Abstract
Objectives
The study's aim is to calculate the parameters for retrograde insertion points for fixed superior pubic ramus fractures.
Methods
From the pubic symphysis, diameter and length of the screw were measured, as well as the angle between the screw axis and the 3 planes.
Results
When the diameter was fixed at 4.5 mm, the maximum lengths were 125 mm and 119 mm.
Conclusions
When the fracture occurs in Zone I, the penetration point could be selected in the pubic symphysis pubis angle to ensure that medial fracture fragments have sufficient screw channel length.
Keywords: Superior pubic ramus fractures, Percutaneous retrograde insertion, Safe zone
1. Introduction
Superior pubic ramus fractures are a common type of fracture in the pelvis. These fractures are often associated with pelvic ring damage. In aging populations, the number of low-energy trauma caused by elderly pubic branch fractures also tended to increase. Therefore, it is necessary to fix the superior pubic ramus.1 There are many negative aspects of classic open reduction and plate fixation, such as trauma, complications, and the length of time the patient is restricted to bed-rest. Percutaneous insertion of long screws into the anterior column has become an important component of orthopedic minimally invasive treatment of pelvic fractures.2 However, due to the selection of the needle insertion point, the needle angle, and the screw diameter, among other elements, a unified procedure has not been agreed upon. This limits the application of this technology, especially for inexperienced surgeons.
Several studies have indicated that there are many retrograde percutaneous insertion points. However, only some of them have been reported according to specific anatomic description.3 In this article, we chose the subpubic angle as the insertion point. From this point, we attempted to calculate the best screw angle and maximum screw diameter and length for fixation of fractures that occur in Zone I, as described by Nakatani.2
2. Materials and methods
We analyzed computed data from half hips of 40 adults (20 women and 20 men) who underwent scanning for a non-pelvic disorder. All CT scans were performed using 0.8-mm slice pelvic CT scanning (Siemens Sensation Open 40-slice CT scanner; Siemens, Erlangen, Germany). Scanning was performed from the anterior superior iliac spine to the lesser trochanter. Data from every case underwent processing as described below.
2.1. Simulating radiographs
The Mimics medical imaging software was used to analyze the computed tomography data and to export the pelvic three-dimensional model. Next, we generated four synchronized windows – axial, coronal, sagittal, and a 3D-model. Based on the Nakatani classification system, Zone I was defined as medial to the obturator foramen, while Zone III was defined as lateral to the obturator foramen. Zone II is located between Zones I and III (Fig. 1).
Fig. 1.

Nakatani system 3D imitation.
2.2. Virtual screw placement and position analysis
The pubic symphysis angle was selected as the insertion point, and simulation of insertion of virtual computer-aided design screws (diameter 2.0 mm) was performed, positioning the screw into the anterior column based on standard surgical techniques as described in the literature.4, 5, 6
The three-dimensional model pelvis underwent a 45° contralateral rotation, enabling us to obtain the Obturator oblique (Judet) toggle transparency treatment. The screw position axis was traced. The virtual screws in “0.1 mm” amplitude gradually increases in diameter until the virtual screws penetrate the pelvic cortex in each of the 4 windows of the pelvic outlet position and the pelvic inlet position as shown in Fig. 2 in Zone I and Zone II. The diameter was read as the maximum screw diameter. The screw length was measured from the insertion point to the Zone II lateral border, and this length was defined as Length 1. The diameter was adjusted to 4.5 mm, and the screw length was increased until it penetrated the pelvic cortex. This length was marked as the maximum length and labeled Length 2 (Fig. 2f). Because it has been shown that the mean screw length and the narrowest diameter have significant differences between men and women,7, 8 we decided to analyze the hip data for men and women separately.
Fig. 2.
The virtual screw and cortex-touching zone in different views: coronal plane (a and b), horizontal plane (c), sagittal plane (d), 3D model of Length 1 (e), diameter 4.5 mm screw of Length 2 (f).
2.3. Establishment of the pelvis coordinate system
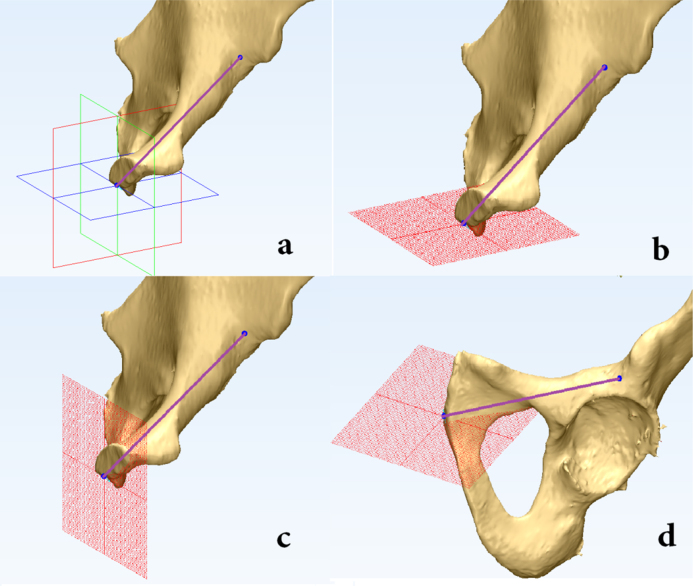
The front iliac spine and the upper pubic symphysis were set as the coordinate points, and the coronal plane was then established using those 3 points. We then chose the two anterior superior iliac spine points to create the horizontal plane through the 2 points and perpendicular to the coronal plane. The upper pubic symphysis was selected as a point through which the sagittal plane passed and was perpendicular to the coronal plane and horizontal plane. The pelvic coordinate system was used to measure the angle between the axis line and planes. All of these points are diagrammed and described in Fig. 3.
Fig. 3.
The pelvis coordinate system: (a), horizontal plane and screw axis (b), sagittal plane and screw axis (c), coronal plane and screw axis (d).
The data were analyzed using SPSS statistical software, comparing the index difference between men and women. We used an independent sample t-test and a paired sample t-test, with an α value of 0.05. p < 0.05 indicates significant difference.
3. Results
The virtual computer-aided design-generated average diameter of the screws is 7.9 ± 0.5 mm in males and 6.56 ± 0.34 mm in females. The minimum diameter is 6.3 mm in males and 5 mm in females. The average Length 1 of the virtual screws is 60.9 ± 2.9 mm in males and 73.7 ± 5.6 mm in females. The minimum Length 1 is 56. 5 mm in males and 65.2 mm in females. The average angle is shown in Table 1.
Table 1.
Summary of dates and statistical correlations.
| Male |
Female |
p value (sex) | |||
|---|---|---|---|---|---|
| Mean | Range | Mean | Range | ||
| Length 1 (mm) | 60.9 ± 2.9 | 56.5–67.5 | 73.7 ± 5.6 | 65.2–85.3 | |
| Length 2 (mm) | 125.3 ± 9.7 | 107.6–143.2 | 119.2 ± 11.7 | 91–134.3 | |
| Max-diameter (mm) | 7.9 ± 0.5 | 6.3–10.5 | 6.56 ± 0.34 | 5–7.5 | |
| Angle direction to the sagittal plane (°) | 50.8 ± 4.5 | 42.84–56.8 | 50.9 ± 3.2 | 46.64–56.43 | >0.05 |
| Angle projection to the coronal plane (°) | 7.8 ± 2.5 | 4.28–10.98 | 8.2 ± 2.2 | 5.06–11.16 | >0.05 |
| Angle projection to the horizontal plane (°) | 37.8 ± 5.1 | 29.23–45.87 | 37.6 ± 3.5 | 31.87–42.27 | >0.05 |
4. Discussion
Percutaneous insertion of screws has the following advantages in comparison with traditional treatment techniques: (1) less surgically invasive, effectively reducing the amount of bleeding, and increasing early rehabilitation; (2) simple to operate and can significantly shorten the operation time; (3) damage is avoided due to the ability to reveal and, around the pubis important nerves, blood vessels, or organs. However, there are some risks for percutaneous screw fixation with pubic fractures: (1) damage to the obturator vascular anastomosis or obturator neurovascular bundle may occur; (2) if the screw is too long, it may enter into the hip joint and damage the femoral head. These disadvantages could be attributed to a lack of understanding of proper trajectory and techniques for screw insertion. Before our study, a great number articles had been published describing the anterograde screw fixation of anterior column acetabular fractures, and this technique is always recommended because the operation is easy and typically causes relatively less damage. When the fracture occurs in Zone II or Zone III, anterograde screw fixation can meet the general requirements. When fractures occur along the Nakatani Zone II, more cross length and insertion points near the anterior acetabular rim, called Zone A as described in a pervious study, are required.3 However, when the fractures occur in Zone I, there may be a failure in fixation, due to a lack in screw length when using an anterograde screw. Thus, the retrograde screw fixation may represent a more proper technique. To enhance the fixed stability, we need to select larger diameter screws and twist the screw as deep as possible.
In the present study, we chose the subpubic angle as the insertion point to achieve enough length and relative maximum diameter across the fracture block in Zone I. We found that, unlike the current general understanding, there was no significant difference between men and women in the needle insertion angle from this point. As described in Table 1, the average diameter of the virtual screw was 7.9 mm in men, and 6.56 mm in women.
Based on these data and our clinical experience, we prefer to insert the screw in this way using a 7.3–6.5 mm diameter and 60–70 mm length for male patients and a 6.5–4.5 mm diameter and 70–80 mm length for female patients. An angle of approximately 50° and 8° between the axis and the sagittal plane and the coronal plane, respectively, was selected for both men and women in clinical practice because it is easy to achieve. We believe that selection of those angles from the subpubic angle is safe for both men and women.
4.1. Ideal screw position
There are several criteria for retrograde percutaneous screw fixation to achieve the ideal screw position. A good retrograde percutaneous screw should have sufficient length across fracture fragments and near the cortex zone. To achieve a higher fixation intensity and a low piercing rate, conventional surgery surgeons often use a multiple perspective approach. Different radiographs could help surgeons discover penetrating screws that appeared safe, and 3D fluoroscopy-based navigation have an outstanding low perforation rate.9 For example, the obturator oblique view can show the pubic branch bone cavity of the vertical wall, and the pelvic inlet view displays the anterior and posterior walls pubic branch canal (Fig. 4).
Fig. 4.
The virtual screw position in AP view (a), and lateral view (b), axial view (c), inlet view (d), outlet view (e), obturator oblique view (f).
Previous studies have indicated that the success rate is lower for pubic branch fractures that occur in Zones I and II compared with fractures in Zone III, with application of force in a fixed manner by a screw. Most failures from our clinic experiment were due to an imbalance in screw length and diameter. There is a consensus that only 3.5–4.5 mm screws should be used in the anterior column.10 Other data from a virtual three-dimensional reconstruction study also support this view.11 Thus, the cross fracture fragment length may be a key point and influenced our decision to use 4.5 mm as the diameter to measure the maximum length (Length 2).
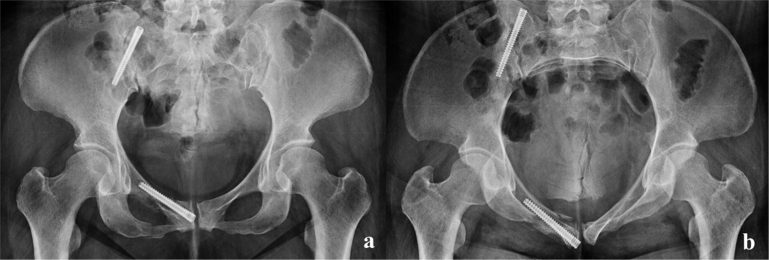
We found that when we selected the pubic symphysis angle as the insertion point, satisfactory screw length and diameter are easily achieved, and fractures that occurred in Zone I were fixed with more stability. However, the selection of these points caused an unacceptable piercing rate in several females. Because of this situation, we prefer to select the point that lies in the middle of the pubic symphysis on the coronal plane (Fig. 5). However, the length would decrease with an increase in the diameter of the screw. Thus, the data regarding females presented herein should be considered and referenced with caution.
Fig. 5.
In this female patient, we select starting points that occur on the upside of the pubic symphysis angle of the coronal plane and refer to this study to provide a date, finally, achieving a good operating result. The fix is stable, and the patient recovery time is acceptable. AP view (a), inlet view (b).
Although there are several interesting findings of the present study, we found that the pelvis anterior column is not a rule cylinder. Therefore, we believe that the “two tier” design principle guides determined by two single-line bony channels actually compromises the regional fracture fixation. For some patients with relatively good pelvic conditions, the guide is well suited. However, because it was not determined to be in accordance with a fixed fracture type, it is easy to simply account for the length but neglect the screw diameter.
Because of the shape constraints of the superior pubic ramus, the fact that the center of the osteotomy plane is not on the same axis, minimization of the osteotomy plane center axis as a guide method has several limitations.
When a cortical penetration screw is found, should it be replaced, or left as is?12 Replacement may decrease the strength of fixation. Once the screw has broken the cortex, removing the screw will lead to a bone defect. Further, there is no significant evidence indicating that replacement of the screw would increase the fixed stability in the upper pubic ramus fracture.
There are some limitations in our study. For example, we failed to establish a unified precise axis coordinate system. Therefore, the insertion positions of the vital screw are not very exact. We only used 4.5 mm-diameter screws to test the maximum length in hip 3-D structures. The pelvis coordinate system also lacks consideration of the influence of elderly pelvic bone hyperplasia, with points possibly selected on the osteophyma. Finally, only 40 individuals were used in our study, and it is difficult to cover all variations of bone morphological features in a sample of that size.
5. Conclusion
When the fracture occurs in Zone I, the penetration point could be selected in the subpubic angle to ensure medial fracture fragments have sufficient screw channel length. We have some tips for young surgeons. First, the Nakatani classification system should be used to determine fracture type. If the fracture is in Zone I, the retrograde method should be chosen to ensure that the medial fracture block has sufficient screw channel length to enhance fixation stability. Others have suggested an anterograde method for easy and safe operation. Second, the patients lay supine on the operating table under anesthesia. Third, a 2.0-mm diameter Kirschner insertion should be used at a pubic symphysis angle. Two of the three angles between the axis and the planes should be chosen to determine the direction of the screw. We suggest using the sagittal plane and coronal plane for easy operation. Fourth, obturator oblique, inlet view, and outlet view should be used to examine the screw cortex-nearing zones.
Conflicts of interest
The authors have none to declare.
References
- 1.Clement N.D., Court-Brown C.M. Elderly pelvic fractures: the incidence is increasing and patient demographics can be used to predict the outcome. Eur J Orthop Surg Traumatol. 2014;24:1431–1437. doi: 10.1007/s00590-014-1439-7. [DOI] [PubMed] [Google Scholar]
- 2.Starr A.J., Nakatani T., Reinert C.M., Cederberg K. Superior pubic ramus fractures fixed with percutaneous screws: what predicts fixation failure? J Orthop Trauma. 2008;22:81–87. doi: 10.1097/BOT.0b013e318162ab6e. [DOI] [PubMed] [Google Scholar]
- 3.Peng Y., Zhang L., Min W., Tang P. Comparison of anterograde versus retrograde percutaneous screw fixation of anterior column acetabular fractures. Int J Comput Assist Radiol Surg. 2015 doi: 10.1007/s11548-015-1308-9. [DOI] [PubMed] [Google Scholar]
- 4.Mouhsine E., Garofalo R., Borens O. Percutaneous retrograde screwing for stabilisation of acetabular fractures. Injury. 2005;36:1330–1336. doi: 10.1016/j.injury.2004.09.016. [DOI] [PubMed] [Google Scholar]
- 5.Puchwein P., Enninghorst N., Sisak K. Percutaneous fixation of acetabular fractures: computer-assisted determination of safe zones, angles and lengths for screw insertion. Arch Orthop Trauma Surg. 2012;132:805–811. doi: 10.1007/s00402-012-1486-7. [DOI] [PubMed] [Google Scholar]
- 6.Hiesterman T.G., Hill B.W., Cole P.A. Surgical technique: a percutaneous method of subcutaneous fixation for the anterior pelvic ring: the pelvic bridge. Clin Orthop Relat Res. 2012;470:2116–2123. doi: 10.1007/s11999-012-2341-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen H., Tang P., Yao Y., She F., Wang Y. Anatomical study of anterior column screw tunnels through virtual three-dimensional models of the pelvis. Eur J Orthop Surg Traumatol. 2015;25:105–110. doi: 10.1007/s00590-013-1410-z. [DOI] [PubMed] [Google Scholar]
- 8.Ochs B.G., Stuby F.M., Stoeckle U., Gonser C.E. Virtual mapping of 260 three-dimensional hemipelvises to analyse gender-specific differences in minimally invasive retrograde lag screw placement in the posterior acetabular column using the anterior pelvic and midsagittal plane as reference. BMC Musculoskelet Disord. 2015;16:240. doi: 10.1186/s12891-015-0697-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ochs B.G., Gonser C., Shiozawa T. Computer-assisted periacetabular screw placement: comparison of different fluoroscopy-based navigation procedures with conventional technique. Injury. 2010;41:1297–1305. doi: 10.1016/j.injury.2010.07.502. [DOI] [PubMed] [Google Scholar]
- 10.Routt M.L., Jr., Simonian P.T., Grujic L. The retrograde medullary superior pubic ramus screw for the treatment of anterior pelvic ring disruptions: a new technique. J Orthop Trauma. 1995;9:35–44. doi: 10.1097/00005131-199502000-00006. [DOI] [PubMed] [Google Scholar]
- 11.Attias N., Lindsey R.W., Starr A.J., Borer D., Bridges K., Hipp J.A. The use of a virtual three-dimensional model to evaluate the intraosseous space available for percutaneous screw fixation of acetabular fractures. J Bone Joint Surg [Br] 2005;87-B:1520–1523. doi: 10.1302/0301-620X.87B11.16614. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Y.Q., Chang S.M., Huang Y.G., Wang X. The femoral neck safe zone: a radiographic simulation study to prevent cortical perforation with multiple screw insertion. J Orthop Trauma. 2015;29:e178–e182. doi: 10.1097/BOT.0000000000000239. [DOI] [PubMed] [Google Scholar]