Abstract
Accidents still represent a major cause of death and disability in children. The resultant traumatic brain injury (TBI) usually needs a multidisciplinary approach of management. Although computed tomographic (CT) head scan is generally a preferred investigation in TBI, however, clear guidelines are required to help decision making by different team members on “when a head CT scan is needed”, its limitations, and “when it is likely to be informative”. The answers to these queries are highlighted, in the present article, with other aspects of treatment of children with TBI. This article discusses different worldwide-accepted approaches for managing children with TBI, and places special emphasis on the issue of “indications for a head CT scan”.
Keywords: CT scan, Multidisciplinary team, Saudi Arabia, Traumatic brain injury
Background
Traumatic Brain Injury (TBI) occurs after an insult to the brain from an external mechanical force that is traumatic in aetiology. This non degenerative, non congenital insult may lead to permanent or temporary impairment of cognitive, physical and psychosocial functions, with an associated diminished or altered state of consciousness [1]. Traumatic brain injury is a leading cause of death and disability in children worldwide. In the United States (US), head trauma in individuals aged 18 years and younger results in about 7400 deaths, over 60,000 hospital admissions, and over 600,000 emergency department visits every year [2,3].
The approach to TBI management may differ from one institute to another according to physicians’ experience and availability of investigation tools. Therefore, the need to unify the clinical approach and the decision of further investigation is warranted. This will waive great challenges from the treating physician, insure consistency in clinical practice, and minimize errors. In fact, maltreatment of patients with TBI may lead to unsatisfactory or even harmful outcomes, which furthermore stresses upon the necessity to pursue a standardized approach for TBI management.
In this article we will try to elaborate on some practical approaches that are widely used in different institutes worldwide, focusing mainly upon the use of head CT scan in children with TBI. We used one of the patients who presented to the Emergency Department (ED) of King Khalid University Hospital (KKUH) in February 2014 as an index case to highlight some areas of potential discrepancies in clinical practice management of children with TBI.
A Tragic Tale
A Saudi family that consists of four members (the father, mother and 2 children) was on the way to attend an outpatient clinic appointment for one of the children. A high-speeding vehicle crashed their car from behind, after which the father (driver) died on the spot. The mother (sitting in the back seat) had multiple fractures and one of the children (our index case, who was sitting in the front seat with unfastened seatbelt) had a severe head trauma. The second child only had few lacerations and he was well at the time of presentation. All of the family members were rushed to KKUH by the help of paramedics.
Care of The Index Case
On arrival to ED, the child was on a spinal board and had a cervical collar applied. On examination, his pulse was weak but regular. He had a heart rate of 104/min, respiratory rate of 18/min, and oxygen saturation of 83% in room air. His Glasgow coma scale (GCS) was 12/15, but it rapidly deteriorated to 10/15 after 20 minutes of admission. He was electively intubated and ventilated. He received 5 boluses of normal saline and a whole blood transfusion. He also required norepinephrine, dopamine and 3% normal saline infusions. Primary and secondary surveys were conducted, which revealed: frontal hematoma, right frontal bone fracture, and lacerations. Both pupils were non-reactive and 2 mm of size. He had normal ear and nose examination. Chest examination showed no deformities, symmetrical movements, and equal air entry bilaterally. His capillary refill time was 3 seconds with cold extremities and weak pulses. His heart sounds were normal. The abdomen was neither distended nor tender to palpation and showed no signs of intra-abdominal bleeding. Back and limbs examinations were unremarkable.
In addition, urgent CT head was performed and it showed a severely comminuted depressed fracture of the right frontal bone extending to orbital roof with an associated frontal scalp hematoma and multiple air pockets (Figure 1A and B). Petechial, tiny hemorrhagic foci in the right frontal lobe were evident on the brain window images as well as subdural hematoma which was evident as the hyper density of the inter hemispheric fissure anteriorly (Figure 2A and B).
Figure 1.
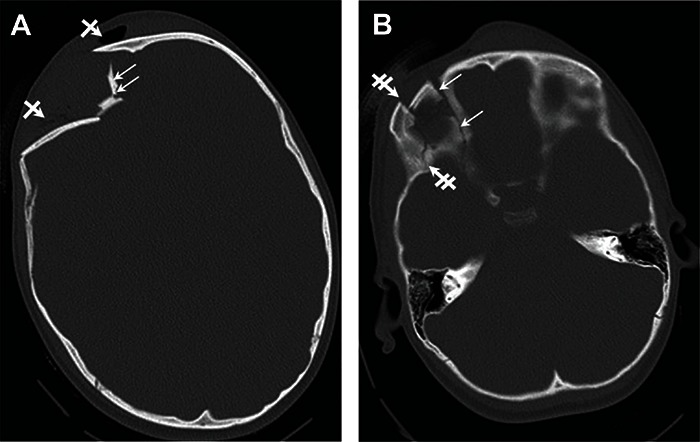
(A) Comminuted depressed fracture of the right frontal bone (small arrows) with scalp hematoma and multiple air pockets seen within it (cross arrows). (B) Fracture extending to orbital roof (small arrows medial aspect and double cross arrows on lateral aspect).
Figure 2.
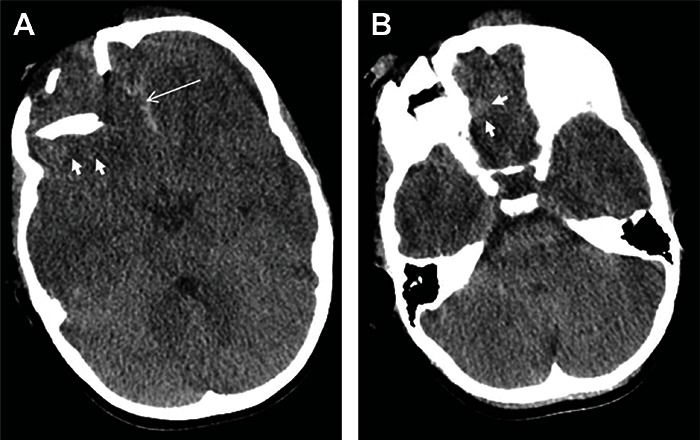
(A and B) - Brain window images showing petechial (tiny) cerebral hemorrhagic foci in the frontal lobe (small white arrows) and subdural hematoma (long arrow in 2A).
A multidisciplinary team approach was taken in the management of our patient. Neurosurgeons operated on him after stabilization by the Pediatric Intensive Care Unit (PICU) team. The child also needed exploratory laparotomy, done by the Pediatric surgeons, because of a query of collection of fluid/blood in the intra-abdominal cavity. The patient remained hospitalized for further management and observation for one month, after which he was discharged in a good condition with follow up appointments in the Neurosurgery and Pediatric clinics. Fortunately, there was no disagreement between different team members in the management approach. Both of, the need for a head CT scan for this child, and the interpretation of findings were straightforward; hence a good outcome has been achieved. Yet, in many similar scenarios, the necessity for CT and the treatment approaches may be arguable. Also, the interpretation of CT scan, and the accuracy in concluding absence of evident brain injuries may be challenging. Thus, identifying a robust system to approach children with TBI would surely reduce the chance of discrepancies in treatment plans between team members and provide an evidence-based management plan that is likely to improve the ultimate outcome.
Indications for a head CT scan (Practical approaches in TBI management)
Four different internationally-agreed and widely used approaches will be discussed in this section. These include:
(1) Pediatric Emergency Care Applied Research Network (PECARN) approach [4] - (Table 1): PECARN conducted a prospective cohort study to identify children at very low risk of clinically-important traumatic brain injuries (ciTBI) for whom CT might be unnecessary. The study included 42,412 children who were enrolled from 25 US hospitals, with around 25% of patients less than 2 years of age. The study’s prediction rule to identify children at very low risk of ciTBI showed a sensitivity of 100% and a 100% negative predictive value (NPV) for ciTBI in children younger than 2 years; while for children aged 2 years and older it showed a sensitivity of 96.8% and a 99.95% NPV for ciTBI. Two patients were missed by the PECARN prediction rule and neither of them required neurosurgery.
Table 1.
Suggested algorithm for a need for CT head in children with TBI, (A) younger than 2 years, and (B) for those aged 2 years and older, with GCS scores of 14–15 [4]*
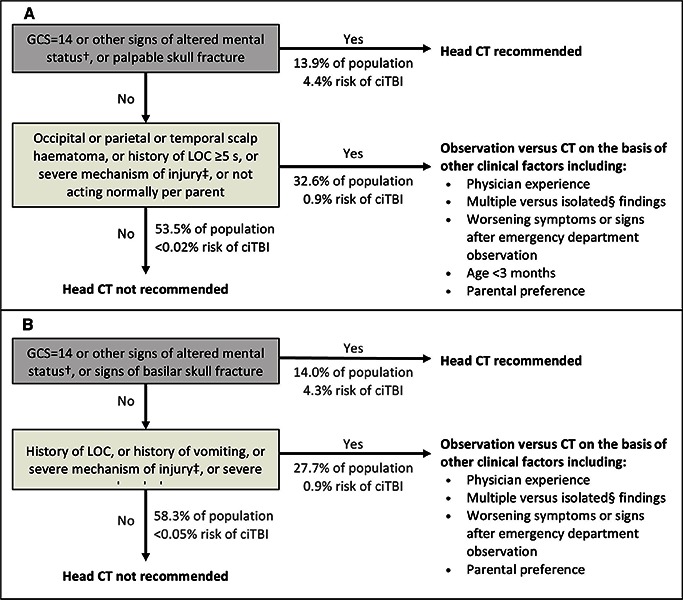 |
ciTBI - clinically-important traumatic brain injury, GCS - Glasgow Coma Scale, LOC - loss of consciousness.
†Other signs of altered mental status: agitation, somnolence, repetitive questioning, or slow response to verbal communication.
‡Severe mechanism of injury: motor vehicle crash with patient ejection, death of another passenger, or rollover; pedestrian or bicyclist without helmet struck by a motorized vehicle; falls of more than 0·9 m (3 feet) (or more than 1·5 m [5 feet] for panel B); or head struck by a high-impact object.
§Patients with certain isolated findings (i.e, with no other findings suggestive of traumatic brain injury), such as isolated LOC, isolated headache, isolated vomiting, and certain types of isolated scalp hematomas in infants older than 3 months, have a risk of ciTBI substantially lower than 1%. Risk of ciTBI exceedingly low, generally lower than risk of CT-induced malignancies. Therefore, CT scans are not indicated for most patients in this group” [4–9].
*Table 1 - Adopted from Kuppermann et al [4].
We believe that the PECARN approach is the most reliable approach. It is derived from a large study on pediatric head injury patients. It includes both derivation and validation populations. Furthermore, it has a fairly simple predication rule that can be easily followed by physicians to develop a clinical decision for the use of neuroimaging.
(2) Canadian Assessment of Tomography for Childhood Head injury (CATCH) [10] - (Table 2): A clinical decision rule for the use of CT scan in children with minor head injury.
Table 2.
Canadian Assessment of CT for Childhood Head injury (CATCH)
CT of the head is required only for children with minor head injury* and any one of the following findings: |
|
High risk (need for neurologic intervention) 1. GCS< 15 at two hours after injury 2. Suspected open or depressed skull fracture 3. History of worsening headache 4. Irritability on examination |
|
Medium risk (brain injury on CT scan) 5. Any sign of basal skull fracture (e.g., hemotympanum, “Raccoon” eyes, otorrhea or rhinorrhea of the cerebrospinal fluid, Battle’s sign) 6. Large, boggy hematoma of the scalp 7. Dangerous mechanism of injury (e.g., motor vehicle crash, fall from elevation ≥ 3 ft [≥ 91 cm] or 5 stairs, fall from bicycle with no helmet) |
CT - computed tomography, GCS – Glasgow Coma Scale.
Minor head injury is defined as injury within the last 24 hours associated with loss of consciousness, definite amnesia, disorientation, persistent vomiting (more than one episode) or persistent irritability in a child below two years of age with a GCS of 13-15.
This prospective study enrolled a total of 3866 patients from 10 Canadian hospitals with 7% being less than 2 years of age. The CATCH rule had 7 criteria to identify the need to use CT for children with minor head injury. The results of this study showed that having any 4 of the high-risk factors had a sensitivity of 100% in predicting outcome of neurosurgical intervention. It also showed that the presence of any factor from the 7-criteria rule would identify any CT-visible brain injury with a sensitivity of 98.1% (99.8 NPV). Three cases of brain injury were missed by 7-criteria CATCH rule in which none required neurosurgery.
(3) Children’s Head Injury Algorithm for the Prediction of Important Clinical Events (CHALICE) [11] – (Table 3):
Table 3.
The children’s head injury algorithm for the prediction of important clinical events rule
|
A computed tomography scan is required if any of the following criteria are present*: History
|
|
Examination
|
|
Mechanism
|
If none of the above variables are present, the patient is at low risk of intracranial pathology
A prospective study in which 22,772 patients were enrolled from 10 hospitals in England. The study aimed to provide a rule for selection of high-risk children with head injury for CT scanning. The CHALICE rule was derived with a sensitivity of 98% (NPV 99.9%) for the prediction of clinically significant head injury. Four missed cases with clinically-significant brain injury were not identified by the CHALICE rule; one of them required neurosurgical intervention.
(4) Scottish Intercollegiate Guidelines Network (SIGN) approach [12] - (Table 5):
Table 5.
SIGN* approach for the management of children with head injury
I. INDICATIONS FOR ADMISSION TO A HOSPITAL WARD |
Children who have sustained a head injury should be admitted to hospital if any of the following risk factors apply:
|
|
In injured children, especially the very young, the possibility of non-accidental injury must be considered:
In such cases a specialist paediatrician with the responsibility for child protection should be involved. Child protection procedures should be followed. Primary and secondary care information systems should identify children on the child protection register and frequent attenders |
II. INDICATIONS FOR DISCHARGE FROM EMERGENCY ROOM (ER) |
Children can be discharged from ER for observation at home if fully conscious and no additional risk factors apply |
III. REFERRAL TO A NEUROSURGICAL UNIT |
Features suggesting that specialist neuroscience assessment, monitoring or management are appropriate include:
|
THE PROCESS OF TRANSFER TO A NEUROSURGICAL UNIT |
|
IV. DISCHARGE PLANNING AND ADVICE |
Before discharge from the ward a patient with a head injury must be assessed by an experienced doctor, who must establish that all the following criteria have been met:
|
V. FOLLOW UP |
|
GCS – Glasgow Coma Scale
SIGN - Scottish Intercollegiate Guidelines Network
Both of SIGN and National Institute of Clinical Excellence (NICE) have published clinical guidelines on head injury in children highlighting the indications of CT head scan post TBI (Table 4) [12,13].
Table 4.
Selection of children (under 16 years) for head CT scan |
CT scanning is required if any of the following features:
|
CT- Computed tomography, GCS- Glasgow coma scale, PMH- Past medical history, RTA- Road traffic accident.
SIGN- Scottish Intercollegiate Guidelines Network,
NICE- National Institute of Clinical Excellence
SIGN guidelines included a comprehensive approach to the management of children with TBI. Apart from indications for CT scan, the guidelines include (Table 5):
Indications for admission to a hospital ward
Indications for discharge from emergency department
Referral to a neurosurgical unit
Discharge planning and advice
Follow up
Conclusion
TBI is a leading cause of death and disability in children. Treating any child with TBI is challenging with controversies in different approaches. The clinical decision of using head CT scan in children with TBI is one of the challenges that face treating physicians. Different approaches and guidelines have been identified to assist clinicians in CT decision making after head trauma. We encourage institutes to adopt the most suitable approach in order to insure consistency of practice and achieve better outcome.
Acknowledgement
The authors would like to acknowledge the family members of this article’s index patient for their kind agreement to use their tale as an educational model.
References
- 1.Stocchetti N, Conte V, Ghisoni L, Canavesi K, and Zanaboni C. Traumatic brain injury in pediatric patients. Minerva Anestesiol 2010, 76(12):1052–9. [PubMed] [Google Scholar]
- 2.Langlois JA, Rutland-Brown W, Thomas KE. Traumatic brain injury in the United States. In: CDC, ed. National Center for Injury Prevention and Control, 2006.
- 3.National Center for Injury Prevention and Control. Traumatic brain injury in the United States: assessing outcomes in children. CDC2006. [No date of update, cited 2014. March 21]. Available from: http://www.cdc.gov/ncipc/tbi/tbi_report/index.htm.
- 4.Kuppermann N, Holmes JF, Dayan PS, Hoyle JD, Jr, Atabaki SM, Holubkov R, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective cohort study. Lancet 2009; 374(3):1160–1170. [DOI] [PubMed] [Google Scholar]
- 5.Greenes DS, Schutzman SA. Clinical significance of scalp abnormalities in asymptomatic head-injured infants. Pediatr Emerg Care 2001; 17: 88–92. [DOI] [PubMed] [Google Scholar]
- 6.Kuppermann N, Holmes JF, Dayan PS, Hoyle J, Atabaki SM, Monroe D N, et al. Does isolated loss of consciousness predict traumatic brain injury in children after blunt head trauma? Acad Emerg Med 2008; 15:S82. [Google Scholar]
- 7.Palchak MJ, Holmes JF, Vance CW, Gelber RE, Schauer BA, Harrison MJ N, et al. Does an isolated history of loss of consciousness or amnesia predict brain injuries after blunt head trauma? Pediatrics 2004; 113:e507–513. [DOI] [PubMed] [Google Scholar]
- 8.Dayan PS, Holmes JF, Hoyle J Jr, Tunik MG, Lichenstein R, Alpern E, et al. Association of traumatic brain injuries (TBI) in children after blunt head trauma with degree of isolated headache or isolated vomiting. Acad Emerg Med 2008; 15:S175–176. [Google Scholar]
- 9.Dayan PS, Holmes JF, Schutzman S, Schunk J, Lichenstein R, Foerster LA, et al. Association of traumatic brain injuries with scalp hematoma characteristics in patients younger than 24 months who sustain blunt head trauma. Pediatr Emerg Care 2008; 24: 727. [Google Scholar]
- 10.Osmond MH, Klassen TP, Wells GA, Correll R, Jarvis A, Gary Joubert G, et al. CATCH: a clinical decision rule for the use of computed tomography in children with minor head injury. CMAJ 2010; 182:341–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dunning J, Daly JP, Lomas JP, Lecky F, Batchelor J, Mackway-Jones K. Derivation of the children’s head injury algorithm for the prediction of important clinical events decision rule for head injury in children. Arch Dis Child 2006; 91:885–891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scottish Intercollegiate Guidelines Network - SIGN [Internet]. Early Management of Patients with a Head Injury; May 2009. [updated 2014. January 20, cited 2014. March 21]. Available from: http://www.sign.ac.uk/guidelines/fulltext/110/index.html.
- 13.National Institute of clinical excellence (NICE) Clinical Guidelines [Internet]. Triage - assessment - investigation and early management of head injury in infants, children and adults; September 2007. [updated 2014. February 10, cited 2014. March 21]. Available from: http://guidance.nice.org.uk/CG56.


