Abstract
In Sudan, several studies have been conducted on low birth weight, a few concentrated on pre-term births per se. The objectives of this study were to describe maternal and obstetric factors predisposing to pre-term delivery, to determine the incidence of early neonatal complications, to identify causes of early neonatal deaths and to determine survival rates relative to gestational age and birth weight. A descriptive hospital-based study was conducted at Soba University Hospital, over a seven months-period, from December 2003 to June 2004. One hundred consecutively born premature infants were followed up from the moment of delivery till the end of the first week of life. Chi squared tests and p-values, using confidence intervals of 95%, were used for analysis. Eighty four mothers gave birth to 100 premature babies who were admitted to the Neonatal Unit of Soba University Hospital. Pregnancy induced hypertension (38.1%), multiple pregnancy ( 29%) and maternal infection ( 42.9%) were the main obstetric factors predisposing to premature birth. Morbidity among the pre-term birth population showed that respiratory distress syndrome was the main disease accounting for 36% and 46.2% of the deaths, respectively. Neonatal jaundice, apnoea, and neonatal infection occurred in 46%, 16% and 14% of the premature infants, respectively. However, respiratory distress syndrome and apnoea have been strongly associated with early neonatal mortality (P<0.05). A survival rate for the whole premature infant study was 74% and survival rates increased with increasing gestational age and increasing birth weight.
Keywords: Prematurity, Early neonatal morbidity and mortality, Survival rates, Sudan
Introduction
Pre-term birth refers to a birth that occurs before 37 completed weeks (less than 259 days) of gestation. Premature infants are grouped by their gestational assessment into very premature (< 29 weeks), premature (29–32 weeks), and transitional (33 – 36 weeks) [1]. However, there is no clear cut off for a very premature infant and it is more variably defined as less than 32, 33 or 34 weeks gestation. Prediction of outcome for an individual infant, especially at the threshold of viability, remains uncertain. It appears to be approximately 23 to 25 weeks gestation or 400 to 500 grams, although exceptions may occur [2]. Survival rates among pre-term infants are expressed as a function of birth weight or gestational age. In Sudan, premature infants are more commonly included within perinatal mortality reports as a part of low birth weight infants rather than being separately investigated.
Studies aiming at predicting survival by gestational age and birth weight for infants can be of great value in facilitating decision making for clinicians and parents. Draper et al [3] conducted a study aiming at predicting survival by gestational age and birth weight for infants between 22 and 32 weeks in the United Kingdom over 3 years. Predicted survival at each and every week was plotted in graphs. Such graphs are produced for a geographically defined population so that they are representative and not biased towards the outcomes of particular centres and they should be regularly updated to allow for improvements in survival of infants.
The objectives of this study were to describe maternal and obstetric factors predisposing to pre-term delivery, the incidence of early neonatal complications associated with premature birth, to identify causes of early neonatal deaths and to determine survival rates relative to gestational age and birth weight.
Materials and Methods
This was a descriptive, prospective hospital based study done at Soba University Hospital, a referral hospital for high risk pregnancies, for a period of seven months. All consecutively live born preterm neonates delivered during the study period and their mothers were enrolled in the study. The study used pre-structured questionnaire pertaining to the preterm neonates and their mothers and the examination and follow up of the preterm infants. The birth weight of the newborn was the first weight obtained after birth (preferably within the first hour) [4]. The gestational age is the duration of gestation measured from the first day of the last menstrual period and expressed in complete weeks or days [4]. Estimation of gestational age after birth was done using certain criteria based on physical maturation and development of the nervous system by utilizing the New Ballard score which is used to estimate gestational age of infants as premature as 20 weeks [5]. Inadequate antenatal care was defined as first antenatal visit after the first trimester of pregnancy or total visits less than three [6]. Respiratory distress syndrome was diagnosed by a typical chest X-ray (initially diffuse reticulogranular mottling of the lung fields and an air bronchogram, then with increasing severity a homogenous ground glass appearance with obscured heart borders), with finding at least 2 or more of the following signs after the first hour of life [7]: Tachypnea, expiratory grunting, sternal and intercostal recessions, and cyanosis in room air or delayed onset of respiration in very immature babies. Intraventricular haemorrhage or bleeding into the ventricles requires repeated ultrasound scans for diagnosis and assessment of the degree of haemorrhage. It is subdivided into grade 2 when the ventricle is not distended and grade 3 when it is [7].
Investigations done for all study population admitted to the nursery included complete blood count, blood urea and serum sodium, potassium and calcium, total and differential serum bilirubin count, cranial and abdominal ultrasound. Investigations for selected cases included: chest X-ray, echo, and others as deemed necessary. Data collected was analyzed by SPSS. Chi squared tests and p-values using confidence intervals of 95% were used for analysis
Results
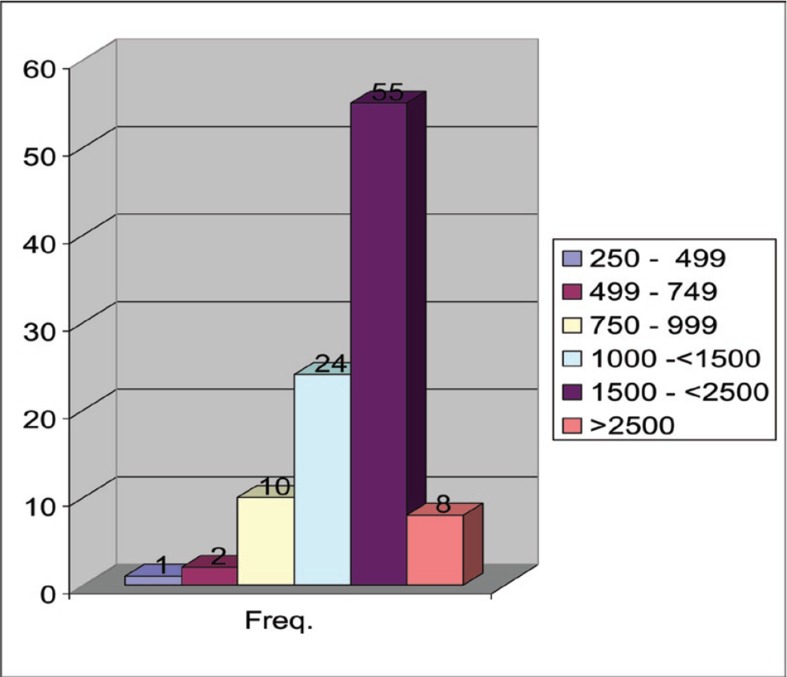
In a seven months period, one hundred consecutive live born pre-term infants delivered in Soba hospital were followed right from the moment they were delivered up to one week of age. The smallest weight live born was 410 g and was of 28 gestational age (Figures 1 and 2).
Figure 1.
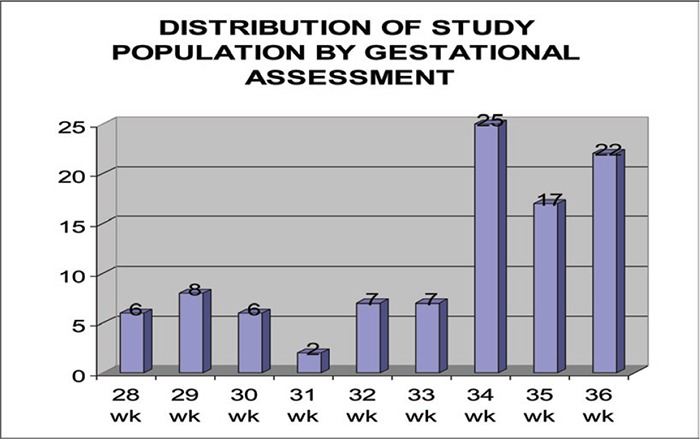
Figure 2.
Distribution of the study population by birth weight.
Pregnancy-induced hypertension was the major factor predisposing to pre-term delivery in the study population (Tables 1 and 2); accounting for 32 (38.1%) of the mothers, maternal infection in 36 (42.9%) of the mothers in the form of pyelonephritis 26 (31%) and abnormal vaginal discharge in 10 (11.9%). However, only four had confirmed infection by appropriate culture.
Table 1.
Previous obstetric history.
Obstetric complication |
Frequency |
% |
|---|---|---|
Inadequate Antenatal care |
10 |
11.9% |
First trimester anaemia |
17 |
20.2% |
Pregnancy induced hypertension |
32 |
38.1% |
Cervical incompetence |
1 |
1.2% |
Polyhydramnios |
4 |
4.8% |
Multiple pregnancy |
13 |
15.5% |
Antepartum heamorrhage |
14 |
16.7% |
Abnormal vaginal discharge |
10 |
11.9% |
Pyelonephritis |
26 |
31% |
Table 2.
Previous obstetric complications
Previous obstetric history |
Frequency |
% |
|---|---|---|
1) Pre- term birth: |
|
|
None |
76 |
90.5% |
Once |
3 |
3.6% |
Two |
3 |
3.6% |
> Two times |
2 |
2.4% |
2) Abortion: |
|
|
None |
64 |
76.2% |
Once |
13 |
15.5% |
Two or more |
7 |
8.3% |
3) Parity: |
|
|
Para 0 |
37 |
44.1% |
Para I |
16 |
19.1% |
Para II or more |
31 |
36.9% |
4) Interpregnancy interval: |
|
|
Primigravida |
30 |
35.7% |
< 18 months |
23 |
27.4% |
18 – < 59 months |
22 |
26.2% |
> 59 months |
9 |
10.7% |
Multiple pregnancies accounted for more than quarter of the premature infants study population (29%). Of these 29 preterm babies, 20 were twins and 9 were triplets.
First trimester anaemia and antepartum haemorrhage were present in 17 (20.2%) and 14 (16.7%) of the mothers respectively.
Almost half of the study population (46%) required routine neonatal resuscitation in the form of suction, stimulation and warming (Table 3). Thirty six (36%) required O2 administration. Bag and mask ventilation was delivered to 15 (15%) of the study sample. Only 3 pre-term neonates required endotracheal intubation and there was a significant association between increasing requirements of neonatal resuscitation and worsening early neonatal outcome (p-value 0.000). The highest frequencies of pre-terms were at 34, 35 and 36 weeks of gestational assessment accounting to 25%, 17% and 22%, respectively (Figure 1). From 28 to 33 weeks, it was consecutively 6%, 8%, 6%, 2%, 7% and 7%.
Table 3.
Relationship between type of neonatal resuscitation and early neonatal outcome.
Type of neonatal resuscitaion at time of delivery |
Frequency |
No. died |
|---|---|---|
Routine |
46 |
6 |
O2 administration |
36 |
8 |
Bag and mask |
15 |
9 |
Endotracheal tube |
3 |
3 |
Total |
100 |
26 |
Most of the study population (55%) was low birth weight pre-term infants (Figure 2), that is, birth weight between 1500 – < 2500 grams. Twenty four (24%) were very low birth weight (1000 – <1500). Extremely low birth weights (<1000) were 13%. Pre-terms with birth weight 2500 – 4000 grams were 8%. The most encountered morbidity among the study population (Table 4) was neonatal jaundice (46%). Six (13.04%) of those neonates died. However, there was no significant association between early neonatal jaundice and early neonatal mortality (P-value 0.06). Respiratory distress syndrome (RDS) caused morbidity in 36% of the pre-term study population. Fifteen (41.6%) of those neonates died. There was a significant association between RDS and early neonatal mortality (P-value 0.04). Other causes of respiratory distress occurred in six neonates (6%). These included two cases of congenital pneumonia, two cases of severe birth asphyxia, with or without intaventricular hemorrhage, cyanotic congenital heart disease and one was of unknown etiology. All these six neonates (100%) died. The association between this morbidity and early neonatal mortality was significant (p-value 0.004).
Table 4.
Incidence of morbidity in the study population and its outcome at the end of the first week of life.
Disease. |
Frequency |
% |
No. of deaths |
P. value |
|---|---|---|---|---|
Severe neonatal asphyxia |
3 |
3 |
3 |
0.03 |
Respiratory distress syndrome |
36 |
36 |
15 |
0.04 |
Other causes of respiratory distress |
6 |
6 |
3 |
0.04 |
Neonatal infections |
14 |
14 |
5 |
0.372 |
Hypoglycemia |
5 |
5 |
2 |
0.464 |
Hypocalcaemia |
9 |
9 |
3 |
0.599 |
Anaemia |
2 |
2 |
1 |
0.434 |
Cyanosis |
8 |
8 |
8 |
0.000 |
Polycythaemia |
1 |
1 |
0 |
0.551 |
Hypothermia |
3 |
3 |
3 |
0.003 |
Apnea |
16 |
16 |
15 |
0.000 |
Convulsions |
1 |
1 |
1 |
0.090 |
Jaundice |
46 |
46 |
6 |
0.06 |
Intraventricular haemorrhage |
18 |
18 |
18 |
0.000 |
Necrotizing enterocolitis |
4 |
4 |
3 |
0.023 |
Bleeding tendency |
8 |
8 |
6 |
0.001 |
All patients who developed intraventricular haemorrhage (18%), cyanosis (8%), severe birth asphyxia (3%) and hypothermia (3%) died. A p-value of 0.000 was found suggesting a very strong association of these morbidities to mortality. Apnea occurred in 16 neonates (16%), 15 (94%) died. It was significantly associated with mortality (p-value 0.000). Necrotizing enterocolitis occurred in 4 (4%) neonates and 3 (75%) of them died. There was a significant association related to mortality (p-value 0.023).
Bleeding tendency occurred in 8 (8%) neonates. Of the 8 pre-terms who developed bleeding tendency, seven were due to disseminated intravascular coagulation (DIC) and one due to haemorrhagic disease of the newborn. Six (75%) of those neonates who developed bleeding tendency died. There was a significant association related to mortality (p-value 0.023).
Neonatal infections, anaemia, hypoglycemia, hypocalcaemia, polycythemia and convulsions occurred in 14%, 5%, 9%, 2%, 1% and 1% of the study population, respectively. However all of them were not significantly associated with mortality (p-values: 0.372, 0.464, 0.599, 0.434, 0.551and 0.090, respectively).
Seventy one (71%) mothers received intramuscular dexamethasone antenataly. Of these 30 of their newborns developed RDS. Of the remaining 21 who didn’t receive dexamethasone, only 6 developed RDS. Dexamethasone was significantly associated with the occurrence of RDS in the study group (p-value 0.008). This was a very unusual finding, is contrary to all authentic literature and needs further research. Twenty six (26%) of the study population died and 33% were discharged. Forty one (41%) remained inside the nursery with 33% still inside the incubator by the end of the first week, and 8% still inside the nursery but outside the incubator. The number one cause of death was respiratory distress syndrome, with or without, intraventricular hemorrhage accounting for 46.2% of the total deaths. Sepsis accounted for 15.4% of the total deaths and perinatal asphyxia 11.5%.
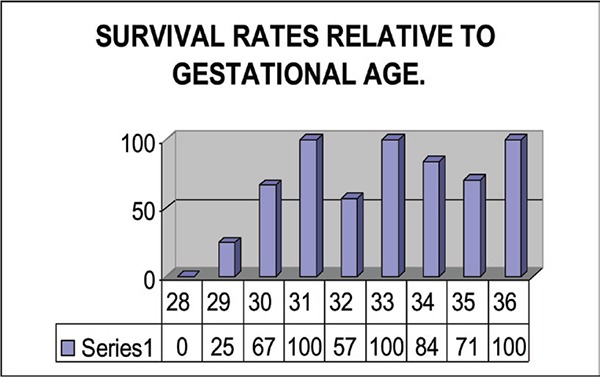
At 28 weeks the survival rate was zero and at 36 weeks it was 100% (Figure 3). Survival rates increased with increasing gestational age. It was 25% at 29 weeks, 57.1% at 32 weeks and 84% at 34 weeks. There was a significant association between increasing gestational assessment and improved early neonatal outcome (p-value 0.00).
Figure 3.
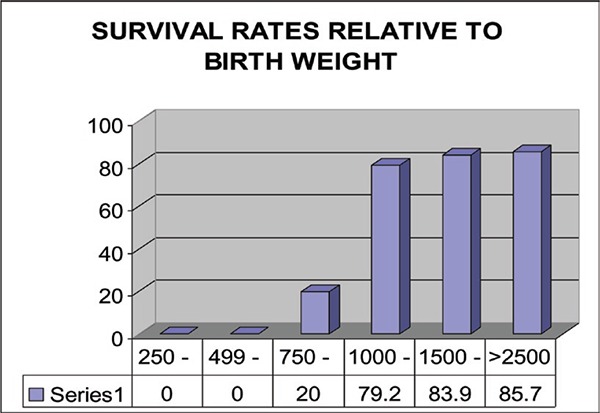
The survival rate of extremely low birth weight (<1000 g) was very low in this study (Figure 4), accounting for only 20% for birth weights 750 to 999g and zero survival rate for birth weights below 750 g. Above 1000 survival rates increased from 79.2% to 83.9% to 85.7% for birth weights 1000 – < 1500, 1500 – < 2500 and more than 2500g, respectively. There was a significant association between increasing birth weight and improved early neonatal outcome (p-value 0.00). Comparison of the outcome of preterms of singleton and multiple births revealed no significant difference (P-value 0.075).
Figure 4.
Discussion
The mothers in this study were adequately followed throughout their pregnancies in 89% of cases and they were referred to Soba University Hospital for close monitoring. The number of mothers in this study who gave birth to 100 neonates was 84, as 13 mothers had multiple pregnancies and 71 had single pregnancies. Previous history of pre-term birth was lacking in 90.48% of mothers, 76.19% of the mothers had no history of abortion, and 44.05% of the mothers were nulliparous. These factors are the reverse for what has been published in the literature as pre-term birth is more commonly associated with a prior history of spontaneous pre-term delivery as suggested by Mercer et al [8] and previous history of abortion is also a risk factor for future pre-term delivery as ascertained by zhou et al [9].
In 38.09% of the mothers, the interpregnancy interval was < 18 months or > than 59 months. Both durations have been associated with higher incidence of pre-term delivery as suggested by Taha et al [10].
The major obstetric complication encountered within the mothers in this study was pregnancy-induced hypertension (38.1%). However first trimester anemia was present in 20.2% of the mothers and maternal infection in 42.9% – Both have been ascertained as related factors in the literature as mentioned by Scholl et al [11] and Mass et al [12], respectively.
Multiple pregnancies accounted for 29% of the pre-term study population. This was similar to the results of two studies conducted by Taffel et al [13] and Ventura et al [14] through the United States National Center for Health Statistics. These studies reported that multiple pregnancies accounted for 13% of all births less than 37 weeks gestation and 15% of all early births less than 32 weeks gestation; that is 28% for the entire pre-term birth population. The major reason for this increase in preterm births is the higher rate of multiple pregnancies which rose by 19% between 1989 and 1996 due to assisted conception techniques [15].
The complications most frequently reported in the literature are hypothermia, respiratory abnormalities (including apnea and respiratory distress syndrome) hypoglycemia, necrotizing enterocolitis and infection [16]. The morbidity is of similar pattern in the present study group; however jaundice (46%) was very common amongst the study group followed by RDS (36%), apnea (16%), infection (14 %) and intraventricular haemorrhage (18%). Respiratory distress syndrome, apnea and intaventricular haemorrhage have all been strongly associated with mortality in this study (P-value <0.05).
Diagnoses of RDS and necrotizing enterocolitis were clinical as there were no mobile radiological units for diagnosis, and these infants are usually very ill and cannot be moved outside the neonatal intensive care unit. Intraventricular hemorrhage was diagnosed by postmortum tap in 8 cases of the 18 who were suspected to have the disease. Though it is routine to perform ultrasound in all pre-terms admitted to Soba University Hospital, those neonates who developed intraventricular haemorrhage were usually very ill and couldn’t be mobilized out of the nursery.
According to this study dexamethasone was significantly associated with the occurrence of RDS in the study group (p-value 0.008). The dose used by obstetricians in Soba University Hospital is 12 mg dexamethasone every 12 hours for 24 hours, which was different from that recommended in the literature as betamethasone 12 mg given intramuscularly 24 hours apart or dexamethasone four dozes 6 mg intramuscularly 12 hours apart as recommended in the literature by the American College of Obstetrics and Gynaecologists [17].
In the present study, about one-quarter (26%) of the pre-terms died during the first week. Of the 13 pre-terms who were less than 1000 g, 11 died. Survival rates increased with increasing gestational and birth weight, as is the case worldwide. The number one cause of mortality in the present study was respiratory distress syndrome (36%).
Conclusion and Recommendations
The major predisposing factors to pre-term deliveries were related to high-risk pregnancy mainly pregnancy induced hypertension, multiple pregnancy and maternal infection. Respiratory distress syndrome was the major factor influencing morbidity and mortality among the pre-term infants. This study recommends training and specialization of health workers on neonatal care and resuscitation, and conduction of more studies over geographically defined regions in Sudan aiming at assessment of prevailing neonatal services provided for preterm infants. Promotion of neonatal intensive care unit facilities, wider availability for mechanical ventilation, and more research on RDS are vitally required.
References
- 1.Rennie JM, Gandy GM. Examination of the newborn In: Rennie JM, Robertson NRC (eds). Textbook of Neonatology (3rd edition). UK: Churchill Livingstone; 1999; 286. [Google Scholar]
- 2.Hack M, Fanaroff AA. Outcomes of children of extremely low birth weight and gestational age in the 1990’s. Early Hum Dev 1999; 53: 193. [DOI] [PubMed] [Google Scholar]
- 3.Elizabeth S, Draper, Monktelow B, Field DJ, James D. Prediction of survival for preterm births by weight and gestational age: Retrospective population based study. BMJ 1999; 319; 1093– 1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maslow N. Standard and Clinical audit In: Rennie JM, Robertson NRC (eds). Textbook of Neonatology (3rd Edition). UK: Churchill Livingstone; 1999; 44. [Google Scholar]
- 5.Ballard JL, Khoury JC, Wedig K, et al. New Ballard Score expanded to include extremely premature infants. J Pediatr 1991; 119: 417. [DOI] [PubMed] [Google Scholar]
- 6.Hildingsson I, Radestad I, Waldenstrom U. Number of antenatal visits and womens’ opinion. Acta Obstit Gynn Scandinavica 2005; 84(3): 248. [DOI] [PubMed] [Google Scholar]
- 7.N McIntosh. The newborn In: Cambell AGM, Neil McIntosh (eds). Forfar and Arneil textbook of Paediatrics (5th edition). UK: Churchill livingstone; 1998;177–250. [Google Scholar]
- 8.Mercer BM, Goldenberg RL, Moawad AH, Meis PJ, Iams JD, Das AF, et al. The preterm prediction study: effect of gestational age and cause of preterm birth on subsequent outcome. National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Am J Obstet Gynecol 1999; 181: 1216. [DOI] [PubMed] [Google Scholar]
- 9.Zhou W, Sorensen HT, Olsen J. Induced abortion and subsequent pregnancy duration. Obstet Gynecol 1999; 94: 948. [DOI] [PubMed] [Google Scholar]
- 10.Taha ET, Gray RH, Abdelwahab MM, Abdelhafiz A. Distribution and determinants of low birth weight in central Sudan. Peadatric and Perinatal Epidemiology 1995; 9: 185–200. [DOI] [PubMed] [Google Scholar]
- 11.Scholl TO, Reilly T. Anemia, iron and pregnancy outcome. J Nutr 2000; 130: 443S. [DOI] [PubMed] [Google Scholar]
- 12.Mass SB, Brennan JP, Silverman N, Van Hoeven KH. Association between a shift in vaginal flora on papanicolaou smear and acute chorioamnionitis and preterm delivery. Diagn Cytopathol 1999; 21: 7. [DOI] [PubMed] [Google Scholar]
- 13.Taffel SM. Health and demographic characteristics of twin births: United States 1988. National Center for Health Statistics. Vital and Health Statistics 1997; 21: 55. [PubMed] [Google Scholar]
- 14.Ventura SJ, Martin JA, Curtin SC, et al. Report of final natality statistics, 1995. Monthly Vital Stat Rep 1997; 45: 11. [PubMed] [Google Scholar]
- 15.Pre-term singleton births- United States, 1989–1996. MMWR 1999; 48–85. [PubMed]
- 16.Mandy GT. Short-term complications of the premature infant. Available at: http://www.uptodate.com/contents/short-term-complications-of-theprematue-infant.
- 17.American College of Obstetricians and Gynecologists. Committee on Obstetric Practice. ACOG Committee Opinion No. 402: Antenatal corticosteroid therapy for fetal maturation. Obstet Gynecol 2008; 111: 805. [DOI] [PubMed] [Google Scholar]