Abstract
Background and Objectives:
Laparoscopic inguinal hernia repair has become increasingly popular as an alternative to open surgery. The purpose of this study was to evaluate the safety and effectiveness of the laparoscopic total extraperitoneal procedure with the use of staple fixation and polypropylene mesh.
Methods:
A retrospective chart review examined outcomes of 1240 laparoscopic hernia operations in 783 patients, focusing on intraoperative and early postoperative complications, pain, and time until return to work and normal physical activities.
Results:
There were no intraoperative complications in this series; 106 patients experienced early postoperative complications across 8 evaluated categories: urinary retention (4.1%), seroma (3.0%), testicular/hemiscrotal swelling (1.9%), testicular atrophy (0%), hydrocele (0.6%), mesh infection (0.1%), and neurological symptoms (transient, 1.0%; persistent, 0.2%). Patients used an average of 5.6 Percocet pills after the procedure, and mean times until return to work and normal activities, including their routine exercise regimen, were 3.0 and 3.8 days, respectively.
Conclusion:
Complication rates and convalescence times were considered equivalent or superior to those found in other studies assessing both laparoscopic and open techniques. The usage of multiple Endostaples did not result in increased neurologic complications in the early postoperative period when compared with findings in the literature. In the hands of an experienced surgeon, total extraperitoneal repair is a safe, effective alternative to open inguinal hernia repair.
Keywords: Inguinal hernia, Laparoscopic, Staple fixation, TEP
INTRODUCTION
Inguinal hernia repair is one of the most commonly performed surgical procedures in the world, with an estimated 800,000 cases per year in the United States alone, and >20 million procedures across the globe annually.1,2 The most common technique for inguinal hernia repair was originally an open, tissue–based suture repair, which eventually evolved to commonly use prosthetics (with various fixation devices of sutures, staples, tacks, and glue) for a tension-free repair with a significantly lower recurrence rate2,3 and lower chronic pain after surgery.4 Laparoscopic repair of the inguinal hernia is becoming an increasingly popular method of herniorrhaphy, with a range of 16.8–41.0% of such operations in the United States (varying with the region and the characteristics of the hernias).5,6
Literature has shown the benefits of laparoscopy (when compared to open repair) to be mostly related to the more minimally invasive nature of the surgery, with lower wound infection rates, faster recovery times, and less postoperative pain.4,7–8 Higher risk of serious intraoperative complications and a sizeable learning curve to master the technique have been identified as negatives to a laparoscopic repair.4,8–11 The 2 most common variations of laparoscopic technique for inguinal hernia repair are the transabdominal preperitoneal (TAPP) repair and the total extraperitoneal (TEP) repair. Studies comparing the 2 techniques have not been collectively conclusive about whether one of them is superior, and there is evidence that both are safe, effective treatments of inguinal hernia.12–16
A review of the literature on inguinal hernia repair elicits a wide variety of experiences, with various combinations of repair type, specific technique, mesh usage, and fixation method, with, of course, different patient populations and different surgeon experience levels. It can be difficult to reach consensus on what the “best” option is in any of these categories for a particular situation, when randomized prospective trials often produce conflicting results. However, large case series' of physicians who have had success with specific combinations of technique, certain meshes, and fixation methods can be helpful in contributing to the knowledge base of how to best use the available materials and surgical strategies to optimize patient outcomes. The purpose of this study was to provide a review of the techniques and results experienced by a single surgeon in a series of 1240 TEP procedures using Endostaples™ (Covidien, Mansfield, Massachusetts, USA) and polypropylene mesh, with a focus on early complications and recovery metrics. This review series evaluates the TEP inguinal hernia repair method, with a description of specific surgical technique, and evaluation of primary outcome of the complication rate, as well as secondary outcomes of recovery metrics and analysis of factors that may be related to complications or more difficult recoveries.
METHODS
Study Design
A retrospective review and analysis examined 1240 cases involving hernia repair via laparoscopy (specifically TEP), performed by a single surgeon, between January 1995 and December 2014 at a major metropolitan academic medical center. The center's Institutional Review Board approved the study, with no specific consents required due to the retrospective, minimal risk nature of the study.
Patients
All participants were hernia patients of 1 surgeon who were surgically treated electively with a TEP repair for a unilateral or bilateral hernia defect, either primary or recurrent (with the exception of 7 patients whose TEP operation was converted to a TAPP approach). A total of 783 patients were operated on for 1240 procedures, where bilateral repair was counted as two separate surgical procedures. There were 722 males (92.2%) and 61 females (7.8%) operated on during this period. The mean age of the patients was 52.4 years (range, 18–92) (Table 1).
Table 1.
Demographics
| Variable | Data |
|---|---|
| Patients, n | 783 |
| Procedures/hernias, n | 1240 |
| Age, y (SD) | 52.4 (14.1) |
| Gender, n (%) | |
| Male | 722 (92.2) |
| Female | 61 (7.8) |
| Hernia laterality, n (%) | |
| Bilateral | 457 (58.4) |
| Unilateral | 326 (41.6) |
| Recurrent hernia, n (%) | 117 (9.4) |
All patients over 18 years were placed in the study, including patients who had concomitant procedures at the time of the inguinal hernia repair. There were 7 cases in which a TEP repair was attempted but then converted to a TAPP approach, because the extraperitoneal space had previously been breached by either pelvic surgery with a lower midline incision or a TEP repair. These patients were included in this analysis, as they were part of the intent-to-treat cohort. Excluded from the study were patients who had concomitant laparoscopic incisional or umbilical hernia repairs with mesh greater than 64 cm2, because it was felt that this would have an impact on analyzing pain and recovery metrics. In addition, any incarcerated hernia that could not be reduced before induction of anesthesia was repaired with a TAPP approach to ensure there was no compromised/ischemic bowel, and these patients were not included in the study. Of the patients who met the exclusion criteria, none had recurrences or any complications (intraoperative or early postoperative).
Setting
One surgeon, a Professor of Surgery at the Icahn School of Medicine, performed all operations at the Mount Sinai Medical Center, a major tertiary academic institution located in New York City. Selection of participants was based on a medical chart review, where almost all patients operated on with TEP during the stated period were included. Minors and patients having concomitant ventral hernia repair with mesh size >64 cm2 were excluded. All procedures performed were on an outpatient basis, with no hospital admissions necessary. No direct contact with patients, beyond normal follow-up, was needed after surgery to complete the study. The chart review took place at the hospital as well as the physician's office.
Surgical Technique
All procedures are completed with patients under general anesthesia and supine, with a Foley catheter placed. The patient is given 1 dose of preoperative antibiotics, either Kefzol or, if they are allergic, Vancomycin. An infraumbilical incision of 1–1.5 cm is made; 0-vicryl stay sutures are placed in the fascia, the first in the midline and the second just off midline on the side opposite of the hernia if unilateral, or on the side of the smaller hernia if bilateral. If there are bilateral defects, the larger side is always repaired first.
The fascia is opened vertically just off the midline; care is taken to not breach the peritoneal cavity. A finger dissection is then performed, aimed first toward the pubis in the midline and then swept to the right and left, not going above the level of the anterior superior iliac spine. This dissection is performed by elevating the abdominal wall with the dissecting finger, so that it all occurs above the ileopubic tract. An AutoSuture 10 mm balloon dissector (Covidien, Mansfield, Massachusetts, USA) is then placed and aimed toward the pubis with the abdominal wall elevated by the surgeon's other hand. The balloon is placed toward the pubis until bone is felt by the stylette of the trocar. Under direct vision with a 30° scope, the balloon is inflated to a maximum of 15 puffs.
The balloon is then deflated and a Hassan trocar placed. A 5-mm short trocar is inserted at ∼4 cm above the pubis and a 10-mm trocar is placed ∼3 to 4 cm above that. These placements depend on the distance between the umbilicus and pubis, and can be quite variable. Blunt dissection starts at the midline with a sweeping motion from side to side. If there is a direct component it is reduced at this time. The surgeon also dissects across the midline to the opposite side of the repair at least halfway to the epigastric vessels. The blunt dissection is then continued laterally from the epigastric vessels to the level of the anterior superior iliac spine; blunt abdominal wall trauma is avoided. The vas deferens and testicular vessels are then elevated, and the indirect sac is reduced high enough so that it can be held down on the posterior flap of the mesh at the conclusion of the procedure. If the patient has a significant cord lipoma, it is also reduced at this time. A piece of Ethicon Prolene mesh (polypropylene) is then cut to a size of 6 in. by 5.5–6 in., folded in half along the 6-in. length, and split from the top down, slightly more than halfway. An absorbable suture is placed to hold the split edges of the mesh together, and the mesh is then rolled into a cigarette shape and placed in the 10-mm trocar. This maneuver is always aimed just below and inferior to the anterior superior iliac spine and above the ileopubic tract, to avoid an iliac vessel injury. The mesh is then placed under the testicular vessels and vas deferens, the holding suture is cut, and the lateral portion of the mesh is then uncurled and laid flat. The Ethicon EMS stapler is used to affix the mesh, with the note that under no circumstances are staples placed below the ileopubic tract lateral to the internal ring. A minimum of 10 staples are used per patient for fixation. The direct space is then approached by uncurling this segment and stapling it high on the transversalis fascia, well above the defect site and to Cooper's ligament and past the midline to the opposite side. A neointernal ring is created by stapling the meshes together, with care being taken not to injure the epigastric vessels. A similar technique is performed on the opposite side if warranted. The retroperitoneum is then deflated, a 30-second pause is taken, and reinsufflation is performed to make certain there is no bleeding. If present, the indirect sacs are placed on top of the mesh, and the mesh is held down while the retroperitoneal gas is evacuated. If the patient has an umbilical defect it is always repaired at the completion of the inguinal repair procedure.
Follow-up
After surgery, all studied patients were given postoperative instructions that included the use of a stationary bicycle/treadmill/elliptical, hyperextension/stretching exercises, and pain management (prescription of 40 pills of Percocet 10/325, 1–2 by mouth every 4 hours as needed, or Tylenol). The only limitations on activity were during the first 48 h, during which the patients were instructed to do no strenuous core exercises, driving, or lifting of more than 15 pounds. After the first 2 postoperative days, the patients were instructed and encouraged to return to full, unrestricted activity and work.
Patients came to the office for follow-up at 1 week, 5–7 weeks, and 5–6 months after surgery, to assess postoperative condition and time until return to work, resumption of activities of daily living (ADL), and any complications. Some patients returned to the office outside of the usual last visit. These patients were evaluated for significance to the study, although most came for non–hernia-related problems.
Data Analysis
The authors performed a medical chart review, examining the medical records of all patients for demographic information (age, sex, hernia type and size, hernia location, primary versus recurrent), operative information (technique used, complications, simultaneous procedures) and postoperative data (return to work/ADL, analgesia required, complications). The recurrence rate was noted for completeness of the clinical picture, but was not the focus of the study because of the short follow-up period. SPSS ver. 20 was used to assess any significant differences in recovery metrics, hernia presentation, and complication rates across the categories of variables collected. Independent t test or Mann-Whitney U test, Pearson's or Spearman's correlation, chi-square or Fisher's exact test, Cochran-Armitage Trend Test (SAS ver. 9.3 used for this test), and Univariate ANOVA or Kruskal-Wallis test (with post hoc pairwise comparisons) were used where appropriate for statistical assessment. A cutoff of P < .05 was used for significance.
RESULTS
Presentation
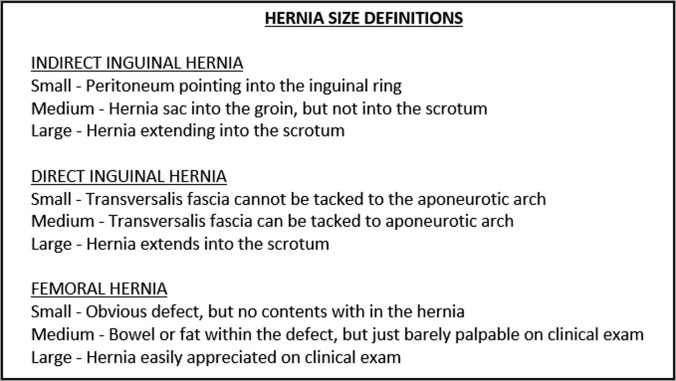
Patient demographics and basic information about the hernias are detailed in Table 1. Of the 1240 hernia repairs considered, 117 (9.4%) presented as recurrent, with the remaining 1123 (90.6%) being primary. Most patients were operated on for bilateral hernias (58.4%) (Table 1). The most prevalent hernia type for both sides was indirect, followed by direct, pantaloon (direct and indirect), complex (some combination of types other than direct and indirect), femoral, and sports, in that order (Table 2). Indirect, direct, and femoral components of all defects were further categorized by size as small, medium, or large, using the surgeon's system of size classification based on an anatomic analysis; the definitions used in this method of size evaluation are delineated in Figure 1. Analysis using these definitions revealed most hernias to be small, followed by medium, and then large (Table 3).
Table 2.
Breakdown of Hernia Types
| Hernia Type | n |
|---|---|
| Indirect, n | 624 |
| Direct, n | 334 |
| Combination, n | 271 |
| Pantaloon (direct and indirect) | 236 |
| Complex | 35 |
| Femoral, n | 8 |
| Sports, n | 2 |
Figure 1.
Criteria used for hernia size classification.
Table 3.
Sizes of the Different Component Types of All Hernias
| Hernia Size | Indirect | Direct | Femoral | Sports |
|---|---|---|---|---|
| Small | 470 (52.7) | 289 (49.9) | 34 (81.0) | 1 (33.3) |
| Medium | 301 (33.7) | 224 (38.7) | 7 (16.6) | 2 (66.7) |
| Large | 121 (13.6) | 66 (11.4) | 1 (2.4) | 0 (0) |
| Total | 892 | 579 | 42 | 3 |
Data are number of cases (% of total).
Hernia size and type distributions were significantly different between the sexes, and also varied with age. Indirect followed by femoral hernias were most common in women, whereas direct followed by indirect were most common in men. Larger hernias were more often seen in men (P < .001), and the average age of patients with large hernias was older (P < .001). Patients who presented with at least one direct hernia were also older, whereas those who presented with at least one indirect hernia were younger (P < .001, P = .001, respectively). A higher percentage of male patients than females presented with at least one recurrent hernia (13.9% vs 4.9%, P = .048).
Procedure and Follow-Up
The TEP technique was used for all inguinal hernia repairs, with the exception of procedures in the 7 patients (0.9%) who underwent a conversion to TAPP repair. The most common concurrent procedure accompanying inguinal repair was umbilical hernia repair. Of the 166 umbilical hernias repaired (21.2% of patients), 93 were repaired without mesh, whereas mesh was used in 73. Within the series, there were 36 other procedures (i.e., not umbilical hernia repairs) performed alongside inguinal repair; these are listed in Table 4 along with details of all concomitant procedures.
Table 4.
Concomitant Operative Procedures
| Concomitant Operation | n |
|---|---|
| Umbilical hernia repair | 166 |
| Without mesh | 93 |
| With mesh | 73 |
| Other procedure | 36 |
| Vasectomy | 2 |
| Cholecystectomy | 5 |
| Hysterectomy | 1 |
| Ovarian cystectomy | 1 |
| Seed implants for bladder cancer | 1 |
| Lysis of adhesions | 4 |
| Excision of soft tissue abdominal wall tumor | 1 |
| Heller myotomy | 1 |
| Gynecologic laparoscopy for infertility | 1 |
| Tubal ligation | 1 |
| Bowel resection | 1 |
| Nissen fundoplication | 1 |
| Appendectomy for chronic pain | 1 |
| Repair of recurrent hydrocele | 1 |
| Incisional hernia repair | 8 |
| Parastomal hernia repair | 1 |
| Epigastric hernia repair | 3 |
| Paraesophageal hernia repair | 1 |
| Spigelian hernia repair | 1 |
| Total | 202 |
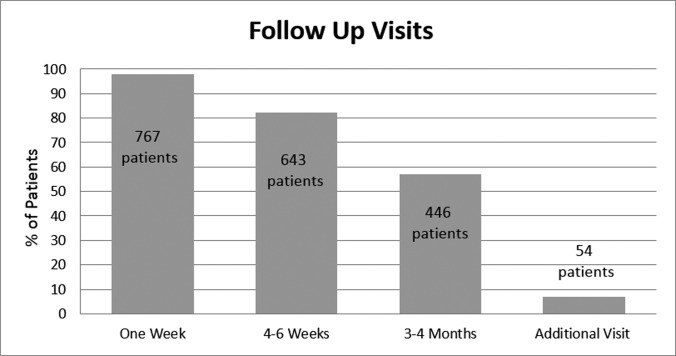
Of the 783 patients considered for this study, 98.0% had a follow-up at the office 1 week after surgery, 82.1% completed follow up at 5–7 weeks after surgery, and 57.0% returned approximately 5–6 months after surgery (Figure 2). In addition, 54 patients (6.9%) returned after their standard postoperative visits, for other unrelated medical issues or further evaluation of specific concerns.
Figure 2.
Postoperative follow-up.
Complications
The 2 major outcomes assessed were intraoperative and postoperative complications. Recurrence rate was also noted for completeness of the clinical picture, but because of lack of standardized long term follow-up, recurrence was not the focus of this paper. No intraoperative complications occurred. There were 106 patients who experienced a total of 114 postoperative complications (13.5% of patients, 9.2% of procedures) across the 8 categories evaluated: seroma (n = 37), urinary retention (n = 32), testicular/hemiscrotal swelling (n = 23), neurological symptoms (12 transient, 2 persistent), hydrocele (n = 7), wound/mesh infection (n = 1), and testicular atrophy (n = 0). Table 5 details the complication rates, both per patient and per case (since bilateral hernia repairs were considered 2 cases); of note, the patients who had bilateral repairs and also experienced a complication all had only unilateral symptoms for the given complication. Six procedures resulted in recurrences (0.5%), with average time to recurrence of 18 moths (range, 3–56); recurrences were not included in the complication rate because, as mentioned previously, the follow-up period in this study was not long enough to properly assess this variable.
Table 5.
Complications
| Complication Category | n | Cases, % | Patients, % |
|---|---|---|---|
| Intraoperative complications | 0 | 0 | 0 |
| Early postoperative complications | |||
| Seroma | 37 | 3.0 | 4.7 |
| Urinary retention | 32 | 2.6 | 4.1 |
| Testicular/hemiscrotal swelling | 23 | 1.9 | 2.9 |
| Transient neurological symptoms | 12 | 1.0 | 1.5 |
| Persistent neurological symptoms | 2 | 0.2 | 0.3 |
| Hydrocele | 7 | 0.6 | 0.9 |
| Testicular atrophy | 0 | 0.0 | 0.0 |
| Mesh infection | 1 | 0.1 | 0.1 |
| Total | 106a | 9.2a | 13.5a |
Some patients experienced more than one complication; 114 total complications occurred, with this number being used to calculate percentage of cases with complication, and 106 being used to calculate percentage of patients with complication.
Seromas all resolved spontaneously before the last office visit. Patients who experienced urinary retention had catheters placed and were started on tamsulosin hydrochloride. Catheters were removed on the third or fourth postoperative day at a urologist's office. All patients had relief of their symptoms with this course of action, and no prostatectomies were required. The presence of a hydrocele was diagnosed by clinical examination, and confirmed by ultrasound. One of the 7 hydroceles spontaneously resolved 4 months after the procedure, and the others were either permanent or required surgical intervention to repair.
Patients were found to have neurological symptoms if they complained of radicular pain immediately after surgery or significant discomfort at their second postoperative visit or later. These patients were advised to perform stretching exercises, with or without a 5-day course of an anti-inflammatory, as per the patient's preference. Patients were instructed in the postoperative visit to call or return to the office if they had any persistent symptoms. If the symptoms had not resolved by the final postoperative visit, the patient was classified as having persistent neurological symptoms. The 2 patients who had persistent neurological problems both experienced hypersensitivity of the scrotal skin and testicle; for 1 patient the hypersensitivity was relieved by support, but still persisted, and for the second patient support did not help. The patient who experienced an infection underwent a reoperation for removal of the implanted mesh, and the mesh was determined to contain a factory contaminant (Mycobacterium fortuitum).
There were no statistically significant differences in complication rates between the sexes, though, of note, there were no cases of female urinary retention. Overall complication rate did not vary with age, but a relationship was discovered within some of the specific complication categories. The average age of patients experiencing urinary retention was significantly higher than those who did not experience this complication (60.4 and 52.0 years, respectively; P = .001). The same phenomenon was seen in patients in whom seromas developed; the average age of patients who had a seroma was 57.1 years, whereas those who did not were an average of 52.2 years of age (P = .036). Of note, although older patients tended to have more direct hernias and larger hernias, neither size nor type was found to be related to urinary retention or seroma formation when controlling for age.
Recovery Metrics
Additional outcomes included pain evaluation and recovery metrics; results are displayed in Table 6. Patients used an average of 5.6 Percocet 10/325 pills (median 3.0; range 0–40) after surgery. Patients took an average of 3.0 days (median, 3.0; range, 1–41) to return to work, and return to ADLs and significant physical activity took an average of 3.8 d (median, 3.0; range, 0–28). Age was significantly, although weakly, negatively correlated with number of Percocets used (Pearson's correlation, R = −0.160; P < .001), time to return to work (Spearman's ρ = −0.075; P = .037), and time to return to ADLs (Spearman's ρ = −0.084; P = .019). Percocet usage varied between the sexes, with an average of 5.8 pills (median, 3.0) consumed by males compared with 3.1 by females (median, 1.5) (P < .001), although time to return to work and ADLs were similar (P = .929; = .850). Hernia size was significantly related to time to return to ADLs, according to 1-way ANOVA results (P = .035) and remained an independently significant factor when controlling for age.
Table 6.
Recovery Metrics
| Metric | Data |
|---|---|
| Percocet Usagea | |
| Average (SD) | 5.6 pills (7.4) |
| Median | 3 pills |
| Range | 0–40 pills |
| Number used (%) | |
| >15 pills | 70 patients (9.0) |
| 6–15 pills | 197 patients (25.3) |
| 1–5 pills | 302 patients (38.8) |
| None | 209 patients (26.9) |
| Return to worka | |
| Average (SD) | 3.0 days (2.1) |
| Median | 3 days |
| Range | 1–41 days |
| Return to work ≤3 days (%) | 583 patients (74.7%) |
| Return to ADLsa | |
| Average (SD) | 3.8 days (2.5) |
| Median | 3 days |
| Range | 0–28 days |
| Return to ADLs ≤1 week (%) | 749 patients (96.0%) |
Percocet usage was not reported by 5 patients; return to work and ADLs were not reported by 3 patients.
Bilateral Versus Unilateral Repairs
Complication rates did not vary significantly between patients who had bilateral repairs compared with those who had only a unilateral repair (P = .507), although mean recovery times were slightly longer and number of Percocets slightly more for patients with bilateral repairs (though not statistically significant). Time to return to work was on average 3.1 days for patients with bilateral repairs and 2.9 days for those with unilateral repairs (P = .065); time to return to ADLs was, on average, 3.9 and 3.6 days in the bilateral and unilateral groups, respectively (P = .062). Percocet usage was 6.0 pills versus 5.1 pills in bilateral versus unilateral repairs, respectively (P = .078).
Simultaneous Procedures
Patients who had a simultaneous procedure along with the inguinal hernia repair did not have a higher complication rate, but there were significant differences in recovery. Kruskal-Wallis H test of 4 groups of patients—no concomitant procedure, umbilical hernia repair without mesh, umbilical hernia repair with mesh, and any other concomitant procedure—found significant differences in Percocet usage and return to ADLs between groups. Post hoc pairwise comparisons found that patients who had umbilical hernia repairs without mesh had significantly higher mean rank time to return to ADLs and higher number of Percocets taken (although no change in return to work) than patients that had no concomitant procedure. In addition, patients who had a concomitant procedure other than umbilical hernia repair displayed significantly higher mean rank time to return to ADLs (although no significant difference in use of Percocet or time to return to work) (Table 7).
Table 7.
Differences in Recovery Metrics for Patients Who Underwent Concomitant Procedures
| A. Return to Work | |||
|---|---|---|---|
| Concomitant Procedure | Mean (days) | Median (days) | Mean Rank |
| Group A: none | 2.9 | 3.0 | 378.94 |
| Group B: umbilical without mesh | 3.1 | 3.0 | 411.41 |
| Group C: umbilical with mesh | 3.3 | 3.0 | 430.71 |
| Group D: other procedure | 3.2 | 3.0 | 448.60 |
| Kruskal-Wallis H | P = 0.059 | ||
| B. Return to ADL | |||
|---|---|---|---|
| Concomitant Procedure | Mean (days) | Median (days) | Mean Rank |
| Group A: none | 3.6 | 3.0 | 377.62a,b |
| Group B: umbilical without mesh | 4.3 | 4.0 | 429.15a |
| Group C: umbilical with mesh | 3.9 | 3.0 | 409.28 |
| Group D: other procedure | 4.3 | 4.0 | 469.57b |
| Kruskal-Wallis H | P = 0.023 | ||
| Post hoc pairwise comparison | aP = 0.041 between groups A and B | ||
| bP = 0.017 between groups A and D | |||
| C. Number of Percocets Taken | |||
|---|---|---|---|
| Concomitant Procedure | Mean (pills) | Median (pills) | Mean Rank |
| Group A: None | 5.3 | 3.0 | 375.40a |
| Group B: Umbilical without mesh | 7.9 | 5.0 | 449.49a |
| Group C: Umbilical with mesh | 6.2 | 4.5 | 423.29 |
| Group D: Other procedure | 4.3 | 3.0 | 412.37 |
| Kruskal-Wallis H | P = 0.012 | ||
| Post hoc pairwise comparison | aP = 0.004 between groups A and B | ||
Surgeon Experience
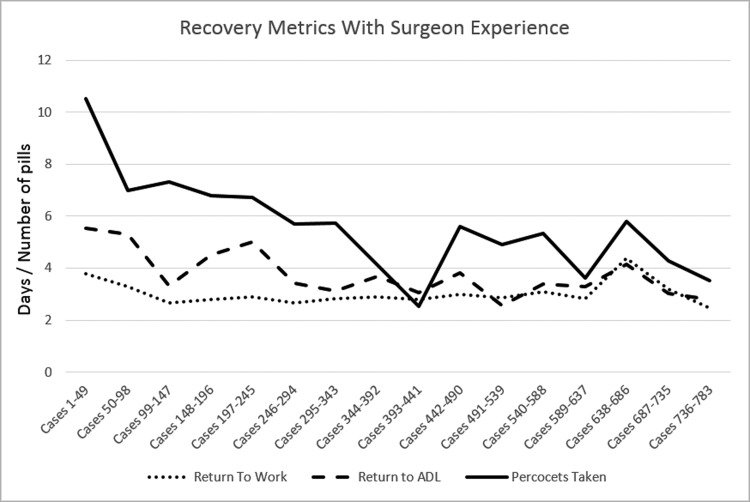
Although the rate of complications and the time patients needed to return to work did not vary much over the time course of the study, the time taken to return to ADLs and the number of Percocets taken decreased as more cases were performed by the surgeon (Figure 3). Number of procedures completed had a negative correlation with both time to return to ADLs (R = −0.662; P = .005) and number of Percocets used (R = −0.732; P = .001).
Figure 3.
Recovery metrics with increasing physician experience.
DISCUSSION
The results of this series support the claim that TEP is a safe and effective repair in the surgical treatment of inguinal hernia. Postoperative complication rates are comparable to and within the generally accepted range of other institutions' results with laparoscopic inguinal hernia repairs. It must be noted that direct comparisons are difficult, owing to the variable selection of complications across different studies. However, examination of the available case series' and controlled trials from recent years shows similar rates of seroma (0.52–37.8%), urinary retention (0.38–8.3%), and persistent pain (0.3–25%) for this series.2,8,10,17–22 In addition, the fact that no intraoperative or immediate postoperative complications were experienced supports the claim of the safety of the TEP procedure and is particularly salient in light of other studies that have found laparoscopic and specifically TEP procedures to have a higher incidence of serious perioperative complications than open procedures.9,13
Convalescence times were shorter than most results available in the literature,7,16,23,24 which is believed to be partly due to the experience and technique of the surgeon. In addition, the surgeon's more aggressive treatment of the recovery period (encouraging active recovery and limiting restrictions) is believed to play a large role in these results, as well as occupational and socioeconomic factors related to the patient population. It would be ideal to include an analysis of the motivational and socioeconomic factors that may impact a patient's recovery in future studies, and perhaps control for variables of this category in more regulated trials. The surgeon's postoperative instructions regarding exercise and return to work were uniform for all the included concurrent procedures and are the same instructions used for laparoscopic repair of inguinal hernia.
A notable observation is the similarity in complication rate between bilateral repairs and unilateral repairs, a finding relevant to the widely debated issue of prophylactic contralateral repair. The absence of a statistically significant difference in return to work, return to ADLs, and usage of narcotics between the bilateral and unilateral groups, along with the similarity in complications, suggests that a bilateral repair does not have notably higher risks or morbidity than a unilateral repair.
When the authors analyzed the data concerning concomitant procedures, they found when combining laparoscopic inguinal hernia repair(s) with open umbilical hernia repair (without mesh) that there was an increase in Percocet usage (mean, 2.6 additional pills) and longer time to return to ADL (mean, 0.7 additional days). Similarly, when combining laparoscopic inguinal hernia repair with other procedures (other than umbilical hernia repair), there was an increase in time to return to ADL (mean, 0.7 additional days). These differences, while reaching statistical significance, were in the authors' opinion, small enough to not have a meaningful clinical impact. The authors believe that these findings should encourage the performance of surgically indicated concomitant procedures.
The use of Foley catheterization in all patients may be criticized in light of recommendations against routine use of catheterization12; however, the standardized use of a catheter was felt to minimize the likelihood of bladder injury or perforation and to increase the likelihood that if such an injury occurred, it would be detected.25 Given the urinary retention rate of 4.1%, use of the Foley catheter does not seem to be associated with an unacceptable level of postoperative urinary consequences, and the lack of any intraoperative complications lends strength to the idea that intraoperative catheterization of patients with TEP inguinal hernia repair could be helpful in preventing bladder injury.
In this series, a minimum of 10 staples were used per patient for mesh fixation, which previous studies have cited as a risk factor for both early postoperative and chronic pain or hypersensitivity.26–28 The prior results were not at all consistent with findings in this study, which had low postoperative narcotic usage, transient neurological sequelae of only 1.0%, and an incidence of only 0.2% of hypersensitivity that persisted past the last postoperative visit. The authors believe that the surgical technique, in particular adequate dissection to identify the anatomy and avoidance of the “triangle of pain” with respect to stapling, is crucial to preventing inguinodynia associated with staples or tacks, as is early return to full physical activity.
Perhaps the greatest weakness in this study is the short follow-up period, which may call any claims as to a low incidence of chronic pain into question. However, given that chronic pain is both predicted by early postoperative pain29 and usually presents as neuropathic pain in the early postoperative period and then persists after 3–6 months,30 the percentage of patients who experience neurological pain within the early postoperative period that this study assessed could be used as a conservative estimate of patients that at least had the potential to develop chronic pain if the symptoms did not go away, or happened to return. In this case, the 14 patients who experienced neurologic pain in the postoperative period (1.8%) is still a relatively low number compared with results in the literature and would lend strength to the claim that fixation devices do not necessarily lead to a high chronic neuropathic pain rate. Aside from chronic pain, the nature of the surgical complications studied would indicate that most adverse effects should have been detected and resolved by the time of the last visit.
Another weakness of this study is that analgesic usage was a measure of postoperative pain; it is not an ideal surrogate measure for pain, as it can be dependent on patients' willingness to take or prior experience with pain medication. The more commonly used hernia-related pain assessment tools currently employed, such as the Carolinas Comfort Score (http://www.carolinashealthcare.org/carolinas-comfort-scale), were not as widely available and verified at the start of the case series, so for consistency in metrics, use of analgesics was the chosen measurement. However, the early return to full activity lends some support to the assessment of pain level and narcotic analgesia requirements. Similarly, the size classification system used is not a standardized universal system, because most classification algorithms used today were not in place at the beginning of the study period.
Despite these weaknesses, the overall results in this series demonstrate relatively low complication rates and short convalescence times. One major reason for these outcomes involves the experience of the operating surgeon. The importance of surgeon experience level is also illustrated in the statistically significant decrease in recovery times and analgesia usage with the later cases in the series. These improvements over time can be partly attributed to the surgeon's becoming more comfortable with encouraging earlier return to activities as he observed results and fine-tuned the routine and nuances of the repair and its results (although the same official postoperative instructions were given to all patients). However, consideration of this type of experience in addition to technical experience is clearly also important if it contributes to better recovery metrics.
In this single-surgeon study, we comprehensively looked at and analyzed a variety of variables and metrics for inguinal hernia repair. The most significant are low narcotic use after surgery and early return to work and ADLs. Fixation with multiple staples was thought by the surgeon to prevent early postoperative migration of the mesh before tissue incorporation, and this technique allowed the surgeon to encourage the patients to begin significant physical activity in the very early postoperative stages. The authors believe that this early activity was one of the contributing factors to the patients' early return to work and resumption of ADLs. The findings in this review series demonstrate that proficiency in laparoscopic approaches can yield good results in several areas and an acceptable level of complications when compared to other studies. In addition, the low rate of early postoperative neurologic complications seen with the use of multiple Endostaples is in contrast to previous studies and supports the claim that Endostaples are not necessarily related to higher incidences of postoperative neurological problems if a careful technique is used. Because of the distinct advantages after surgery and low complication rates, laparoscopic inguinal hernia surgery, particularly the described technique for TEP with an experienced surgeon operating, is recommended as a safe and effective alternative to older open procedures, with clear benefits and limited risks.
Contributor Information
Mark A. Reiner, Department of Surgery, Icahn School of Medicine and the Mount Sinai Healthcare System, New York, New York, USA..
Erin R. Bresnahan, Icahn School of Medicine at Mount Sinai, New York, New York, USA..
References:
- 1. Bittner R, Schwarz J. Inguinal hernia repair: current surgical techniques. Lagenbecks Arch Surg. 2012;397:271–282. [DOI] [PubMed] [Google Scholar]
- 2. Poelman MM, van den Heuvel B, Deelder JD, et al. EAES Consensus Development Conference on endoscopic repair of groin hernias. Surg Endosc. 2013;27:3505–3519. [DOI] [PubMed] [Google Scholar]
- 3. Basile F, Biondi A, Donati M. Surgical approach to abdominal wall defects: history and new trends. Int J Surg. 2013;11(Suppl 1):S20–S23. [DOI] [PubMed] [Google Scholar]
- 4. Simons MP, Aufenacker T, Bay-Nielsen M, et al. European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2009;13:343–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Miserez M, Peeters E, Aufenacker T, et al. Update with level 1 studies of the European Hernia Society guidelines on the treatment of inguinal hernia in adult patients. Hernia. 2014;18:151–163. [DOI] [PubMed] [Google Scholar]
- 6. Saleh F, Okrainec A, D'souza N, Kwong J, Jackson TD. Safety of laparoscopic and open approaches for repair of the unilateral primary inguinal hernia: an analysis of short-term outcomes. Am J Surg. 2014;208:195–201. [DOI] [PubMed] [Google Scholar]
- 7. Bobo Z, Nan W, Qin Q, Tao W, Jianguo L, Xianli H. Meta-analysis of randomized controlled trials comparing Lichtenstein and totally extraperitoneal laparoscopic hernioplasty in treatment of inguinal hernias. J Surg Res. 2014;192:409–420. [DOI] [PubMed] [Google Scholar]
- 8. Eker HH, Langeveld HR, Klitsie PJ, et al. Randomized clinical trial of total extraperitoneal inguinal hernioplasty vs Lichtenstein repair: a long-term follow-up study. Arch Surg. 2012;147:256–260. [DOI] [PubMed] [Google Scholar]
- 9. Kouhia S, Vironen J, Hakala T, Paajanen H. Open mesh repair for inguinal hernia is safer than laparoscopic repair or open non-mesh repair: A Nationwide Registry Study of Complications. World J Surg. 2015;39:1878–1884. [DOI] [PubMed] [Google Scholar]
- 10. Li J, Wang X, Feng X, Gu Y, Tang R. Comparison of open and laparoscopic preperitoneal repair of groin hernia. Surg Endosc. 2013;27:4702–4710. [DOI] [PubMed] [Google Scholar]
- 11. O'reilly EA, Burke JP, O'Connell PR. A meta-analysis of surgical morbidity and recurrence after laparoscopic and open repair of primary unilateral inguinal hernia. Ann Surg. 2012;255:846–853. [DOI] [PubMed] [Google Scholar]
- 12. Bittner R, Arregui ME, Bisgaard T, et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia International Endohernia Society (IEHS). Surg Endosc. 2011;25:2773–2843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gass M, Banz VM, Rosella L, Adamina M, Candinas D, Güller U. TAPP or TEP? Population-based analysis of prospective data on 4,552 patients undergoing endoscopic inguinal hernia repair. World J Surg. 2012;36:2782–2786. [DOI] [PubMed] [Google Scholar]
- 14. Köckerling F, Schug-pass C, Jacob DA, Keller T. The intra- and postoperative complication rate of TEP in patients undergoing unilateral endoscopic inguinal hernia repair is not higher compared with TAPP. World J Surg. 2013;37:933–934. [DOI] [PubMed] [Google Scholar]
- 15. Köckerling F, Bittner R, Jacob DA, et al. TEP versus TAPP: comparison of the perioperative outcome in 17,587 patients with a primary unilateral inguinal hernia. Surg Endosc. 2015;29:3750–3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Antoniou SA, Antoniou GA, Bartsch DK, et al. Transabdominal preperitoneal versus totally extraperitoneal repair of inguinal hernia: a meta-analysis of randomized studies. Am J Surg. 2013;206:245–252.e1. [DOI] [PubMed] [Google Scholar]
- 17. Krishna A, Misra MC, Bansal VK, Kumar S, Rajeshwari S, Chabra A. Laparoscopic inguinal hernia repair: transabdominal preperitoneal (TAPP) versus totally extraperitoneal (TEP) approach: a prospective randomized controlled trial. Surg Endosc. 2012;26:639–649. [DOI] [PubMed] [Google Scholar]
- 18. Sivasankaran MV, Pham T, Divino CM. Incidence and risk factors for urinary retention following laparoscopic inguinal hernia repair. Am J. Surg. 2014;207:288–292. [DOI] [PubMed] [Google Scholar]
- 19. El-dhuwaib Y, Corless D, Emmett C, Deakin M, Slavin J. Laparoscopic versus open repair of inguinal hernia: a longitudinal cohort study. Surg Endosc. 2013;27:936–945. [DOI] [PubMed] [Google Scholar]
- 20. Swadia ND. Laparoscopic totally extra-peritoneal inguinal hernia repair: 9 year's experience. Hernia. 2011;15:273–279. [DOI] [PubMed] [Google Scholar]
- 21. Eklund A, Montgomery A, Bergkvist L, Rudberg C. Chronic pain 5 years after randomized comparison of laparoscopic and Lichtenstein inguinal hernia repair. Br J Surg. 2010;97:600–608. [DOI] [PubMed] [Google Scholar]
- 22. Langeveld HR, van't Riet M, Weidema WF, et al. Total extraperitoneal inguinal hernia repair compared with Lichtenstein (the LEVEL-Trial): a randomized controlled trial. Ann Surg. 2010;251:819–824. [DOI] [PubMed] [Google Scholar]
- 23. Bansal VK, Misra MC, Babu D, et al. A prospective, randomized comparison of long-term outcomes: chronic groin pain and quality of life following totally extraperitoneal (TEP) and transabdominal preperitoneal (TAPP) laparoscopic inguinal hernia repair. Surg Endosc. 27:2373–2382. [DOI] [PubMed] [Google Scholar]
- 24. Tolver MA, Strandfelt P, Forsberg G, Hjørne FP, Rosenberg J, Bisgaard T. Determinants of a short convalescence after laparoscopic transabdominal preperitoneal inguinal hernia repair. Surgery. 2012;151:556–563. [DOI] [PubMed] [Google Scholar]
- 25. Ulker K, Akso O, Cecen K, Ermuthlu CS, Temur I, Kilic E. CO2 flow dynamics of bladder injury during laparoscopy and the effect of the content of the abdominal viscera during injury–experimental study. Adv Clin Exp Med. 2015;24:775–781. [DOI] [PubMed] [Google Scholar]
- 26. Kaul A, Hutfless S, Le H, et al. Staple versus fibrin glue fixation in laparoscopic total extraperitoneal repair of inguinal hernia: a systematic review and meta-analysis. Surg Endosc. 2012;26:1269–1278. [DOI] [PubMed] [Google Scholar]
- 27. Shah NS, Fullwood C, Siriwardena AK, Sheen AJ. Mesh fixation at laparoscopic inguinal hernia repair: a meta-analysis comparing tissue glue and tack fixation. World J Surg. 2014;38:2558–2570. [DOI] [PubMed] [Google Scholar]
- 28. Schwab R, Willms A, Kröger A, Becker HP. Less chronic pain following mesh fixation using a fibrin sealant in TEP inguinal hernia repair. Hernia. 2006;10:272–277. [DOI] [PubMed] [Google Scholar]
- 29. Tolver MA, Rosenberg J, Bisgaard T. Early pain after laparoscopic inguinal hernia repair: a qualitative systematic review. Acta Anaesthesiol Scand. 2012;56:549–557. [DOI] [PubMed] [Google Scholar]
- 30. Alfieri S, Amid PK, Campanelli G, et al. International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Hernia. 2011;15:239–249. [DOI] [PubMed] [Google Scholar]