Abstract
Neonatal respiratory distress (NRD) is a common neonatal problem, which is responsible for high morbidity and mortality. There are few published studies in developing countries addressing neonatal respiratory distress. There is no previously published study in Sudan on this problem. The objective of the study is to determine the frequency, different causes, immediate outcome. It was a prospective, descriptive, cross sectional hospital-based study which was carried out in neonatal intensive care unit (NICU) of Omdurman Maternity Hospital, between February-March 2013. The study enrolled all Sudanese newborns from 0-28 days including normal, low and high birth weight of different gestational ages admitted to the neonatal intensive care unit and diagnosed as neonatal respiratory distress. The frequency of NRD was calculated, the causes and immediate outcome were determined. Results showed that the frequency rate of NRD was (4.83%) among the total number of hospital (2071) live births during the period of the study. The commonest causes were transient tachypnoea of the newborn (TTN) in 28% of cases, sepsis in 24% of cases and hyaline membrane disease (HMD) in 15% of cases. The outcome of NRD was: cure in 56% of cases, death in 36% of cases, and patients discharged with complications in 8% of cases. In conclusion, the study confirmed the importance of NRD with a frequency rate of 4.83%, morbidity of 8% and mortality of 36% of cases. The causes and immediate outcome were determined and discussed. Some recommendations were suggested in order to reduce its frequency, morbidity and mortality.
Keywords: Neonate, Respiratory distress, Transient tachypnoea of newborn, Hyaline membrane disease, Neonatal sepsis
Introduction
Neonatal mortality accounts for 40% of deaths in children under five years of age [1]. Globally, there has been a considerable decline in under-five and infant mortality in the past decades. However, neonatal mortality remained relatively unchanged especially in developing countries [1].
Neonatal mortality is more observed in developing countries. The highest neonatal mortality rates are seen in sub Saharan Africa. In Asia the average rates are lower but this region accounts for over 60% of the estimated global total, mainly because of the large population and high fertility rate [2].
Efforts to achieve the UN Millennium Development Goal 4 of reducing childhood mortality by two-thirds by 2015 are focused on reducing neonatal deaths in high mortality countries [3].
The case fatality rate for neonatal respiratory distress in India is 30-40%. It was 19% in the Bondicherry study. Case fatality is highest for newborns with hyaline membrane disease (20-40% in developed countries and 50-75% in India). It ranges from 14.3% to 30-37% for meconium aspiration-related respiratory distress deaths [1].
Respiratory distress in newborn is manifested by tachypnoea (more than 60 breaths per minute), apnea, and retraction of respiratory muscles, reduced air exchange, nasal flaring, cyanosis, grunting, inspiratory stridor and feeding difficulties [4].
The incidence of neonatal respiratory distress (NRD) is ranging from 2.2% to 7.6% in developed countries and from 0.7% to 8.3% in India [1]. A study conducted in India in 1996 found that the incidence of NRD to be 7%.[1] Also Respiratory distress is observed in nearly 7% of newborns in Turkey in 2011 [5].
In Sudan there was no previous published data addressing the neonatal respiratory distress.
The objective of this study is to determine the frequency of respiratory distress, to study the causes and determine the immediate outcome in the biggest maternity hospital in Sudan
Patients And Methods
This study was a prospective, descriptive, cross sectional hospital-based study, carried out from February to March 2013. It included all newborns satisfying the inclusion criteria. The sample size was calculated according to the equation below:
N= Z2(PQ)/D2
Where: N= sample size, Z= statistical certainty (1.96 at 95% level of confidence), P= prevalence=7%=0.07, Q= probability of failure =1-P = 1 - 0.07= 0.93, D= desired margin of error= (0.05) or 5%
Therefore N=1.96 X 1.96X 7 X 93 /25 =100.
i.e. the sample size equals 100.
The study included all newborns from 0-28 days that had been admitted to NICU of Omdurman Maternity Hospital, which is considered as the biggest maternity hospital in the country, serving about 2.5 million population. The inclusion criteria are to enrol all Sudanese newborns from 0-28 days with low, normal or high birth weight of different gestational ages admitted into NICU, diagnosed as neonatal respiratory distress. The study excluded non Sudanese newborns and newborns whose parents refused to be admitted to the study. An ethical clearance was obtained from the concerned authorities; also a verbal consent was taken from the parents. Using an interviewer-administered questionnaire, data was collected for each patient including personal data, full perinatal history, maternal history, different risk factors for different causes and immediate outcome. The causes were determined for each patient and immediate outcome was cure, death or discharge with complications. More information, to use if needed, were taken from relevant neonatal admission files. Data was collected in two months time and was analyzed by statistician using SPSS.
Results
Among 2071 newborns delivered during the study period, 177 (8.6%) newborns were admitted to Neonatal Intensive Care Unit (NICU), 100 of them were due to neonatal respiratory distress (NRD). Therefore the calculated frequency rate of NRD was 4.83% among all newborn delivered. NRD constituted 56.5% of newborn admitted to NICU. The age of newborns with respiratory distress is 7 days and below in 98% of them, only 2% were of 8-14 days of age. Fifty four percent of them were males, with a male:female ratio of 1.2:1. Forty nine percent of babies were of different degrees of low birth weight, 48% of normal birth weight and only 3% of large birth weight. Thirty eight percent of them were preterm compared to 62% term babies (Table 1). Sixty one percent of those babies families were of low income, 38% of moderate income, and only 1% of families were of high income (according to World Bank Classification, 2011).
Table 1.
Demographic data of the newborns
Age (in days) |
1-7 |
8 – 14 |
15-28 |
Total (%) |
(%) |
(98) |
(2) |
(0) |
(100) |
Birth weight |
Low |
Normal |
Large |
|
(%) |
(49) |
(48) |
(3) |
(100) |
Gestational age |
Preterm |
Term |
Post term |
|
(%) |
(38) |
(62) |
(0) |
(100) |
Socioeconomic status |
Low |
Normal |
High |
|
(%) |
(61) |
(38) |
(1) |
(100) |
The most common cause of NRD was found to be transient tachypnoea of the newborn (TTN) in 28% of cases with case fatality rate (CFR) of zero percent, followed by sepsis in 24% of cases with CFR of 33.3%. While the least cause was inborn errors of metabolism in 1% with CFR of 100% (Table 2).
Table 2.
Frequency of causes of neonatal respiratory distress and their outcome
Immediate outcome |
Case fatality rate (%) |
Total |
|||
|---|---|---|---|---|---|
Cured (%) |
Discharged with complications (%) |
Died |
|||
Transient tachypnea of newborn |
28 (100) |
0 (0) |
0 |
0 |
28 |
Sepsis |
16 (66.7) |
0 (0) |
8 |
33.3 |
24 |
Hyaline membrane disease |
2 (13.3) |
0 (0) |
13 |
86.7 |
15 |
Congenital heart disease |
0 (0) |
4(44.4) |
5 |
55.6 |
9 |
Meconium aspiration syndrome |
3 (50) |
1 (16.7) |
2 |
33.3 |
6 |
Hydrocephalus |
0 (0) |
2 (40.0) |
3 |
60 |
5 |
Congenital choanal atresia |
0 (0) |
1 (33.3) |
2 |
66.7 |
3 |
Congenital diaphragmatic hernia |
0 (0) |
0 (0) |
2 |
100 |
2 |
Hypoglycemia |
5(100) |
0 (0) |
0 |
0 |
5 |
Metabolic. causes |
0 (0) |
0 (0) |
1 |
100 |
1 |
Hypocalcemia |
2(100) |
0 (0) |
0 |
0 |
2 |
Total |
56 (56) |
8 (8) |
36 |
36 |
100 |
The overall immediate outcome of neonatal respiratory distress was a cure in 56% of cases, death in 36% of cases, and cases discharged with complications were 8% of the cases (Figure 1).
Figure 1.
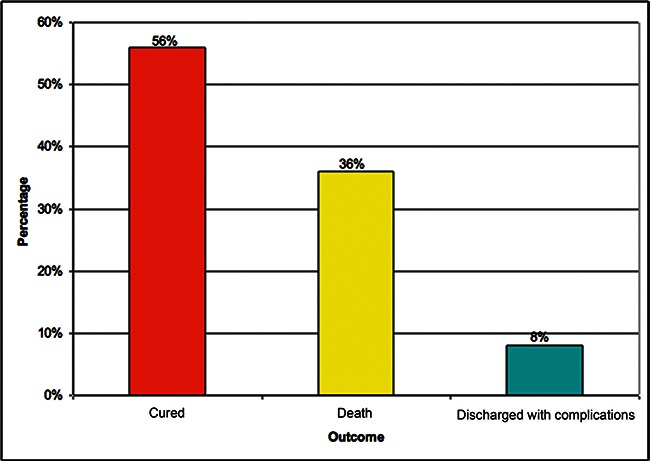
Frequency of immediate outcome
Discussion
The frequency of neonatal respiratory distress (NRD) is found to be 4.83%, while the incidence rate in developing countries such as in India is (0.7 to 8.3%). It is lower than the prevalence in Bondcherry study (7%) [1] and in the Turkish study of 7% [5]. Italian study showed an incidence of 2.2% [6]. Switzerland study showed that the incidence of NRD in infants admitted to neonatal units was doubled over the last thirty years from 1.9% to 3.8% of the whole neonatal population and from 30% to 53% of all infants admitted to neonatal unit [7]. The proportion of neonates with the NRD who are admitted to the neonatal unit (53%) is similar to the proportion in this study (56.5%), but is higher than in China (Qians) study (20.5%) [8].
In this study, 61% of the mothers are of low socioeconomic status, 38% of newborns are premature and also 49% of them are of low birth weight. These factors together with others lead to increase risk of developing NRD and hence increase its frequency (Table 1). TTN was found as common cause of NRD may be due to fact that most of the newborns are term babies (Table 2). TTN accounts for large proportion in contradistinction to other Indian study [9], which showed that pneumonia accounted for 68.6% of causes and was considered the commonest cause of NRD. Comparison between the causes and their fatalities in this study with other studies showed that Italian [6] and Qian’s [8] studies have less frequencies and case fatality rates than the Indian [10] and our study (Table 3). It is expected to find such result because the facilities, the good care, and the prompt management of labour and newborns in the developed countries is far advanced than in the developing ones. However, Qian’s and Italian studies show some fatalities in cases of transient tachypnoea of the newborns which was not reported in this study.
Table 3.
Comparison between common causes and fatality of neonatal respiratory distress in our study with other studies.
Cause |
TTN |
Sepsis |
HMD |
MAS |
||||
|---|---|---|---|---|---|---|---|---|
F% |
CFR (%) |
F% |
CFR (%) |
F% |
CFR (%) |
F% |
CFR (%) |
|
The present study |
28 |
0 |
24 |
33.3 |
15 |
86.7 |
6 |
33.3 |
Indian study [10] |
42.7* |
- |
17 |
- |
9.3 |
57.1 |
10.7* |
21.8 |
Italian study [6] |
0.93 |
1.3* |
0.07 |
21.7 |
1.16 |
24 |
0.06 |
10.3 |
Qian’s study [8] |
1.83 |
5* |
- |
- |
5.44 |
31.4 |
3.13 |
17.8 |
CFR - Case fatality rate, F - Frequency, HMD - Hyaline newborn disease, MAS - Meconium aspiration syndrome, TTN - Transient tachypnoea of the newborn.
These figures are higher than those in our study.
Another Sudanese study, showed that meconium aspiration syndrome (MAS) occurred in only 0.85% of cases with CFR of 8.7%, which is very much lower than this study [11]. In both studies mortality is much higher if compared with other results in literature, where one study showed that MAS was responsible for 1.4% of all neonatal intensive care unit admission with CFR of 2.8% [12]. Qian’s study, showed that among total nursery admission, 4.51% had pulmonary infection with 13.6% CFR [8]. This cause per se was not apparent in this study, but probably included in the cases of neonatal sepsis with CFR of 33.3%.
The results indicate that NRD is a common neonatal problem among admitted newborns to NICU accounting for 58.5% of total admission. HMD, neonatal sepsis and MAS in this study contributed largely to mortality. These causes are to some extend preventable and treatable; therefore, their morbidity and mortality can be reduced. The immediate outcome of NRD is cure in 56%, patients discharged with complications are 8% and death occurred in 36% of cases (Figure 1). Many efforts are needed to improve the morbidity and mortality rates. The high fatality rate can be explained by inadequate antenatal care, less use of steroid in prematurity antenataly, less meticulous management of high risk pregnancies beside unavailability of synthetic surfactant and mechanical ventilation. Improving facilities and prompt management of high risk pregnancies, labour and affected newborns will definitely reduce the frequency, morbidity and mortality of NRD.
Conclusion
Neonatal respiratory distress has been found to be a common neonatal problem with considerable neonatal morbidity and mortality. Its frequency rate was 4.83% among the total number of hospital deliveries. The commonest causes of neonatal respiratory distress were TTN in 28% of cases, followed by sepsis in 24%, then HMD in 15%.
The outcome of neonatal respiratory distress was found as: a cure rate of 56%, mortality rate of 36% and patients discharged with complications (morbidity rate) in 8%.
Recommendations
For reduction of the frequency, morbidity and mortality of NRD, the following are recommended:
Good antenatal care with good attention of high risk pregnancies and good monitoring with partogram and cardiotocography (CTG) during labour.
Antenatal maternal use of steroids in prematurity and prophylactic use of antibiotics in premature rupture of membranes (PROM).
Prompt management of neonatal respiratory distress, including availability of equipped NICU with ventilator and surfactant facilities.
Acknowledgement
The authors would like to acknowledge all the nursery staff of Omdurman Maternity Hospital for their help. We are also thankful to the parents of the newborns for allowing us to carry out this study on their children.
References
- 1.Kumar A, Bhat BV. Epidemiology of respiratory distress of newborns. Indian J Pediatr. 1996; 63:93–8. [DOI] [PubMed] [Google Scholar]
- 2.Ayaz A, Saleem S. Neonatal mortality and prevalence of practices for newborn care in Squatter Settlement of Karachi, Pakistan. PLOS ONE, 2010; 5(11):e13783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jehan I, Harris H, Salat S, Zeb A. Neonatal mortality, risk factors and causes, Bulletin of the World Health Organization 2009; 87:130–138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Martin R, Saker F. Overview of neonatal respiratory distress, Up to date. Available at: http://www.uptodate.com/contents/overview-of-neonatal-respiratory-distress-disorders-of-transition Accessed on 25May, 2014.
- 5.Fedakar A, Aydoğdu C. Clinical Features of neonates treated in the intensive Care Unit for Respiratory distress. Turk J Ped 2011; 53:173–179. [PubMed] [Google Scholar]
- 6.Rubaltelli FF, Dani C, Reali MF, Bertini G, Wiechmann L, Tangucci M, Spagnolo A. Acute neonatal respiratory distress in Italy. Acta Paediatr 1998; 87:1261–1268. [DOI] [PubMed] [Google Scholar]
- 7.Ersch J, Roth-Kleiner M, Baeckert P, Bucher HU. Increasing incidence of respiratory distress in neonates. Acta Paediatr 2007; 96:1577–81. [DOI] [PubMed] [Google Scholar]
- 8.Qian LL, Liu CQ, Guo YX, Jiang YJ. Current status of neonatal acute respiratory disorders. Chin Med J (Engl) 2010; 123:2769–75. [PubMed] [Google Scholar]
- 9.Mathur NB, Maulana A. Neonatal respiratory distress with special reference with pneumonia. Indian Ped 2002; 39:529–537. [PubMed] [Google Scholar]
- 10.Kumar A, Bhat Bv. Respiratory distress in newborn. Indian J Matern child Health. 1996; 7:8–10. [PubMed] [Google Scholar]
- 11.Mohammed RA. Meconium aspiration syndrome incidence, risk factors and immediate outcome in maternity hospital. MD thesis 2013, SMSB, Khartoum. [Google Scholar]
- 12.Espinheira MC, Grilo M, Rocha G, Guedes B, Guimaraes H. Meconium aspiration syndrome - the experience of a tertiary center. Rev Port Pneumol 2011; 17:71–6. [PubMed] [Google Scholar]


