Abstract
This is a prospective hospital based study conducted in Soba University Hospital (SUH), Neonatal Intensive Care Unit (NICU) between January 2012 and January 2013, to determine the prevalence and risk factors of retinopathy of prematurity (ROP) among preterm babies admitted to Soba NICU and to assess the outcome of those babies. Ninety-two neonates with gestational age less than 34 weeks at birth were included in the study. Thirty-three of them were males and 59 were females. All of them were admitted to the NICU due to prematurity. Data was collected in a structured questionnaire. Thirty-four infants (37%) developed ROP in one or both eyes; 12 (35.3%) of them developed stage 3 and underwent laser therapy, 2 of them had aggressive posterior form, which was treated with Evastin injection. Seven (20.3%) neonates diagnosed as stage 2, and 13 (37.7%) had stage 1. Statistically, there were significant relationships between ROP and gestational age, birth weight (BW), oxygen therapy, sepsis, and blood transfusion (p=0.000). No significant relationship was found between the occurrence of ROP and sex of the baby, respiratory distress syndrome (RDS), hyperbilirubineamia, intraventricular haemorrage (IVH) and necrotizing enterocolitis (NEC), p >0.000 in all of them. The prevalence of ROP in this study was 37%. Low BW, low gestational age, oxygen therapy, and blood transfusion were all significant risk factors for ROP. ROP should be highlighted in Sudan, and screening program should be recommended for all premature babies.
Keywords: Intensive care, laser, Neonate, Prematurity, Retinopathy, Soba University Hospital, Sudan
Introduction
Retinopathy of prematurity [ROP], formerly known as retrolental fibroplasia because of its end stage appearance, is a developmental vascular proliferative disorder that affects the retina of preterm babies with incomplete retinal vascularization [1,2]. Next to cortical blindness, ROP is the most common cause of childhood blindness in the United States. Despite the advances in the management of retinal conditions, ROP remains a major cause of blindness in premature infants, and the incidence is increasing with increased survival of infants born at very early gestational age [3,4]. The condition typically begins at 34 weeks postmenstrual age, although it may be seen as early as 30 to 32 weeks. It affects a substantial number of premature infants worldwide, both the incidence and severity increase with decreasing gestational age and birth weight. Ocular outcome is poor in preterm infants with untreated severe ROP [5].
Materials and Methods
Study area and sample
This is a prospective hospital based study, which was conducted in Soba University Hospital NICU in one-year time (January 2012—January 2013). All preterm babies born in the hospital with gestational age less than 34 week, who were admitted to the NICU during the study period, were included. Follow up of the babies was conducted in referral clinics at SUH and Mecca Eye Complex Hospital.
Sample size calculation
Sample size: n= t2xp (1-p)/ m2
t= confidence level at 95 %(standard value of 1.96)
p= estimated prevalence of ROP
m= margin of error at 5 %(standard value of 0.05)
n=the total number of preterm babies involved in this study (required sample size) was 92.
Written approval was taken from Soba University Hospital and Mecca Eye Complex Hospital administration.
Statistical Analysis
The data was analyzed and the results were expressed in to figures, tables and graphs, Chi squared test was used to test the significant difference between the variables. Using the statically package for social science (SPSS), p value of ≤ o.oo5 is considered significant.
Results
The data were collected and analyzed from the records of 92 babies (Table 1). Fifty-one (64.1%) of the studied babies had gestational ages ranging from 32–34 weeks. 25 (27.2%) babies with gestational ages between 30 to less than 32 weeks. While 13 (14.1%) of the babies with GA of 28 - <30 weeks, only 3 (3.3%) babies had GA ≤28 weeks. Extreme low BW infants (≤1000 grams) were only 6 (6.5%) among the studied group. Very low BW (VLBW) (1000-≤ 1500 grams) were 47 infants (51.1%), while low BW (LBW) infants (1500 -≤ 2500 grams) were 42.3 %.
Table 1.
Birth weight in relation to retinopathy of prematurity
| Birth weight | ||||||||
|---|---|---|---|---|---|---|---|---|
| Diagnosis | ≤ 1000 gm | 1000 - ≤ 1500 gm | 1500 - ≤ 2000 gm | 2000 - ≤ 2500 gm | ||||
| N | % | N | % | N | % | N | % | |
| ROP | 2 | 33.3 | 27 | 57.4 | 5 | 14.3 | 0 | 0.0 |
| No ROP | 4 | 66.7 | 20 | 42.6 | 30 | 85.7 | 4 | 100.0 |
| Total | 6 | 100.0 | 47 | 100.0 | 35 | 100.0 | 4 | 100.0 |
ROP - Retinopathy of prematurity
Out of the 92 infants, 34 babies (37%) developed some form of ROP, 14 of them (41.1%) developed severe ROP of stage 3 that required laser therapy and intraocular Evastin injections. 7 babies developed stage 2 and just required follow up, while 13 babies developed stage 1 with spontaneous regression (Tables 2 &3).
Table 2.
Stages of retinopathy of prematurity among the study group
| Stages | No. of babies | Percentage |
|---|---|---|
| Stage 1 | 13 | 38.2 |
| Stage 2 | 7 | 20.6 |
| Stage 3 | 14 | 41.2 |
| Total | 34 | 100.0 |
Table 3.
Treatment models of ROP among the study group
| Stages | No. of babies | Percentage |
|---|---|---|
| Laser therapy | 12 | 35.3 |
| Intraocular Evastin injection | 2 | 5.9 |
| Spontaneous regression | 13 | 38.2 |
| Follow up | 7 | 20.6 |
| Total | 34 | 100.0 |
Thirty-two of the studied infants underwent eye check at 36 weeks of age, 27 between 37–40 weeks of age and only 12 of them underwent eye check between 31-34 weeks of gestation.
All the studied infants required oxygen therapy (100%). It was continuous in 63 (68.5%) infants, while it was interrupted in 29 (31.5%) infants (Table 4).
Table 4.
Days on oxygen therapy among the study group
| Days | No. of babies | Percentage |
|---|---|---|
| ≤ 5 | 45 | 48.9 |
| 5 - ≤ 10 | 17 | 18.5 |
| 10 - 20 | 29 | 31.5 |
| > 20 | 1 | 1.1 |
| Total | 92 | 100.0 |
Twenty-six of the studied babies received blood transfusion, 22(84.6%) of them developed ROP, while 4 (15.4%) of them were not affected. The difference was statistically significant.
Figure 1.
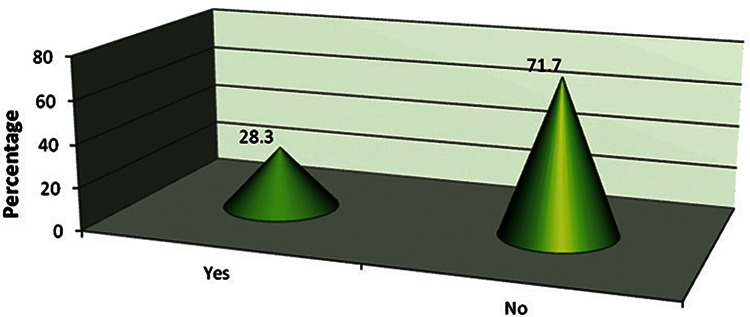
Blood transfusion among the study group
Discussion
This is the first conducted study in Sudan regarding ROP. Ninety-two infants with gestational age less than 34 weeks were studied regarding the prevalence, risk factors and outcome of ROP. The study showed strong association between the occurrence of ROP and the low gestational age. The results were similar to the ones obtained by M Abdulrahim at King Fahad Armed Forces in Jeddah, January 2007- October 2009 [6].
In our study, most of the studied babies had BW less than1500 grams, there is statically significance between LBW and the occurrence of ROP. Vivek B Wani et al in Kuwait obtained the same results, January 2001- August 2003 [7]. Although RDS represented the most common complication of prematurity, hence the use of oxygen for long time, yet there is no direct significance between ROP and RDS [8,9].
As revealed in our study, HAA in Egypt, January 2009-December 2010, obtained similar results that showed significant relation between ROP and blood transfusion [10].
Out of the 92 studied infants, 34 (37%) developed some form of ROP in one or both eyes. Of those, 14 (41.1%) were in stage 3 of the disease and 12 of them (35.3%) were treated with laser therapy. Two patients developed aggressive posterior form and were treated with intraocular Evastin injection; 7 babies (20.6%) were in stage 2, and 13 of the infants (38.2%) developed stage one with spontaneous regression [11].
Only 12 babies had eye examination done between 31-34 weeks of age, this is because there was no facilities available for ROP screening in the unit, and babies needed to go to Mecca Eye Complex Hospital after discharge
Conclusion
This is the first study regarding ROP in Sudan. The prevalence of ROP in SUH among preterm babies during January 2012 to January 2013 was 37%, which is significant and should be highlighted.. As early detection and management t is beneficial in avoidance of blindness, screening programs should be adopted in all neonatal care units.
Recommendations
Screening programs should be part of the management protocols of all neonatal care units.
Collaboration between neonatologist and ophthalmologist is needed to offer early management.
Raising the awareness among doctors regarding the magnitude of the problem is of a paramount importance.
References
- 1.American Academy of Pediatrics, Section on Ophthalmology; American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus. Screening examination of premature infants for retinopathy of prematurity. Pediatrics 2006; 117:572–6. [DOI] [PubMed] [Google Scholar]
- 2.Palmer EA, Flynn JT, Hardy RJ, Phelps DL, Phillips CL, Schaffer DB, et al. Incidence and early course of retinopathy of prematurity. The Cryotherapy for Retinopathy of Prematurity Cooperative Group. Ophthalmology 1991; 98:1628–40. [DOI] [PubMed] [Google Scholar]
- 3.Repka MX, Palmer EA, Tung B. Involution of retinopathy of prematurity. Cryotherapy for Retinopathy of Prematurity Cooperative Group. Arch Ophthalmol 2000; 118:645–9. [DOI] [PubMed] [Google Scholar]
- 4.Hussain N, Clive J, Bhandari V. Current incidence of retinopathy of prematurity, 1989–1997. Pediatrics 1999; 104:e26. [DOI] [PubMed] [Google Scholar]
- 5.Todd DA, Wright A, Smith J, NICUS Group. Severe retinopathy of prematurity in infants ≤30 weeks’ gestation in New South Wales and the Australian Capital Territory from 1992 to 2002. Arch Dis Child Fetal Neonatal Ed 2007; 92:F251–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rekha S, Battu RR. Retinopathy of prematurity incidence and risk factors. Indian Pediatr 1996; 33:999–1003. [PubMed] [Google Scholar]
- 7.Wani VB, Kumar N, Sabti K, Raizada S, Rashwan N, Shukkur MM, et al. Results of screening for retinopathy of prematurity in a large nursery in Kuwait: Incidence and risk factors. Indian J Ophthalmol 2010; 58:204–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shah VA, Yeo CL, Ling YL, Ho LY. Incidence, risk factors of retinopathy of prematurity among very low birth weight infants in Singapore. Ann Acad Med Singapore 2005; 34:169–78. [PubMed] [Google Scholar]
- 9.Seiberth V, Linderkamp O. Risk factors in retinopathy of prematurity. A multivariate statistical analysis. Ophthalmologica 2000; 214:131–5. [DOI] [PubMed] [Google Scholar]
- 10.Hakeem AH, Mohamed GB, Othman MF. Retinopathy of prematurity: a study of prevalence and risk factors. Middle East Afr J Ophthalmol 2012; 19:289–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Early Treatment For Retinopathy Of Prematurity Cooperative Group. Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol 2003; 121:1684–94. [DOI] [PubMed] [Google Scholar]


