Abstract
Background
The aim of this study was to determine the current practices and preferences of the arthroscopic surgeons of Delhi in the diagnosis, treatment and rehabilitation of patients with anterior cruciate ligament (ACL) injury.
Methods
It was a cross-sectional descriptive study conducted among arthroscopic surgeons of Delhi. A survey was conducted using a questionnaire that was sent either by e-mail or by direct contact to all sixty arthroscopic surgeons of Delhi.
Results
Forty-eight (80%) surgeons responded to our questionnaire. Maximum participants (83.3%) used semitendinosus/gracilis tendon autograft for ACL reconstruction (ACLR) and only 2.1% were using bone-patellar-tendon-bone (BPTB) autograft. Most preferred method of graft fixation was an ‘interference screw’ on the tibial side and an ‘endobutton’ on the femoral side, which was preferred by 95.83% and 93.75% surgeons, respectively. Almost all respondents (97%) used a bio-absorbable interference screw for tibial side graft fixation. Postoperative bracing was advised for <3 weeks by 47.9% surgeons and for 3–6 weeks by 31.3%. The results were analysed using statistical analysis.
Conclusion
Surgeon preferences in ACLR differ considerably among the arthroscopic surgeons of Delhi. There is majority consensus for using Hamstring autograft (single bundle) with a suspensory fixation on the femoral side and an aperture fixation on the tibial side. Transportal technique of making the femoral tunnel and preservation of amputation stump were the preferred methods. However, differences exist over the timing of surgery, rehab after surgery, pain management, etc.
Keywords: Anterior cruciate ligament injury, ACL Reconstruction, Hamstring autograft, Transportal technique, Rehabilitation
1. Introduction
The incidence of anterior cruciate ligament (ACL) injury is rising in India, but there are little epidemiological details available regarding the current practices for ACL reconstruction (ACLR) followed by arthroscopic surgeons in this region. This injury has significant social and economic implications. There is no consensus among the arthroscopic surgeons regarding the various issues related to the management of ACL injury like indications, surgical techniques, graft selection, fixation method and postoperative rehabilitation protocol. Hence, controversy remains prevalent amongst the arthroscopic surgeons, regarding non-surgical and surgical treatment of this injury. As a consequence of this variability, management protocol varies widely among surgeons of the same region.
To the best of our knowledge, no study has been published until now related to ACLR practices followed by arthroscopic surgeons of Delhi. However, several studies of other countries have been described in the literature (Table 1). The goal of this study was to determine the current practice followed by the members of the Delhi Arthroscopy Society (DAS) related to ACLR surgery.
Table 1.
Various studies showing anterior cruciate ligament reconstruction practices followed by arthroscopic surgeons worldwide.
| Sr. No. | Authors | Country | Year of publication | No. of respondents | Choice of grafts (in per cent) |
Choice of femoral fixation device (in per cent) |
Femoral portal preparation (in per cent) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HS | BPTB | Other | Endobutton | Screw | Cross pin | AM | TT | |||||
| 1. | Sandhu et al. | India | 2008 | 24 (57.14%) | 40.7 | 35.6 | 18.7 | 10.73 | 75.5 | <12.75 | NA | NA |
| 2. | Duquin et al. | USA | 2009 | 993 (57%) | 32 | 46 | 22 | NA | NA | |||
| 3. | Mc Rae et al. | Canada | 2011 | 283 (49%) | 73 | 29.9 | 7.3 | 51.5 | 36 | 12.5 | 27.9 | 69.6 |
| 4. | Mahnik et al. | Croatia | 2013 | 39 (75%) | 95 | 05 | 0 | 62 | 05 | 33 | 67 | 33 |
| 5. | Chechik et al. | 57 different | 2013 | 261 | 63 | 26 | 11 | 40 | 46 | 10 | 68 | 31 |
| 6. | Vaishya et al. | India (Delhi) | 2015 | 46 (80%) | 83.3 | 14.6 | 2.1 | 93.75 | 4.2 | 89.6 | 10.4 | |
2. Material and methods
A survey of current practices of ACLR followed by arthroscopic surgeons of DAS in Delhi was done. In this study, we have either sent a Proforma (questionnaire) by email to all the sixty registered members of the DAS or contacted them directly. Only 46 out of 60 orthopaedic surgeons working in both private and government organisations in Delhi responded to the questionnaire. Their preferences regarding various aspects of ACLR were noted. This included their experience in ACLR, the number of ACLR surgery done per year, preference for timing of surgery, anaesthesia, graft, tunnelling technique, implant used, etc. Their opinion regarding postoperative bracing, weight bearing and pain management was also noted. These data were evaluated, and statistical analysis was done using SPSS software.
3. Results
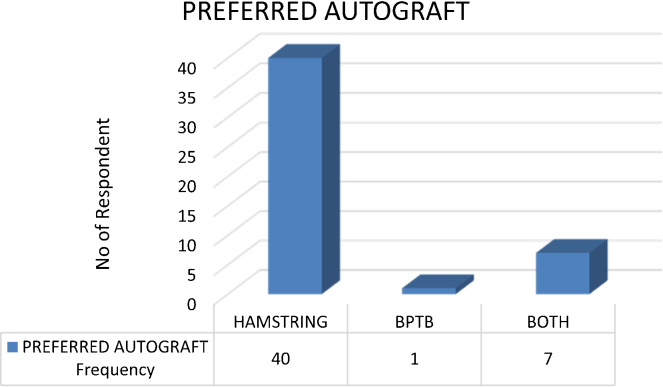
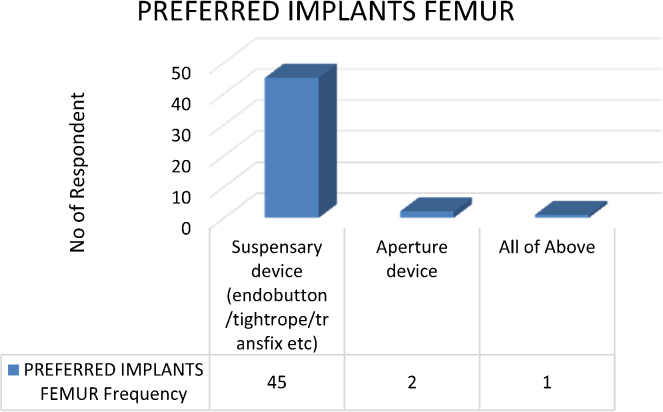
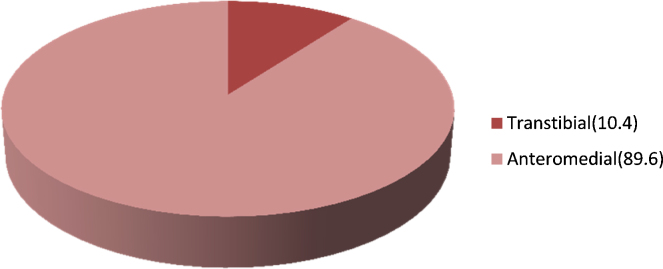
In this study, we analysed the preferences of 48 arthroscopic surgeons with the experience of ACLR surgery varying from 3 to 25 years. The majority of the respondents (31%) were performing >75 ACLR surgeries per year, while surgeons who perform <25 and between 25 and 50 ACLR per year are 27% each. Only 15% perform 50–75 surgeries per year. A total of 47.9% surgeons prefer to do ACLR at 3–6 weeks after ACL injury, while 29.2% prefer >6 weeks, and 22.9% prefer <3 weeks period. Preoperative knee magnetic resonance imaging (MRI) seems to be an important investigation for 91.66% of surgeons. Regarding anaesthesia of choice, 75% surgeons prefer spinal anaesthesia (SA), 16.7% prefer general anaesthesia (GA) and 8.3 prefer spinal plus epidural anaesthesia. A total of 93.7% surgeons use tourniquet throughout the surgery, while 6.3% use it during graft harvest only. Autografts are the graft of choice by most of the surgeons. None of them prefer allografts or synthetic grafts for ACLR. Amongst autografts, hamstring tendon graft is preferred by 83.3% surgeons, whereas 2.1% use bone-patella-tendon-bone (BPTB) graft, and 14.6% have no specific preference (Fig. 1). Most of the surgeons, i.e. 83.33%, like to perform single bundle reconstruct, while 10.4% surgeons perform double bundle and 6.3% surgeons have no specific preference. Intra-operatively, 91.6% surgeons prefer to preserve torn ACL remnants, while 8.3% excise it. Various types of fixation devices were used for fixation of the graft into tibial and femoral tunnels. Most preferred one is interference screw on the tibial side and endobuttons on the femoral side, which are preferred by 95.83% and 93.75% surgeons, respectively (Fig. 2). A total of 97.9% surgeons use outside in technique for tibial drilling and 89.6% surgeons prefer transportal approach for femoral tunnel preparation (Fig. 3). Postoperative bracing was advised for <3 weeks by 47.9% surgeons and for 3–6 weeks by 31.3%. About 14.6% surgeons do not prefer postoperative bracing. A total of 75% surgeons prefer early postoperative weight bearing before 3 weeks, while 25% prefer weight bearing after 3 weeks of surgery. Most of the surgeons, i.e. 72.9%, do not follow any special pain-relieving regimen for postoperative pain control, while 27% use various pain control interventions like femoral block, intra-articular sensorcaine or ropivacaine, epidural analgesia, etc.
Fig. 1.
Preferred choice of autograft followed in our study.
Fig. 2.
Preferred choice of implants used for fixation of graft on the femoral side.
Fig. 3.
Anteromedial or trans-tibial approach for femoral tunnel preparation.
4. Discussion
This survey was conducted amongst all the sixty registered members of DAS. Although all members were included in the study, only 48 (80%) members responded to our questionnaire. The responses showed diversity in various practices of ACLR amongst the respondents. Most of the parameters like graft choice, fixation devices and type of anaesthesia are dependent on surgeon's choice, patient's preference, previous surgical history, donor site morbidity, etc.
In an international survey of 261 orthopaedic surgeons from 57 countries by Chechik et al., 1 regarding their practices of ACLR, it was found that Hamstring autografts were preferred grafts of choice (63%) followed by BPTB (26%) graft. Anteromedial arthroscopic portal for femoral tunnel was preferred (68%) over trans-tibial portal (31%). Single bundle reconstruction was routinely performed by 67% of surgeons, while 33% perform double bundle reconstruction. Endobutton (40%) was the most preferred implant for the fixation of the graft into the bone tunnels, followed by bio-absorbable screw (34%), metallic interference screw (12%) and rigid fix (10%). This survey also showed that the surgeon's preferences changed with geography, as demonstrated by different choices of surgeons from North America compared to others worldwide. Hence, showing common practices in ACLR are less correlated with scientific evidence.
Hoewever, in a survey conducted by Duquin et al., 2 amongst members of the American Orthopaedic Society for Sports Medicine, it was found that the preferred graft for ACLR was BPTB autograft (46%) followed by hamstring tendon (32%) and allografts (22%). They noticed that arthroscopic single incision ACLR using BPTB autograft and interference screws as a fixation device was preferred by most of the members.
Mahnik et al.3 conducted a survey amongst the 39 doctors of Croatia Orthopaedic and Traumatology Society regarding current ACLR practices. Results of the questionnaire showed that 95% participants used hamstring tendon autograft for ACLR, while 5% used BPTB. The accessory anteromedial arthroscopic portal was preferred by 67% doctors, while 33% used trans-tibial approach. Regarding fixation methods at the femoral site, 62% used suspensory fixation methods, followed by cross pins (33%) and bio screw (5%). At the tibial site, almost all surgeons used a bio-absorbable screw (97%). Most of the surgeons (43.59%) used functional braces and 23.08% used knee immobilisers postoperatively, while 17.95% did not prefer any postoperative brace. Full weight bearing walk was advised at 6 weeks postoperatively by 38.46% surgeons. At 3 weeks postoperatively, it was advised by 33.34% and immediate postoperatively by 25.64% of surgeons, while 2.56% allowed full weight bearing after two months.
McRae et al.4 studied various opinions of 283 Canadian Orthopaedic Association members regarding ACLR practice. The author found that 73% preferred hamstring autograft. For the preparation of the femoral tunnel, 70% preferred trans-tibial approach, while 28% preferred transportal approach through the anteromedial portal. Immediately after surgery, full weight bearing was started by 72% and range of motion by 75% of the surgeons. Tunnel widening was the most common complication found in this study. Most of the surgeons also advised earlier resumption of sports activities.
Mail survey conducted by Sandhu et al., 5 amongst the members of Indian Arthroscopy Society and Indian Association of Sports Medicine, showed (50%) that surgeons performed ACLR after 3–6 weeks of injury. Single incision technique was used by 62.5%, while two incision techniques were used by 29.2% of surgeons. Hamstring tendon graft and BPTB graft were preferred by 40.7% and 35.6% surgeons, respectively. Regarding implant choice, 50% used a bio-absorbable screw and 25.5% used interference screw. Use of postoperative brace was denied by 62.3% of surgeons.
5. Number of ACLR performed per year
Mahnik et al.3 in their study found that 75% of the respondent members of Croatian Orthopaedics and Traumatology Association performed <50 ACLR per year. Most of the surgeries are done by a young surgeon with experience of fewer than ten years in ACLR. In our study, 46% of surgeons performed more than 50 ACLR per year, while 54% performed <50 ACLR per year. We noticed from our survey that the surgeons with higher experience and volume had been using double bundle ACLR, vis-à-vis the surgeons with lesser experience.
6. Preoperative MRI
Preoperative confirmation of ACL tear is very important and is done by radiological methods, particularly MRI. MRI is considered to be an investigation of choice for assessing ACL morphology.6, 7 In our study, out of 48 participants, 44 (91.7%) had preferred to have preoperative MRI. We believe that a confirmatory diagnosis of ACL tear by MRI preoperatively is justified to avoid the surprises during the surgery. Furthermore, MRI can pick up associated meniscal, articular cartilage and other lesions, which may require addressal during the ACLR surgery.
7. Anaesthesia
ACLR can be performed under GA or SA or spinal combined with epidural analgesia. The choice of anaesthesia in ACLR is either patient's or surgeon's preference dependent. Various studies showed that SA gives good and long-lasting pain control than GA in common orthopaedic procedures.8, 9 Macdonald et al.10 found that patients with double bundle ACLR have more pain than single bundle reconstruction. They also found that SA recipients had less pain in the acute postoperative period than those who received GA. The patients of double bundle ACLR who received SA had significantly less pain for first 14 postoperative days than those who received GA. The data from National Survey of Ambulatory Surgery showed that between 1994 and 2006, use of regional anaesthesia for ACLR increased (0.7–30.8%) with or without concomitant GA, while use of GA decreased.11 Our study results showed parallel observations to the above studies. Regional anaesthesia was preferred by 83.33% and GA by 16.7% of surgeons.
8. Tourniquet
During ACLR, instead of the tourniquet, a mixture of adrenaline and morphine can be used without any disturbance in vision and operation time. Also, it will prevent tourniquet-associated immediate postoperative pain and haemarthrosis.12 Some studies showed that the arthroscopic ACLR can be carried out effectively without the use of tourniquet and use of tourniquet does not add any extra benefit when compared with non-tourniquet arthroscopic knee surgeries.13, 14 In our study, majority (97.9%) use tourniquet during the surgery out of which 6.3% does not advise it during graft harvest.
9. Timing
Timing of ACLR after injury is an important factor in terms of postoperative clinical outcome. An ACLR before 3 weeks is reported to be associated with arthrofibrosis, and prolong rehabilitation,15 while delayed ACLR of more than one year is associated with osteoarthritis, cartilage defects and meniscal injuries.16 Collins et al.17 found that 86% of ACLR were done within six months, and 94% of ACLR were done within one year of injury. In our study, majority of the surgeons (47.9%) were doing ACLR between 3 and 6 weeks after injury followed by those who prefer after 6 weeks (29.2%) and below 3 weeks (22.9%). Thus, most of the surgeons consider a safe period of 3 weeks to 1 year for performing an ACLR.
10. Graft
For ACLR, various grafts are used, including commonly used autografts like Hamstring and BPTB grafts. Other used grafts are allografts and synthetic grafts. There does not seem to be a clear consensus over the best graft material so far.18 Various types of grafts have their pros and cons, and graft is often selected on the basis of their advantage and disadvantages in a particular patient. A BPTB graft is considered to be the “gold standard” graft because of its good patient's satisfaction and clinical results in long term follow-up.19 It has bone blocks on either side of the tendon that allows rapid healing and integration within tunnels.20 Good strength, consistency and ease of harvest are the main advantages of BPTB. Problems with BPTB graft are patellar tendon rupture, anterior knee pain, difficulty in kneeling, patellar/tibial fracture and quadriceps weakness.21 Hamstring tendon graft is now the most commonly used autograft for ACLR. Semitendinosus tendon at its tibial insertion site, with or without gracilis tendon, is harvested. This tendon is folded to increase the thickness and thus strength of the graft. Also, various suspensory methods of fixation, like endobutton, transfix can be used effectively with Hamstring graft. Load failure for hamstring graft is 2422 N, while for BPTB graft, it is 1785 N, which indicate its stiffness and strong construct.22 The problems with Hamstring graft include reduced strength of knee flexion and tibial rotation. A rare possibility of sciatic or saphenous nerve injury is there that resolves with time. Allografts are rarely used, and synthetic graft needs further evaluation. In our survey, 100% of the surgeons preferred autograft. Hamstring preference was shown by 83.3% of surgeons followed by BPTB (14.6%) and both BPTB/Hamstring (2.1%), which were consistent with most of the recent published studies (Table 1).
11. Femoral tunnelling
The femoral tunnel can be created trans-tibial (through the tibial tunnel) or transportal (through anteromedial arthroscopic portal). Transportal assesses of femoral tunnel preparation help in anatomical placement of tunnel location and hence improve the position of both femoral and tibial tunnel compared with trans-tibial route.23 Transportal assesses give good postoperative clinical knee score, good anteroposterior and knee rotational stability and help in rapid recovery.24 Most of the participants in our study preferred transportal (89.6%) route over trans-tibial (10.4%) route for the preparation of femoral tunnel, which is consistent with the findings of Chechik et al. and Mahnik et al.
12. Single versus double bundle
Double bundle ACLR restores normal anatomy better than that of single bundle ACLR. Some studies found no advantage of double bundle reconstruction over single bundle reconstruction in clinical outcomes. Further, double bundle reconstruction is more costly and time consuming.25 So recently, “Anatomical” or “Footprint” ACLR technique is most widely used due to its biomechanical advantages over non-anatomical construction.26 In our study, most of the participants (83.3%) preferred single bundle ACLR, which goes parallel with the findings of Chechik et al. Double bundle reconstruction was preferred by 10.4%, while both techniques were used by 6.3% of participants and these were mostly more experienced arthroscopic surgeons.
13. ACL remnant preservation
Native ACL remnants have mechanoreceptors, which contribute to proprioception and joint position sense,27 and hence, preserving ACL remnants, while ACLR helps to retain these functions. Mechanoreceptors, particularly at the tibial side of ACL remnant, do not go under degeneration and atrophy within one year, and hence, remnant preservation during ACLR preserves proprioceptive functions.28 Recent studies have shown that ACL remnant preservation during ACLR showed improved knee stability, side-to-side laxity and return to sports.29 ACL remnant preservation was also done by the majority of surgeons (91.7%) in our study.
14. Fixation device (implant)
In ACLR, graft within the bone tunnel (femoral or tibial) is secured with the fixation device or implant that helps in proper healing and fixation of the graft into the tunnel. The suspensory method of fixation like endobutton or transfix are methods of choice at femoral fixation site, while interference screw followed by intrafix are the method of choice for tibial side fixation. In our study, preferred implant at femoral side was suspensory method (93.75%) followed by aperture fixation method (4.2%), while at tibial side, fixation preferred method was interference screw (95.83%), either bio or metal screw.
15. Bracing
Postoperative use of knee brace is a controversial issue. Many studies showed that the post-ACLR brace application is useless, and the results of the group without the brace are slightly better.30, 31 Postoperative knee bracing has no beneficial effects on pain.32 In our study, we saw different types of postoperative bracing practices. Out of 48 members, 23 (47.9%) advised brace for <3 weeks, 15 (31.3%) for 3–6 weeks, 3 (6.3%) for >6 weeks and 7 (14.6%) did not advise any brace.
16. Postop weight bearing
Beynnon et al.33 studied comparison of accelerated versus non-accelerated rehabilitation. The author found that early weight bearing included in accelerated rehabilitation protocol has good compliance compared with the non-accelerated protocol. Kruse et al. found that immediate postoperative weight bearing is safe. Grant34 also found that immediate weight bearing after ACLR surgery, the range of motion of knee from 0° to 90° and strengthening with closed chain exercises were safe. Rick et al.35 found that postoperatively early weight bearing is beneficial and may have a role in decreasing patellofemoral pain. They also found the early motion to be safe and avoid chances of arthrofibrosis. In our study, 33 out of 48 (68.6%) surgeons allowed early weight bearing, i.e. before 3 weeks postoperatively, and 12 out of 48 (25%) allowed it after 3 weeks. Thus post-ACLR weight bearing practices of surgeons in our study go parallel with guidelines of recent literature.
17. Postoperative analgesia
As with any surgery, knee arthroscopy is also usually associated with postoperative pain. Postoperative pain following ACLR is associated with restriction of movements and thus affects early rehabilitation. Various modalities for postoperative pain control after ACLR are adopted. These include epidural analgesia, femoral nerve block and intra-articular analgesia. Dauri et al.36 concluded that epidural analgesia and continuous femoral block with combined ropivacaine and sufentanil has good analgesia control than an intra-articular infusion of the same drug combination. Intra-articular analgesia has good pain control than the extra-articular use of the same drugs.37, 38 The best combination for intra-articular analgesia is bupivacaine with opioids,39, 40 and amongst the opioids, morphine should be preferred. In our survey, we found diversity in methods of postoperative analgesia. Out of 48, only 13 surgeons used special measures for pain control.
This study has certain limitations, as only the registered members of DAS were included in the survey. But it is not known whether this population provides the true representation of current practices in managing ACL injuries in Delhi. Moreover, the response rate of the members was 80%, which is comparable to many other previous surveys performed in other nations. The results of this survey when compared to other studies show some variations in certain aspects of ACLR, as previously mentioned in the text.
Conflicts of interest
The authors have none to declare.
Acknowledgment
We are grateful to all the members of Delhi Arthroscopy Society for their willingness to participate in this survey.
References
- 1.Chechik O., Amar E., Khashan M. An international survey on anterior cruciate ligament reconstruction practices. Int Orthop. 2013;37(February (2)):201–206. doi: 10.1007/s00264-012-1611-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duquin T.R., Wind W.M., Fineberg M.S. Current trends in anterior cruciate ligament reconstruction. J Knee Surg. 2009;22(January (1)):7–12. doi: 10.1055/s-0030-1247719. [DOI] [PubMed] [Google Scholar]
- 3.Mahnik A., Mahnik S., Dimnjakovic D. Current practice variations in the management of anterior cruciate ligament injuries in Croatia. World J Orthop. 2013;4(October (4)):309–315. doi: 10.5312/wjo.v4.i4.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McRae S.M., Chahal J., Leiter J.R. Survey study of members of the Canadian Orthopaedic Association on the natural history and treatment of anterior cruciate ligament injury. Clin J Sports Med. 2011;21(May (3)):249–258. doi: 10.1097/JSM.0b013e318219a649. [DOI] [PubMed] [Google Scholar]
- 5.Sandhu J.S., Kaur D., Sarika Current practice variations in the management of anterior cruciate ligament injuries among the orthopaedic surgeons of India. J Orthop. 2008;5:e12. [Google Scholar]
- 6.Atik O.S., Cavusoglu A.T., Ayanoglu T. Is magnetic resonance imaging reliable for the evaluation of the ruptured or healed anterior cruciate ligament? Jt Dis Relat Surg. 2015;26(1):38–40. doi: 10.5606/ehc.2015.09. [DOI] [PubMed] [Google Scholar]
- 7.Naraghi A., White L.M. MR imaging of cruciate ligaments. Magn Reson Imaging Clin N Am. 2014;22(November (4)):557–580. doi: 10.1016/j.mric.2014.07.003. [DOI] [PubMed] [Google Scholar]
- 8.Jordan C., Davidovitch R.I., Walsh M. Spinal anesthesia mediates improved early function and pain relief following surgical repair of ankle fractures. J Bone Jt Surg Am. 2010;92:368–374. doi: 10.2106/JBJS.H.01852. [DOI] [PubMed] [Google Scholar]
- 9.Gonano C., Ursula L., Sitzwohl C. Spinal versus general anesthesia for orthopedic surgery: anesthesia drug and supply costs. Anesth Analg. 2006;102:524–529. doi: 10.1213/01.ane.0000194292.81614.c6. [DOI] [PubMed] [Google Scholar]
- 10.Macdonald Simon A., Mark Heard S. A comparison of pain scores and medication use in patients undergoing single-bundle or double-bundle anterior cruciate ligament reconstruction. Can J Surg. 2014;57(June (3)):E98–E104. doi: 10.1503/cjs.018612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buller L.T., Best M.J., Baraga M.G., Kaplan L.D. Trends in anterior cruciate ligament reconstruction in the United States. Orthop J Sports Med. 2015;3(January (1)) doi: 10.1177/2325967114563664. 2325967114563664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reda W., ElGuindy A.M., Zahry G. Anterior cruciate ligament reconstruction; is a tourniquet necessary? A randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2015:19. doi: 10.1007/s00167-015-3582-z. [DOI] [PubMed] [Google Scholar]
- 13.Wu H., Chen L.X., Li Y.L. Tourniquet used in anterior cruciate ligament reconstruction: a system review. Eur J Orthop Surg Traumatol. 2014;24(August (6)):999–1003. doi: 10.1007/s00590-013-1351-6. [DOI] [PubMed] [Google Scholar]
- 14.Nakayama H., Yoshiya S. The effect of tourniquet use on operative performance and early postoperative results of anatomic double-bundle anterior cruciate ligament reconstruction. J Orthop Sci. 2013;18(July (4)):586–591. doi: 10.1007/s00776-013-0405-2. [DOI] [PubMed] [Google Scholar]
- 15.Evans S., Shaginaw J., Bartolozzi A. ACL reconstruction – it's all about timing. Int J Sports Phys Ther. 2014;9(April (2)):268–273. [PMC free article] [PubMed] [Google Scholar]
- 16.Vaishya R., Mahana M., Vijay V. Treatment for acute anterior cruciate ligament tear: five-year outcome of randomised trial. BMJ. 2013;346:f232. doi: 10.1136/bmj.f232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Collins J.E., Katz J.N., Donnell-Fink L.A. Cumulative incidence of ACL reconstruction after ACL injury in adults: role of age, sex and race. Am J Sports Med. 2013;41(March (3)):544–549. doi: 10.1177/0363546512472042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaerf D.A., Pastides P.S., Sarraf K.M. Anterior cruciate ligament reconstruction best practice: a review of graft choice. World J Orthop. 2014;5(January (1)):23–29. doi: 10.5312/wjo.v5.i1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koh H.S., In Y., Kong C.G. Factors affecting patients’ graft choice in anterior cruciate ligament reconstruction. Clin Orthop Surg. 2010;2:69–75. doi: 10.4055/cios.2010.2.2.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Macaulay A.A., Perfetti D.C., Levine W.N. Anterior cruciate ligament graft choices. Sports Health. 2012;4:63–68. doi: 10.1177/1941738111409890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Allum R. Complications of arthroscopic reconstruction of the anterior cruciate ligament. J Bone Jt Surg Br. 2003;85:12–16. doi: 10.1302/0301-620x.85b1.13956. [DOI] [PubMed] [Google Scholar]
- 22.Dheerendra S.K., Khan W.S., Singhal R. Anterior cruciate ligament graft choices: a review of current concepts. Open Orthop J. 2012;6:281–286. doi: 10.2174/1874325001206010281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yau W.P., Fok A.W., Yee D.K. Tunnel positions in transportal versus trans-tibial anterior cruciate ligament reconstruction: a case-control magnetic resonance imaging study. Arthroscopy. 2013;29(June (6)):1047–1052. doi: 10.1016/j.arthro.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 24.Mandal A., Shaw R., Biswas D. Transportal versus trans-tibial drilling technique of creating a femoral tunnel in arthroscopic anterior cruciate ligament reconstruction using hamstring tendon autograft. J Indian Med Assoc. 2012;110(November (11)):773–775. [PubMed] [Google Scholar]
- 25.Stefani G., Mattiuzzo V., Prestini G. Single and double bundle ACL reconstruction: a prospective randomized study with mid-term (44 months) follow-up. J Bone Jt Surg Br. 2011;93–B(Supp. II):176. [Google Scholar]
- 26.Bedi A., Altchek D.W. The footprint anterior cruciate ligament technique: an anatomic approach to anterior cruciate ligament reconstruction. Arthroscopy. 2009;25(October (10)):1128–1138. doi: 10.1016/j.arthro.2009.03.008. [DOI] [PubMed] [Google Scholar]
- 27.Georgoulis A.D., Pappa L., Moebius U. The presence of proprioceptive mechanoreceptors in the remnants of the ruptured ACL as a possible source of re-innervations of the ACL autograft. Knee Surg Sports Traumatol Arthrosc. 2001;9(November (6)):364–368. doi: 10.1007/s001670100240. [DOI] [PubMed] [Google Scholar]
- 28.Sha L., Zhao L. Quantitative study on mechanoreceptors in tibial remnants of the ruptured anterior cruciate ligament in human knees. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2010;24(November (11)):1318–1322. [PubMed] [Google Scholar]
- 29.Takazawa Y., Ikeda H., Kawasaki T. ACL reconstruction preserving the ACL remnant achieves good clinical outcomes and can reduce subsequent graft rupture. Orthop J Sports Med. 2013;1(September (4)) doi: 10.1177/2325967113505076. 2325967113505076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mayr H.O., Stüeken P., Münch E.O. Brace or no brace after ACL graft? Four-year results of a prospective clinical trial. Knee Surg Sports Traumatol Arthrosc. 2014;22(May (5)):1156–1162. doi: 10.1007/s00167-013-2564-2. [DOI] [PubMed] [Google Scholar]
- 31.Kruse L.M., Gray B., Wright R.W. Rehabilitation after anterior cruciate ligament reconstruction – a systematic review. J Bone Jt Surg Am. 2012;94(October (19)):1737–1748. doi: 10.2106/JBJS.K.01246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hiemstra L.A., Heard S.M., Sasyniuk T.M. Knee immobilization for pain control after a hamstring tendon anterior cruciate ligament reconstruction: a randomized clinical trial. Am J Sports Med. 2009;37(January (1)):56–64. doi: 10.1177/0363546508322896. [DOI] [PubMed] [Google Scholar]
- 33.Beynnon B.D., Uh B.S., Johnson R.J. Rehabilitation after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind comparison of programs administered over two different time intervals. Am J Sports Med. 2005;33(March (3)):347–359. doi: 10.1177/0363546504268406. [DOI] [PubMed] [Google Scholar]
- 34.Grant J.A. Updating recommendations for rehabilitation after ACL reconstruction: a review. Clin J Sports Med. 2013;23(November (6)):501–502. doi: 10.1097/JSM.0000000000000044. [DOI] [PubMed] [Google Scholar]
- 35.Wright R.W., Preston E., Fleming B.C. ACL reconstruction rehabilitation: a systematic review part I. J Knee Surg. 2008;21(July (3)):217–224. doi: 10.1055/s-0030-1247822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dauri M., Polzoni M., Fabbi E. Comparison of epidural, continuous femoral block and intraarticular analgesia after anterior cruciate ligament reconstruction. Acta Anaesthesiol Scand. 2003;47(January (1)):20–25. doi: 10.1034/j.1399-6576.2003.470104.x. [DOI] [PubMed] [Google Scholar]
- 37.Akhondzade R., Pipelzade M.R., Gousheh M.R. Comparison of the analgesic effect of intra-articular and extra-articular injection of morphine and ketamine compound in arthrotomy lower limb surgery under spinal anesthesia. Pak J Med Sci. 2014;30(September (5)):942–945. doi: 10.12669/pjms.305.4775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sajedi P., Nemati M., Mosavi S.H. A randomized controlled trial for the effectiveness of intraarticular versus intravenous midazolam on pain after knee arthroscopy. J Res Med Sci. 2014;19(May (5)):439–444. [PMC free article] [PubMed] [Google Scholar]
- 39.Arti H., Arti S. The effects of intraarticular opioids in pain relief after arthroscopic meniscectomy: a randomized clinical trial study. Pak J Med Sci. 2013;29(April (2)):625–628. doi: 10.12669/pjms.292.2809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Imani F., Entezary S., Razi M. The effect of intra-articular meperidine and bupivacaine 0.5% on postoperative pain of arthroscopic knee surgery; a randomized double-blind clinical trial. Anesthesiol Pain Med. 2015;5(February (1)):e27470. doi: 10.5812/aapm.27470. [DOI] [PMC free article] [PubMed] [Google Scholar]