Abstract
Dietary management, in particular salt and protein restriction is fundamental for the proper care of CKD patients. Therefore, a practical guide to the dietary treatment may be helpful among progressive CKD patients. In Japan, two academic societies such as Japanese Society of Nephrology and Japanese Society for Dialysis Therapy have recently published Guidelines for Dietary Management for non-dialysis dependent CKD and dialysis-dependent CKD, respectively.
In this manuscript, we summarized the practical guide for salt and protein restriction from the Japanese Society of Nephrology to retard the progression of CKD to endstage renal disease. This guide will promote further the collaboration of Nephrologists and Dietitians.
Background
CKD is common and the number of patients on renal replacement therapy (RRT) is estimated more than 330,000 in Japan [1]. It is becoming a social and economic burden. More than half of incident dialysis patients are CKD associated with diabetes mellitus (DM) and hypertension. Early detection and treatment would be necessary to retard the progression of CKD. Therefore, life-style modification including dietary management is important in patients with DM, hypertension, dyslipidemia, obesity, metabolic syndrome, and hyperuricemia. Among the dietary management, salt and protein restriction are critical for CKD patients, however it is influenced by differences in ethnic, regional, and cultural factors. We recently summarized a manual for dietician and other medical staff concerning life-style and dietary management in CKD patients (written in Japanese) [2, 3].
Discussion
Manual for dietary management
Table 1 summarized the guidance for lifestyle and dietary modification in CKD patients. Firstly, it is important diagnose the current stage of CKD (eGFR and proteinuria), cause of CKD, and also it is helpful to obtain the recent trend in CKD progression, pattern and slope of eGFR decline. Check the current medication and adherence to the drug therapy. Cessation of smoking and weight control should be accompanied with salt restriction and protein restriction. Until favorable results obtained, several rounds will be needed (Table 2).
Table 1.
Guidance for Lifestyle and dietary modification in CKD patients (Cited with permission from the Japanese Society of Nephrology)
| 1. Lifestyle and Dietary Modification | |
| 2. Weight control: BMI < 25.0 kg/m2 | |
| 3. Salt restriction: NaCl 3 to 6 g/day (if hypertensive) | Target blood pressure: <130/80 mmHg |
| 4. Protein restriction (Body weight as body mass index 22.0 kg/m2) | Stage 3a: 0.8 to 1.0 g/kg/day |
| Stage 3b: 0.6 to 0.8 g/kg/day | |
| Stage 4/5: 0.6 to 0.8 g/kg/day | |
| Stage 5D: HD patient 0.9 to 1.2 g/kg/day | |
| PD patient 0.9 to 1.2 g/kg/day | |
| 5. Potassium restriction (if hyperkalemia) | Stage 3b: ≤2000 mg/day |
| Stage 4/5: ≤1500 mg/day | |
| 6. Glucose (if DM present): HbA1c < 7.0 % | |
| 7. Lipids (if dyslipidemia): LDL-C < 120 mg/dL | |
Table 2.
Flow chart for Lifestyle and dietary modification (Cited with permission from the Japanese Society of Nephrology)
| 1st Round | 1) Obtain good rapport with patient |
| 2) Make a checklist for individual patient | |
| 3) Clear the priority (What is the category in the checklist?) | |
| For: Protein restriction, Salt restriction | Use the manual of Guidance (30 min in each guidance) |
| For: Weight control, Hypertension, Hyperglycemia | Hyperkalemia, Smoking cessation, Hyperlipidemia, Hyperuricemia, Use algorithm (30 min in each guidance) |
| 2nd Round: If not satisfactory, repeat the guidance again | If the first priority was successful, then try second |
| 3rd Round: If not satisfactory, repeat the guidance again (Continue counselling) | |
| If the second priority was not-successful, then repeat the guidance again |
Steps for salt and protein restriction
-
Use the checklist
Obtain clinical and laboratory information of the patient.
-
Check the current problem
Adherence to drug therapy should be checked. Important categories are body mass index (BMI), blood pressure, fasting blood glucose, LDL-cholesterol.
-
Guidance by category
Salt (NaCl) Restriction, Protein Restriction
-
Guidance by algorithm
BMI, Blood Pressure, Blood Glucose, Lipid, Smoking Cessation, Potassium, Uric Acid
-
Useful materials
Salt content in food staff
Salt restriction
-
Rationale
Salt restriction is essential for CKD patients. If not adequately controlled, salt retention may cause edema, heart failure and hypertension. Daily intake from foods and additives should be estimated carefully. In particular, salt intake may vary with cooking process.
-
Practical Guide
We summarized several tools to help adhering to salt restriction.
-
Salt content in seasoning (Fig. 1)
Use spoon to estimate the amount of added seasoning, in particular when uses common seasoning materials such as table salt, source, and Miso.
Estimate roughly as salt (gram) per one small spoon.
Select low salt seasoning and law salt food staffs (Avoid too much).
Check the salt ingredient in each food staff.
-
Salt content in processed food (Fig. 2)
Processed foods are difficult to check. When expressed as salt content as “mg”, salt content should be calculated as: Na (mg) X 2.54/1000 = Salt (g)
-
Tips for cooking (Fig. 3)
Salt restricted food is often regarded as “non-palatable”. Adherence to salt restriction could be improved by using other seasoning materials without salt. It may take time to adjust salt restriction.
-
Restaurant (Fig. 4)
Generally, cooked-food and diet outside home are salt-rich, although it may differ by restaurant or region. It may be helpful to “recall what and how much have eaten, etc.” Advice to check the nutrient content when buy the cooked foods.
Fig. 1.
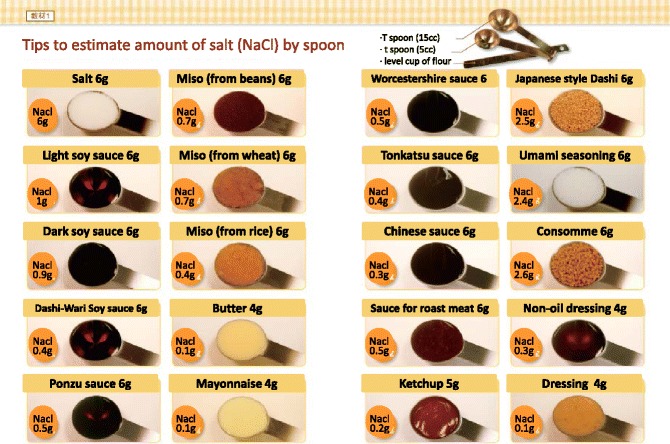
Estimating of salt content in the seasoning material
Fig. 2.
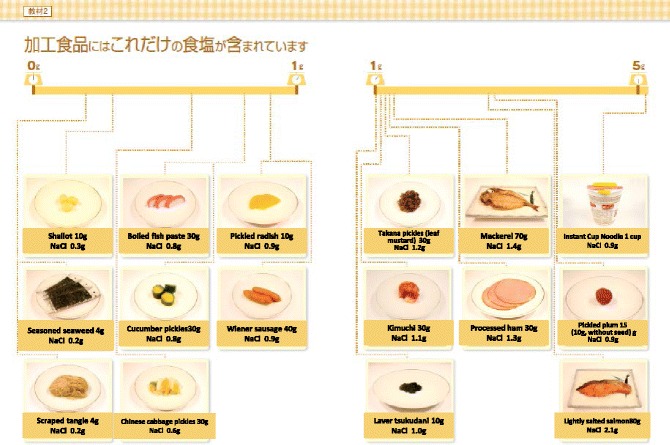
Rough estimate of salt content in the processed foods
Fig. 3.
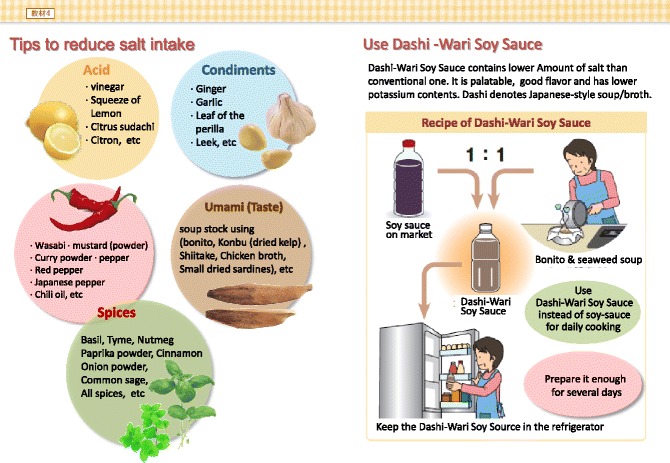
Tips for salt restriction Use other than soy-source
Fig. 4.
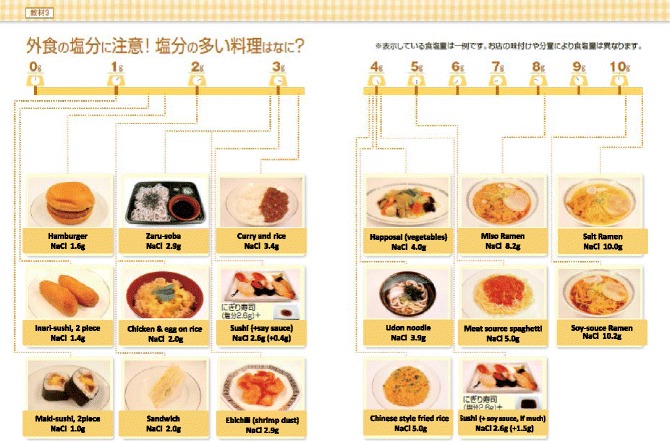
Examples of salty foods at restaurants. (All figures are cited from “Manual for CKD life and dietary guidance manual for physicians and co-medical staffs; edited by the Japanese Society of Nephrology”. Sample Legends: Sample 1. A sample of breakfast. Sample 2. A sample of lunch. Sample 3. A sample of dinner. Sample 4. A sample of balanced diet. (All cited from “Manual for CKD life and dietary guidance manual for physicians and co-medical staffs; edited by the Japanese Society of Nephrology”)
Some tips;
/Ask low salt cooking at restaurant/Do not drink soup when ordering/
/Use separate dish for dressing or mayonnaise/Select food easy to estimate salt intake/When eat-out, restrict salt more than usual at home
-
e)
Avoid too much salt restriction
Too much, less than 3 g/day, salt restriction is dangerous if adequate food intake has not accompanied.
Protein restriction
-
Rationale
Ingested protein is finally metabolized to water, carbon dioxide, and other compounds, mainly containing nitrogen. Protein (amino acids) is used to construct body protein and also used for energy production. Water and nitrogen compounds are excreted from kidney. Nitrogenous compounds will retain in the blood as kidney function deteriorates resulting uremic symptoms such as nausea, vomiting, anorexia, and anemia. Electrolyte-imbalance such as hyperkalemia, hyperphosphatemia, and metabolic acidosis may appear in CKD stage 3 patients. To prevent such symptoms, protein restriction is indicated timely in accordance with remaining kidney function to prevent complications and also retard the progression of CKD.
-
Quality of protein
Human body is constructed by protein such as elastin, collagen, hemoglobin, enzymes, and hormones. Essential amino acid such as leucine, isoleucine, valine, lysine, tryptophan, phenylalanine, threonine, methionine, histidine should be supplied as human cannot synthesize them. Foods with high content of essential amino acid expressed as high amino acid score is regarded as good quality protein food staff. Generally, animal meats are high amino acid score, but not so high in vegetables including soybean products (Table 3).
If protein intake is over 60 g/day, deficiency of essential amino acid is rarely occur. However, in case of protein restriction, insufficient intake of essential amino acid and energy may occur, therefore careful monitoring is recommended to prevent protein-energy wasting (PEW). CKD patients with stage 3b to 5 should be managed with trained dietician and nephrologist.
-
Lipid intake
Lipid intake should be 20 to 25 % of the total energy intake. N-3 poly-unsaturated fatty acid is recommended for preventing atherosclerosis.
-
Energy intake
While practicing protein restriction, adequate energy intake should be maintained. Too strict protein restriction may result energy intake deficiency. In particular patients with CKD stage 4 to 5. When energy intake is not sufficient, ingested protein is used for energy, but not for protein construction, resulting muscle and/or wasting. In patients with CKD stage 3b to 5, protein restriction of less than 0.8 g/kg/day should be performed with guidance of special medical team.
-
Practical Guide (Table 4)
Patients are instructed to adhere protein restriction by using learning tools to estimate amount of protein, amino acid score, and salt. (Sample 1, 2, 3 and 4).
Table 3.
Amino-acid score in common food in Japan(1973 FAO/WHO) (Cited with permission from the Japanese Society of Nephrology)
| Food | Amino-acid score |
|---|---|
| Salmon | 100 |
| Saury | 100 |
| Mackerel | 100 |
| Pork, Sirloin | 100 |
| Beef | 100 |
| Chicken, Round | 100 |
| Milk | 100 |
| Chicken Egg | 100 |
| Polished Rice | 65 |
| Soba | 65 |
| Sweet Potato | 88 |
| Potato | 68 |
| Soybean | 86 |
| Fermented Soybean (Natto) | 84 |
| Okura | 57 |
| Green Beans | 68 |
| Turnip | 45 |
| Asparagus | 68 |
Table 4.
Nutrient content in food common in Japan, expressed grams of food): Food Samples for protein restriction, adjusted to body size (Cited with permission from the Japanese Society of Nephrology)
| Height, cm | 174 | 157 | 152 | 148 |
| Energy, kcal/day | 2000 | 1800 | 1600 | 1400 |
| Protein, g/day | 55 | 45 | 40 | 35 |
| Rice, | 540 | 480 | 390 | 330 |
| Egg | 50 | 25 | 25 | 25 |
| Meat | 60 | 60 | 50 | 45 |
| Fish | 60 | 60 | 50 | 45 |
| Soybeans | 20 | 20 | 20 | 0 |
| Milk Products | 120 | 90 | 90 | 90 |
| Vegetables | 300 | 300 | 300 | 300 |
| Potato | 100 | 100 | 100 | 100 |
| Fruits | 120 | 120 | 120 | 120 |
| Sugar/sweets | 20 | 20 | 20 | 20 |
| Harusame (Gelatin Noodles) | 25 | 25 | 25 | 25 |
| Oils | 25 | 25 | 25 | 25 |
| Energy Additive, kcal | 100 | 100 | 100 | 100 |
Three meals a day. Energy Additive; ex) soft-drinks containing carbohydrate 250 ml≑100 kcal
Sample 1.
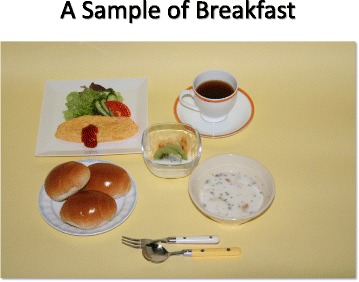
A sample of breakfast
Sample 2.
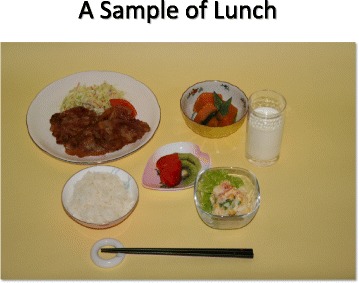
A sample of lunch
Sample 3.
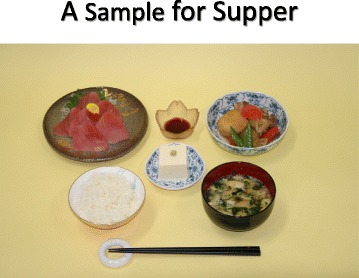
A sample of dinner
Sample 4.
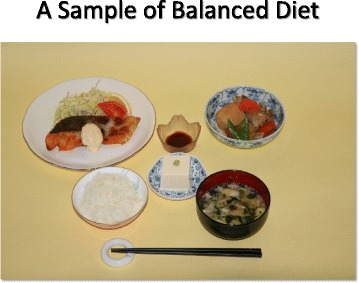
A sample of balanced diet (All cited from “Manual for CKD life and dietary guidance manual for physicians and co-medical staffs; edited by the Japanese Society of Nephrology”)
Summary
We have done a strategic outcome study for chronic kidney disease: Frontier of Renal Outcome Modifications in Japan (FROM-J study) [4]. Management of CKD requires multi-disciplinary involvement. In this study, we prospectively observed the effects of intervention from dietitians and supportive care in CKD patients in addition to usual care recommended by Japanese Society of Nephrology [5]. Through this study, we published practical guidebook with full involvement from dietitian’s society [2, 3].
Acknowledgements
Not applicable.
Funding
This study was supported in part by a Grant-in-Aid for Research on Advanced Chronic Kidney Disease (REACH-J). Practical Research Project for Renal Diseases from Japan Agency for Medical Research and development, AMED.
Availability of data and materials
Not applicable.
Authors’ contributions
Both authors contributed equally to the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Contributor Information
Kunitoshi Iseki, Email: Chihokun_ohra@yahoo.co.jp.
Kunihiro Yamagata, Email: k-yamaga@md.tsukuba.ac.jp.
References
- 1.Yamagata K, Yagisawa T, Nakai S, Nakayama M, Imai E, Hattori M, Iseki K, Akiba T. Prevalence and incidence of chronic kidney disease stage G5 in Japan. Clin Exp Nephrol. 2015;19:54–64. doi: 10.1007/s10157-014-0978-x. [DOI] [PubMed] [Google Scholar]
- 2.Manual of diet and lifestyle modification for CKD patients: for physicians and co-medical staffs. Edited by the Japanese Society of Nephrology (in Japanese). 2015
- 3.Manual of diet and lifestyle modification for CKD patients: Practical guide for dietary guidance. Edited by the Japanese Society of Nephrology (in Japanese). 2015
- 4.Yamagata K, Makino H, Akizawa T, Iseki K, Itoh S, Kimura K, Koya D, Narita I, Mitarai T, Miyazaki M, Tsubakihara Y, Watanabe T, Wada T, Sakai O. Advisory Committee for FROM-J. Design and methods of a strategic outcome study for chronic kidney disease: Frontier of Renal Outcome Modifications in Japan. Clin Exp Nephrol. 2010;14:144–51. doi: 10.1007/s10157-009-0249-4. [DOI] [PubMed] [Google Scholar]
- 5.Practice Guide for CKD (2009, in Japanese). www.jsn.or.jp
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


