Abstract
There is growing evidence that diversely defined blood pressure variability (BPV) is an independent predictor of hypertensive target organ damage (TOD) and cardiovascular events. Several mechanisms have been speculated to underlie episodes of increased BPV, including the impairment of autonomic or hormonal regulation, renal dysfunction, and increased arterial stiffness. Within-home BPV, defined as differences in BP values obtained on a single occasion at home, could have prognostic significance for hypertensive TOD. It is typically thought that BP values are decreased with repeated measurements on a single occasion at home, but in the present subanalysis of 4,149 J-HOP (Japan Morning Surge-Home Blood Pressure) study patients, approximately 20% of the patients' home BP values were increased or unchanged by repeated measurements on a single occasion. In addition, those patients were likely to have hypertensive TOD. Thus, home BP measurement should be taken twice or more to detect the increase trend in home BP, which has been defined as within-home BPV.
Key Words: Blood pressure variability, Home blood pressure, Multiple measurement on a single occasion
Relationship between Blood Pressure Variability and Hypertensive Target Organ Damage and Prognosis
There is growing evidence that diversely defined blood pressure variability (BPV) is an independent predictor of hypertensive target organ damage (TOD) and cardiovascular events [1,2,3]. In particular, long-term BPV was defined as visit-to-visit BP fluctuation at a clinic, which was a strong predictor of stroke in systolic BP (SBP), independent of the mean SBP value [4]. Mid-term BPV has been defined as day-by-day BP fluctuation in home BP (HBP) values, and it has been also shown to contribute to the risks of total, cardiovascular, and stroke mortality [5]. Short-term BPV is defined as reading-to-reading BP fluctuation in ambulatory BP measurements, which has also been demonstrated to be a significant and independent predictor of mortality and of cardiovascular and stroke events [6].
Several mechanisms have been suggested to underlie episodes of increased BPV, including the impairment of autonomic or hormonal regulation, renal dysfunction, and increased arterial stiffness [7]. Each of the above-described types of BPV has been examined in light of the clinical implications of multiple BP measurements and clinical applications. Even for multiple BP measurements obtained on one occasion, the BPV was reported to be a prognostic marker of cardiovascular events [1], in a phenomenon named ‘within-visit BPV’ in clinic BP measurement. Conversely, some studies showed no association of within-visit BPV with outcomes [8].
In accordance with this trend, within-home BPV (defined as differences in BP values obtained on a single occasion at home) could have prognostic significance for hypertensive TOD. However, our previous guideline for HBP measurement recommended taking one BP measurement twice a day, in the morning and evening. We revised this recommendation to an average of two measurements on each occasion (morning and evening) in accordance with the European guideline [9]. Within-home BPV has not been studied sufficiently. In the present study, we conducted a subanalysis of the Japan Morning Surge-Home Blood Pressure (J-HOP) study to determine whether the differences in BP values measured on a single occasion at home can be used to predict hypertensive TOD, and our results demonstrated that an increased trend in HBP values obtained on a single occasion is associated with hypertensive TOD [10].
Brief Methods and Protocol of the J-HOP Study
The J-HOP study enrolled 4,149 ambulant patients. HBP values were measured by the patients, using a validated upper arm cuff oscillometric BP device according to the Japanese Society of Hypertension 2004 guidelines [11]. This device automatically takes three measurements at 15-second intervals after a measurement button is pressed once. For the measurement of HBP, the patients were instructed to take their BP in a sitting position after at least 2 min of rest, and to measure their morning HBP and evening HBP in a sitting position each day for a 2-week period. All data in the HBP measurement device were downloaded to a computer and sent to the study control center.
The single-occasion difference in HBP values was defined as the difference between the first HBP value minus the average of the second and third HBP values. To avoid using an arbitrary definition, we defined the median quintile group (third quintile) as the comparator group. We hypothesized that the differences in BP values measured on a single occasion at home can be used to predict hypertensive TOD, and we contend that our findings provide evidence for recommending multiple BP measurements on a single occasion at home.
Results of Our Subanalysis of the J-HOP Study
The first BP and the mean BP values of twice measurements have been shown in table 1. We divided all 4,149 patients of the J-HOP into quintile groups according to the differences between their first home SBP values and the average of the second and third home SBP values. Compared to the median quintile group, the patients in the first quintile group (i.e., those with elevated second and third home SBP values compared to the first value) were significantly older, significantly more likely to be male, and had significantly lower body mass index values, a significantly higher percentage of alpha-blocker medication use, a significantly higher smoking rate, a significantly higher rate of diabetes mellitus, and a significantly higher average of the second and third home SBP values. Compared to the quintile median, the fifth quintile patients (i.e., those with the greatest differences between their first home SBP values and the average of the second and third home SBP values) were significantly older, significantly more likely to be female, and had a significantly higher rate of hypertension, a significantly lower smoking rate, and significantly higher average home SBP.
Table 1.
Single versus twice BP measurement(s) for within-home BPV
| First BP value, mm Hg | 136.2±15 |
| Mean BP value of twice measuremen ts, mm Hg | 135.5±14 |
| p value | <0.001 |
Compared to the quintile median, the fifth quintile patients (i.e., those with the greatest differences between their first home SBP values and the average of the second and third home SBP values) were significantly older, significantly more likely to be female, and had a significantly higher rate of hypertension, a significantly lower rate of smoking, and significantly higher average home SBP values. Compared to the quintile median values, the TODs of the first quintile patients were significantly higher brain natriuretic peptide (BNP) levels, significantly higher NT-pro BNP levels, significantly higher brachial-ankle pulse wave velocity values, and significantly lower estimated glomerular filtration rate (eGFR) values. There were no significant differences among the quintile groups based on the difference between the first and the average of the second and third home SBP values in the left ventricular mass index, the urinary albumin creatinine ratio, the level of high-sensitivity cardiac troponin, or the intima-media thickness. On the other hand, compared to the quintile median values, the TODs of the first quintile patients were significantly higher NT-pro BNP. There were no significant differences among the quintile groups according to the difference between the first and the average of the second and third home SBP values in the other TODs.
We performed a UNIANOVA to test these TOD indicators independently of their association with the difference between the first and the average of the second and third home SBP values. Significantly different factors among quintile groups were selected as covariates for the confounding effects in the UNIANOVA, and the Bonferroni test was used for the multiple pairwise comparisons compared with the median quintile group. In the post hoc test, compared to the quintile median, the first quintile patients had independently and significantly higher BNP, higher NT-pro BNP, and lower eGFR values.
Changes in BP Values Obtained on a Single Occasion
Approximately 20% of the patients' home SBPs were not changed or were increased by the repeated measurements on a single occasion. In addition, 20% of the patients' home SBP values were decreased by >5 mm Hg with repeated measurement. Several studies have shown that SBP has a tendency to decrease with repeated measurement after the first reading; the reported differences between the first and second measurements were the averaged values 2.3 [12] and 3.5 mm Hg [13]. These repeated-measurement BP differences obtained on a single occasion have been observed for 7 [14] and 6 days [15]. However, these results were calculated from mass data. When the focus was on individual subjects' SBP changes over repeated (triplicate) measurements, decreased SBP was seen in 60% of the subjects, increased SBP was observed in 30%, and no change was seen in 10% [16]. Thus, it is important to keep in mind that with repeated measurements, many individuals will show increased HBP.
Mechanisms by Which the Increase in the Second and Third Values Would Result in Adverse Outcomes
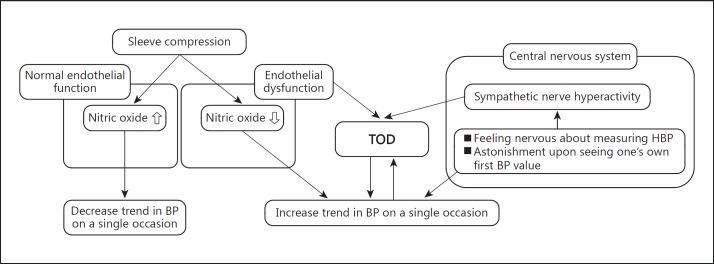
Several studies have noted that sympathetic nerve hyperactivity was associated with deteriorated BNP [17] and chronic kidney disease [18]. Easy sympathetic nerve hyperactivation due to an individual's astonishment upon seeing his or her own first BP values causes an elevation of SBP in the second and third measurements on a single occasion. Thus, the patients who easily develop sympathetic nerve hyperactivation may be likely to have deteriorated hypertensive TOD values: i.e., increased BNP, increased NT-pro BNP, and decreased eGFR (fig. 1).
Fig. 1.
Mechanisms and relations underlying the increased BP trend on a single occasion of HBP measurements, sympathetic nerve hyperactivity, and hypertensive TOD. The relationship between the increased BP trend on a single occasion of HBP measurement and endothelial dysfunction is also shown.
It has been speculated that peripheral vasodilatation could be induced by nitric oxide, which was activated with compression sleeves in patients with normal endothelial function [19]. Therefore, the BP would be unlikely to decrease in patients with endothelial dysfunction, who are likely to be associated with TOD (fig. 1).
Clinical Applications of Our Findings
The methods and vision for applying our present findings in clinical settings are as follows. (1) It is typically thought that BP values decrease with repeated measurement on a single occasion at home, but approximately 20% of the J-HOP patients' HBP values were increased or unchanged by repeated measurements on a single occasion. (2) It is especially important to check the increase trend in HBP by multiple measurements on a single occasion for patients who are older, male, with a lower body mass index, taking an alpha-blocker, smokers, and those with diabetes. (3) Patients who show an increase trend in HBP should be examined for hypertensive TOD, even if their HBP values are not very high, and (4) HBP should be measured twice or more to detect the increase trend in HBP (i.e., within-home BPV).
BP has been thought to decrease with repeated measurement on a single occasion at home, but in practice, this trend was observed in a clinical trial calculated from mass data. It is noteworthy that 1 of 5 J-HOP patients' HBPs was increased or not changed by repeated measurements on a single occasion. In addition, hypertensive TOD could be predicted by multiple measurements on a single occasion, whereas the hypertensive TOD could not be predicted by only a single measurement. Thus, multiple measurements should be employed on a single occasion for HBP measurement, and it is important to evaluate not only the absolute BP values but also the within-home BPV.
References
- 1.Rothwell PM, Howard SC, Dolan E, et al. Effects of beta blockers and calcium-channel blockers on within-individual variability in blood pressure and risk of stroke. Lancet Neurol. 2010;9:469–480. doi: 10.1016/S1474-4422(10)70066-1. [DOI] [PubMed] [Google Scholar]
- 2.Wei FF, Li Y, Zhang L, et al. Beat-to-beat, reading-to-reading, and day-to-day blood pressure variability in relation to organ damage in untreated Chinese. Hypertension. 2014;63:790–796. doi: 10.1161/HYPERTENSIONAHA.113.02681. [DOI] [PubMed] [Google Scholar]
- 3.Kikuya M, Hozawa A, Ohokubo T, et al. Prognostic significance of blood pressure and heart rate variabilities: the Ohasama study. Hypertension. 2000;36:901–906. doi: 10.1161/01.hyp.36.5.901. [DOI] [PubMed] [Google Scholar]
- 4.Rothwell PM, Howard SC, Dolan E, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895–905. doi: 10.1016/S0140-6736(10)60308-X. [DOI] [PubMed] [Google Scholar]
- 5.Kikuya M, Ohkubo T, Metoki H, et al. Day-by-day variability of blood pressure and heart rate at home as a novel predictor of prognosis: the Ohasama study. Hypertension. 2008;52:1045–1050. doi: 10.1161/HYPERTENSIONAHA.107.104620. [DOI] [PubMed] [Google Scholar]
- 6.Hansen TW, Thijs L, Li Y, et al. International Database on Ambulatory Blood Pressure in Relation to Cardiovascular Outcomes Investigators. Prognostic value of reading-to-reading blood pressure variability over 24 hours in 8,938 subjects from 11 populations. Hypertension. 2010;55:1049–1057. doi: 10.1161/HYPERTENSIONAHA.109.140798. [DOI] [PubMed] [Google Scholar]
- 7.Parati G, Faini A, Valentini M. Blood pressure variability: its measurement and significance in hypertension. Curr Hypertens Rep. 2006;8:199–204. doi: 10.1007/s11906-006-0051-6. [DOI] [PubMed] [Google Scholar]
- 8.Muntner P, Levitan EB, Reynolds K, et al. Within-visit variability of blood pressure and all-cause and cardiovascular mortality among US adults. J Clin Hypertens. 2012;14:165–171. doi: 10.1111/j.1751-7176.2011.00581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Parati G, Stergiou GS, Asmar R, et al. European Society of Hypertension practice guidelines for home blood pressure monitoring. J Hum Hypertens. 2010;24:779–785. doi: 10.1038/jhh.2010.54. [DOI] [PubMed] [Google Scholar]
- 10.Shibasaki S, Hoshide S, Eguchi K, et al. Japan Morning Surge-Home Blood Pressure (J-HOP) Study Group Increase trend in home blood pressure on a single occasion is associated with B-type natriuretic peptide and the estimated glomerular filtration rate. Am J Hypertens. 2015;28:1098–1105. doi: 10.1093/ajh/hpu295. [DOI] [PubMed] [Google Scholar]
- 11.Imai Y, Otsuka K, Kawano Y, et al. Japanese Society of Hypertension Japanese Society of Hypertension (JSH) guidelines for self-monitoring of blood pressure at home. Hypertens Res. 2003;26:771–782. doi: 10.1291/hypres.26.771. [DOI] [PubMed] [Google Scholar]
- 12.Johansson JK, Niiranen TJ, Puukka PJ, et al. Optimal schedule for home blood pressure monitoring based on a clinical approach. J Hypertens. 2010;28:259–264. doi: 10.1097/HJH.0b013e328332fa5e. [DOI] [PubMed] [Google Scholar]
- 13.Stergiou GS, Nasothimiou EG, Kalogeropoulos PG, et al. The optimal home blood pressure monitoring schedule based on the Didima outcome study. J Hum Hypertens. 2010;24:158–164. doi: 10.1038/jhh.2009.54. [DOI] [PubMed] [Google Scholar]
- 14.Verberk WJ, Kroon AA, Kessels AG, et al. The optimal scheme of self blood pressure measurement as determined from ambulatory blood pressure recordings. J Hypertens. 2006;24:1541–1548. doi: 10.1097/01.hjh.0000239289.87141.b6. [DOI] [PubMed] [Google Scholar]
- 15.Stergiou GS, Skeva II, Zourbaki AS, et al. Self-monitoring of blood pressure at home: how many measurements are needed? J Hypertens. 1998;16:725–731. doi: 10.1097/00004872-199816060-00002. [DOI] [PubMed] [Google Scholar]
- 16.Kawabe H, Saito I, Saruta T. Influence of repeated measurement on one occasion, on successive days, and on workdays on home blood pressure values. Clin Exp Hypertens. 2005;27:215–222. [PubMed] [Google Scholar]
- 17.Sakata K, Iida K, Mochiduki N, et al. Brain natriuretic peptide (BNP) level is closely related to the extent of left ventricular sympathetic overactivity in chronic ischemic heart failure. Intern Med. 2009;48:393–400. doi: 10.2169/internalmedicine.48.1599. [DOI] [PubMed] [Google Scholar]
- 18.Neumann J, Ligtenberg G, Klein IH, et al. Sympathetic hyperactivity in hypertensive chronic kidney disease patients is reduced during standard treatment. Hypertension. 2007;49:506–510. doi: 10.1161/01.HYP.0000256530.39695.a3. [DOI] [PubMed] [Google Scholar]
- 19.Sinoway LI, Hendrickson C, Davidson WR, Jr, et al. Characteristics of flow-mediated brachial artery vasodilation in human subjects. Circ Res. 1989;64:32–42. doi: 10.1161/01.res.64.1.32. [DOI] [PubMed] [Google Scholar]