Abstract
Objective
Diabetes mellitus (DM) is associated to the morphological and componential characteristics of atheromatous plaques. It has proven that plaque textures are related to plaque components and beneficial for atherosclerotic risk stratification. The aim of this study is to compare plaque textures in patients with and without DM, and examine the relationship between HbA1c levels and the ultrasound plaque textures in atherosclerotic patients.
Methods
A total of 136 participants (among them 66 are diabetic and 70 are non-diabetic) suffering from carotid plaques were included. About 300 texture features were extracted from the ultrasound images of plaques using the algorithms of histogram, absolute gradient, run-length matrix, gray-level co-occurrence matrix, autoregressive model and wavelet transform, respectively. Thirty optimal features were selected by the Fisher coefficient and the mutual information measure. The most discriminating feature (MDF) was obtained from the linear discriminant analysis for the optimal features. Linear regression model was performed to investigate the relationship between HbA1c and MDF. The receiver operating characteristics (ROC) curve was further developed to validate the relation between the estimated HbA1c (models output) and diabetes status.
Results
A total of 12 texture features showed statistical difference between patients with and without DM. The MDF was significant higher in non-diabetic patients (0.326 ± 0.049) than diabetic patients (−0.346 ± 0.052) (p < 0.001). The optimal regression model (r = 0.348, p < 0.001) for HbA1c included a constant (p < 0.001) and the MDF (p < 0.001). The areas under ROC curve used to estimate HbA1c was 0.828.
Conclusions
The results indicate that there is a quantitative relationship between the HbA1c levels and plaque textures in ultrasonic images of atherosclerotic patients, which may suggest that texture analysis of the ultrasonic image of plaque is a promising method for evaluating the cardiovascular risk caused by DM in patients with plaques.
Keywords: Ultrasound imaging, Carotid plaque, Texture, HbA1c, Cardiovascular disease
Background
Diabetes mellitus (DM) enable to accelerate atherosclerosis and increase the risk of cardiovascular diseases [1, 2]. Carotid intima-media thickening (IMT) measured by ultrasound imaging and carotid artery elasticity evaluated by ultrasound radio frequency technology have been utilized for assessing the impact of DM on the plaques [3, 4]. These schemes, however, ignore some essential information about the plaque surface and morphology. Substantial evidences have indicated that quantitative textural analysis of the medical images can provide more useful diagnostic information [5], and is useful for atherosclerotic risk stratification [6]. Thus, it is significant to characterize carotid plaques using textures in patients with and without DM, which may help to evaluate the risk of cardiovascular events caused by DM.
DM are associated with the morphological and the componential characteristics of carotid plaques [3, 7]. In previous studies, Wilhjelm et al. [8] found that texture features of the ultrasound plaques was correlated with the histologically determined relative volume of soft materials. Niu et al. [9] indicated that texture features extracted from ultrasound images of the carotid arterial wall were useful in identifying arterial surface roughness. Rakebrandt et al. [10] reported that there are five texture classes match with the plaque contents including fibrin, elastin, calcium, haemorrhage and lipid. The above studies may imply that some plaque textures are different in patients with and without DM. Furthermore, HbA1c is a risk factor for cardiovascular diseases in type 2 diabetes [11], and is related to the mortality in heart failure patients with diabetes [12]. However, few studies have investigated the relationship between HbA1c and plaque textures.
The aim of this study is to compare plaque textures in patients with and without DM, and examine the relationship between HbA1c levels and plaque textures in atherosclerotic patients.
Subjects and methods
Subjects
A total of 136 subjects (among them 66 are diabetic and 70 are non-diabetic) suffering from carotid plaques were investigated in present study. From October 2011 to February 2015, the patients received carotid artery examination at the department of ultrasound, the third affiliated hospital of Sun Yat-sen University. All participants provided the written informed consent. The study protocol was approved by the Institutional Review Board of the third affiliated hospital of Sun Yat-sen University (Guangzhou, China).
In this study, the diagnostic criteria for diabetes are defined as fasting plasma glucose (FPG) level of ≥7.0 mmol/L, and/or 2-h plasma glucose value of ≥11.1 mmol/L, and/or HbA1c level of ≥6.5 %, and/or treatment with either hypoglycemic agents or insulin [13, 14]. Patients with acute or chronic infectious disease, alcohol or drug abuse, retinopathy, or uncontrolled hypertension were excluded. Information regarding age, gender, total number of plaques, systolic blood pressure (SBP), diastolic blood pressure (DBP), body mass index (BMI), total cholesterol, triglyceride, low density lipoprotein cholesterol, high density lipoprotein cholesterol, lipoprotein, apolipoprotein A1, apolipoprotein B100, FPG, HbA1c and medication use were collected.
Carotid ultrasonography
The study was performed by a specialized physician with 5 years vascular ultrasound working experience using a Toshiba AplioXG SSA-790A ultrasound Platform equipped with a 5–12 MHz linear-array transducer (PLT-805AT) and Esaote MyLab90 ultrasound Platform equipped with a 4–13 MHz linear-array transducer (LA523). The carotid artery was examined with the head tilted slightly upward in the mid-line position. The transducer was manipulated so that the near and far walls were parallel to the transducer footprint, and the lumen diameter was maximized in the longitudinal plane.
To improve the comparability of the plaque images obtained by different ultrasound systems at different settings, all images were standardized according to the scheme proposed by Sabetai et al. [15] before texture analysis. Furthermore, it is more clinically significant to focus on echolucent plaques, since these plaques are more potentially unstable than echo-rich plaques [16]. Gray-scale median (GSM) analysis is an objective and reproducible method for evaluating the echogenicity of carotid plaque [15]. In case there were multiple plaques in one individual, the plaques with the lowest GSM value among them was selected as the representative for the following texture analysis [17]. Two operators performed the GSM measurement independently, and the interoperator reproducibility was evaluated with a kappa value. The disagreement of the two operators were discussed and re-evaluated, then an agreement was finally achieved.
Many studies have shown that carotid intima-media thickening (IMT) is a high risk factor of the future cardiovascular events [18–20]. Maximum IMT (Plaque-IMTmax) was defined as the greatest axial thickness among the plaques in the carotid arteries [21, 22], and was measured in this study.
Texture analysis
MaZda is an effective tool for texture analysis and offers an approach for texture feature extraction, selection and reduction [23]. In MaZda, we can draw regions of interest with arbitrary shapes, as shown in Fig. 1. It provides six various algorithms, such as histogram, absolute gradient, run-length matrix, co-occurrence matrix, autoregressive model and wavelet for features extraction [5, 23]. In present study, about 300 texture features of carotid plaques were extracted using MaZda, as shown in Table 1.
Fig. 1.
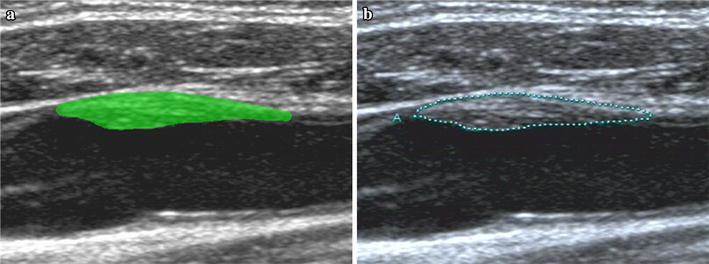
The region of interest selection. a The region of interest selection according to (b) using MaZda software. b Plaque defined by a specialized physician with 5 years vascular ultrasound working experience
Table 1.
Texture features
| Histogram (1) mean, (2) variance, (3) skewness, (4) kurtosis and (5) percentiles 1, 10, 50, 90 and 99 % |
| Absolute gradient (1) mean, (2) variance, (3) skewness, (4) kurtosis and (5) percentage of pixels with nonzero gradient |
| Run-length matrix (1) run-length nonuniformity, (2) grey-level nonuniformity, (3) long-run emphasis, (4) short run emphasis and (5) fraction of image in runs. Parameters computed for horizontal, 45° vertical and 135° orientation |
| Co-occurrence matrix (1) angular second moment, (2) contrast, (3) correlation, (4)sum of squares, (5) inverse difference moment, (6) sum average, (7) sum variance, (8) sum entropy, (9) entropy, (10) difference variance and (11) difference entropy. Parameters are computed for 4 orientations: (a, 0), (0, a), (a, a), (a, −a) and 5 distances: a = 1, 2, 3, 4, 5; between image pixels |
| Autoregressive model (1) model parameter vector includes 4 parameters and (2) standard deviation of the driving noise |
| Wavelet (1) Energy of wavelet coefficients in low-frequency subbands, (2) horizontal high-frequency subbands, (3) vertical high-frequency subbands and (4) diagonal high-frequency subbands at successive scales |
Texture feature selection and reduction
In order to select optimal features among the large number of texture features of the plaques from diabetic and non-diabetic patients, the methods based on Fisher coefficient and mutual information measure were used to select 15 optimal features, respectively. Furthermore, linear discriminant analysis (LDA) was implemented for the combined feature set, and the most discriminating features (MDF) were obtained.
Fisher coefficient
Fisher coefficient is defined as a ratio of between-class scatter D to within-class variance V [24]:
| 1 |
where , and denote the mean, the variance and the priori probability of class i, respectively. Texture features with larger Fisher coefficient are selected as optimal features.
Mutual information measure
Mutual information (MI), a measure of dependence between two random variables, is defined as [25]:
| 2 |
where X and Y are random variables, H is the entropy. In case of X stores values of texture features and Y stores the classification decision. Then, a large MI between X and Y means that X is a useful texture features for classification. Then the MI for each texture features is calculated by [25, 26]:
| 3 |
where means the class category, is the total number of class, is the number of histogram bins used for feature discretization, denotes discretized value of .
Linear discriminant analysis
LDA is a useful method for feature reduction [24]. The aim of LDA is to find a transform matrix W such that the ratio of determinants is maximized. Where and are the between-class scatter matrix and the within-class scatter matrix. These matrices can be given as formulas (4, 5).
| 4 |
| 5 |
where denotes the i-th pattern in class k, is the mean vector of class k. It has proved that such a transform matrix is composed of eigenvectors corresponding to largest eigenvalues of . The MDF can be obtained when the original data is transformed by the means of matrix as formula (6).
| 6 |
Statistical analysis
All statistical analysis was performed with PASW Statistics 18 and p less than 0.05 was considered statistically significant. All values were presented as the mean value ±SD, or real number of patients with the percentage in parentheses. Independent sample ttest was used to examine the baseline clinical parameters between the diabetic and non-diabetic patients. Pearson correlation analysis was conducted to investigate the relationship between HbA1c and the variables including age, BMI, total number of plaques, SBP, DBP, plaque-IMTmax and MDF. Linear regression analysis was carried out by considering the HbA1c as a dependent variable and regarding the MDF as independent variable. The optimized regression model was obtained to estimate the HbA1c. Further, the receiver operating characteristics (ROC) curve was developed to test the relationship between the estimated HbA1c (models output) and diabetes status.
Results
Baseline characteristics of study participants
Table 2 describes the baseline characteristics of the study population (n = 136), which includes 66 patients with DM (age, mean ± SD, 67.8 ± 10.0 years) and 70 patients without DM (age, mean ± SD, 69.4 ± 9.8 years). The BMI (23.9 ± 3.1 vs 22.0 ± 2.8 kg/m2, p = 0.001), triglyceride (1.90 ± 1.57 vs 1.31 ± 0.89, p = 0.009 mmol/L), HbA1c (8.87 ± 2.25 vs 5.50 ± 0.41 %, p < 0.001) and FPG (10.76 ± 4.26 vs 5.14 ± 0.70 mmol/L, p < 0.001) were significantly different in patients with and without DM. In the DM group, the ratio of patients using oral hypoglycemic agent, insulin, both oral hypoglycemic agent and insulin, and no drug for treatment were 50 % (n = 33), 21.2 % (n = 14), 9.1 % (n = 6), and 19.7 % (n = 13).
Table 2.
Baseline characteristics of 136 subjects
| Characteristics | Diabetes (n = 66) | Non-diabetes (n = 70) | t | p |
|---|---|---|---|---|
| Age, mean (SD) | 67.8 ± 10.0 | 69.4 ± 9.8 | −0.972 | 0.333 |
| Male gender, n (%) | 43 (65) | 46 (66) | 0.068 | 0.946 |
| Total number of plaques | 2.1 ± 1.2 | 2.0 ± 1.1 | 0.533 | 0.104 |
| Hypertension, n (%) | 43 (65) | 44 (63) | 0.277 | 0.783 |
| CHD, n (%) | 18 (27.3) | 22 (31.4) | −0.528 | 0.598 |
| SBP (mm Hg) | 136.9 ± 19.0 | 139.1 ± 22.0 | −0.642 | 0.522 |
| DBP (mm Hg) | 75.8 ± 9.2 | 76.7 ± 12.8 | 0.465 | 0.643 |
| BMI (kg/m2) | 23.9 ± 3.1 | 22.0 ± 2.8 | 3.437 | 0.001 |
| Total cholesterol (mmol/L) | 4.78 ± 1.20 | 4.46 ± 1.17 | −1.548 | 0.116 |
| Triglyceride (mmol/L) | 1.90 ± 1.57 | 1.31 ± 0.89 | 2.677 | 0.009 |
| HDL-cholesterol (mmol/L) | 1.05 ± 0.28 | 1.13 ± 0.34 | −1.484 | 0.140 |
| LDL-cholesterol (mmol/L) | 3.04 ± 0.97 | 2.86 ± 1.06 | 1.023 | 0.308 |
| Lipoprotein A (mg/L) | 211.9 ± 219.2 | 284.9 ± 288.7 | −1.652 | 0.101 |
| Apolipoprotein A1(g/L) | 1.29 ± 0.31 | 1.31 ± 0.26 | −0.362 | 0.718 |
| Apolipoprotein B100 (g/L) | 1.20 ± 0.47 | 1.17 ± 1.23 | 0.163 | 0.871 |
| HbA1c (%) | 8.87 ± 2.25 | 5.50 ± 0.41 | 11.940 | <0.001 |
| FPG (mmol/L) | 10.76 ± 4.26 | 5.14 ± 0.70 | 10.611 | <0.001 |
| Plaque-IMTmax (mm) | 2.4 ± 0.8 | 2.5 ± 0.8 | −0.635 | 0.527 |
Data are presented as the mean value ±SD or percentage of subjects
CHD coronary heart disease, SBP systolic blood pressure, DBP diastolic blood pressure, BMI body mass index, HDL-cholesterol high density lipoprotein cholesterol, LDL-cholesterol low density lipoprotein cholesterol, FPG fasting plasma glucose
Plaques selection
There was a good agreement between the two operators in selecting the plaque with the lowest GSM value in one individual with multiple plaques. The interoperator reproducibility was 97.79 % (kappa value = 0.965), and the 3 controversial plaques were discussed and re-evaluated, then eventually an agreement was achieved.
Texture selection and reduction
A total 30 optimal features were selected based on the Fisher coefficient and the mutual information measure. Among the optimal features, 12 features (7 feature extracted by run-length matrix and 5 features extracted by wavelet) were considered to be statistically different in patients with and without DM, as shown in Table 3. In order to reduce the number of the optimal features, LDA was further performed to gain the MDF. The MDF (−0.035 ± 0.052 vs 0.033 ± 0.050, p < 0.001) showed significant difference in the diabetic and the non-diabetic patients.
Table 3.
Statistically different features between diabetic and non-diabetic plaques
| Features | Non-diabetes (n = 70) | Diabetes (n = 66) | Fisher | MI | t | p |
|---|---|---|---|---|---|---|
| WavEnLH_s-4 | 756.21 ± 418.35 | 522.48 ± 385.45 | 0.342 | 0.109 | 3.383 | 0.001 |
| Vertl_Fraction | 0.883 ± 0.056 | 0.847 ± 0.096 | 0.213 | 0.036 | 2.630 | 0.010 |
| 135dr_ShrtREmp | 0.921 ± 0.037 | 0.893 ± 0.0716 | 0.25 | 0.066 | 2.866 | 0.005 |
| Vertl_ShrtREmp | 0.915 ± 0.040 | 0.886 ± 0.072 | 0.243 | 0.046 | 2.810 | 0.006 |
| WavEnLL_s-2 | 16,327 ± 4554 | 13,092 ± 7191 | 0.229 | 0.055 | 2.2733 | 0.007 |
| WavEnLL_s-1 | 16,327 ± 4559 | 13,474 ± 7337 | 0.224 | 0.041 | 2.705 | 0.008 |
| WavEnLH_s-3 | 465.39 ± 275.86 | 343.30 ± 247.33 | 0.220 | 0.039 | 2.712 | 0.008 |
| 135dr_Fraction | 0.892 ± 0.052 | 0.858 ± 0.091 | 0.213 | 0.040 | 2.627 | 0.010 |
| 45dgr_ShrtREmp | 0.918 ± 0.038 | 0.892 ± 0.073 | 0.210 | 0.038 | 2.606 | 0.011 |
| WavEnLL_s-3 | 15,479 ± 4811 | 12,802 ± 7299 | 0.193 | 0.069 | 2.510 | 0.014 |
| Horzl_ShrtREmp | 0.816 ± 0.095 | 0.757 ± 0.169 | 0.191 | 0.048 | 2.491 | 0.014 |
| 45dgr_Fraction | 0.887 ± 0.053 | 0.854 ± 0.095 | 0.184 | 0.040 | 2.444 | 0.016 |
| MDF | 0.033 ± 0.050 | −0.035 ± 0.052 | – | – | 7.712 | <0.001 |
WavEnLH_s-3 and WavEnLH_s-4 are energy of wavelet coefficients in vertical high-frequency subbands at scale 3 and 4; WavEnLL_s-1, WavEnLL_s-2 and WavEnLH_s-3 are energy of wavelet coefficients in low-frequency subbands at scale 1, 2 and 3; 45dgr_Fraction, Vertl_Fraction and 135dr_Fraction are fraction of image in runs computed for 45°, vertical and 135° orientation; Vertl_ShrtREmp, Horzl_ShrtREmp, 45dgr_ShrtREmp, Vertl_ShrtREmp and 135dr_ShrtREmp are short run emphasis computed for horizontal, 45° vertical and 135° orientation
MDF most discriminating feature, MI mutual information
Pearson correlation of the study variables with HbA1c
Pearson correlation analysis was implemented to examine the relationship between HbA1c and the variables including age, BMI, total number of plaques, SBP, DBP and MDF. Table 4 indicates that the HbA1c is positively correlated with BMI (r = 0.182, p = 0.034), whereas HbA1c is negatively correlated with the MDF (r = −0.348, p < 0.001).
Table 4.
Pearson correlation of the study variables with HbA1c
| Age (year) | BMI (kg/m2) | TNP | SBP (mmHg) | DPB (mmHg) | Plaque-IMTmax (mm) | MDF | ||
|---|---|---|---|---|---|---|---|---|
| HbA1c (%) | Pearson | −0.123 | 0.182 | −0.022 | −0.071 | 0.084 | −0.097 | −0.348 |
| p | 0.155 | 0.034 | 0.795 | 0.408 | 0.333 | 0.262 | <0.001 | |
BMI body mass index, TNP total number of plaques, SBP systolic blood pressure, DBP diastolic blood pressure, MDF most discriminating feature
Linear regression model for HbA1c
Table 5 shows that the optimal model for HbA1c (r = 0.348, p < 0.001) is achieved by stepwise regression method. The model included a constant (p < 0.001) and the MDF (p < 0.001). The optimized regression equation can be described as formula (7) to estimate the HbA1c.
| 7 |
where is the MDF.
Table 5.
Linear regression model of HbA1c with the coefficients of the variables involved
| Model | Variables/constant | Coefficients | P | 95.0 % confidence interval | |
|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||
| HbA1c (r = 0.392, p < 0.001) | Constant | 7.136 | <0.001 | 6.766 | 7.506 |
| MDF | −13.297 | <0.001 | −19.407 | −7.186 | |
MDF most discriminating feature
Further, the ROC curve was developed to validate the relationship between the estimated HbA1c and diabetes status, and the area under the ROC curve was 0.828 (Fig. 2).
Fig. 2.
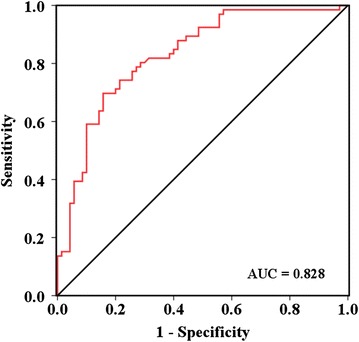
The receiver operating characteristics curve for validating the relationship between estimated HbA1c and diabetes status. AUC represents areas under receiver operating characteristics curve
Discussion
In this study, a total of 12 texture features showed significant difference in diabetic and non-diabetic patients. Previous studies indicated that MD impacted the vascular structure and function [27, 28], increased the IMT of common carotid artery [3], and modified the relationships between carotid plaque calcium, composition and inflammation [7]. The textural differences may be a candidate parameter reflecting the morphological and componential differences of the carotid plaques in patients with and without DM. The texture features including the fraction of image in runs computed for 45°, vertical and 135° orientation, and the short run emphasis computed for horizontal, 45°, vertical and 135° orientation were statistically higher in non-diabetic patients than diabetic patients. The fraction of image in runs is a measurement of the percentage of image pixels that are part of any of the runs considered for the matrix computing and it should have a low value for images with linear structure [5, 29]. Moreover, the short run emphasis, a feature emphasizing the short runs, is a measure of the proportion of short runs occurring in the image [5, 29]. Given the above, it may suggest that diabetes tend to impact plaques with a linear structure in the surface.
In previous studies, Virmani et al. [30] indicated that the BMI was significantly higher in diabetic patients (30.5 ± 7.41 kg/m2) than in non-diabetic patients (26.6 ± 5.4 kg/m2) (p = 0.001). Nozue et al. [31] showed that BMI was significantly different in the participants with MD or not (25.3 ± 3.9 vs 23.8 ± 2.7 kg/m2, p = 0.01). Marso et al. [32] indicated that the median triglycerides in acute coronary syndrome patients with MD was 144 mg/dL, whereas that in patients without MD was 101 mg/dL (p < 0.001). In the study of Lee et al. [33] reported that the median triglycerides in subjects with HbA1c ranged from 3.6 to 5.2, from 5.3 to 5.4, from 5.6 to 5.7, and from 5.8 to 6.4 were 109.1, 116.1, 120.2, and 127.9 mg/dL, respectively (p < 0.001). These findings are consistent with our results, in which the BMI (23.9 ± 3.1 vs 22.0 ± 2.8 kg/m2, p = 0.001) and triglycerides (1.90 ± 1.57 vs 1.31 ± 0.89 mmol/L, p = 0.009) are statistically different in the patients with and without DM.
Ultrasound IMT measurements were considered as a strong predictor of future cardiovascular events [18–20]. Recent studies suggested that the increased IMT was not an independent predictor of plaque development [34, 35]. Compare with carotid IMT, carotid plaque predicts cardiovascular events more accurately [36, 37]. In this study, the carotid plaque-IMTmax showed no statistical difference in patients with and without DM (2.4 ± 0.8 vs 2.5 ± 0.8 mm, p = 0.527), whereas the MDF was significant higher in diabetic patients (0.033 ± 0.050) than in non-diabetic patients (−0.035 ± 0.052) (p < 0.001). It may suggest that the MDF is more effective than carotid plaque-IMTmax in illustrating the difference of plaques in patients with and without DM. Additionally, MDF make it possible to evaluate the stability of the plaque. Compared with the conventional features (i.e. plaque-IMTmax) that are evaluated visually, the MDF is an abstract feature that extracted from texture features without visual evaluation.
HbA1c testing reflects the average plasma glucose over the previous 2–3 months [38]. Mukai et al. [39] indicated that the crude average of the maximum carotid intima-media thickness increased significantly with rising quartiles of HbA1c. Daida et al. [40] examined the association between HbA1c and plaque regression, and suggested that plaque regression was less pronounced in patients with high HbA1c levels compare with those with low levels. In present study, we found a relationship between the HbA1c levels and plaque textures in atherosclerotic patients, which may be useful for evaluating the impact of long-term blood glucose level on the carotid plaques. Furthermore, Eeg-Olofsson et al. [11] indicated that higher HbA1c levels increased the risks of cardiovascular disease, coronary heart disease and total mortality. Ikeda et al. [41] showed that HbA1c was an independent risk factor for cardiovascular disease. The relationship between the MDFs and HbA1c may suggest that the MDFs can be used to assess cardiovascular risk, which may elevate the value of B-mode ultrasonography examination.
The main limitation was that this method could be applied only to patients with carotid plaques. The atheromatous plaque, however, was a common complication of diabetes and had a high prevalence in population [42, 43]. Besides, the number of subjects was relatively small in this study. A longitudinal, prospective study utilizing carotid ultrasound evaluation in a large number of diabetic patients with plaques is required to assess the precise prognostic value of plaque textures in determining future cardiovascular events caused by DM.
Conclusion
In conclusion, the results of present study indicated that the textures of the carotid plaques were statistically different in patients with and without DM. The relationship between the HbA1c levels and plaque textures may suggest that texture analysis of the ultrasound images of carotid plaques is a promising method to evaluate the risk of cardiovascular events caused by DM in patients with plaques.
Authors’ contributions
XWH, YLZ, RQZ, HRZ and LLN took part in the design of this study, collected and analyzed the data, interpreting the data, wrote the manuscript. LM participated analytical methods, interpretation of results, wrote the manuscript. MQ, WZ participated analytical methods, interpretation of results. All authors were involved in making revisions to the manuscript. Finally, all authors reviewed the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The work was supported by 973 Program (Grant No. 2015CB755500) and National Science Foundation Grants (NSFC Grant Nos. 81527901, 11325420, 11302239, 11574341, 11304341), Shenzhen Basic Science Research (JCYJ20140417113430580).
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- DM
diabetes mellitus
- MDF
most discriminating feature
- ROC
receiver operating characteristics
- IMT
intima-media thickening
- FPG
fasting plasma glucose
- SBP
systolic blood pressure
- DBP
diastolic blood pressure
- BMI
body mass index
- GSM
gray-scale median
- Plaque-IMTmax
maximum intima-media thickening
- LDA
linear discriminant analysis
- MI
mutual information
- CHD
coronary heart disease
- HDL-cholesterol
high density lipoprotein cholesterol
- LDL-cholesterol
low density lipoprotein cholesterol
- WavEnLH_s-3 and WavEnLH_s-4
energy of wavelet coefficients in vertical high-frequency subbands at scale 3 and 4
- WavEnLL_s-1, WavEnLL_s-2 and WavEnLH_s-3
energy of wavelet coefficients in low-frequency subbands at scale 1, 2 and 3
- 45dgr_Fraction, Vertl_Fraction and 135dr_Fraction
fraction of image in runs computed for 45°, vertical and 135° orientation
- Vertl_ShrtREmp, Horzl_ShrtREmp, 45dgr_ShrtREmp, Vertl_ShrtREmp and 135dr_ShrtREmp
short run emphasis computed for horizontal, 45°, vertical and 135° orientation
- TNP
total number of plaques
Footnotes
Xiao-Wei Huang and Yan-Ling Zhang contributed equally to this work and are co-first authors
Hai-Rong Zheng, Rong-Qin Zheng and Li-Li Niu are co-corresponding authors
Contributor Information
Xiao-Wei Huang, Email: xw.huang@siat.ac.cn.
Yan-Ling Zhang, Email: 15136102@qq.com.
Long Meng, Email: long.meng@siat.ac.cn.
Ming Qian, Email: ming.qian@siat.ac.cn.
Wei Zhou, Email: wei.zhou@siat.ac.cn.
Rong-Qin Zheng, Email: zhengrongqin@hotmail.com.
Hai-Rong Zheng, Email: hr.zheng@siat.ac.cn.
Li–Li Niu, Phone: 86-755-86392299, Email: ll.niu@siat.ac.cn.
References
- 1.Pasterkamp G. Methods of accelerated atherosclerosis in diabetic patients. Heart. 2013;99(10):743–749. doi: 10.1136/heartjnl-2011-301172. [DOI] [PubMed] [Google Scholar]
- 2.Chait AandBornfeldt KE Diabetes and atherosclerosis: is there a role for hyperglycemia? J Lipid Res. 2009;50(Suppl):S335–S339. doi: 10.1194/jlr.R800059-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gomez-Marcos MA, Recio-Rodriguez JI, Patino-Alonso MC, Agudo-Conde C, Gomez-Sanchez L, Rodriguez-Sanchez E, et al. Relationship between intima-media thickness of the common carotid artery and arterial stiffness in subjects with and without type 2 diabetes: a case-series report. Cardiovasc Diabetol. 2011;10:3. doi: 10.1186/1475-2840-10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang L, Yin JK, Duan YY, Liu X, Xu L, Wang J, et al. Evaluation of carotid artery elasticity changes in patients with type 2 diabetes. Cardiovasc Diabetol. 2014;13:39. doi: 10.1186/1475-2840-13-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Castellano G, Bonilha L, Li LM, Cendes F. Texture analysis of medical images. Clin Radiol. 2004;59(12):1061–1069. doi: 10.1016/j.crad.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 6.Acharya UR, Sree SV, Krishnan MM, Molinari F, Saba L, Ho SY, et al. Atherosclerotic risk stratification strategy for carotid arteries using texture-based features. Ultrasound Med Biol. 2012;38(6):899–915. doi: 10.1016/j.ultrasmedbio.2012.01.015. [DOI] [PubMed] [Google Scholar]
- 7.Menegazzo L, Poncina N, Albiero M, Menegolo M, Grego F, Avogaro A, et al. Diabetes modifies the relationships among carotid plaque calcification, composition and inflammation. Atherosclerosis. 2015;241(2):533–538. doi: 10.1016/j.atherosclerosis.2015.06.013. [DOI] [PubMed] [Google Scholar]
- 8.Wilhjelm JE, Gronholdt ML, Wiebe B, Jespersen SK, Hansen LK, Sillesen H. Quantitative analysis of ultrasound B-mode images of carotid atherosclerotic plaque: correlation with visual classification and histological examination. IEEE Trans Med Imaging. 1998;17(6):910–922. doi: 10.1109/42.746624. [DOI] [PubMed] [Google Scholar]
- 9.Niu L, Qian M, Yang W, Meng L, Xiao Y, Wong KK, et al. Surface roughness detection of arteries via texture analysis of ultrasound images for early diagnosis of atherosclerosis. PLoS ONE. 2013;8(10):e76880. doi: 10.1371/journal.pone.0076880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rakebrandt F, Crawford DC, Havard D, Coleman D, Woodcock JP. Relationship between ultrasound texture classification images and histology of atherosclerotic plaque. Ultrasound Med Biol. 2000;26(9):1393–1402. doi: 10.1016/S0301-5629(00)00314-8. [DOI] [PubMed] [Google Scholar]
- 11.Eeg-Olofsson K, Cederholm J, Nilsson PM, Zethelius B, Svensson AM, Gudbjornsdottir S, et al. New aspects of HbA1c as a risk factor for cardiovascular diseases in type 2 diabetes: an observational study from the Swedish National Diabetes Register (NDR) J Intern Med. 2010;268(5):471–482. doi: 10.1111/j.1365-2796.2010.02265.x. [DOI] [PubMed] [Google Scholar]
- 12.Aguilar D, Bozkurt B, Ramasubbu K, Deswal A. Relationship of hemoglobin A1C and mortality in heart failure patients with diabetes. J Am Coll Cardiol. 2009;54(5):422–428. doi: 10.1016/j.jacc.2009.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mellitus ECotDaCoD Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003;26(Suppl 1):S5–S20. doi: 10.2337/diacare.26.2007.s5. [DOI] [PubMed] [Google Scholar]
- 14.Goldenberg R, Punthakee Z. Definition, classification and diagnosis of diabetes, prediabetes and metabolic syndrome. Can J Diabetes. 2013;37(Suppl 1):S8–S11. doi: 10.1016/j.jcjd.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 15.Sabetai MM, Tegos TJ, Nicolaides AN, Dhanjil S, Pare GJ, Stevens JM. Reproducibility of computer-quantified carotid plaque echogenicity: can we overcome the subjectivity? Stroke. 2000;31(9):2189–2196. doi: 10.1161/01.STR.31.9.2189. [DOI] [PubMed] [Google Scholar]
- 16.Nordestgaard BG, Gronholdt ML, Sillesen H. Echolucent rupture-prone plaques. Curr Opin Lipidol. 2003;14(5):505–512. doi: 10.1097/00041433-200310000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Irie Y, Katakami N, Kaneto H, Takahara M, Nishio M, Kasami R, et al. The utility of ultrasonic tissue characterization of carotid plaque in the prediction of cardiovascular events in diabetic patients. Atherosclerosis. 2013;230(2):399–405. doi: 10.1016/j.atherosclerosis.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 18.Sharma K, Blaha MJ, Blumenthal RS, Musunuru K. Clinical and research applications of carotid intima-media thickness. Am J Cardiol. 2009;103(9):1316–1320. doi: 10.1016/j.amjcard.2009.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finn AV, Kolodgie FD, Virmani R. Correlation between carotid intimal/medial thickness and atherosclerosis: a point of view from pathology. Arterioscler Thromb Vasc Biol. 2010;30(2):177–181. doi: 10.1161/ATVBAHA.108.173609. [DOI] [PubMed] [Google Scholar]
- 20.Kadota A, Miura K, Okamura T, Fujiyoshi A, Ohkubo T, Kadowaki T, et al. Carotid intima-media thickness and plaque in apparently healthy Japanese individuals with an estimated 10-year absolute risk of CAD death according to the Japan Atherosclerosis Society (JAS) guidelines 2012: the Shiga Epidemiological Study of Subclinical Atherosclerosis (SESSA) J Atheroscler Thromb. 2013;20(10):755–766. doi: 10.5551/jat.17244. [DOI] [PubMed] [Google Scholar]
- 21.Hirano M, Nakamura T, Kitta Y, Sano K, Kodama Y, Kobayashi T, et al. Assessment of carotid plaque echolucency in addition to plaque size increases the predictive value of carotid ultrasound for coronary events in patients with coronary artery disease and mild carotid atherosclerosis. Atherosclerosis. 2010;211(2):451–455. doi: 10.1016/j.atherosclerosis.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 22.Mizuma A, Kijima C, Iijima K, Goto Y, Honma K, Yasuda T, et al. Relationship between atherosclerotic risk factors and aortic plaques in patients with first-ever ischaemic stroke. Heart Lung Circ. 2014;23(10):930–935. doi: 10.1016/j.hlc.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 23.Szczypinski PM, Strzelecki M, Materka A, Klepaczko A. MaZda–a software package for image texture analysis. Comput Methods Programs Biomed. 2009;94(1):66–76. doi: 10.1016/j.cmpb.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 24.Duda RO, Hart PE, Stork DG. Pattern classification. New York: Wiley; 2000. [Google Scholar]
- 25.Tourassi GD, Frederick ED, Markey MK, Floyd CE., Jr Application of the mutual information criterion for feature selection in computer-aided diagnosis. Med Phys. 2001;28(12):2394–2402. doi: 10.1118/1.1418724. [DOI] [PubMed] [Google Scholar]
- 26.Mazda user’s manual. http://www.eletel.p.lodz.pl/mazda/download/mazda_manual.pdf. Accessed 12 Nov 2015.
- 27.Gomez-Marcos MA, Recio-Rodriguez JI, Patino-Alonso MC, Agudo-Conde C, Gomez-Sanchez L, Gomez-Sanchez M, et al. Cardio-ankle vascular index is associated with cardiovascular target organ damage and vascular structure and function in patients with diabetes or metabolic syndrome, LOD-DIABETES study: a case series report. Cardiovasc Diabetol. 2015;14:7. doi: 10.1186/s12933-014-0167-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cox AJ, Hsu FC, Agarwal S, Freedman BI, Herrington DM, Carr JJ, et al. Prediction of mortality using a multi-bed vascular calcification score in the diabetes heart study. Cardiovasc Diabetol. 2014;13:160. doi: 10.1186/s12933-014-0160-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Galloway MM. Texture analysis using gray level run lengths. Comput Graph Image Process. 1975;4(2):172–179. doi: 10.1016/S0146-664X(75)80008-6. [DOI] [Google Scholar]
- 30.Virmani R, Burke AP, Kolodgie F. Morphological characteristics of coronary atherosclerosis in diabetes mellitus. Can J Cardiol. 2006;22(Suppl B):81b–84b. doi: 10.1016/S0828-282X(06)70991-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nozue T, Yamamoto S, Tohyama S, Fukui K, Umezawa S, Onishi Y, et al. Impact of diabetes mellitus on coronary atherosclerosis and plaque composition under statin therapy—subanalysis of the TRUTH study. Circ J. 2012;76(9):2188–2196. doi: 10.1253/circj.CJ-11-1303. [DOI] [PubMed] [Google Scholar]
- 32.Marso SP, Mercado N, Maehara A, Weisz G, Mintz GS, McPherson J, et al. Plaque composition and clinical outcomes in acute coronary syndrome patients with metabolic syndrome or diabetes. JACC Cardiovasc Imaging. 2012;5(3 Suppl):S42–S52. doi: 10.1016/j.jcmg.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 33.Lee YH, Shin MH, Choi JS, Rhee JA, Nam HS, Jeong SK, et al. HbA1c is significantly associated with arterial stiffness but not with carotid atherosclerosis in a community-based population without type 2 diabetes: the Dong-gu study. Atherosclerosis. 2016;247:1–6. doi: 10.1016/j.atherosclerosis.2016.01.032. [DOI] [PubMed] [Google Scholar]
- 34.Rundek T, Gardener H, Della-Morte D, Dong C, Cabral D, Tiozzo E, et al. The relationship between carotid intima-media thickness and carotid plaque in the Northern Manhattan Study. Atherosclerosis. 2015;241(2):364–370. doi: 10.1016/j.atherosclerosis.2015.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Garcia Garcia J, Roquer J, Serena J, Castillo J, Blanco M, Diaz-Maroto I, et al. Carotid intima-media thickness is not associated with markers of atherosclerosis in stroke patients. J Stroke Cerebrovasc Dis. 2016;25(5):1070–1075. doi: 10.1016/j.jstrokecerebrovasdis.2016.01.002. [DOI] [PubMed] [Google Scholar]
- 36.Inaba Y, Chen JA, Bergmann SR. Carotid plaque, compared with carotid intima-media thickness, more accurately predicts coronary artery disease events: a meta-analysis. Atherosclerosis. 2012;220(1):128–133. doi: 10.1016/j.atherosclerosis.2011.06.044. [DOI] [PubMed] [Google Scholar]
- 37.Alonso N, Traveset A, Rubinat E, Ortega E, Alcubierre N, Sanahuja J, et al. Type 2 diabetes-associated carotid plaque burden is increased in patients with retinopathy compared to those without retinopathy. Cardiovasc Diabetol. 2015;14:33. doi: 10.1186/s12933-015-0196-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012;35(Suppl 1):S64–S71. doi: 10.2337/dc12-s064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mukai N, Ninomiya T, Hata J, Hirakawa Y, Ikeda F, Fukuhara M, et al. Association of hemoglobin A1c and glycated albumin with carotid atherosclerosis in community-dwelling Japanese subjects: the Hisayama Study. Cardiovasc Diabetol. 2015;14:84. doi: 10.1186/s12933-015-0247-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Daida H, Takayama T, Hiro T, Yamagishi M, Hirayama A, Saito S, et al. High HbA1c levels correlate with reduced plaque regression during statin treatment in patients with stable coronary artery disease: results of the coronary atherosclerosis study measuring effects of rosuvastatin using intravascular ultrasound in Japanese subjects (COSMOS) Cardiovasc Diabetol. 2012;11:87. doi: 10.1186/1475-2840-11-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ikeda F, Doi Y, Ninomiya T, Hirakawa Y, Mukai N, Hata J, et al. Haemoglobin A1c even within non-diabetic level is a predictor of cardiovascular disease in a general Japanese population: the Hisayama study. Cardiovasc Diabetol. 2013;12:164. doi: 10.1186/1475-2840-12-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001;414(6865):782–787. doi: 10.1038/414782a. [DOI] [PubMed] [Google Scholar]
- 43.Boyle JP, Thompson TJ, Gregg EW, Barker LE, Williamson DF. Projection of the year 2050 burden of diabetes in the US adult population: dynamic modeling of incidence, mortality, and prediabetes prevalence. Popul Health Metr. 2010;8:29. doi: 10.1186/1478-7954-8-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets during and/or analysed during the current study available from the corresponding author on reasonable request.


