fox K, Grana G. Protective buffering and psychological distress among couples coping with breast cancer: The moderating role of relationship satisfaction. Journal of Family Psychology. 2007a;21:380–388. doi: 10.1037/0893-3200.21.3.380. [DOI] [PubMed] [Google Scholar]
- Manne S, Rubin S, Edelson M, Rosenblum N, Bergman C, Hernandez E, Carlson J, Rocereto T, Winkel G. Coping and communication-enhancing intervention versus supportive counseling for women diagnosed with gynecological cancers. Journal of Consulting and Clinical Psychology. 2007b;75:615–628. doi: 10.1037/0022-006X.75.4.615. [DOI] [PubMed] [Google Scholar]
- Manne S, Badr H, Zaider T, Nelson C, Kissane D. Cancer-related communication, relationship intimacy, and psychological distress among couples coping with localized prostate cancer. Journal of Cancer Survivorship. 2010;4:74–85. doi: 10.1007/s11764-009-0109-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novalis P, Rojcewicz S, Peele R. Clinical manual of supportive therapy. Washington, D.C: American Association Press; 1993. [Google Scholar]
- Porter LS, Keefe FJ, Baucom DH, Hurwitz H, Moser B, Patterson E, Kim HJ. Partner-assisted emotional disclosure for patients with gastrointestinal cancer: results from a randomized controlled trial. Cancer. 2009;115:4326–4338. doi: 10.1002/cncr.24578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schag C, Heinrich R. CAncer Rehabilitation Evaluation System. Santa Monica, CA: Cares Consultants; 1988. [Google Scholar]
- Scheier MF, Helgeson VS, Schulz R, Colvin S, Berga SL, Knapp J, Gerszten K. Moderators of interventions designed to enhance physical and psychological functioning among younger women with early-stage breast cancer. Journal of Clinical Oncology and Research. 2007;25:5710–5714. doi: 10.1200/JCO.2007.11.7093. [DOI] [PubMed] [Google Scholar]
- Scott JL, Halford WK, Ward BG. United we stand? The effects of a couple coping intervention on adjustment to early stage breast or gynecological cancer. Journal of Consulting and Clinical Psychology. 2004;72:1122–1135. doi: 10.1037/0022-006X.72.6.1122. [DOI] [PubMed] [Google Scholar]
- So WKW, Marsh G, Ling WM, Leung FY, Lo JCK, Yeung M, Li GKH. Anxiety, depression and quality of life among Chinese breast cancer patients during adjuvant therapy. European Journal of Oncology Nursing. 2010;14(1):17–22. doi: 10.1016/j.ejon.2009.07.005. [DOI] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1975;38:15–28. [Google Scholar]
- Spiegel D, Classen C. Goals and Effect of Group Support. In: Spiegel D, Classen C, editors. Group therapy for cancer patients: A research-based handbook of psychosocial care. New York, NY: Basic Books; 2000. pp. 27–53. [Google Scholar]
- Spiegel D, Yalom I. A support group for dying patients. International Journal of Group Psychotherapy. 1978;28:233–245. doi: 10.1080/00207284.1978.11491609. [DOI] [PubMed] [Google Scholar]
- Reese JB, Porter LS, Regan KR, Keefe FJ, Azad NS, Diaz LA, Haythornthwaite JA. A randomized pilot trial of a telephone-based couples intervention for physical intimacy and sexual concerns in colorectal cancer. Psycho-Oncology. 2014;23:1005–1013. doi: 10.1002/pon.3508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahdaninia M, Omidvari S, Montazeri A. What predicts anxiety and depression in breast cancer patients: A follow-up study. Social Psychiatry and Epidemiology. 2010;45:355–361. doi: 10.1007/s00127-009-0068-7. [DOI] [PubMed] [Google Scholar]
- van Gestel Y, Voogd Q, Vingerhoets A, Mols F, Niewwenhuijzen G, van Driel O, van Berlo L, van de Poll-Franse L. A comparison of quality of life, disease impact and risk perception in women with invasive breast cancer and ductal carcinoma in situ. European Journal of Cancer. 2007;43:549–556. doi: 10.1016/j.ejca.2006.10.010. [DOI] [PubMed] [Google Scholar]
- Veit CT, Ware JE. The structure of psychological distress and well-being in general populations. Journal of Consulting and Clinical Psychology. 1983;51:730–742. doi: 10.1037//0022-006x.51.5.730. [DOI] [PubMed] [Google Scholar]
- Yalom I. Curative Factors – Overview. In: Yalom I, editor. The Theory and Practice of Group Psychotherapy. New York: Basic Books; 1975. pp. 70–104. [Google Scholar]
- Zimet Dahlem N, Zimet SG, Farley G. The multidimensional scale of perceived social support. Journal of Personality Assessment. 1988;52:30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- Zubrod C, Schneiderman M, Frei E, Brindley C, Gold GL, Shnider B, et al. Appraisal of methods for the study of chemotherapy of cancer in man: Comparative therapeutic trial of nitrogen mustard and triethylene thiophosphoramide. Journal of Chronic Disease. 1960;11:17–33. [Google Scholar]