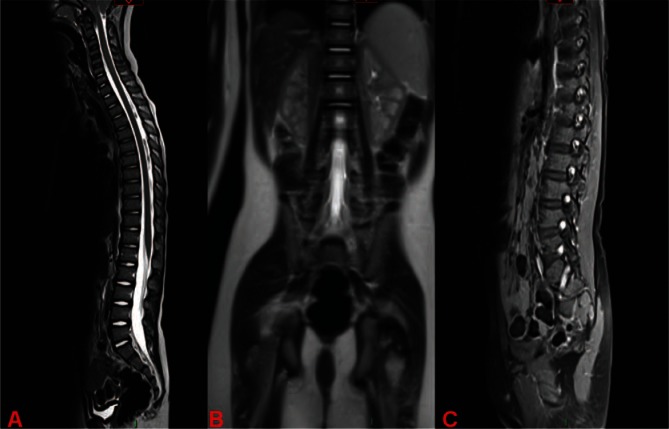
A previously well 3 ½-years-old boy presents with wide-based unsteady gait and frequent falls for the last few days. He has been miserable and complaining of ‘leg pains’. His parents say that he is now unable to stand and has not been able to sit up in bed unaided for one day. This presentation was preceded by a diarrheal illness 2 weeks ago. His spinal MRI with contrast is shown.
Figure 1.
Spinal MRI images.
What is the likely diagnosis (choose one)
Transverse myelitis
Acute poliomyelitis
Guillain–Barré syndrome
Discitis
Acute post-infectious cerebellitis
Extended answer is on next page.
Answer
c. Guillain–Barré syndrome.
These images demonstrate a normal spinal cord signal (image A: the spinal cord is seen uniformly black on T2 sequence with the surrounding cerebrospinal fluid (CSF) seen bright here). However, there is avid contrast enhancement (i.e. brightness) of the cauda equina (image B) and peripheral nerves as they are coming off the spine as shown in image C (see Figure 2 below). Appearances are suggestive of inflammatory radioclopathy and polyneuropathy, the whole marker of Guillain–Barré syndrome. Breakdown of the blood-spinal barrier is responsible for this contrast enhancement.
Figure 2.

Same T2-weighted spine MRI images as in figure 1. Left image shows cauda equina enhancement. Right image shows nerve roots enhancement as indicated by arrows.
Transverse myelitis is usually preceded by a viral infection in more than two-thirds of patients [1]. The presentation is with back pain, sphincter dysfunction, weakness and a level of sensory loss or numbness. Spinal MRI shows abnormal cord signals. An example is presented in Figure 3.
Paralytic poliomyelitis presents with painful muscle spasms followed by asymmetric proximal flaccid paralysis that is likely to affect the legs more than the arms. The weakness is not progressive (i.e. not ascending) beyond the acute febrile phase. The spinal cord is not normal on MRI and can show hyperintense lesions in the anterior horn regions with ventral nerve roots enhancement [1].
Discitis is an inflammation of the vertebral disk space often in relation to infection and is almost always associated with vertebral osteomyelitis. The presentation is with acute-onset back pain, refusal to walk, fever and localized tenderness.
Acute post-infectious cerebellitis presents with acute ataxia characterized by unsteady wide-based gait plus other cerebellar signs such as nystagmus. Deep tendon reflexes are preserved, and neither weakness nor pain is a feature. Brain MRI may be considered to rule out a posterior fossa tumor or acute demyelinating encephalomyelitis (ADEM).
Figure 3.

T2-weighted spinal MRI of a 4-year-old boy with longitudinally extensive transverse myelitis. Note the abnormal hyperintensity signal (bright areas) involving the entire spinal cord from the lower medulla down to the conus. This case is unusual in that transverse myelitis typically involves fewer segments.
Clinical Notes
Clinical presentation of Guillain–Barré syndrome (GBS) is with progressive motor weakness of more than one limb. Loss of ankle jerk and knee reflex is necessary for making the diagnosis. In children, the gait initially becomes unsteady and wide-based due to distal weakness. This can be confused with cerebellar ataxia. Pain is present in up to 80% [2]. Unfortunately, this may be mistaken for other conditions in young children such as ‘irritable hip’ or other orthopedic causes leading to a delay in the diagnosis.
Investigations
Cerebrospinal fluid (CSF): Shows high protein content with normal white cell count (in this patient it was 2.3 g/L!). Typically, this is seen after the first week from symptoms onset.
Nerve conduction studies: demonstrate a demyelinating or axonal pattern. These are usually not tolerated and difficult to interpret in children less than 5 years.
Spinal MRI: Although not always necessary, it is helpful where doubt exists about other diagnoses such as transverse myelitis, discitis, tumors or spinal cord infarction.
Treatment
- Immunotherapy:
- Intravenous immunoglobulins (IVIG): A recent Cochrane systematic review found moderately strong evidence that IVIG therapy speeds up recovery in children compared to supportive care. There is some low-quality evidence suggesting improvement in long-term disability [3]. The total dose is 2 g//kg divided over 2–5 days.
- Steroids: Another Cochrane review found no benefit from steroids treatment and a suggestion from one study that they may delay recovery [4].
- Pain control:
- Regular analgesia (e.g. paracetamol/ibuprofen)
- Neuropathy pain: Commonly used agents are gabapentin, carbamazepine, and amitriptyline, either solely or in combination.
Close monitoring for autonomic instability (blood pressure, respiratory status and cardiac dysrhythmias).
Early mobilization and physiotherapy (with proper pain control) are advised.
Patient Outcome
The patient was given IVIG over 5 days with remarkable improvement from a mobility perspective He also received combined gabapentin and amitriptyline to control neuropathic pain. These were subsequently weaned after 3 months. He responded well to physiotherapy. At 6 months follow-up he was almost back to his pre-morbid state and was ‘up and These were running’.
KEY LEARNING POINTS.
-
➢
Back and leg pain can be presenting features in Guillain–Barré syndrome.
-
➢
Spinal MRI with contrast, when obtained, typically demonstrates nerve root enhancement thus establishing the diagnosis especially when neurophysiologic studies are not feasible in very young children.
-
➢
Non-contrast MRI sequences are usually normal. Contrast must be given.
-
➢
Spinal MRI helps in ruling out other differential diagnoses thus guiding treatment.
-
➢
IVIG therapy is effective in speeding up recovery and improving long term disability.
-
➢
Use of regular analgesia and other agents is recommended to improve comfort and to allow early mobilization and physiotherapy.
References
- 1.Singhi P,Griffin DE, Newton C. Central Nervous System Infections in Childhood (International Child Neurology Association). 1st Ed Mac Keith Press, London, 2014. [Google Scholar]
- 2.Pentland B, Donald S. Pain in the Guillain Barre syndrome: a clinical review. Pain 1994; 59:159–64. [DOI] [PubMed] [Google Scholar]
- 3.Hughes RAC, Swan AV, van Doorn PA. Intravenous immunoglobulin for Guillain-Barré syndrome. Cochrane Database of Systematic Reviews 2014, Issue 9 Art. No.: CD002063 DOI: . [DOI] [PMC free article] [PubMed]
- 4.Hughes RAC, van Doorn PA. Corticosteroids for Guillain-Barré syndrome. Cochrane Database of Systematic Reviews 2012, Issue 8 Art. No.: CD001446 DOI: . [DOI] [PubMed]