Abstract
Background and Aims
Patients with complex colon polyps were traditionally referred for surgery to avoid adverse events associated with endoscopic resection. Recent advances in endoscopic imaging as well endoscopic hemostasis and clip closure allow for the use of endoscopic mucosal resection (EMR) as an alternative to surgery for such lesions. To determine the outcome of treatment of complex colon polyps with EMR as an alternative to surgery, we conducted a retrospective observational study.
Methods
Two hundred three patients with complex colon polyps referred to an EMR center as an alternative to surgery. Patients underwent a protocol driven EMR.. The primary endpoint was the complete resection rate. Secondary endpoints were safety, residual adenoma rate, and incidence of missed synchronous polyps.
Results
EMR was performed in 155 patients and was deferred in 48 patients who were referred to surgery. EMR specimens revealed benign polyps in 149 and cancer in 6 patients. EMR adverse events occurred in seven patients, requiring hospitalization in five of them. None of the patients died of their adverse events. Surveillance colonoscopy at 4-6 months after resection of a benign lesion in 137 patients revealed residual adenoma at the scar site in 6 patients and additional synchronous precancerous lesions in 117 patients that were not removed by the referring endoscopist. None underwent surgery for failure of EMR. The overall precancerous lesion burden was 2.83 per patient, the adenoma burden was 2.13 per patient, and the serrated polyp burden was 0.69 per patient.
Conclusions
EMR can be used instead of surgery for complex colon polyps in 75 percent of patients with few adverse events and few residual adenomas at resection sites. In addition, careful repeat examination of the entire colon for synchronous lesions overlooked by the referring endoscopist is required for the majority of patients.
INTRODUCTION
Endoscopists in community practice should be able to resect majority of pedunculated and sessile polyps less than 2 cm safely. 1 However, large polypoid or flat lesions (>2 cm), polyps located in near the appendicular orifice, ileocecal valve, dentate line or over a fold, and lesions that are tethered to the colon wall after prior incomplete resections, referred to as “complex colon polyps” are technically challenging for endoscopists in community practice to resect completely and safely.2, 3 These lesions carry an increased risk of colorectal cancer. In addition, fear of adverse events, high recurrence rates (approximately 10-20%) after piecemeal resection and the potential for medico-legal risk associated with interval cancers after incomplete resection frequently lead to referral for surgery.4-6 Although surgery prevents the risk of recurrence of these lesions, it exposes patients to substantial risks, including mortality and morbidity.7
Growing evidence of the relative efficacy, safety, as well cost-effectiveness of endoscopic resection of complex colon polyps when compared with surgery indicates a need for centers dedicated to caring for patients with such lesions.8 To that end, we created a dedicated colon EMR center in 2009, where all patients referred to this center undergo management using a standardized protocol (table 1). In the present study, our aim was to define the outcomes of patients with complex colon polyps referred to our EMR center and assess EMR according to the key performance indicators proposed by the British Society of Gastroenterology and Association of Coloprocotologists of Great Britain and Ireland.9
TABLE 1.
EMR protocol
|
Before the
procedure |
Clinic visit: evaluation and counseling for 1 hour in the clinic using figures and YouTube videos (https://www.youtube.com/user/GottumukkalaSRaju). |
| Preparation: split-dose polyethylene glycol-electrolyte solution. | |
| Procedure | Sedation: Conscious sedation/anesthesia. |
| Endoscope: Cap-fitted high definition colonoscope. | |
|
Submucosal injection: Saline with Indigo Carmine or methylene blue. | |
|
Resection:
A) Snare resection: en bloc resection ≤20 mm; piecemeal resection >20 mm; current setting: EndoCut Q 3-1-3. B) Cold biopsy avulsion of 2- to 3-mm residue at the edge that is not amenable to snare resection. C) Hot biopsy avulsion of residual polyp in the resection base not amenable to snare resection. | |
|
Confirmation of complete resection: Close-up photographs of the entire resection edge every 5 mm to confirm a round mucosal pit pattern and, thus, complete resection. | |
|
Argon plasma coagulation: Routine ablation of the edge. Settings: 0.8-L flow and 25-30 W; 0.8-L flow and 50-60 W for lesions with prior resections and tethering of the edges. All macroscopic disease removed prior to ablation with argon plasma coagulation. Repeat photo documentation of cleared resection edge. | |
|
Clip closure: Complete clip closure or clip closure of a deep resection with exposure of the muscularis propria in large lesions (>3-4 cm). Photo documentation: Multiple photos are taken to document every step of the procedure – lesion, injection, resection, ablation, clip closure. | |
| Recovery | Patients are discharged from the EMR center as soon as they meet the discharge criteria with instructions for diet, activity, medications, and follow-up. |
|
After the
procedure (0-5 days) |
Diet: Full liquid diet on days 0-2, low-residue diet on days 3 and 4, regular diet on day 5. E-mail reports: Patients instructed to e-mail their progress daily for the first 5 days. |
|
After the
procedure (10-14 days) |
Telephone call: Endoscopist checks for complications and reports pathology results to the patients. |
| Surveillance |
Six and 18 months after EMR: Colonoscopy to check for residual polyp at the scar site and clear the colon of any polyps missed by the referring endoscopist. Biopsy the scar for residual tumor in patients with nodular scar and submit in different jars for larger scars; biopsies are deferred in patients with smooth scars with round pit patterns and innominate grooves. |
METHODS
Patients
Prospectively collected data on all patients referred to the colon EMR center at The University of Texas MD Anderson Cancer Center from 2009 to 2014 were analyzed retrospectively. The MD Anderson Institutional Review Board approved the study. The data were derived from a retrospective study as well as a prospective one (ClinicalTrials.gov identifier: NCT01827241; initiated in April 2013).
Procedures
All patients underwent EMR under a standardized protocol by a single operator (Table 1). During surveillance colonoscopy to check the EMR scar site, we screened the entire colon for additional polyps as our policy was to resect the index lesion referred for EMR and retrieve the specimen without checking the colon for additional polyps.
Outcome measures
Endoscopic technical success of endoscopic resection was defined as the ability to resect a colon polyp completely using EMR. Adverse events were defined as those occurring during or after EMR that required hospitalization, repeat endoscopic intervention, transfusions, or surgery. A residual polyp was defined as a tumor at the EMR site documented via biopsy analysis during surveillance endoscopy. Missed polyps were defined as those away from the site of original resection that were removed during surveillance endoscopy after EMR.
Data collection and analysis
All patient data were collected from electronic medical records and endoscopy reports using a natural language processing tool developed in our EMR center. Variables collected included patient age, sex, race, and body mass index; EMR details; adverse events; colon polyp morphology, pathology, and recurrence; and referral for surgery.10 The data was collected using a detailed structured field format in an endoscopic reporting system (Endoworks; Olympus, Center Valley, Penn). Detailed photo documentation of each entire EMR was undertaken, with about 20-30 photos per resection. In addition, videos of all large EMRs (n=120) were recorded to review the procedures, and the majority of them were posted to YouTube on the EMR Channel (https://www.youtube.com/playlist?list=PL43D6FC92ECCD341E) to help educate endoscopists interested in learning about EMR. Surveillance endoscopy data were documented with extensive photography of each resection scar. Categorical variables were summarized by absolute frequency and percentage. Median values and range (minimum and maximum) were calculated for time variables. Two sample test of proportions was used to compare type and outcomes of resection for lesions grouped by size (<20mm or >20 mm). Analyses were performed in Stata 14.0 data analysis software (StataCorp, College Station, TX).
RESULTS
Patient demographics
Two hundred three patients with complex colon polyps were referred to our center for EMR as an alternative to surgery. The mean age of the patients was 64.02 years (range, 29-88 years), with an equal distribution of men (n=99) and women (n=104). The majority of the patients were white (n=162) and either overweight or obese (n=154).
The majority of the lesions were in the right colon (n=114) or transverse colon (n=46). Also, most of the lesions were large (>20 mm) in size, n=142; 10-20 mm, n=56 and nonpolypoid (n=161) (Table 2).
TABLE 2.
Demographics of the study patients with complex colon polyps referred for EMR
| Total number of patients referred | 203 |
| Mean age, y (range) | 64.02 (29-88) |
| Sex | |
| Male | 99 |
| Female | 104 |
| Race | |
| White | 162 |
| Black | 19 |
| Hispanic | 7 |
| Asian | 15 |
| Overweight/obese | 154 (76%) |
| Antithrombotic use | 86 (42%) |
| Aspirin | 59 |
| Clopidogrel | 10 |
| Warfarin (Coumadin) | 9 |
| Enoxaparin | 7 |
| Dabigatran | 1 |
EMR
Of the 203 patients referred to our center, 7 with large lesions (> 20 mm) had to have deferral of EMR after colonoscopy owing to obvious endoscopic features of frank malignancy, although their original biopsies performed by the referring endoscopist did not reveal cancer and the referring endoscopist did not suspect cancer. Based on the detailed narrow band imaging of the lesion, endoscopist suspected cancer and established the diagnosis of cancer via directed biopsy of the focus of cancer in the polyp demonstrating optical signs of cancer and subsequently referred these patients for surgery.
Of the 195 patients without endoscopic features of frank malignancy, 41 had to have deferral of EMR owing to technical difficulties in performing complete, safe resection as outlined in Table 3. Specifically, these problems were difficult endoscopic access to the lesion (n=16), failure to lift the lesion from extensive scarring related to prior endoscopic intervention (n=14), inability to completely and safely cut multiple or large polyps (n=9), and inability to identify a lesion referred for EMR (n=2). In the last group, one patient had a lesion not marked with a tattoo, whereas the other was reported as a 2-cm cecal lesion that was marked with a tattoo.
TABLE 3.
Location, size, and resectability of complex colon polyps in patients referred for EMR
| Size of colon polyp |
||||
|---|---|---|---|---|
| Characteristics | >20 mm (n=142) [70%] |
10-20 mm (n=56) [28%] |
<10mm (n=5) [2%] |
Total (n=203) |
|
Location of polyp
| ||||
| Appendix | 1 | 0 | 1 | 2 |
|
| ||||
| Cecum | 28 | 17 | 3 | 48 |
|
| ||||
| Ileocecal valve | 11 | 1 | 1 | 13 |
|
| ||||
| Ascending colon | 35 | 16 | 0 | 51 |
|
| ||||
| Hepatic flexure | 9 | 2 | 0 | 11 |
|
| ||||
| Transverse colon | 21 | 8 | 0 | 29 |
|
| ||||
| Splenic flexure | 4 | 2 | 0 | 6 |
|
| ||||
| Descending colon | 5 | 1 | 0 | 6 |
|
| ||||
| Sigmoid colon | 6 | 6 | 0 | 12 |
|
| ||||
| Rectosigmoid colon | 3 | 0 | 0 | 3 |
|
| ||||
| Rectum | 19 | 3 | 0 | 22 |
|
| ||||
| Successful resection | 99 (70%) |
52 (93%) |
4 (80%) |
155 (76%) |
|
| ||||
| En bloc resection | 28 | 36 | 3 | 67 |
|
| ||||
| Piecemeal resection | 71 | 16 | 1 | 88 |
|
| ||||
| Deferred resection | 43 (30%) |
4 (7%) |
1 (20%) |
48 (24%) |
|
| ||||
| Failure to identify lesion | 1* | 1** | 0 | 2 |
|
| ||||
| Obvious cancer | 7 | 0 | 0 | 7 |
|
| ||||
| Difficult-to-access lesion | 14 | 1 | 1 | 16 |
|
| ||||
| Difficult-to-lift lesion | 12 | 2 | 0 | 14 |
|
| ||||
| Large lesion | 7 | 0 | 0 | 7 |
|
| ||||
| Multiple polyps | 2 | 0 | 0 | 2 |
|
| ||||
|
Pathology of biopsy specimens prior
to referral |
||||
|
| ||||
| Benign | 142 | 56 | 5 | 203 |
|
| ||||
|
Pathology of endoscopic resected
specimens |
99 | 52 | 4 | 155 |
|
| ||||
| Benign | 94 | 51 | 4 | 149 |
|
| ||||
| Cancer | 5 | 1 | 0 | 6 |
Cecal polyp of 2 cm, biopsy (adenoma), and a tattoo was placed prior to referral: scar noted, no polyp on two examinations performed 6 months apart, and first examination done with a second senior endoscopist observing the procedure using white light, narrow band imaging, and dye spray chromoendoscopy.
Ascending colon lesion of 1-2 cm, original biopsies negative for adenoma, no tattoo was placed prior to referral: examined twice and no lesion was found even with chromoendoscopy; two 5-mm adenomas were removed, and at 1 year of follow-up, no lesion was found during follow-up except for a small adenoma.
Obvious cancer in the complex polyp missed by the referring gastroenterologist was more frequent in patients with > 20 mm lesions compared to those with < 20 mm lesions (8/142 vs 0/61 - 5.6% vs 0% p =0.06). In addition, failure to access the lesion (14/142 vs 2/61 - 9.8% vs 3.2%, p=0.11) and failure to lift the lesion after submucosal injection (11/142 vs 2/61 - 7.7% vs 3.2%, p=0.23) for resection were frequent in patients with >20 mm lesions compared to those with <20 mm lesions. There was a higher rate of successful resection for < 20 mm lesions than >20 mm lesions (91.8% vs. 69.7%, p<0.001) (figures 1-3).
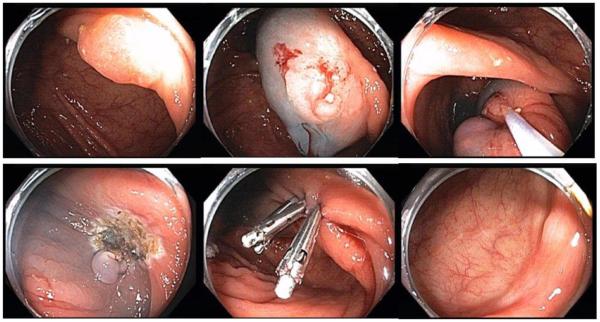
Figure 1.
EMR of a cecal lesion after two prior failed resections
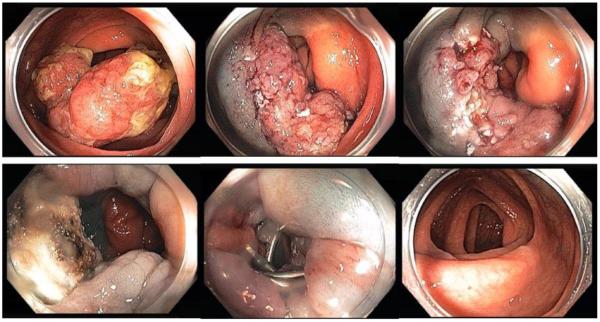
Figure 3.
EMR of a large ascending colon sessile lesion
EMR was successful in 155 patients (technical success rate of 76%). The resected polyp specimens were benign in 149 patients and cancer in 6 patients. Four of these six cancer patients who subsequently underwent surgery had a focus of a cancer in the piecemeal resected EMR specimens; surgical resected specimens revealed scar tissue with no cancer in the colon or regional lymph nodes.
The median duration of the EMR procedure was 56 min (range: 8-178 min), 51 min (12-91 min), and 42 min (range: 35-55 min) for > 20 mm, 10-20 mm, and < 10 mm lesions. The median number of clips utilized for closure was 6 (range: 2-14)
Adverse events
EMR adverse events occurred in seven patients (3%). Five patients presented with delayed bleeding more than 24 hours after EMR, requiring hospitalization, transfusions, and endoscopic therapy. The median duration of onset of adverse events was 6 days after EMR. One patient in whom a 3-mm perforation developed during EMR without any fluid escaping into the peritoneal cavity underwent immediate endoscopic closure followed by discharge from the endoscopy unit; re-examination 6 and 24 hours later did not demonstrate any signs of peritonitis, and the patient did well without hospitalization. One patient developed fever and left lower quadrant after biopsy of an appendicular lesion (which was not removed because it looked like cancer) that required antibiotics. None of the patients had to undergo emergency surgery during or after EMR. Furthermore, no procedure-related deaths occurred.
Residual tumor at the resection site
Of the 149 patients with a benign tumor who had undergone resection, 137 patients had surveillance colonoscopy 4-6 months after either en-bloc (n=59) or piecemeal resection (n-78). Twelve patients did not have an identifiable scar; 16 patients had a clean well-healed smooth scar with no visible tumor, and these patients did not undergo biopsy of the scar; and 109 patients underwent biopsies of the visible scar at the resection site. During first surveillance examination, six patients revealed residual adenoma at the resection scar site. Five of these patients were referred after prior failed resection (snare resections (n=1) or EMR (n=4); during second surveillance examination, three patients had small residual adenoma (< 5mm) that was treated with cold biopsy excision and ablation; one patient had no residual adenoma and one patient hasn't had second surveillance examination (Table 4). The residual adenomas were small and easily managed by endoscopy, without the need for surgery.
TABLE 4.
Outcome of surveillance in the study patients referred for colon EMR
| No. of patients |
||||
|---|---|---|---|---|
| Outcome of Resection |
Size of colon polyp |
|||
| >20 mm | 10-20 mm |
<10 mm | Total | |
|
Successful resection En-bloc EMR + Piecemeal EMR |
99 (28+71) |
52 (36+16) |
4 (3+1) |
155 (67+88) |
|
| ||||
| Short-term follow-up | 99 | 52 | 4 | 155 |
|
| ||||
| Complications (En-bloc EMR + Piecemeal EMR + incomplete resection or biopsy) |
6 (1+3+2) |
1 (0+1+0) |
0 (0+0+0) |
7 (1+4+2) |
|
| ||||
| Surgery for complications | 0 | 0 | 0 | 0 |
|
| ||||
|
Long-term follow-up
| ||||
| Resection site surveyed (En-bloc EMR + Piecemeal EMR) |
87 (26 +61) |
46 (30+16) |
4 (3+1) |
137 (59+78) |
|
| ||||
| Scars not seen (En-bloc EMR + Piecemeal EMR) |
3 (1+2) |
7 (5+2) |
2 (2+0) |
12 (8+4) |
|
| ||||
| Scar seen, biopsy done (En-bloc EMR + Piecemeal EMR) |
73 (21+52) |
34 (25+9) |
2 (1+1) |
109 (47+62) |
|
| ||||
| Scar seen, no biopsy | 11 (4+7) |
5 (4+1) |
0 (0+0) |
16 (8+8) |
|
| ||||
|
Residual adenoma (En-bloc EMR + Piecemeal EMR) |
3 (0+3) |
2 (1+1) |
1 (0+1) |
6 (1+5) |
|
| ||||
| Surgery for residual adenoma | 0 | 0 | 0 | 0 |
|
| ||||
| Rest of the colon surveyed | 87 | 46 | 4 | 137 |
|
| ||||
| No. of patients with additional adenomas/SSP |
71 (71%) |
42 (81%) |
4 (100%) |
117 (75%) |
|
| ||||
| Adenoma burden (no. of adenomas/patient) |
1.95 | 2.41 | 3.00 | 2.13 |
|
| ||||
| SSP burden (no. of SSPs/patient) | 0.57 | 0.93 | 0.50 | 0.69 |
|
| ||||
| Total adenoma + SSP burden | 2.50 | 3.34 | 3.50 | 2.83 |
SSP, sessile serrated polyp
Missed polyps
One hundred and thirty seven patients underwent surveillance colonoscopy at 4-6 months; 117 (85%) of these patients revealed additional precancerous lesions that were not removed by the referring endoscopist prior to referral. Forty-five patients had advanced adenomas. The overall precancerous lesion burden was 2.83 per patient, the adenoma burden was 2.13 per patient, and the serrated polyp burden was 0.69 per patient (Table 4).
Reasons for Surgery in Patients Referred for EMR
A. EMR Deferred Group (n=46)
In the obvious cancer group (n=7), surgery was deferred in two patients due to advanced age and multiple comorbid conditions; two patients underwent surgery at an outside facility; and the remaining three patients underwent surgery at our institution (T2N0M0 in 2 patients; and T1N0M0 in 1 patient).
In the difficult to access the lesion group (n=16), surgery was deferred in two patients due to advanced age and comorbid conditions; seven patients preferred to have surgery at an outside facility; and the remaining seven patients underwent right hemicolectomy at our institution (pathology: serrated adenoma (n=2), tubular adenoma (n=1), and tubulovillous adenoma (n=4).
In the difficult to lift lesion group (n=14), nine patients preferred to have surgery at an outside facility; and the remaining five patients underwent surgery (right hemicolectomy in 4 and left hemicolectomy in 1) at our institution (pathology: tubular adenoma (n=1).
In the large and multiple lesion group (n=9), three patients preferred to have surgery at an outside facility; and the remaining six patients underwent surgery (right hemicolectomy (n=5) and transanal excision (n=1) at our institution (pathology: tubular adenoma (n=1), tubulovillous adenoma (n=4), and villous adenoma (n=1).
B. EMR Successful Group
Six patients, who underwent successful piecemeal resection, revealed cancer in the resection specimens. Two patients decided to defer surgery and both were free from tumor recurrence on two surveillance examinations at 3-4 month and 14-16 month intervals. Remaining four patients underwent surgery, which revealed well-healed scars at the resection site without any evidence of tumor.
C. Complications of Surgery
Postoperative surgical complications occurred in six of 25 patients who underwent surgery at our facility (anastomotic leak (n=2); prolonged ileus (n=2); urinary retention (n=1); confusion and delirium (n=1)). There was no mortality related to surgery.
DISCUSSION
Our study demonstrated that EMR was effective in the management of more than 75% of patients with complex colon polyps with low rates of adverse events (4.5%) and residual tumors (4%). EMR was successful in the management of patients with ≤ 20 mm lesions as well as those with > 20 mm lesions (92% and 70% respectively). Although quality metrics for the management of large and complex colon polyps have yet to be finalized in the United States, our outcomes meet the key performance indicators proposed by the British Society of Gastroenterology and the Association of Coloprocotologists of Great Britain and Ireland.9
The rate of primary surgery for complex colon polyps varies based on the regional referral patterns and expertise of the center. The rate of primary surgery for large polyps in the Bowel Cancer Screening Program of England (2006-2009) ranged from 7% to 36%.11 Also, the rate of complete resection in that program varied from 78% to 100%, with the rate of persistence of adenoma at the resection site ranging from 6% to 18%.11-19 which supports referral of patients with complex colon polyps for primary endoscopic therapy instead of surgery. Referral to surgery for benign polyps >20 mm in size is dependent on the endoscopist and can vary from 0 to 46.6 % per endoscopist. 20 More than 75% of patients with complex colon polyps referred to our EMR center have undergone successful endoscopic resection of their polyps and thereby avoided surgery; about 24% referred to our center have had to undergo primary surgery. Luigiano et al reported similar outcomes, further substantiating the need for referral to an EMR center to avoid unnecessary surgery.21 None of the patients in this study had to have surgery for the management of adverse events or failure of endoscopic therapy resulting in local recurrence of tumor. Similar to the observations of Buchner et al,16 our study included patients with small polyps referred for EMR, with the majority of them referred because of tethering of the polyps after failed resections. As EMR expertise becomes more widespread, the patients referred to tertiary centers will be increasingly limited to those with more challenging anatomy.
Our study also revealed that 1 in 25 patients referred for EMR had frank cancer, highlighting the need for education of endoscopists referring patients for resection on optical diagnosis of cancer in a large polypoid and nonpolypoid lesions and for the use of one or two directed biopsies of the area haroboring the most advance pathology (cancer) in the polyp based on surface pit pattern (type V) instead of random biopsy analysis of a polyp to best characterize the lesion.22-25 This would minimize unnecessary procedures and cancer treatment delays and reduce costs.
In addition, this study sheds light the current practice of referring endoscopists when faced with a complex polyp. Extensive biopsies to sample multiple random areas of the polyp and snare resection to obtain a larger specimen to document the absence of cancer in the colon lesions as well as placement of tattoos at the lesion sites should be avoided because these measures cause severe fibrosis and can prevent successful removal of lesions as well as increase complication rate should EMR be attempted.26 Failure to lift the lesion accounted for 1 in 15 of all complex lesions referred to our center and as a reason for referral to surgery in over 25% of patients referred to our center for EMR.
Recent studies report 25%-32% residual adenoma or recurrence of tumor at the resection site. 12, 27 Although piecemeal resection of colorectal tumors is reported to be associated with a higher residual/recurrence rate than is en bloc resection (20% versus 3%),4, 28, 29 we observed a low residual colorectal tumor rate (4.4%) with EMR in the present study. This may have resulted from the use of a protocol of performing EMR in a clean colon (Boston Bowel Preparation Scale of 8 or 9) and drying up the colon segment to define the lesion better, routine use of a cap fitted colonoscope that facilitated better evaluation and resection of the entire lesion (even it extended over a fold), complete excision of the lesion to create a clean resection base and edges similar to the ones observed after endoscopic submucosal dissection, multiple photographs of the entire resection edge and base that permitted time for careful examination of the entire resection during the freeze mode before a picture was saved, and routine ablation of the edges with argon plasma coagulation.30, 31 The risk of residual adenoma is higher in those complex polyps ≤ 20 mm (8.3%) compared to those with >20 mm (4.1%). This could be due to referral of smaller tethered lesions after failed prior resections which are difficult to cut completely compared to complete resection of treatment naïve larger lesions. High recurrence rates (25%) observed in a recent Dutch study, where endoscopists with low-case volumes performed EMR, emphasize the importance of centralization.32 Because of significant risk of second (34%) and third (20%) recurrence after endoscopic resection of first recurrence in expert hands and the need for multiple procedures, it is best to defer incomplete resections of large and complex polyps and refer such patients s to an EMR center.33
The complication rate for EMR was low in our study (4.5%), although the majority of the lesions resected were located in the right colon and were large, carrying a high risk of adverse events.3, 34-37 In our center, based on our animal experimental work and clinical experience, our technique of deep submucosal approximation of resection defects with clips, enables us to discharge patients, even those who reside far from the EMR center, soon after they recover without the need for hospitalization or a visit to a short-term hospital unit for observation, thereby reducing the cost of their care. 38-40, 41 A recent randomized controlled study documented the benefits of clip closure after EMR.42 Although endoscopists have debated the benefit of using clips for this purpose, we believe that deep approximation of a wound using clips correctly reduces postpolypectomy bleeding and overall cost of care.18, 43-45 Additional factors that may contribute to the lower adverse event rates in our study include the use of a microprocessor-generated cut and dietary restrictions prescribed to patients to prevent detachment of eschars. These approaches should be investigated further. Daily progress reports e-mailed by the patients have enabled us to take care of patients with postpolypectomy bleeding without delay. None of the patients in the present study had to have surgery for management of adverse events, and none of them died.
A recent cost-effective analysis of endoscopic resection and surgical resection suggests that endoscopic resection is cost-effective for removal of complex colon polyps; the cost of endoscopic resection was $5,570/patient with 9.640 quality-adjusted life-years, while laparoscopic resection costs $18,717/patient with 9.577 quality-adjusted life-years.8 Our high technical success of complete resection and low adverse event rate confirms that this could be achieved in the United States.
Although it is clear that patients with complex and large polyps are at high risk for metachronous polyps as well as synchronous polyps in patients with flat adenomas,46-48 our study demonstrated the importance of repeat examination of the entire colon during surveillance examination of the EMR scar site at 6 months given a high percentage of patients (85%) with additional polyps that were not addressed by the referring endoscopist. Although the majority of referral EMR centers treat polyps and discharge patients to their referring physicians for follow-up, careful surveillance examination of the entire colon is important to identify cancer-related synchronous lesions.
Our study was limited in that a single operator performed it at a tertiary referral center. In addition, although this was a retrospective study, we used a structured format for data collection, all patients were closely followed for the first 5 days by electronic communication, and careful examination of the scar with a cap fitted colonoscope, along with a repeat screening of the entire colon for any missed polyps by an endoscopist experienced in high quality colon screening offers several insights on the management of these patient.
In summary, referral to an EMR center prevents surgery in three of four patients with complex colon lesions. The morbidity and mortality rates for colonoscopic resection for colon EMR are low, as is the residual polyp rate. Consideration of thorough examination of the entire colon during follow-up surveillance examination to remove any missed synchronous lesions is important.
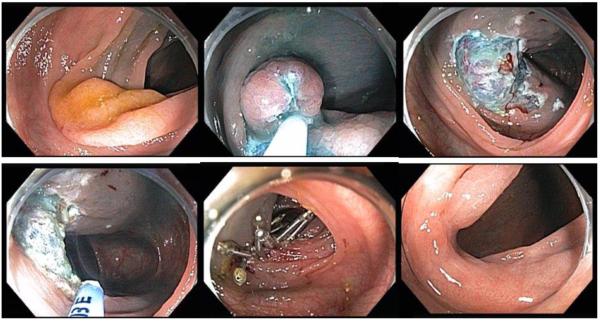
Figure 2.
EMR of an ascending colon flat lesion
Acknowledgements
The John Stroehlein Distinguished Professorship supported this work. We thank Mr. Donald Norwood for editing the final manuscript. Research support for this study from the National Institutes of Health/National Cancer Institute under award number P30CA016672 (and K07CA160753 to M. Pande).
Footnotes
DISCLOSURE: All authors disclosed no financial relationships relevant to this publication.
REFERENCES
- 1.Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Gastrointest Endosc. 2015;81:31–53. doi: 10.1016/j.gie.2014.07.058. [DOI] [PubMed] [Google Scholar]
- 2.Sanchez-Yague A, Kaltenbach T, Raju G, et al. Advanced endoscopic resection of colorectal lesions. Gastroenterol Clin North Am. 2013;42:459–77. doi: 10.1016/j.gtc.2013.05.012. [DOI] [PubMed] [Google Scholar]
- 3.Rutter MD, Nickerson C, Rees CJ, et al. Risk factors for adverse events related to polypectomy in the English Bowel Cancer Screening Programme. Endoscopy. 2014;46:90–7. doi: 10.1055/s-0033-1344987. [DOI] [PubMed] [Google Scholar]
- 4.Belderbos TD, Leenders M, Moons LM, et al. Local recurrence after endoscopic mucosal resection of nonpedunculated colorectal lesions: systematic review and meta-analysis. Endoscopy. 2014;46:388–402. doi: 10.1055/s-0034-1364970. [DOI] [PubMed] [Google Scholar]
- 5.Aziz Aadam A, Wani S, Kahi C, et al. Physician assessment and management of complex colon polyps: a multicenter video-based survey study. Am J Gastroenterol. 2014;109:1312–24. doi: 10.1038/ajg.2014.95. [DOI] [PubMed] [Google Scholar]
- 6.Rex DK, Bond JH, Feld AD. Medical-legal risks of incident cancers after clearing colonoscopy. Am J Gastroenterol. 2001;96:952–7. doi: 10.1111/j.1572-0241.2001.03677.x. [DOI] [PubMed] [Google Scholar]
- 7.Ahlenstiel G, Hourigan LF, Brown G, et al. Actual endoscopic versus predicted surgical mortality for treatment of advanced mucosal neoplasia of the colon. Gastrointest Endosc. 2014;80:668–76. doi: 10.1016/j.gie.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 8.Law RD, A., Gregory D, et al. Endoscopic Resection is Cost-effective Compared to Laparoscopic Resection in the Management of Complex Colon Polyps: An Economic Analysis. Gastrointest Endosc. 2016 doi: 10.1016/j.gie.2015.11.014. (in press) [DOI] [PubMed] [Google Scholar]
- 9.Rutter MD, Chattree A, Barbour JA, et al. British Society of Gastroenterology/Association of Coloproctologists of Great Britain and Ireland guidelines for the management of large non-pedunculated colorectal polyps. Gut. 2015;64:1847–73. doi: 10.1136/gutjnl-2015-309576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raju GS, Lum PJ, Slack RS, et al. Natural language processing as an alternative to manual reporting of colonoscopy quality metrics. Gastrointest Endosc. 2015;82:512–19. doi: 10.1016/j.gie.2015.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee TJ, Rees CJ, Nickerson C, et al. Management of complex colonic polyps in the English Bowel Cancer Screening Programme. Br J Surg. 2013;100:1633–9. doi: 10.1002/bjs.9282. [DOI] [PubMed] [Google Scholar]
- 12.Knabe M, Pohl J, Gerges C, et al. Standardized long-term follow-up after endoscopic resection of large, nonpedunculated colorectal lesions: a prospective two-center study. Am J Gastroenterol. 2014;109:183–9. doi: 10.1038/ajg.2013.419. [DOI] [PubMed] [Google Scholar]
- 13.Moss A, Bourke MJ, Williams SJ, et al. Endoscopic mucosal resection outcomes and prediction of submucosal cancer from advanced colonic mucosal neoplasia. Gastroenterology. 2011;140:1909–18. doi: 10.1053/j.gastro.2011.02.062. [DOI] [PubMed] [Google Scholar]
- 14.Moss A, Williams SJ, Hourigan LF, et al. Long-term adenoma recurrence following wide-field endoscopic mucosal resection (WF-EMR) for advanced colonic mucosal neoplasia is infrequent: results and risk factors in 1000 cases from the Australian Colonic EMR (ACE) study. Gut. 2015;64:57–65. doi: 10.1136/gutjnl-2013-305516. [DOI] [PubMed] [Google Scholar]
- 15.Binmoeller KF, Weilert F, Shah J, et al. "Underwater" EMR without submucosal injection for large sessile colorectal polyps (with video) Gastrointest Endosc. 2012;75:1086–91. doi: 10.1016/j.gie.2011.12.022. [DOI] [PubMed] [Google Scholar]
- 16.Buchner AM, Guarner-Argente C, Ginsberg GG. Outcomes of EMR of defiant colorectal lesions directed to an endoscopy referral center. Gastrointest Endosc. 2012;76:255–63. doi: 10.1016/j.gie.2012.02.060. [DOI] [PubMed] [Google Scholar]
- 17.Carvalho R, Areia M, Brito D, et al. Endoscopic mucosal resection of large colorectal polyps: prospective evaluation of recurrence and complications. Acta Gastroenterol Belg. 2013;76:225–30. [PubMed] [Google Scholar]
- 18.Liaquat H, Rohn E, Rex DK. Prophylactic clip closure reduced the risk of delayed postpolypectomy hemorrhage: experience in 277 clipped large sessile or flat colorectal lesions and 247 control lesions. Gastrointest Endosc. 2013;77:401–7. doi: 10.1016/j.gie.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 19.Repici A, Conio M, De Angelis C, et al. Insulated-tip knife endoscopic mucosal resection of large colorectal polyps unsuitable for standard polypectomy. Am J Gastroenterol. 2007;102:1617–23. doi: 10.1111/j.1572-0241.2007.01198.x. [DOI] [PubMed] [Google Scholar]
- 20.Le Roy F, Manfredi S, Hamonic S, et al. Frequency of and risk factors for the surgical resection of nonmalignant colorectal polyps: a population-based study. Endoscopy. 2016 doi: 10.1055/s-0034-1392976. (in press) [DOI] [PubMed] [Google Scholar]
- 21.Luigiano C, Iabichino G, Pagano N, et al. For "difficult" benign colorectal lesions referred to surgical resection a second opinion by an experienced endoscopist is mandatory: A single centre experience. World J Gastrointest Endosc. 2015;7:881–8. doi: 10.4253/wjge.v7.i9.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tanaka S, Nagata S, Oka S, et al. Determining depth of invasion by VN pit pattern analysis in submucosal colorectal carcinoma. Oncol Rep. 2002;9:1005–8. [PubMed] [Google Scholar]
- 23.Onishi T, Tamura S, Kuratani Y, et al. Evaluation of the depth score of type V pit patterns in crypt orifices of colorectal neoplastic lesions. J Gastroenterol. 2008;43:291–7. doi: 10.1007/s00535-008-2161-1. [DOI] [PubMed] [Google Scholar]
- 24.Hayashi N, Tanaka S, Hewett DG, et al. Endoscopic prediction of deep submucosal invasive carcinoma: validation of the narrow-band imaging international colorectal endoscopic (NICE) classification. Gastrointest Endosc. 2013;78:625–32. doi: 10.1016/j.gie.2013.04.185. [DOI] [PubMed] [Google Scholar]
- 25.Kobayashi Y, Kudo SE, Miyachi H, et al. Clinical usefulness of pit patterns for detecting colonic lesions requiring surgical treatment. Int J Colorectal Dis. 2011;26:1531–40. doi: 10.1007/s00384-011-1246-0. [DOI] [PubMed] [Google Scholar]
- 26.Han KS, Sohn DK. Biopsy and nonlifting sign in endoscopically resectable colorectal cancers. Gastrointest Endosc. 2008;68:615. doi: 10.1016/j.gie.2008.03.1120. [DOI] [PubMed] [Google Scholar]
- 27.Woodward T, Crook JE, Raimondo M, et al. Improving complete EMR of colorectal neoplasia: a randomized trial comparing snares and injectate in the resection of large sessile colon polyps. Gastrointest Endosc. 2015;81:673–81. doi: 10.1016/j.gie.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 28.Wang J, Zhang XH, Ge J, et al. Endoscopic submucosal dissection vs endoscopic mucosal resection for colorectal tumors: a meta-analysis. World J Gastroenterol. 2014;20:8282–7. doi: 10.3748/wjg.v20.i25.8282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Woodward TA, Heckman MG, Cleveland P, et al. Predictors of complete endoscopic mucosal resection of flat and depressed gastrointestinal neoplasia of the colon. Am J Gastroenterol. 2012;107:650–4. doi: 10.1038/ajg.2011.473. [DOI] [PubMed] [Google Scholar]
- 30.Tang SJ, Raju GS. Endoscopic Photography and Image Documentation (with videos) Gastrointest Endosc. 2015 doi: 10.1016/j.gie.2015.05.050. [DOI] [PubMed] [Google Scholar]
- 31.Anders M, Rosch T. Endoscopic mucosal resection of large colorectal adenomas: Only for expert centers? United European Gastroenterol J. 2015;3:171–3. doi: 10.1177/2050640615577535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barendse R, Musters G, Fockens P, et al. Endoscopic mucosal resection of large rectal adenomas in the era of centralization: Results of a multicenter collaboration. United European Gastroenterol J. 2014;2:497–504. doi: 10.1177/2050640614554218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kim HG, Sethi S, Banerjee S, et al. Outcomes of endoscopic treatment of second recurrences of large nonpedunculated colorectal adenomas. Surg Endosc. 2016 doi: 10.1007/s00464-015-4497-y. (in press) [DOI] [PubMed] [Google Scholar]
- 34.Choung BS, Kim SH, Ahn DS, et al. Incidence and risk factors of delayed postpolypectomy bleeding: a retrospective cohort study. J Clin Gastroenterol. 2014;48:784–9. doi: 10.1097/MCG.0000000000000027. [DOI] [PubMed] [Google Scholar]
- 35.Sawhney MS, Salfiti N, Nelson DB, et al. Risk factors for severe delayed postpolypectomy bleeding. Endoscopy. 2008;40:115–9. doi: 10.1055/s-2007-966959. [DOI] [PubMed] [Google Scholar]
- 36.Buddingh KT, Herngreen T, Haringsma J, et al. Location in the right hemi-colon is an independent risk factor for delayed post-polypectomy hemorrhage: a multi-center case-control study. Am J Gastroenterol. 2011;106:1119–24. doi: 10.1038/ajg.2010.507. [DOI] [PubMed] [Google Scholar]
- 37.Metz AJ, Bourke MJ, Moss A, et al. Factors that predict bleeding following endoscopic mucosal resection of large colonic lesions. Endoscopy. 2011;43:506–11. doi: 10.1055/s-0030-1256346. [DOI] [PubMed] [Google Scholar]
- 38.Raju GS, Ahmed I, Brining D, et al. Endoluminal closure of large perforations of colon with clips in a porcine model (with video) Gastrointest Endosc. 2006;64:640–6. doi: 10.1016/j.gie.2006.02.040. [DOI] [PubMed] [Google Scholar]
- 39.Raju GS, Saito Y, Matsuda T, et al. Endoscopic management of colonoscopic perforations (with videos) Gastrointest Endosc. 2011;74:1380–8. doi: 10.1016/j.gie.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 40.Raju GS, Kaltenbach T, Soetikno R. Endoscopic mechanical hemostasis of GI arterial bleeding (with videos) Gastrointest Endosc. 2007;66:774–85. doi: 10.1016/j.gie.2007.04.020. [DOI] [PubMed] [Google Scholar]
- 41.Parikh ND, Zanocco K, Keswani RN, et al. A cost-efficacy decision analysis of prophylactic clip placement after endoscopic removal of large polyps. Clin Gastroenterol Hepatol. 2013;11:1319–24. doi: 10.1016/j.cgh.2012.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang QS, Han B, Xu JH, et al. Clip closure of defect after endoscopic resection in patients with larger colorectal tumors decreased the adverse events. Gastrointest Endosc. 2015;82:904–9. doi: 10.1016/j.gie.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 43.Li LY, Liu QS, Li L, et al. A meta-analysis and systematic review of prophylactic endoscopic treatments for postpolypectomy bleeding. Int J Colorectal Dis. 2011;26:709–19. doi: 10.1007/s00384-011-1141-8. [DOI] [PubMed] [Google Scholar]
- 44.Tamai N, Matsuda K, Sumiyama K, et al. Prophylactic hemostasis for postpolypectomy mucosal defect using endoclip under infrared imaging endoscopy. Surg Technol Int. 2010;19:91–6. [PubMed] [Google Scholar]
- 45.Pohl H. Clipping after polyp resection: uncertainties of a randomized trial. Gastrointest Endosc. 2015;82:910–1. doi: 10.1016/j.gie.2015.06.035. [DOI] [PubMed] [Google Scholar]
- 46.Park SK, Kim JW, Park SH, et al. Risk of developing metachronous colon neoplasm after polypectomy: comparison of one-stage versus two-stage polypectomy. Surg Endosc. 2014;28:1634–40. doi: 10.1007/s00464-013-3363-z. [DOI] [PubMed] [Google Scholar]
- 47.Martinez ME, Baron JA, Lieberman DA, et al. A pooled analysis of advanced colorectal neoplasia diagnoses after colonoscopic polypectomy. Gastroenterology. 2009;136:832–41. doi: 10.1053/j.gastro.2008.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Naravadi V, Gupta N, Early D, et al. Prevalence of advanced histological features and synchronous neoplasia in patients with flat adenomas. Gastrointest Endosc. 2016 doi: 10.1016/j.gie.2015.08.040. (in press) [DOI] [PubMed] [Google Scholar]