Abstract
Background
Individuals with aphasia often receive therapy from a speech-language pathologist during acute rehabilitation. The literature demonstrates that group-based therapy provides a natural, social environment for language rehabilitation in mild-moderate and/or chronic aphasia; however, the communication of persons with acute, severe non-fluent aphasia during group treatment has not been fully explored.
Objective
This observational study investigated patient communication during acute rehabilitation. The primary objective was to determine whether participants initiate more communication during group therapy sessions when compared to individual therapy sessions.
Method
Ten participants with severe non-fluent aphasia were observed during one individual and one group session during their stay in an acute, inpatient rehabilitation facility. Communicative initiations were tallied and categorized based on type, target, and purpose.
Results
Participants initiated communication more often during group sessions than during individual sessions. During groups, participants used more vocalizations and facial expressions to communicate, and the purpose was more often for social closeness than in individual sessions. Participants produced fewer different, real words in group vs. individual sessions, but other measures of communication skill did not differ significantly between the two settings.
Conclusion
In the aphasia group treatment described in this study, participants initiated more communication, with greater diversity of expressive modalities and more varied communicative purposes. Participants in group therapy also showed an increased tendency to communicate for the purpose of social closeness. These findings suggest that there are important differences in the communication of patients participating in group vs. individual speech therapy for treatment of acute, severe non-fluent aphasia.
Keywords: Aphasia, Adults, Intervention, Acute rehabilitation, Language disorders, Group therapy, Service delivery, Outcomes, Social communication
BACKGROUND AND RATIONALE
The current aphasia rehabilitation literature provides evidence that behavioral therapy with a speech-language pathologist (SLP) improves language functions in individuals with aphasia.1 SLP therapy can take many forms and an important distinction exists between individual therapy, between an SLP and a single person with aphasia, and group therapy, where multiple persons with aphasia participate in treatment together.2 The group paradigm promotes pragmatic skills and increases the variety of communication functions and speech acts.3,4 There is evidence in the literature that group therapy is effective for improving language and communication in aphasia. For example, Elman and Bernstein-Ellis (1999) found that group therapy, compared to no therapy, led to improved performance on objective communication and language measures in chronic aphasia.5 Elman suggests that the intangibles of the group paradigm (providing a wider array of communication partners, more natural tasks, peer modeling, and support) may lead to carryover and generalization of treatment gains.6 More recently, Elman identified the unique ability of group treatment to connect people with aphasia to one another, when compared with individual treatment alone.7
While historical models of aphasia assessment and treatment focused on linguistic competence, SLPs now also devote attention to pragmatic competence and overall functionality of communication.3,4 A greater emphasis is placed on improving patients’ social communication skills to increase life participation.8 Clinicians strive to facilitate generalization of communicative competence to natural, community-based settings.9 While aphasia groups can be impairment-based, the nature of the group setting tends to elicit functional, naturalistic forms of communication. The group treatment described in this pilot study aims to produce measurable patient outcomes in both linguistic and pragmatic competence, with an overarching goal of increasing functionality of communication in individuals with acute, severe non-fluent aphasia, whose verbal output is extremely limited.
The main hypothesis for this study is that group therapy provides a more supportive environment for initiating communication, when compared to individual treatment sessions. Multiple lines of research point toward the importance of initiation in communication. Wilcox (1983) identifies initiating and sustaining an interaction as one of three pragmatic skills required for socially appropriate communication.4 A competent communicator has been defined as someone who shows interest in others, actively participates, and takes turns in a symmetrical fashion.10,11 Initiation is a relevant factor in communication in aphasia, particularly in the group setting, as exemplified by the Aphasia Center of California's use of initiation as a goal for members of its communication groups.12 The concept of initiation is particularly relevant for individuals with severe, non-fluent aphasia. Because of these patients’ limited communicative output, clinicians may employ highly structured interventions during one-on-one treatment sessions, focusing on repeated production of a limited number of targets. These interventions may be effective but may also minimize the opportunity for patients’ spontaneous initiation. Additionally, the nature of one-on-one SLP treatment can generate a role imbalance between “incompetent” patient and “competent expert” practitioner.13 Group treatment may afford greater opportunity for patients to initiate communication, capitalizing on preserved ability and maximizing perceived communication competence. As such, group treatment may afford greater opportunity for the type of generalization that is so essential to social models of aphasia rehabilitation.14
Previous research on aphasia groups has often focused on mild-moderate aphasia treatment and/or effectiveness of communication in the chronic stage, as opposed to acute, severe aphasia.5,15,16 It has also focused on support and counseling rather than direct language measures. The current pilot study aimed to fill these gaps by critically examining the communication characteristics of persons with severe aphasia during individual vs. group therapy during acute rehabilitation. It was implemented via observation during the participants’ natural course of therapy, so the study design was partially constrained by the real-life characteristics of therapy in an inpatient hospital setting (e.g., 1-hour sessions, varying group size, potential family presence). Although this observational approach limited our control over the design, we present an ecologically valid set of data regarding the differences between typical individual and group treatment in our particular hospital setting.
We addressed two primary research questions:
Do participants with acute, severe non-fluent aphasia initiate more frequent communication during group treatment than individual treatment, and what is the nature of those communicative attempts?
Do other measures of communication skills (e.g., yes/no question accuracy, number of different real words, percent accurate automatic speech) differ between treatment settings?
We predicted that participants would initiate more frequent communicative acts during group treatment sessions when compared with individual treatment sessions. Additionally, we predicted that the overall quality of communication would not be reduced in the group setting, i.e., other important aspects of language function would not differ between the two settings. This latter research question is important for addressing potential criticisms of group therapy, which are considered in the Discussion section.
METHODS
The study received approval from the MedStar Health Research Institute Institutional Review Board.
Participants
The participants were 10 inpatients in an acute rehabilitation program. All participants had onset of a left-hemisphere stroke within the previous three months, as confirmed by computerized tomography (CT) scan, magnetic resonance imaging (MRI) or physician examination. All participants were diagnosed with severe non-fluent or global aphasia based on a Western Aphasia Battery Fluency subtest score of 0, 2, or 4.17,18 Many of the participants had a suspected diagnosis of concomitant verbal apraxia, a common comorbidity of non-fluent aphasia. All participants were native English speakers without history of mental illness or significantly decreased visual and/or hearing acuity. See Table 1 for demographic information.
Table 1.
Characteristics of the ten participants.
| Participant | Gender | Age | Time Post Onset (weeks) | Education (years) | Occupation | Handedness | Site of Lesion | BDAE Complex Ideational Material | WAB Fluency |
|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 62 | 2 | 16 | Retired; FBI | R | Left MCA occlusion | 1 | 0 |
| 2 | M | 49 | 3 | 12 | HVAC installation | R | Left MCA and right posterior parietal lobe infarcts | 2 | 4 |
| 3 | F | 87 | 2 | 12 | Retired; food service | R | Left frontal ischemic infarcts | 0 | 2 |
| 4 | F | 39 | 11 | 16 | Nurse | L | Acute left temporoparietal infarcts, non-acute left frontal and cerebellar infarcts | 0 | 2 |
| 5 | F | 61 | 2 | 12 | Retired; unknown | R | Left basal ganglia hemorrhage | 0 | 0 |
| 6 | F | 51 | 2 | 12 | Director for DC housing authority | L | L MCA infarct | 1 | 2 |
| 7 | F | 66 | 2 | 18 | Retired; Bureau of Printing and Engraving | R | L MCA ischemic infarct | 4 | 0 |
| 8 | M | 56 | 3 | 10 | Restaurant cook | R | L frontoparietal infarct with extension into the basal ganglia | 2 | 1 |
| 9 | M | 67 | 2 | 16 | Retired; branch head at the Naval Air Station | R | L insular infarct with occlusion of the M2 branch of the MCA | 0 | 4 |
| 10 | M | 49 | 11 | 16 | Personal security guard for a government official | R | L MCA infarct | 0 | 0 |
Procedures
The Augmentative Communication Group (ACG) is an SLP-led group for persons with severe aphasia in an acute, inpatient rehabilitation facility. Many aphasia groups described in the literature are conversation-based and are relatively stable in membership over time, but ACG differs in both aspects.5,19 It blends traditional, impairment-based approaches with more functionally-driven, life participation approaches. ACG membership changes frequently, often day-by-day, with group size ranging from 2-6 participants. Mean group size for the ten sessions observed for this study was 3.5 (SD=1.27). Only one individual was being observed for the research study during any given group session.
Each ACG session begins with a “warm-up” consisting of introductions, a review of the session's plan, and a set of automatic speech tasks (i.e., counting 1-10, days of the week, months of the year). Depending on the particular needs of the group, basic motor speech tasks may be included. Then, there is a structured language activity such as object naming/gesturing, simple cooking procedures (e.g., making lemonade), or games (e.g., card games, dominoes). The activity incorporates established cueing hierarchies for auditory comprehension and verbal expression with an emphasis on multi-modal communication and principles of Melodic Intonation Therapy.20 Although the group is not specifically designed to target increased patient initiations, the structured activities are designed to encourage interactions between group members. The treatment activities during individual sessions also included automatics, yes/no questions and other auditory comprehension tasks, structured conversation, as well as some reading/writing activities (see Table 2 for specific activities of each observed session).
Table 2.
Description of the treatment activities for each individual and group session observed. All group therapy activities were preceded by a “warm-up” consisting of introductions, a review of the plan for the day's session, and a set of automatic speech tasks.
| Participant | Group size (# patients) | Description of activities during individual treatment | Description of activities during group treatment |
|---|---|---|---|
| 1 | 3 | • Automatic speech tasks • Apraxia drills • Oral-motor movements • Functional gestures • Reading/writing (word level) |
• Structured conversation re: previous daily activities • Game of “Hangman” |
| 2 | 2 | • Structured conversation re: football • Category naming • Writing |
• Structured conversation re: weekend plans • Game of “Wheel of Fortune” |
| 3 | 5 | • Counting/automatics • Apraxia drills • Yes/no questions • Structured conversation re: cooking |
• Yes/no questions • Making choices on communication boards • Structured conversation re: personal information |
| 4 | 4 | • Structured conversation • Automatics • Reading – matching task • Yes/no questions • Writing personal information |
• Making lemonade (using multiple modalities in order to make requests for utensils, ingredients, etc.) |
| 5 | 2 | • Automatics • Yes/no questions • Structured conversation re: pie • Writing at word level • Singing • Communication book/core words |
• Game of “Go Fish” |
| 6 | 3 | • Structured conversation re: lunch • Yes/no questions • Reading at word level • Picture description |
• Making pudding |
| 7 | 3 | • Structured conversation • Communication boards • Core words and apraxia drills • Writing/reading at word level • Functional gestures |
• Singing • Auction |
| 8 | 3 | • Structured conversation re: football • Automatics • Yes/no questions • Naming (verbal and written) • Reading at word level |
• Singing • Game of “Hangman” |
| 9 | 4 | • Structured conversation • Reading • Oral spelling • Picture description • Automatic speech tasks |
• Making lemonade |
| 10 | 6 | • Oral-motor movements • Yes/no questions • Reading/writing at word level • Structured conversation |
• Singing • Auction |
For this study, participants were observed during one ACG session and one individual session on the same day. All sessions were conducted by a single certified SLP with four years of clinical experience, who was blinded to the objectives and measures of the study. The researchers provided no guidelines regarding her choice of treatment activities for individual or group sessions; the observed activities thus represent a clinically-informed set of tasks selected to target the participants’ treatment goals. The order of sessions within the day was counterbalanced across participants, with 5 participants receiving group treatment first and 5 participants receiving individual treatment first. To ensure that participants had adjusted to the group treatment process, observations occurred between the fifth and tenth ACG-treatment days. All observations were performed live by a certified SLP with two years of clinical experience (M.F.) and included:
The occurrence of participant-initiated communicative behaviors
Accuracy of yes/no responses
Accuracy of speech automatics (counting 1-10)
Number of different, real words produced during non-automatic speech tasks
For this study, initiation was defined as “a self-generated expressive act not in direct response to communication from a conversational partner,” in order to capture all (and only) instances in which the participant took the pragmatic role of initiator. This definition encompasses verbal and non-verbal communication, as recent literature shows that gestures can play an important role in the communication (and recovery trajectory) of individuals with aphasia.21,22
When documenting participant-initiated communication, the observer categorized the specific characteristics of each communicative act, including type, target, and purpose of the attempt. The types of communication included: verbalization, vocalization, facial expression/eye contact, pointing/showing, iconic, and tactile. Potential targets of the communicative act were: the SLP, a peer, an observer, or the participant himself/herself. The purposes of communication included: information transfer, expression of wants/needs, social closeness, social etiquette, and self-talk. The purpose for each initiation was identified based on observation of the communicative context, resulting in some instances when the observer judged the purpose of the communicative act to be unidentifiable.
To ensure certainty of yes/no response accuracy, only transparent responses to objective/factual questions were used; responses to questions regarding preferences (e.g., “Do you like football?”) or other unverifiable information were excluded. Self-corrected responses to yes/no questions were counted as a singular, correct response. For accuracy of speech automatics (e.g., counting 1-10), productions with sound distortions or phonemic paraphasias were considered to be accurate if they were recognizable in context. To identify the number of different, real words produced by each participant, all spoken utterances (except automatic speech) were transcribed by the observer during the session. The first instance of each recognizable word produced was counted as a novel word. We acknowledge the inherent challenges in performing accurate, reliable live transcription, but we were unfortunately unable to videotape group sessions due to privacy reasons. Note that our participants produced mostly single word utterances and the average number of words produced by a participant during an entire 60-minute session was 47.7 words (see Table 3 for individual data), making live scoring feasible. All data were analyzed in SPSS 21 using nonparametric Wilcoxon signed-rank tests for related samples.
Table 3.
Observation data by individual participant and group means/standard deviations calculated across all 10 participants [*Participant 9 produced no transparent yes/no responses during either session].
| Participant | Number of Initiations | Percentage accuracy: Yes/no questions | Percentage accuracy: Counting 1-10 | Number of different, real words | ||||
|---|---|---|---|---|---|---|---|---|
| Individual | Group | Individual | Group | Individual | Group | Individual | Group | |
| 1 | 1 | 5 | 85.71 | 100 | 72 | 52.5 | 7 | 5 |
| 2 | 2 | 5 | 100 | 100 | 100 | 100 | 203 | 65 |
| 3 | 2 | 8 | 86.67 | 100 | 73.33 | 68.33 | 42 | 21 |
| 4 | 22 | 14 | 50 | 66.66 | 70 | 78 | 55 | 48 |
| 5 | 7 | 20 | 83.3 | 76.9 | 60 | 30 | 8 | 10 |
| 6 | 21 | 29 | 78.3 | 100 | 95 | 82.5 | 85 | 61 |
| 7 | 7 | 9 | 100 | 100 | 5 | 30 | 1 | 4 |
| 8 | 4 | 14 | 80 | 0 | 58 | 50 | 70 | 50 |
| 9 | 17 | 19 | --- | --- | 14 | 20 | 163 | 56 |
| 10 | 2 | 4 | 85.71 | 100 | 0 | 0 | 0 | 0 |
| Mean (SD) | 8.5(2.62) | 12.7(2.56) | 83.3(4.6) | 82.6(10.6) | 54.7(11.4) | 51.1(9.9) | 63.4(22.3) | 32.0 (8.3) |
Inter-rater reliability
For three randomly selected participants, sessions were simultaneously observed by a second certified SLP with 13 years of clinical experience (B.H.). Data were collected throughout the 60-minute treatment sessions by both SLPs without awareness of each other's recordings. Inter-rater reliability was very good for number of initiations (r=0.95) and for the specific category codes of type, target, and purpose (r=0.90). Additionally, inter-rater reliability was excellent for accuracy of yes/no responses (r=0.99), accuracy of automatics (r=0.98), and number of different, real words produced (r=0.99).
RESULTS
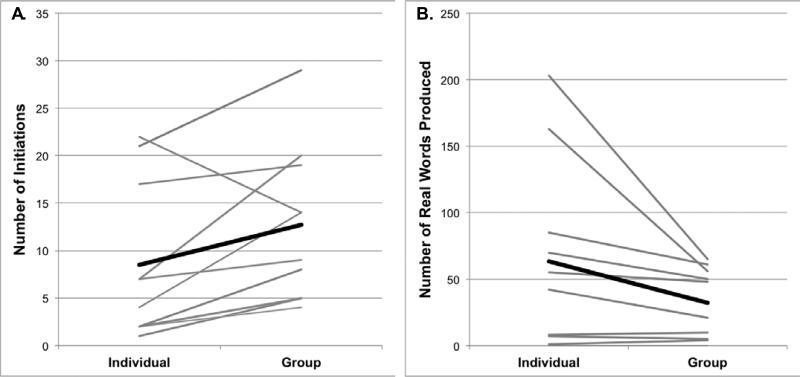
Overall, participants initiated communication significantly more often during group treatment than in individual treatment (Wilcoxon Z=2.045, p=.041). Participants took the role of initiator an average of 12.7 times (SD=2.56) during group therapy, whereas they initiated communication during individual treatment an average of 8.5 times (SD=2.62) (see Figure 1A and Table 3). This pattern was fairly consistent across the group of participants, with 9/10 participants initiating more communication in group therapy when compared to individual therapy (Binomial p=.01)
Figure 1.
Observational data taken from the individual and group sessions, with each thin, gray line representing a single participant across the two settings and each thick, black line representing the group mean (across N=10). A. Number of initiations produced in each session (see Discussion text for a description of the single participant with a downward slope). B. Number of different, real words produced in each session.
The type, target, and purpose of patient-initiated communication also differed between the two treatment settings. With regard to the type of communication, participants in group settings used more frequent vocalizations (Z=2.232, p=.026) and facial expressions (Z=2.161, p=.031) when compared to individual treatment (See Table 4). Participants also communicated more frequently for the purpose of social closeness (Z=2.677, p=.007) during group treatment compared to individual treatment (See Table 4). There was also a significant difference in the variety of ways in which these participants communicated. In group, participants demonstrated more varied targets of initiations (Z=2.714, p=.007), different types of initiations (Z=2.215, p=.027), and marginally different purposes for initiations (Z=1.912, p=.056), when compared to individual treatment.
Table 4.
Types and purposes of patient-initiated communicative exchanges in individual vs. group therapy (raw observational data collapsed across n=10).
| Individual | % of total | Group | % of total | ||
|---|---|---|---|---|---|
| Types of Patient-Initiated Communication | Vocalization | 17 | 20 | 27 | 21.3 |
| Verbalization | 50 | 58.8 | 48 | 37.8 | |
| Facial Expression/Eye Contact | 18 | 21.2 | 39 | 30.7 | |
| Point/Show | 9 | 10.6 | 14 | 11 | |
| Iconic | 15 | 17.6 | 28 | 22 | |
| Tactile | 0 | 0 | 0 | 0 | |
| Purposes of Patient-Initiated Communication | Information Transfer | 29 | 34.1 | 44 | 34.6 |
| Wants/Needs | 9 | 10.6 | 7 | 5.5 | |
| Social Closeness | 7 | 8.2 | 52 | 40.9 | |
| Social Etiquette | 9 | 10.6 | 12 | 9.4 | |
| Self-talk | 33 | 38.8 | 27 | 21.3 | |
| Unknown | 4 | 4.7 | 6 | 4.7 | |
Accuracy of yes/no responses (Z=1.016, p=.31, Group mean 82.6% (SD=10.6%), Individual 83.3% (4.6%)) and accuracy of speech automatics (Z=−.771, p=.44, Group 51.1%(9.9%), Individual 54.7%(11.4%)) did not significantly differ across treatment type. Participants did, however, produce fewer different real words during group treatment compared with individual treatment (Z=−2.134, p=.033, Group 32.0(8.3%), Individual 63.4(22.3%)) (see Figure 1B).
DISCUSSION
Aphasia researchers have identified the need for additional research in early post-stroke recovery.23 Our findings demonstrate that persons with severe non-fluent aphasia in the early stages of post-stroke recovery display different communication behaviors in group vs. individual therapy. As described in the Methods section, we did not control the SLP's selection of treatment activities across the two settings, so our findings cannot be interpreted as resulting purely from the difference in number of patients present during each treatment type. A prospective comparison of group vs. individual therapies (matched on treatment tasks and other variables) would be needed to address this question; however, findings of such a tightly controlled study might not generalize to clinical practice. In clinical settings, SLPs take advantage of the unique therapeutic opportunities provided by different session types, so group and individual sessions differ substantially in their format. In this pilot study, we sought to examine these natural differences and draw our conclusions in the context of all aspects of our group treatment setting, including the number of participants as well as the more naturalistic, socially interactive tasks that the SLP is likely to select in such an environment.
This study was not designed to prove that group therapy is more effective than individual therapy for acute, severe non-fluent aphasia. Rather, we set out to examine measurable differences in these participants’ communication across the two settings. We describe observations in the clinically relevant context of our acute rehabilitation hospital. The primary outcome measure was the number of initiations made by persons with aphasia during group and individual speech therapy sessions, as initiation plays an important pragmatic role in communication.4 The results of the study demonstrate that individuals with acute, severe non-fluent aphasia more readily initiate communication in group treatment when compared to individual treatment. As shown in Figure 1A, nine of ten individual participants followed this pattern. Notably, the majority of the communication initiated by Participant 4 (the only outlier) during her individual session was repeated self-talk during a reading task, suggesting that her outlier status resulted from an inflated number of productions of a single utterance. Additionally, we do not assume that quantity of output necessarily equals quality, although it should be noted that this population is not prone to the excessive/inappropriate output observed in other patients with neurological disorders or injury (e.g., traumatic brain injury or Wernicke's aphasia).
Our data regarding type, target, and purpose of each communicative exchange suggest that group treatment can be a natural communication setting. Participants used a larger variety of expressive modalities for a greater number of communicative purposes while participating in group therapy. In groups, participants were more likely to initiate communication via vocalizations (e.g., laughter) or facial expressions (e.g., eye contact, smiling), suggesting that group settings facilitate the use of a wider variety of communicative acts. The purpose of peer-to-peer communication during group observation frequently appeared social in nature (e.g., commiseration, shared attention, providing assistance), supporting prior research indicating that one of the primary benefits of group treatment sessions is the opportunity for peer-to-peer communication.5,6,19
In our observations, we attempted to address potential criticisms of group therapy, specifically that (1) fewer instances of clinician-driven feedback may result in decreased accuracy or success of communicative output from group members; and that (2) group therapy sessions may not provide as many opportunities for active, expressive output as individual sessions, due to the collaborative, project-centered nature of group activities or simply the larger number of communicators competing for floor time. To address the first concern, we collected data regarding accuracy of yes/no responses and accuracy of automatic speech production; results show that participants were able to achieve similar levels of performance in these objective measures across the two treatment settings. To address the second concern, we examined the number of different, real words during each session. We found that participants produced a greater number of different words in individual sessions when compared to group settings. This result might demonstrate a limitation of group therapy, but there are two alternate interpretations. First, the observed individual therapy sessions may have been more constrained to the verbal domain, whereas group therapy may have allowed for more nonverbal communication (see Table 4 for evidence of these differences). Second, the quality of verbal output may have differed across the two settings. During individual sessions, verbal output often emerged during repetition or structured naming tasks, whereas verbal output in group settings resulted from more conversational, unstructured contexts. Specific investigation of the nature and quality of verbal output in these two settings would be useful to explain such differences.
To demonstrate whether these findings truly reflect a positive role of group therapy in aphasia recovery, future research should explore the relationships between patient-initiated communication, general measures of communicative effectiveness, and other objective language outcomes (e.g., performance on a standardized aphasia battery). Further research should also focus on determining the ideal size and format of group treatments to maximize the potential positive characteristics identified here, as these aspects could not be experimentally manipulated within the constraints of this pilot, observational study. Importantly, further studies will also be needed to evaluate outcomes of inpatient aphasia rehabilitation programs that include group therapy versus those that are restricted to individual therapy alone.
CONCLUSION
In today's rehabilitation health care environment, SLPs are expected to achieve functional outcomes quickly and efficiently. Group therapy creates a milieu to address functional, pragmatic communication goals for those with severe aphasia by eliciting increased initiation of communication and a greater diversity of expressive modalities, when compared to individual therapy. Although the design of this study does not allow us to determine why these differences exist, our findings represent preliminary evidence of measurable differences in patient communication across the two settings and indicate that group therapy is a valuable adjunct to individual SLP interventions for persons with acute, severe non-fluent aphasia.
Acknowledgments
M.E.F. is supported by National Institutes of Health (NIH) Grant F31DC014875. P.E.T. is supported by National Institutes of Health (NIH) Grant KL2TR000102, Doris Duke Charitable Foundation Grant 2012062, and the Vernon Family Trust.
Footnotes
Disclosures
No authors have any conflicts of interest to disclose at the time of submission.
Reporting Requirements
This manuscript was prepared in accordance with the reporting standards for observational studies provided by the STROBE checklist.
References
- 1.Brady M, Kelly H, Godwin J, Enderby P. Speech and language therapy for aphasia following stroke (Review). Cochrane Libr. 2012:5. doi: 10.1002/14651858.CD000425.pub3. [DOI] [PubMed] [Google Scholar]
- 2.Fama ME, Turkeltaub PE. Treatment of poststroke aphasia: Current practice and new directions. Semin Neurol. 2014;1(212):504–513. doi: 10.1055/s-0034-1396004. [DOI] [PubMed] [Google Scholar]
- 3.Lyon JG. Communication use and participation in life for adults with aphasia in natural settings: The scope of the problem. Am J speech-language Pathol. 1992;1:7–14. [Google Scholar]
- 4.Wilcox MJ. Aphasia: pragmatic considerations. Top Lang Disord. 1983;3:35–48. [Google Scholar]
- 5.Elman RJ, Bernstein-Ellis E. The efficacy of group communication treatment in adults with chronic aphasia. J Speech, Lang Hear Res. 1999;(42):411–419. doi: 10.1044/jslhr.4202.411. [DOI] [PubMed] [Google Scholar]
- 6.Elman RJ. Introduction to group treatment of neurogenic communication disorders. In: Elman RJ, editor. Group Treatment of Neurogenic Communication Disorders: The Expert Clinician's Approach. 2nd ed. Plural Publishing, Inc.; San Diego: 2007. [Google Scholar]
- 7.Elman RJ. The importance of aphasia group treatment for rebuilding community and health. Top Lang Disord. 2007;27:300–308. [Google Scholar]
- 8.Chapey R, Duchan JF, Elman RJ, et al. Life-Participation Approach to Aphasia: A Statement of Values for the Future. In: Chapey R, editor. Language Intervention Strategies in Aphasia and Related Neurogenic Communication Disorders. 4th ed. Lippincott Williams and Wilkins; Baltimore, MD: 2001. pp. 279–289. [Google Scholar]
- 9.Williamson D. Maximizing Outcomes in Group Treatment of Aphasia: Lessons Learned From a Community-Based Center. Perspect Neurophysiol Neurogenic Speech Lang Disord. 2014;24(3):100. doi:10.1044/nnsld24.3.100. [Google Scholar]
- 10.Light JC. Interaction involving individuals using augmentative and alternative communication systems: state of the art and future directions. Augment Altern Commun. 1988;4:66–82. [Google Scholar]
- 11.Light JC, Binger C. Building communication competence for individuals who use augmentative and alternative communication. Paul H. Brookes Publishing Co.; Baltimore: 1988. [Google Scholar]
- 12.Bernstein-Ellis E, Elman RJ. Aphasia group communication treatment: The Aphasia Center of California approach. In: Elman RJ, editor. Group Treatment of Neurogenic Communication Disorders: The Expert Clinician's Approach. 2nd ed. Plural Publishing, Inc.; San Diego: 2007. [Google Scholar]
- 13.Simmons-Mackie N, Damico JS. Social Role Negotiation in Aphasia Therapy: Competence, Incompetence, and Conflict. In: Kovarsky D, Maxwell M, Duchan JF, editors. Constructing (in)competence: Disabling Evaluations in Clinical and Social Interaction. Psychology Press; New York: 2013. pp. 313–341. [Google Scholar]
- 14.Kearns KP, Elman RJ. Group therapy for aphasia: Theoretical and practical considerations. In: Chapey R, editor. Language Intervention Strategies in Adult Aphasia. 4th ed. Williams & Wilkins; Baltimore: 2001. pp. 316–337. [Google Scholar]
- 15.Bollinger RL, Musson ND, Holland AL. A study of group communication intervention with chronically aphasic persons. Aphasiology. 1993;7(3):301–313. [Google Scholar]
- 16.Wertz RT, Collins MJ, Weiss D, et al. Veterans Administration cooperative study on aphasia: a comparison of individual and group treatment. J Speech Hear Res. 1981;24(4):580–594. doi: 10.1044/jshr.2404.580. [DOI] [PubMed] [Google Scholar]
- 17.Kertesz A. Western Aphasia Battery - Revised. 2006 [Google Scholar]
- 18.Trupe EH. Reliability of rating spontaneous speech in the Western Aphasia Battery: Implications for classification. In: Brookshire R, editor. Clinical Aphasiology Conference: Proceedings of the conference. BRK Publishers; Minneapolis: 1984. pp. 55–69. [Google Scholar]
- 19.Simmons-Mackie N, Damico JS. Engagement in Group Therapy for Aphasia. Semin Speech Lang. 2009;1(212):18–26. doi: 10.1055/s-0028-1104531. doi:10.1055/s-0028-1104531. [DOI] [PubMed] [Google Scholar]
- 20.Helm-Estabrooks N, Martin AL. Manual of aphasia therapy. Pro-Ed; Austin, TX: 1991. [Google Scholar]
- 21.Rose ML. The utility of arm and hand gestures in the treatment of aphasia. Int J Speech Lang Pathol. 2006;8(2):92–109. doi:10.1080/14417040600657948. [Google Scholar]
- 22.Marshall J, Best W, Cocks N, et al. Gesture and naming therapy for people with severe aphasia: a group study. J Speech Lang Hear Res. 2012;55(3):726–38. doi: 10.1044/1092-4388(2011/11-0219). doi:10.1044/1092-4388(2011/11-0219) [DOI] [PubMed] [Google Scholar]
- 23.Peach RK. Further Thoughts regarding Management of Acute Aphasia following Stroke. Am J Speech-Language Pathol. 2001;10(1):29–36. doi:10.1044/1058-0360(2001/005) [Google Scholar]