Introduction
Growing evidence indicates that the nation is facing a shortage of cancer care providers needed to provide high quality cancer care. As the U.S. population ages, the treatment options for cancer expand, and cancer survival rates increase; therefore, the current oncology workforce is without proportionate replacement for expected attrition [1–3]. A nurse practitioner (NP) working within the specialty field of oncology (i.e., an oncology NP [ONP]) is expected to assume the role of cancer-care provider; however, he or she may enter the field with limited cancer experience and knowledge. Due to provider shortages, ONPs may be encouraged to assume an autonomous workload (i.e. working independently without supervision) without completing a formal orientation to cancer care that guarantees entry-level competency to cancer care practice.
NPs are traditionally educated to care for patients afflicted by a broad range of diseases and conditions—not patients with specific diseases [4]. Meanwhile, cancer care reaches across all patient populations, which renders the educational preparation of an NP, merely centered on a typical patient population program (i.e., family, adult, acute care, and women’s health), entirely inadequate for the care of the cancer patient and his or her family. Therefore, for ONPs educated in any of these patient population programs, additional education specific to the ONP role is necessary for the provision of safe and appropriate care of the cancer patient—and his or her family—throughout the trajectory of cancer care [5–9]. Currently, orientation models for NPs working in any form of specialty care are non-standardized and vary in format. For example, some standard orientation models may include on the job or learn as you go training, which likely is marked with high variability in content, quality, and motivation of the assigned preceptor. Another orientation model includes a basic introduction to cancer care with registered nurses, which is indeed useful, but not in itself sufficient for the complexity of the NP role. Still another model of orientation to oncology is a random mix of web-based and on-site courses. However, this model does not feature a scaffolded curriculum that begins with essential knowledge and then builds in complexity.
In addition, these different methods not only exhibit variable standards regarding curriculum quality and formal mentoring, but also lack consideration of the specific learning needs of the new NP. Unfortunately, ONPs need to learn the basics of staging and considerations of predicative and prognostic features of individual malignancies before treating new patients or patients who have progressed and require new treatment decisions. While physicians traditionally determine the cancer therapy used to treat a particular patient, the ONP still must be able to communicate meaningful patient assessments and treatment discussions. Nonetheless, limitations, such as a lack of motivated mentors, limited opportunities to practice the desired skill set, and a lack of orientation structure that is based on a specific curriculum and entry level competencies specific to oncology NPs may hinder the ONP’s transition to practice.
In response to these examples of inadequate and non-standardized orientation to the specialty role of ONP, a web-enhanced educational tool, funded through the National Cancer Institute, was developed for use in the United States: Oncology Nurse Practitioner Web Education Resource (ONc-PoWER). Web-enhanced education is one method that can provide specialized orientation education; moreover, it can deliver individualized, sequential learning that is specific to the ONP role. A web-enhanced orientation to oncology, combined with opportunities for local clinical application, is an ideal method for ensuring standard entry level competency content; moreover, it provides a realistic clinical orientation specific to the local cancer care practice culture [10]. This article describes the framework for the development and dissemination of ONc-PoWER.
ONc-PoWER began life as a set of asynchronous, web-enhanced lectures. Over time, the pedagogical design of ONc-PoWER was enhanced through a better understanding of adult learning theory and principles germane to effective online education. In its current form, ONc-PoWER first presents foundational material and then offers more complex material in a staged fashion. Moreover, the pedagogical enhancement resulted in the decision to abandon traditional PowerPoint presentation slides and create five interactive modules that feature lifelike characters in authentic clinical story settings. As a result, ONc-PoWER introduces learners to Gina, a recent NP graduate and new ONP who faces everyday challenges and tasks. Gina has the look and sound of a new ONP who is excited and nervous about her new position. In each module, Gina is assigned an onsite, clinical mentor, Sandra, who provides support, direction, and encouragement. It is through Sandra that ONc-PoWER helps the student “solve” Gina’s dilemmas as a new ONP by presenting relevant content that originally would have been introduced via traditional PowerPoint presentations. In this way, Gina is not simply given data on a new patient; she is required to solicit information from the patient through interactive questions and patient responses, which are modeled throughout the ONc-PoWER modules.
Factors and Information That Shape the ONP Curriculum
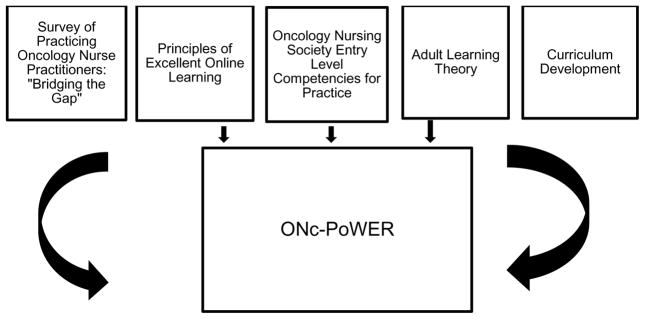
The development of ONc-PoWER was based upon (1) essential education for NPs new to cancer care, (2) adult learning theory, (3) Bloom’s Taxonomy), and (4) foundations of quality online education (see Figure 1).
Figure 1.
Factors and Information that Shaped ONc-PoWER Module Development
Essential Education
As the ONP role has grown, additional sources have guided the need, content, and delivery mode for courses designed for the ONP. Two of these sources include the Oncology Nursing Society’s (ONS) entry-level competencies [11] and a “Bridging the Gap” survey of working NPs in oncology [12]. In 2007, a national expert consensus panel convened through the ONS and not only created a set of entry level competencies for NPs entering oncology practice [11] but also conducted a national validation process from practicing oncology NPs and educators. These competencies were created using established national NP standards, through the consultation of the National Organization of Nurse Practitioner Faculties (NONPF) and the American Nurses Credentialing Center (ANCC). The ANCC templates for family, adult, women’s health and acute care NPs were used to develop the ONP entry-level competencies [11, 13].
In 2010, a working group of experienced NPs, established through the ONS, developed a cross sectional, descriptive study, which featured a 30-item electronic survey, to assess learning needs at entry into and through the first year of practice for ONPs. In the first year of practice, 90% of ONPs rated themselves as prepared or very prepared in standard NP competencies such as obtaining patient history, performing physical exams, and documenting findings. However, a majority of ONPs rated themselves as somewhat prepared or not at all prepared in the important clinical areas of chemotherapy/biotherapy competency (n = 81, 77.9%), recognizing and managing oncologic emergencies (n = 77, 70.2%), and recognition and management of drug toxicities (n = 63, 60.6%). The primary source of oncology education for ONPs new to practice was almost exclusively the collaborating/supervising physician (n = 84, 80.8%) [12]). Therefore, additional essential education beyond entry level competences for professional practice was clearly needed for ONPs. Hence, a curriculum crosswalk was conducted to ensure that the content of ONc-PoWER included all entry-level competencies.
The Adult Learner
Knowles’ Adult Learning Theory asserts that adults learn best when content can be made immediately relevant [14]. Once an adult learner accesses content and deems it relevant, the content then must make sense to the adult learner, and this can be accomplished by first providing the adult learner with essential information and then enabling him or her to apply the information in real-life scenarios [14]. For the ONP new to cancer care, even the routine daily clinical care of the patient and family with cancer and his or her family creates a learning need, and this need is met through the curriculum of the ONc-PoWER program. ONc-PoWER’s five modules introduce common patient scenarios that the ONP will certainly encounter: (1) the new patient visit, (2) presenting and documenting a patient visit, (3) the patient undergoing treatment, survivorship visits, and a potential oncologic emergency, (4) the patient requiring a transition to palliative and then hospice care, and (5) addressing self-care and career considerations. These scenarios and their related content were specifically developed based on the presumed educational needs of the new ONP, which is not included in a typical population-focused NP program. In this way, the content is more immediately relevant to the learner and more likely to be utilized and retained.
Bloom’s Taxonomy of Learning
According to Bloom’s taxonomy, to promote the process of learning, content should be arranged in order of increasing sophistication as part of a hierarchical learning objectives that progress from basic delivery/processing of information to higher-level educational competencies such as synthesis [15]. The ONc-PoWER curriculum advances from essential introductory cancer care information to a synthesis of related concepts and skills through a patient case study. For example, in Module 1 of ONc-PoWER, a new patient, Donald Cole, is recently diagnosed with colon cancer. The ONP is given information about staging and the use of national diagnostic and treatment guidelines such as the National Comprehensive Cancer Network (NCCN). Gina, the new ONP, is guided through the history and physical of this patient by her onsite clinical mentor Sandra, which introduces this information to the ONP student. The NCCN guidelines are linked in the curriculum (National Comprehensive Cancer Network)[16] so that the new ONP can use the guidelines as if Donald Cole were an actual patient. In Module 2, Gina is provided a typical pathology report and must analyze the information in order to present her findings to Sandra. Following this, Gina must apply and synthesize a variety of information as she prepares her written and oral summary of the patient. These activities in the modules are presented in a manner that is organized and sequential, building from basic skills and knowledge and extending through the application and evaluation of information that is embedded in individualized patient scenarios.
Web-Enhanced Principles
Any instructional strategy must be supported by sound educational principles that help to guide the teaching and learning process. The gold standard principles for quality education, which are widely adopted for undergraduate education, are also applicable to web-enhanced graduate educational programs. The Seven Principles for Good Practice in Undergraduate Education was developed in 1987 by Chickering and Gamson [17]. These principles are composed of the following:
Good practice encourages student-faculty contact;
Good practice encourages cooperation among students;
Good practice encourages active learning;
Good practice gives prompt feedback;
Good practice emphasizes time on task;
Good practice communicates high expectations;
Good practice respects diverse talents and ways of learning.
These standards must also be applied when creating programs that enhance all levels of NP practice—including specialized NPs such as ONPs. According to the 2013 Sloan Consortium, over 7 million students pursuing higher education are enrolled in at least one web-enhanced course [18]. Furthermore, according to Grade Change Tracking Online Education in the United States (2014) 33% of higher education students take at least one online course and graduate students are more inclined than undergraduate students to enroll in online courses [19]. This number is expected to grow because students find the flexibility a key determinant for enrollment [20]. Consequently, ONPs or any NPs new to a specialty role may be familiar with this teaching style and welcome the freedom they offer in comparison to the standard classroom format.
Creating quality web-enhanced educational materials requires more than simply uploading materials from a pre-existing face-to-face class onto a web-based course management system. In creating the content for any web-based program, a non-profit organization, Quality Matters, guides faculty and course developers to create high quality online courses. The organization emphasizes that course design must begin with a foundation of measurable competencies, essential outcomes, and evidence based practice [21]. Educational materials must not only actively engage and resonate with the learner, but also encourage him or her to seek mentorship and the support of his or her peers [22–23]. Best practices incorporate a variety of interactive strategies to accommodate the multiple learning styles, skills, and experiences of the adult learners [21, 24]. In addition, a well-designed online program must demand time on task and communicate high expectations for the learners. QM standards promote a variety of authentic assessment techniques, prompt feedback, and consistent faculty support to keep the learner motivated and engaged [21].
Although all seven of Chickering and Gamson’s principles were incorporated into ONc-PoWER, three of the principles (i.e., student-faculty interaction, active learning, and prompt feedback) figure the most prominently in the ONc-PoWER curriculum, as they highlight pedagogical strategies used to create ONc-PoWER modules. These strategies are not specific to the ONP, and they can easily be adapted to other NP continuing education courses that feature web-enhanced specialty content.
Student-Faculty Interaction
Maintaining student-faculty contact in a course is important because it not only provides a mechanism for students to assess their own learning, but also allows the instructor an opportunity to assess his or her teaching as well as the learning of his or her students. Encouraging this student-faculty interaction can be a challenge in a course featuring web-enhanced format because courses of this nature typically meet in real-time less frequently and feature less face-to-face interaction. Nonetheless, the learning/teaching management systems used in delivering web-enhanced courses (e.g., Blackboard or Moodle) do provide various mechanisms that promote frequent and convenient student-instructor contact such as discussion boards, wikis, or journals. For example, an exploratory study of 22 experienced nurse educators who taught web-enhanced courses with Blackboard or Moodle reported that purposeful reflection, which challenged students to ask “What next?” was a key component in maintaining student-faculty contact [25]. Another study of over 200 adult students enrolled in web-enhanced courses reported that students who perceived having high contact with their instructor also had higher learning and satisfaction scores with the course content and mode of delivery, and this contact was facilitated via discussion boards, wikis, and journals [26].
In creating ONc-PoWER, we integrated student-faculty interaction into the course design; however, we also recognized regional and local differences in the manner in which oncology is practiced as well as state-to-state differences in the scope of NP practice. To provide local application of content, each learner was asked to identify a local preceptor (i.e., an MD, NP, or physician assistant) willing to serve as his or her mentor. Announcements posted on the Blackboard course management system and emails sent to students and mentors were utilized to provide guidance, structure and orientation to the course. ONc-PoWER modules were also provided to the mentor in advance, which provided suggestions about how to apply the material in clinical practice. For example, as the ONP is working through the content on palliative care, the mentor received an email informing him or her that (1) his or her ONP is learning didactic content about palliative care and (2) it would be an appropriate time to introduce his or her ONP to the palliative care resources available at his or her particular oncology site. The web-enhanced material and emails provide a consistent structure, which allows for not only the delivery of standardized oncology knowledge, but also the appropriate application of this knowledge in the local clinical context through the student-mentor contact integrated into the ONc-PoWER curriculum. Currently, ONc-PoWER allows for the individualization of messages to the mentor from the instructor. Future iterations of ONc-PoWER will facilitate the delivery of electronic messages from the mentor to the ONP that can direct further learning opportunities.
Active Learning
Active learning, as the name suggests, is a process whereby learners are actively engaged in the learning process, rather than passively absorbing knowledge. Web-enhanced learning, such as that featured in ONc-PoWER, aligns with Knowles’ adult learning theory and places more responsibility about learning on the learner [27]. Active learning has been cited as a strategy that promotes critical thinking [28]. Consequently, creating effective active learning strategies, particularly through characters like Gina and Sandra who face those same clinical decisions, supports good web-enhanced teaching practice. For example, NP students have been found to prefer case studies and cooperative learning as active learning teaching strategies that promote critical thinking [29]. Nonetheless, planning commensurate learning activities requires more attention to detail prior to course delivery and includes—but is not limited to—a consideration of guidelines, mode(s) of delivery, and student expectations. Additionally, feedback to students must occur beginning with the onset of any teaching/learning session. Although this routinely occurs in most face-to-face courses, in a web-enhanced course, it is difficult for both faculty and students to experience the nonverbal communication exchanges that can signify understanding or lack of understanding of course content.
Consistent with these studies, ONc-PoWER guidelines emphasize active learning and instant feedback. All content presented in ONc-PoWER is reinforced through interactive activities. For example, in the ONc-PoWER modules, the learner is asked to utilize various embedded resources, respond to questions, and/or complete activities. In the ONc-PoWER module, the learner is presented content with embedded challenges related to (1) a new patient, (2) ongoing oncology care strategies, (3) a potential oncologic emergency or oncology self-care, and (4) professional development. This content is presented by way of PowerPoint presentations, videos, links to relevant web pages, and interactive learning activities (e.g., discussion board posts, self-check questions, and response tree). The ONP responds to the content and activities that represent real-life clinical situations. For example, in the follow-up patient module, the learner first must access national guidelines regarding the appropriative follow-up care for a specific malignancy and then respond appropriately to a long- term survivor still requesting frequent oncology follow-up because of concerns regarding possible recurrence. All feedback to the learner is delivered in a positive manner (e.g., “this response could be better by adding an empathic statement”). Furthermore, incorrect responses prompt the learner to review previous presented content. In contrast to a stagnant, teacher-centered didactic lecture, ONc-PoWER presents challenges immediately after each presentation.
Conclusion
The ONc-PoWER curriculum was created in response to the needs of quality web-enhanced learning in nursing in consultation with a variety of resources: ONS competencies for entry to advanced practice in oncology nursing, a survey of recalled learning needs on entry to practice from ONPs, the principles of adult learning, the principles of stepped curriculum development, and the standards of excellence in web-enhanced education. Evaluation of the curriculum by new ONPs and their onsite mentors is currently occurring. ONc-PoWER, as a web-enhanced method of curriculum development and dissemination, can also serve community focused primary care NPs in meeting the needs of patients and families for cancer screening, cancer diagnosis, cancer survivorship, and, when necessary, end-of-life care.
Acknowledgments
This project was supported by the National Cancer Education Grants Program (R25 CA148050-04).
Footnotes
The authors declare no conflicts of interest.
References
- 1.Erikson C, Salsberg E, Gaetano F, Bruinooge S, Goldstein M. Future supply and demand for oncologists: Challenges to assuring access to oncology services. Journal of Oncology Practice. 2007;2(3):79. doi: 10.1200/JOP.0723601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Warren J, Mariotto A, Meekins A, Topor M, Brown M. Current and future utilization of services from medical oncologists. Journal of Clinical Oncology. 2008;26(19):3242–3247. doi: 10.1200/JCO.2007.14.6357. [DOI] [PubMed] [Google Scholar]
- 3.IOM (Institute of Medicine) Ensuring Quality Cancer Care through the Oncology Workforce: Sustaining research and care in the 21st century: Workshop summary. Washington, DC: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 4.Kinney A, Hawkins R, Hudman K. A descriptive study of the role of the oncology nurse practitioner. Oncology Nursing Forum. 1997;24(1):811–820. [PubMed] [Google Scholar]
- 5.Rudy EB, Davidson LJ, Daly BJ, Clochesy JM, Sereika S, Baldisseri M, Hravnak M, Ross T, Ryan C. Care activities and outcomes of patients cared for by acute care nurse practitioners, physician assistants: A comparison. American Journal of Critical Care. 1998;7(4):267–281. [PubMed] [Google Scholar]
- 6.Kleinpell R, Hravnak M. Strategies for Success in the Acute Care Nurse Practitioner Role. Critical Care Nursing Clinics of North America. 2005;17(1):177–181. doi: 10.1016/j.ccell.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 7.Hravnak M, Tuite P, Baldisseri M. Expanding acute care nurse practitioner and clinical nurse specialist education: Invasive procedure training and human simulation in critical care. AACN Clinical Issues. 2005;16(1):89–100. doi: 10.1097/00044067-200501000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Melander S, Kleinpell R, Hravnak M, King J, Miller K. Post-masters certification programs for nurse practitioners: Population specialty role preparation. Journal of the American Academy of Nurse Practitioners. 2008;20:63–68. doi: 10.1111/j.1745-7599.2007.00293.x. [DOI] [PubMed] [Google Scholar]
- 9.Kleinpell R, Hravnak M, Settles J, Melander S. Making the web work for acute care NP education. Nurse Practitioner. 2009;34(4):8–10. doi: 10.1097/01.NPR.0000348314.07871.7b. [DOI] [PubMed] [Google Scholar]
- 10.LeFlore J, Thomas PE, Ziekle MA, Buus-Frank ME, et al. Educating neonatal nurse practitioners for the 21st century. Journal of Perinatal Nurse Nursing. 2011;25(2):200–205. doi: 10.1097/JPN.0b013e318218137a. [DOI] [PubMed] [Google Scholar]
- 11.Oncology Nurse Society. Oncology Nurse Practitioner Competencies. 2007 https://www.ons.org/sites/default/files/npcompentencies.pdf.
- 12.Rosenzweig M, Giblin J, Mickle M, et al. the Bridging the Gap Working Group. Bridging the gap: A descriptive study of knowledge and skill needs in the first year of oncology nurse practitioner practice. Oncology Nursing Forum. 2012;39(2):195–201. doi: 10.1188/12.ONF.195-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Population-focused Nurse Practitioner Competencies. 2013 http://c.ymcdn.com/sites/www.nonpf.org/resource/resmgr/competencies/populationfocusnpcomps2013.pdf.
- 14.Knowles M. Andragogy in Action. San Francisco: Jossey-Bass; 1984. [Google Scholar]
- 15.Bloom BS. Taxonomy of Educational Objectives: The Classification of Educational. Goals. New York: Longmas; 1964. [Google Scholar]
- 16.National Comprehensive Cancer Network. 2015 http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
- 17.Chickering A, Gamson Z. Faculty Inventory. Racine: Johnson Foundation; 1987. Seven Principles of Good Practice in Undergraduate Education. [Google Scholar]
- 18.Online Learning Consortium. 2013 http://onlinelearningconsortium.org/join/national-distance-learning-week-2015.
- 19.Allen IE, Seaman J. Grade Change: Tracking Online Education in the United States. Babson Survey Research Group and Quahog Research Group, LLC; 2014. http://www.onlinelearningsurvey.com/reports/gradechange.pdf. [Google Scholar]
- 20.US Department of Education. Web Tables: Enrollment in Distance Education Courses, by State: Fall 2012. 2014 http://nces.ed.gov/pubs2014/2014023.pdf.
- 21.QM: Quality Matters. 2014 https://www.qualitymatters.org.
- 22.Lockyer Lori, et al. Online mentoring and peer support: using learning technologies to facilitate entry into a community of practice. Research in Learning Technology [Sl] 10(1) http://dx.doi.org/10.3402/rlt.v10i1.11298. [Google Scholar]
- 23.Ge X, Planas LG, Er N. A Cognitive Support System to Scaffold Students’ Problem-based Learning in a Web-based Learning Environment. Interdisciplinary Journal of Problem-Based Learning. 2010;4(1) http://dx.doi.org/10.7771/1541-5015.1093. [Google Scholar]
- 24.Voelkel S. Combining the formative with the summative: the development of a two stage online test to encourage engagement and provide personal feedback in large classes. Research in Learning Technology, [Sl] 2013 Apr;21 http://dx.doi.org/10.3402/rlt.v21i0.19153. [Google Scholar]
- 25.Bonnell W, Boehm H. Improving feedback to students online. Teaching tips from experienced faculty. Journal of Continuing Education. 2011;42(11):503–509. doi: 10.3928/00220124-20110715-02. [DOI] [PubMed] [Google Scholar]
- 26.Richardson J, Swan K. Examining social presence in online courses in relation to student’s perceived learning and satisfaction. Online Learning Consortium formerly the Journal of Asynchronous Learning Networks. 2003;7(1) http://itecideas.pbworks.com/f/v7n1_richardson.pdf. [Google Scholar]
- 27.Andrew Koch J, Salamonson S, Everett YB, et al. Nursing students’ perception of a web-based intervention to support learning. Nurse Education Today. 2010;30(6):584–590. doi: 10.1016/j.nedt.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 28.Nelson LP. Do active-learning strategies improve students’ critical thinking? Higher Education Studies. 2014;4(2):77. [Google Scholar]
- 29.Youngblood N, Beitz JM. Developing critical thinking with active learning strategies. Nurse Educator. 2001;26(1):39–42. doi: 10.1097/00006223-200101000-00016. [DOI] [PubMed] [Google Scholar]